Abstract
Objective
The aim of this study was to evaluate whether excursions of blood pressure from the optimal mean arterial pressure during and after cardiac surgery are associated with postoperative delirium identified using a structured examination.
Design
Prospective, observational study.
Setting
University hospital.
Participants
The study included 110 patients undergoing cardiac surgery.
Interventions
Patients were monitored using ultrasound-tagged near-infrared spectroscopy to assess optimal mean arterial pressure by cerebral blood flow autoregulation monitoring during cardiopulmonary bypass and the first 3 hours in the intensive care unit.
Measurements and Main Results
The patients were tested preoperatively and on postoperative days 1 to 3 with the Confusion Assessment Method or Confusion Assessment Method for the Intensive Care Unit, the Delirium Rating Scale-Revised-98, and the Mini Mental State Examination. Summative presence of delirium on postoperative days 1 through 3, as defined by the consensus panel following Diagnostic and Statistical Manual of Mental Disorders-IV-TR criteria, was the primary outcome. Delirium occurred in 47 (42.7%) patients. There were no differences in blood pressure excursions above and below optimal mean arterial pressure between patients with and without summative presence of delirium. Secondary analysis showed blood pressure excursions above the optimal mean arterial pressure to be higher in patients with delirium (mean ± SD, 33.2 ± 26.51 mmHgxh v 23.4 ± 16.13 mmHgxh; p ¼ 0.031) and positively correlated with the Delirium Rating Scale score on postoperative day 2 (r = 0.27, p = 0.011).
Conclusions
Summative presence of delirium was not associated with perioperative blood pressure excursions; but on secondary exploratory analysis, excursions above the optimal mean arterial pressure were associated with the incidence and severity of delirium on postoperative day 2.
Keywords: cerebral autoregulation, cardiopulmonary bypass, delirium, cardiac surgery, hemodynamics, perioperative care, cerebral blood flow
DELIRIUM IS AN acute and fluctuating state of confusion and disorientation, characterized by changes in attention, cognition, consciousness, and perception, affecting up to 25% to 50% of patients after cardiac surgery.1,2 This condition remains a serious healthcare burden, particularly due to its association with higher medical costs, increased morbidity, long-term cognitive deficits, and greater mortality.3,4 Progress in preventing postoperative delirium has been hindered by the lack of a full understanding of its pathophysiology. Proposed mechanisms include pre-existing brain inflammation exacerbated by surgery; induced immunologic perturbations; ischemic brain injury; hypoxia; and an imbalance of neurotransmitters, including cholinergic deficiency.5 Several risk factors have been identified for delirium, including older age, preexisting cognitive impairment, depression, history of stroke, atrial fibrillation, anemia, infection, preoperative treatment with beta-blockers, alcohol, benzodiazepines, and nicotine abuse.6–9
In prior studies, the authors showed that hemodynamic management during cardiopulmonary bypass (CPB) was a potentially modifiable risk factor for major complications of cardiac surgery. The authors have found that blood pressure excursions below the lower limit of cerebral blood flow (CBF) autoregulation were associated with major organ morbidity, including stroke, acute kidney injury, and mortality.10,11 More recently, the authors demonstrated that blood pressure management after cardiac surgery in the intensive care unit (ICU) was an important determinant of brain cellular injury.12 The authors further found that blood pressure excursions above the upper limit of CBF autoregulation during CPB were associated independently with clinically detected postoperative delirium.13 Many episodes of delirium, however, go undetected clinically without the performance of detailed delirium assessments using structured examinations and chart review.14 Thus, the relationship between perioperative blood pressure excursions below and above the limits of CBF autoregulation and the full spectrum of hyperactive, hypoactive, and mixed delirium is unknown.
Precise management of blood pressure during cardiac surgery and in the ICU based on autoregulation monitoring requires the availability of clinical monitors that provide an accurate and continuous measurement of CBF. The authors’ prior investigations have been based primarily on the measurement of CBF using transcranial Doppler, a technique associated with limitations including susceptibility to motion and electrical artifact and dependence on location of a transtemporal ultrasound insonating window. The authors recently demonstrated that CBF measured using a novel ultrasound-tagged near-infrared spectroscopy (UT-NIRS) technique compared favorably with that measured using transcranial Doppler for autoregulation monitoring.15 This method could provide a clinically reliable means for determining blood pressure targets both during and after surgery in the ICU.
The aim of this pilot study was to evaluate whether blood pressure excursions below and above the optimal mean arterial pressure (MAP) measured by CBF autoregulation monitoring using new noninvasive UT-NIRS technology were associated with frequency of delirium defined by the consensus panel in the early postoperative period (postoperative days 1–3). The secondary aim of the study was to determine whether the severity or types of delirium were associated with perioperative blood pressure management.
METHODS
From July 2013 to June 2015, 110 patients undergoing cardiac surgery with CPB were enrolled in a prospective, observational study (clinical trial registration number NCT02084394). The study was approved by the Institutional Review Board of The Johns Hopkins Medical Institutions, and all patients provided written, informed consent before participation.
Patient Care
General anesthesia was induced with midazolam, fentanyl, and isoflurane; vecuronium was used for muscle relaxation. A catheter placed in the radial artery was used for continuous monitoring of arterial blood pressure. Nonpulsatile CPB was performed with a target flow between 2.0 and 2.4 L/min/m2. Arterial blood gases were measured 10 minutes after initiation of CPB, and then hourly. Normocarbia was maintained by adjusting CPB gas flow based on continuous in-line blood gas monitoring, and pH was adjusted using α-stat pH management. In the ICU, the blood pressure was recorded continuously via a catheter placed in the radial artery. Blood gases were measured as needed, and normocarbia and oxygenation were adjusted. Fentanyl (50–100 μg) was given intravenously as needed for pain control after surgery, and propofol was used until extubation.
Monitoring of CBF Autoregulation
UT-NIRS monitoring was performed using a CerOx monitor (Ornim, Kfar Saba, Israel) during CPB and for the first 3 hours after admission to the ICU.16,17 UT-NIRS methodology recently has been described for the noninvasive measurement of microcirculatory blood flow in a small volume of superficial gray matter (1 cm3), using sensors attached to the forehead.16 This approach is based on the acoustic-optic effect whereby focused, low-power ultrasound is used to modulate light in the near-infrared spectrum in tissue.16,17 The ultrasound-tagged photons that travel through the region of interest in the tissue undergo a Doppler effect that is filtered and measured at the skin surface. Analog arterial pressure data from the operating room hemodynamic monitor and CerOx signals were sampled with an analog-to-digital converter at 60 Hz and then processed with ICM+ software version 6.1 (University of Cambridge, Cambridge, UK) as previously described.18,19 To limit the analysis to the frequency of slow vasogenic waves (0.05–0.003 Hz), relevant to cerebral autoregulation, the signals were time-integrated as nonoverlapping 10-second mean values, which is equivalent to applying a moving average filter with a 10-second time window and resampling at 0.1 Hz. The latter was performed to eliminate high-frequency noise from the respiratory and pulse frequencies, while allowing for detection of oscillations and transients that occur below 0.05 Hz.18,19 The signals were further high-pass filtered with a direct current cut-off set at 0.003 Hz to remove slow drifts associated with hemodilution at the onset of bypass, blood transfusions, cooling, and rewarming. A continuous moving Pearson’s correlation coefficient was calculated between the changes in MAP and CerOx data, generating the variable correlation flow index (CFx).15 Consecutive paired 10-second averaged values from 300 seconds’ duration were used for each calculation, incorporating 30 data points for each index.18,19 CFx approaches zero or is negative when cerebral autoregulation is functional, whereas the CFx value approaches 1 when reaching limits of cerebral autoregulation.
Patient Outcomes
Delirium Assessment
Delirium was assessed using rigorous methodology during the postoperative period. The Confusion Assessment Method (CAM) was used for all nonintubated patients.20 For patients who still were intubated, the CAM-ICU was used.21 The assessment was performed by trained research assistants. This assessment included a structured cognitive examination, which consisted of a patient interview, the MMSE, Digit Span Forwards and Reverse, and timed Months of Year backwards. Research assistants also queried nurses, family members or friends of the patients, and the medical record for evidence of delirium over the 24-hour period (confusion, agitation, hallucinations, delusions, inattention, and motor retardation). This information was used to determine the CAM rating for a delirium diagnosis, and the Delirium Rating Scale-Revised-98 (DRS-R-98) was used to evaluate delirium severity.22 A diagnosis of delirium was performed by a consensus panel following Diagnostic and Statistical Manual of Mental Disorders-IV-TR criteria.20 The consensus panel included a psychiatrist, anesthesiologist, and research assistants who were completely blinded from the results of cerebral autoregulation monitoring. Multiple measures were taken to ensure quality assurance. The research assistants underwent a formal training protocol with a psychiatrist that included group delirium assessments of at least 10 patients, with co-rating and discussion. In addition, trained delirium assessors and the psychiatrist conducted co-ratings of patients in the study approximately once every 2 weeks to ensure consistency. Delirium was assessed on each postoperative day 1 to 3. Patients who experienced delirium on any of these day were considered as having postoperative delirium.
Data Analysis
The normality of the distribution of the data was assessed using the Kolmogorov-Smirnov test. Continuous variables were analyzed using Student’s t-test for data that were normally distributed. Continuous data that remained non-normally distributed after logarithmic transformation were analyzed using the Mann-Whitney test. Categorical variables were analyzed using Fisher’s exact test, and test for correlation was performed using Pearson’s correlation or Spearman’s correlation if data were not normally distributed.
The DRS-R-98 score was used as a continuous variable to assess severity of delirium. To determine optimal MAP during CPB and in the ICU, the CFx was categorized and averaged in 5 mmHg MAP bins for each patient.18 Optimal MAP was defined as the MAP in which CFx was lowest, which indicated MAP in which changes in blood pressure were least correlated with changes in cerebral blood flow12,15 (Fig 1). The right- and left-sided optimal MAP values were averaged to define the individual optimal MAP. Blood pressure excursions below (area under the curve [AUC] < OptMAP) and above (AUC > OptMAP) the optimal MAP (mmHgxh) were calculated as the sum of the product of the difference in MAP from the optimal MAP and the time spent at each MAP. The sum of the blood pressure excursions below or above the optimal MAP during CPB and the first 3 hours in the ICU was used for the analysis. For the primary outcome, AUC < OptMAP and AUC > OptMAP were assessed for their association with the presence of summative delirium, defined by the consensus panel on postoperative days 1 through 3. Exploratory analysis was performed to assess for the association between perioperative blood pressure and delirium for each postoperative day with analysis of variance for multiple testing. To examine the effect of blood pressure management on the severity of delirium, AUC > OptMAP was assessed for the association with DRS-R-98 assessments on postoperative days 1 to 3; p values < 0.05 were considered statistically significant. All analyses were performed using Stata (Version 13.1; Stata Corp, College Station, TX).
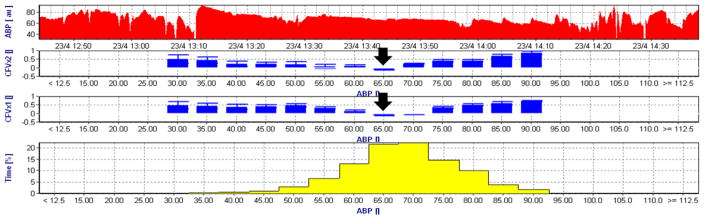
Fig 1.
Representative cerebral autoregulation monitoring graphic results obtained during cardiopulmonary bypass. The top graph shows the arterial blood pressure (ABP) trend during the monitoring period. The next 2 graphs represent the correlation flow index (CFx) from the left and right brain hemispheres averaged in 5 mmHg bins. The last graph shows the percentage of time for each 5 mmHg mean arterial pressure (MAP) bins during the recording period. The CFx represents a moving Pearson’s correlation coefficient between slow-wave changes in cerebral flow index and MAP. When cerebral blood flow is in the autoregulation range, CFx is close to zero, but when MAP is below or above the autoregulation range, CFx approaches 1. Optimal blood pressure, which is a blood pressure associated with the most robust autoregulation, is 65 mmHg for this patient, indicated by ABP with the lowest CFx (black arrows).
RESULTS
Of 110 patients who were enrolled in this study, 7 patients were excluded from the analysis due to being comatose during the first 3 postoperative days, and 4 other patients were excluded from the analysis due to refusal of the postoperative assessments. Of the 7 comatose patients, 2 patients had experienced documented stroke. One of them recovered and was discharged with residual disability, whereas the other patient died from multiorgan failure. Two other patients died due to cardiogenic shock and multiorgan failure, and 3 other patients remained intubated until postoperative day 5 due to difficulty in weaning from the ventilator or remained sedated per open chest protocol. These 3 patients were discharged neurologically intact.
Demographic data for the patients with completed delirium assessments are listed in Table 1. The mean age of the patients was 65 ± 8.8 years, and the duration of CPB was 129 ± 64.2 minutes. Forty-seven patients (47.5%) developed delirium on one of the 3 days after surgery. Patients with a history of tobacco smoking (61.7% v 36.5%; p = 0.016) and usage of a calcium channel blocker (34.0% v 13.5%; p = 0.018) were more likely to experience delirium after surgery. In addition, patients with peripheral vascular disease (12.8% v 1.9%; p = 0.051) and patients taking statins (68.1% v 48.1%; p = 0.06) demonstrated a tendency to develop delirium after surgery. Thirty-two patients experienced delirium on postoperative day 1. Of these patients, delirium was classified as hypoactive in 14 (43.8%), hyperactive in 1 (3.1%), and mixed in 13 (40.6%). The delirium experienced by 4 (12.5%) patients was unable to be classified. Thirty patients experienced delirium on postoperative day 2. In 14 patients (46.7%) the delirium was hypoactive, in 1 (3.3%) was hyperactive, and in 14 (46.7%) it was mixed; the delirium of 1 patient (3.3%) could not be classified. On postoperative day 3, 23 patients presented with delirium. Of these, the delirium in 12 patients (52.2%) was hypoactive, in 1 it was hyperactive (4.4%), and in 10 it was mixed (43.5%). The results of delirium assessments are listed in Table 2. CAM-ICU was only used on postoperative day 1 in 3 patients. CAM-ICU results were positive in 1 patient and negative in 2 patients.
Table 1.
Demographic and Operative Characteristics of the Entire Cohort of the Study Participants With and Without Delirium
| Entire | Delirium (−) | Delirium (+) | p Value | |
|---|---|---|---|---|
|
| ||||
| n = 99 | n = 52 | n = 47 | ||
| Age* | 65 ± 8.8 | 64 ± 9.0 | 66 ± 9.2 | 0.22 |
| Male (%) | 61 (61.6%) | 31 (59.6%) | 30 (63.9%) | 0.69 |
| Baseline estimated glomerular filtration rate (mL × min1 × 1.73 m2)* | 69.1 ± 19.8 | 73.7 ± 16.1 | 68.7 ± 19.4 | 0.16 |
| Chronic obstructive pulmonary disease (%) | 11 (11.1%) | 6 (11.5%) | 5 (10.6%) | 1 |
| Hypertension (%) | 69 (69.7%) | 34 (65.4%) | 35 (74.5%) | 0.38 |
| Diabetes (%) | 26 (26.3%) | 9 (17.3%) | 17 (36.2%) | 0.041 |
| History of tobacco use (%) | 48 (48.5%) | 19 (36.5%) | 29 (61.7%) | 0.016 |
| Chronic heart failure (%) | 13 (13.1%) | 5 (9.6%) | 8 (17.0%) | 0.37 |
| Aspirin (%) | 68 (68.7%) | 35 (67.3%) | 33 (70.2%) | 0.83 |
| Angiotensin-converting enzyme inhibitors-I (%) | 5 (5.1%) | 5 (9.6%) | 0 (0.0%) | 0.06 |
| Angiotensin II receptor blocker (%) | 11 (11.1%) | 6 (11.5%) | 5 (10.6%) | 1 |
| Calcium channel blocker (%) | 23 (23.2%) | 7 (13.5%) | 16 (34.0%) | 0.018 |
| Beta-adrenergic receptor blocker (%) | 54 (54.5%) | 26 (50.0%) | 28 (59.6%) | 0.42 |
| Statin (%)† | 57 (57.6%) | 25 (48.1%) | 32 (68.1%) | 0.06 |
| Diuretics (%) | 32 (32.3%) | 14 (26.9%) | 18 (38.3%) | 0.28 |
| Antidepressant (%) | 18 (18.2%) | 7 (13.5%) | 11 (23.4%) | 0.3 |
| Peripheral vascular disease (%) | 7 (7.1%) | 1 (1.9%) | 6 (12.8%) | 0.051 |
| Prior cerebral vascular accident (%) | 5 (5.1%) | 4 (7.7%) | 1 (2.1%) | 0.37 |
| Prior TIA (%) | 2 (2.0%) | 1 (1.9%) | 1 (2.1%) | 1 |
| Surgical procedure | 0.1 | |||
| CABG (%) | 50 (50.5%) | 22 (42.3%) | 28 (59.6%) | |
| CABG + AVR (%) | 11 (11.1%) | 5 (9.6%) | 6 (12.8%) | |
| AVR/MVR (%) | 32 (32.3%) | 22 (42.3%) | 10 (21.2%) | |
| Aortic root (%) | 4 (4.1%) | 1 (1.9%) | 3 (6.4%) | |
| Others (%) | 2 (2.0%) | 2 (3.9%) | 0 | |
| Duration of cardiopulmonary bypass (min)* | 129 ± 64.2 | 119 ± 46.7 | 125 ± 46.9 | 0.59 |
| Total cross-clamp time (min)* | 81 ± 29.0 | 76 ± 29.8 | 85 ± 26.9 | 0.16 |
NOTE. The listed p values are for comparisons between patients with and without delirium.
Abbreviations: TIA, transient ischemic attack; CABG, coronary artery bypass graft; AVR, aortic valve replacement; MVR, mitral valve replacement or repair.
Data are listed as mean ± standard deviation for continuous variables that were normally distributed.
Statin, HMG-CoA inhibitor.
Table 2.
Results of Delirium Assessments on Postoperative Days 1 to 3
| CAM/CAM-ICU | MMSE | DRS-R-98 | |
|---|---|---|---|
| POD1 | 28 (28.3%) | 28 (26–29) | 4 (2.0–6.3) |
| POD2 | 25 (27.5%) | 28 (26–30) | 3 (2.0–6.8) |
| POD3 | 19 (20.7%) | 29 (27–30) | 3 (1.0–5.0) |
NOTE. Data are listed as n (%) for categorical variables and median (interquartile range) for continuous variables that were non-normally distributed. CAM-ICU only was used on postoperative day 1 in 3 patients.
Abbreviations: CAM, confusion assessment method; ICU, intensive care unit; MMSE, Mini Mental State Examination; DRS-R-98, Delirium Rating Scale-Revised-98.
Physiologic data during CPB and for the first 3 hours in the ICU are listed for patients with and without delirium in Table 3. The CFx in the ICU was significantly higher in patients with delirium (0.14 ± 0.08 v 0.09 ± 0.12, p = 0.038), but there were no differences in other listed data between patients with and without delirium. There were no significant differences in CFx both before (0.27 ± 0.16 v 0.29 ± 0.16, p = 0.75) and after CPB (0.25 ± 0.16 v 0.29 ± 0.16, p = 0.19) between patients with and without delirium. Blood pressure excursions below (AUC < OptMAP) and above (AUC > OptMAP) the optimal MAP defined by cerebral autoregulation monitoring for patients with and without delirium are listed in Table 4. There were no significant differences in AUC > OptMAP or AUC < OptMAP between patients with and without summative presence of delirium from postoperative days 1 through 3. However, exploratory analysis on each postoperative day revealed that AUC > OptMAP was significantly higher in patients with delirium on postoperative day 2.
Table 3.
Physiologic Data During Cardiopulmonary Bypass and the First 3 Hours in the Intensive Care Unit for the Entire Cohort of Patients With and Without Delirium
| No Delirium | Delirium | p Value | ||
|---|---|---|---|---|
|
| ||||
| n = 52 | n = 47 | |||
| CPB | MAP (mmHg) | 71 ± 7.3 | 70 ± 7.3 | 0.4 |
| CFx | 0.34 ± 0.19 | 0.34 ± 0.16 | 0.93 | |
| Optimal MAP (mmHg) | 70 ± 8.4 | 70 ± 10.7 | 0.96 | |
| Hb (g/dL) | 9.4 ± 1.1 | 9.3 ± 1.3 | 0.46 | |
| pH | 7.39 ± 0.03 | 7.38 ± 0.03 | 0.48 | |
| PO2 (mmHg) | 249 ± 45.6 | 251 ± 27.4 | 0.8 | |
| PCO2 (mmHg) | 41.1 ± 2.0 | 41.1 ± 1.8 | 0.96 | |
| ICU | MAP (mmHg) | 75 ± 8.5 | 77 ± 8.6 | 0.36 |
| CFx | 0.09 ± 0.12 | 0.14 ± 0.08 | 0.038 | |
| Optimal MAP (mmHg) | 75 ± 6.6 | 76 ± 10.4 | 0.45 | |
| Hb (g/dL) | 10.7 ± 1.3 | 10.4 ± 1.3 | 0.21 | |
| pH | 7.35 ± 0.04 | 7.35 ± 0.05 | 0.81 | |
| PO2 (mmHg) | 128 ± 31.9 | 122 ± 43.3 | 0.41 | |
| PCO2 (mmHg) | 39 ± 5.0 | 39 ± 3.8 | 0.78 | |
NOTE. The listed p values are for comparisons between patients with and without delirium. Cerebral flow index (CFx) is the Pearson correlation constant between cerebral blood flow index and mean arterial pressure averaged for the respective perioperative periods. Data are listed as mean ± SD.
Abbreviations: CPB, cardiopulmonary bypass; MAP, mean arterial pressure; Hb, hemoglobin; ICU, intensive care unit.
Table 4.
Blood Pressure Excursions Below and Above Optimal Blood Pressure During Perioperative Period (CPB + ICU) Determined by Cerebral Blood Flow Autoregulation Monitoring Among Patients Who Developed or Did Not Develop Delirium
| Delirium (−) | Delirium (+) | p Value | |
|---|---|---|---|
| AUC >optimal MAP (mmHgxh) | |||
| Overall | 24.0 ± 15.85 | 27.5 ± 24.64 | 0.40 |
| POD 1 | 23.9 ± 18.98 | 31.0 ± 22.78 | 0.12 |
| POD 2 | 23.4 ± 16.13 | 33.2 ± 26.51 | 0.031 |
| POD 3 | 23.8 ± 17.07 | 26.1 ± 19.91 | 0.59 |
| AUC <optimal MAP (mmHgxh) | |||
| Overall | 21.9 ± 18.81 | 23.4 ± 20.32 | 0.70 |
| POD 1 | 22.2 ± 18.24 | 19.6 ± 16.66 | 0.50 |
| POD 2 | 21.3 ± 17.72 | 19.4 ± 14.57 | 0.61 |
| POD 3 | 21.6 ± 18.29 | 22.7 ± 19.57 | 0.82 |
NOTE. Data are listed as mean ± SD. Analysis of variance was used to test for the statistical significance.
Abbreviations: MAP, mean arterial pressure; POD, postoperative day.
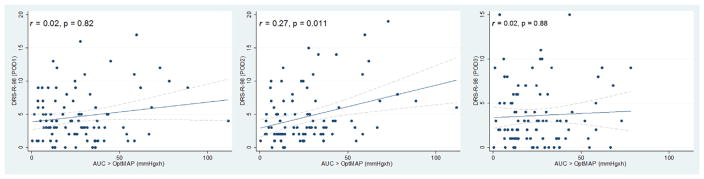
To examine whether blood pressure management during the early perioperative period had any effect on the severity of delirium, AUC > OptMAP and AUC < OptMAP were assessed for the association with DRS-R-98 on each postoperative day. Blood pressure excursions above the optimal MAP (AUC > OptMAP) was correlated positively with DRSR-98 scores on postoperative day 2 (r = 0.27, p = 0.011) but not on postoperative days 1 and 3 (Fig 2).
Fig 2.
Scatter plot of blood pressure excursions above optimal mean arterial pressure (MAP) and Delirium Rating Scale-Revised-98 (DRS-R- 98) from postoperative days 1 through 3. Demonstration of correlation between the severity of delirium determined using the DRS-R-98 test from postoperative day 1, day 2, and day 3 with the product of the magnitude and duration that blood pressure was above optimal MAP determined with cerebral autoregulation monitoring (AUC > OptMAP). There was a correlation between severity of delirium measured using the DRS-R-98 test and AUC > OptMAP on postoperative day 2.
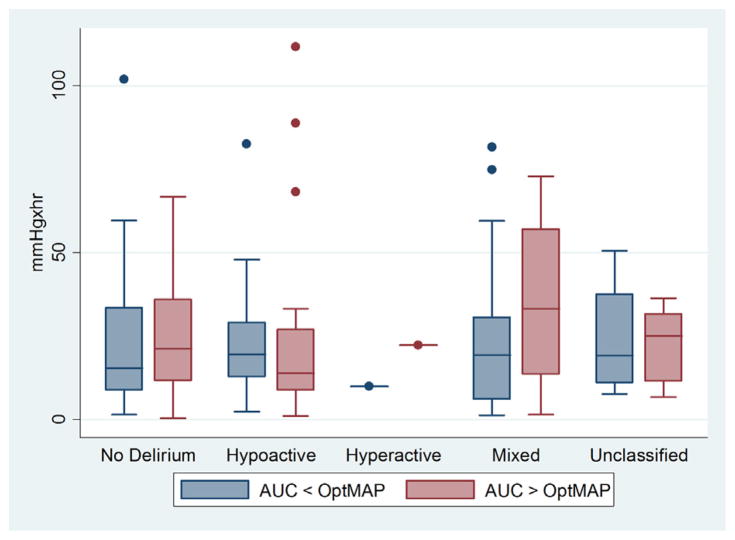
Figure 3 shows AUC > OptMAP and AUC < OptMAP for the subtypes of delirium. There were no significant differences in blood pressure excursions beyond optimal MAP among different subtypes of delirium.
Fig 3.
Box and whisker plot comparing the product of the magnitude and duration that blood pressure was above (AUC > OptMAP) and below (AUC < OptMAP) the optimal MAP determined with subtypes of delirium. There were no differences in AUC > OptMAP and AUC < OptMAP among the subtypes of delirium. The horizontal line in the shaded box represents the median value, and the shaded box represents the interquartile range. The error bars below and above the shaded area represent ±1.5× the interquartile range; points beyond the error bar are outliers.
DISCUSSION
The results of this study showed that blood pressure excursions during CPB and in the ICU after surgery above and below the optimal MAP measured using cerebral autoregulation monitoring were not associated with summative presence of delirium on postoperative days 1 through 3. However, blood pressure excursions above the optimal MAP were associated with delirium on postoperative day 2 and also were correlated positively with severity of delirium assessed using the DRS-R-98 test on postoperative day 2. There were no significant differences in blood pressure excursions below and above the optimal MAP among the delirium subtypes.
In previous investigations the authors found that blood pressure excursions during CPB below the cerebral autoregulation range were associated with acute kidney injury and major morbidity and mortality.10,11 The authors also recently reported that blood pressure below optimal CBF autoregulation levels after cardiac surgery in the ICU were associated with evidence of cerebral injury measured using the sensitive brain injury biomarker glial fibrillary acid protein.12 In contrast to low blood pressure, the authors have found that the magnitude and duration that blood pressure is above the upper limit of CBF autoregulation during CPB were associated with postoperative delirium.13 Cerebral hyperperfusion is observed in other clinical conditions, including after carotid endarterectomy, in which cerebral hyperperfusion is associated with cerebral edema, delirium, and intracerebral hemorrhage.23–25 Increased blood pressure under conditions of impaired autoregulation increases CBF, leading to transudation of fluid into the pericapillary astrocytes and interstitium of the brain.25 This results in vasogenic white matter edema, especially in the vertebrobasilar circulation territory of the posterior parietal and occipital regions.25 Cerebral hyperperfusion due to impaired autoregulation is suggested to be the mechanism for delirium occurring in nonsurgical patients with acute hypertensive emergencies.26
In this study, optimal MAP was used rather than the lower or upper limit of cerebral autoregulation, which are defined by using admittedly arbitrary cut-offs. Cerebral vasoreactivity is not dichotomous, but rather continuous and graded. Targeting MAP to a blood pressure associated with the most robust autoregulation, defined as optimal MAP, is more relevant clinically. In the authors’ prior study, optimal MAP was used to define hypotension. In that study, postoperative blood pressure management below the optimal MAP was associated with increase in glial fibrillary acid protein, indicating brain cellular injury.12 Furthermore, defining limits of autoregulation is sometimes difficult in situations in which blood pressure variations are small while the lowest CFx may be readily apparent.15, 27
Secondary exploratory analysis showed a significant difference in blood pressure excursions above optimal CBF, with the incidence of delirium defined by the consensus panel on postoperative day 2, which also was correlated positively with severity of delirium assessed using the DRS-R-98. In the authors’ prior findings, linking blood pressure above optimal CBF autoregulation during CPB with delirium, delirium was defined based on the presence of confusion, agitation, or any change in mental status—all identified by clinical staff. The lack of a standard patient interview by a psychiatrist or clinically trained researcher in the assessment for delirium in that study may have under-recognized hypoactive forms of delirium.13 Thus, the findings presented in this study further overcame a limitation of the authors’ prior investigations by performing detailed, standardized delirium assessments by trained researchers.
Delirium consists of several pyschomotor subtypes, divided into hypoactive, hyperactive, and mixed types.28 The hypoactive subtype is characterized by patients being quiet but and disinterested with decreased motion. On the other hand, patients with the hyperactive type present with agitation. The main characteristic of delirium is inattention, and motor subtypes have comparable disturbances of key diagnostic features such as cognitive and thought process abnormalities. Among these subtypes, the mixed subtype is the most phenomenologically intense, but hypoactive subtypes have the poorest prognosis.29 Differences in the presentation of symptoms may suggest different pathologic mechanisms in the development of delirium. However, this study demonstrated that there were no significant differences in AUC > OptMAP and AUC < OptMAP among the delirium subtypes.
Several limitations should be considered in interpreting these results. The sample size of this pilot study likely was too small to exclude blood pressure excursions above the optimal blood pressure as being associated with delirium. Furthermore, delirium assessments were limited to the first 3 days after surgery. The primary hypothesis that blood pressure excursions outside the limit of cerebral autoregulation during CPB and the first 3 hours in the ICU, in which major fluctuations in blood pressure are most likely to occur, focused the assessment to early postoperative periods. The result indicating that cerebral hyperperfusion was associated with postoperative delirium may suggest a similar pathophysiology that is observed in cerebral hyperperfusion syndrome, which becomes apparent within the first 5 days after carotid endartectomy. 24 These observations may suggest future studies to observe the effect of blood pressure outside the limit of cerebral autoregulation for a longer time span. This study did not adjust for the perioperative analgesic and sedative drug usage. The effect of sedatives, especially benzodiazepines, have been well-documented to be associated with delirium in critically ill patients.9 The patients in this study received midazolam only during surgery and not after surgery. However, the possible effect of midazolam on influencing the delirium findings must be considered.
In conclusion, summative presence of delirium (postoperative days 1 through 3) was not associated with perioperative blood pressure excursions, but on secondary exploratory analysis excursions above the optimal MAP were associated with incidence and severity of delirium on postoperative day 2. Blood pressure management in the early perioperative period might have an effect on the development of delirium; however, further studies are needed to confirm the effect of blood pressure management on the incidence of delirium.
References
- 1.Whitlock EL, Torres BA, Lin N, et al. Postoperative delirium in a substudy of cardiothoracic surgical patients in the BAG-RECALL clinical trial. Anesth Analg. 2014;118:809–817. doi: 10.1213/ANE.0000000000000028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martin BJ, Arora RC. Delirium and cardiac surgery: Progress - and more questions. Crit Care. 2013;17:140. doi: 10.1186/cc12610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 4.Jackson JC, Gordon SM, Hart RP, et al. The association between delirium and cognitive decline: A review of the empirical literature. Neuropsychol Rev. 2004;14:87–98. doi: 10.1023/b:nerv.0000028080.39602.17. [DOI] [PubMed] [Google Scholar]
- 5.Trabold B, Metterlein T. Postoperative delirium: Risk factors, prevention, and treatment. J Cardiothorac Vasc Anesth. 2014;28:1352–1360. doi: 10.1053/j.jvca.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 6.Koster S, Hensens AG, Schuurmans MJ, et al. Risk factors of delirium after cardiac surgery: A systematic review. Eur J Cardiovasc Nurs. 2011;10:197–204. doi: 10.1016/j.ejcnurse.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 7.Tully PJ, Baker RA, Winefield HR, et al. Depression, anxiety disorders and Type D personality as risk factors for delirium after cardiac surgery. Aus N Z J Psychiatry. 2010;44:1005–1011. doi: 10.3109/00048674.2010.495053. [DOI] [PubMed] [Google Scholar]
- 8.Katznelson R, Djaiani G, Mitsakakis N, et al. Delirium following vascular surgery: Increased incidence with preoperative beta-blocker administration. Can J Anaesth. 2009;56:793–801. doi: 10.1007/s12630-009-9148-0. [DOI] [PubMed] [Google Scholar]
- 9.Zaal IJ, Devlin JW, Hazelbag M, et al. Benzodiazepine-associated delirium in critically ill adults. Intensive Care Med. 2015;41:2130–2137. doi: 10.1007/s00134-015-4063-z. [DOI] [PubMed] [Google Scholar]
- 10.Ono M, Brady K, Easley RB, et al. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J Thorac Cardiovasc Surg. 2014;147:483–489. doi: 10.1016/j.jtcvs.2013.07.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ono M, Arnaoutakis GJ, Fine DM, et al. Blood pressure excursions below the cerebral autoregulation threshold during cardiac surgery are associated with acute kidney injury. Crit Care Med. 2013;41:464–471. doi: 10.1097/CCM.0b013e31826ab3a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hori D, Ono M, Rappold TE, et al. Hypotension after cardiac operations based on autoregulation monitoring leads to brain cellular injury. Ann Thorac Surg. 2015;100:487–493. doi: 10.1016/j.athoracsur.2015.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hori D, Brown C, Ono M, et al. Arterial pressure above the upper cerebral autoregulation limit during cardiopulmonary bypass is associated with postoperative delirium. Br J Anaesth. 2014;113:1009–1017. doi: 10.1093/bja/aeu319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Inouye SK, Foreman MD, Mion LC, et al. Nurses’ recognition of delirium and its symptoms: Comparison of nurse and researcher ratings. Arch Intern Med. 2001;161:2467–2473. doi: 10.1001/archinte.161.20.2467. [DOI] [PubMed] [Google Scholar]
- 15.Hori D, Hogue CW, Jr, Shah A, et al. Cerebral autoregulation monitoring with ultrasound-tagged near-infrared spectroscopy in cardiac surgery patients. Anesth Analg. 2015;121:1187–1193. doi: 10.1213/ANE.0000000000000930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schytz HW, Guo S, Jensen LT, et al. A new technology for detecting cerebral blood flow: A comparative study of ultrasound tagged NIRS and 133Xe-SPECT. Neurocrit Care. 2012;17:139–145. doi: 10.1007/s12028-012-9720-2. [DOI] [PubMed] [Google Scholar]
- 17.Ron A, Raceheli N, Breskin I, et al. Measuring tissue blood flow using ultrasound modulated diffused light. Proc SPIE 8223, Photons Plus Ultrasound: Imaging and Sensing 82232J. 2012 [Google Scholar]
- 18.Brady K, Joshi B, Zweifel C, et al. Real-time continuous monitoring of cerebral blood flow autoregulation using near-infrared spectroscopy in patients undergoing cardiopulmonary bypass. Stroke. 2010;41:1951–1956. doi: 10.1161/STROKEAHA.109.575159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brady KM, Mytar JO, Lee JK, et al. Monitoring cerebral blood flow pressure autoregulation in pediatric patients during cardiac surgery. Stroke. 2010;41:1957–1962. doi: 10.1161/STROKEAHA.109.575167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adamis D, Rooney S, Meagher D, et al. A comparison of delirium diagnosis in elderly medical inpatients using the CAM, DRS-R98, DSM-IV and DSM-5 criteria. Int Psychogeriatr. 2015;27:883–889. doi: 10.1017/S1041610214002853. [DOI] [PubMed] [Google Scholar]
- 21.Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–1379. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Trzepacz PT, Mittal D, Torres R, et al. Validation of the Delirium Rating Scale-revised-98: Comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci. 2001;13:229–242. doi: 10.1176/jnp.13.2.229. [DOI] [PubMed] [Google Scholar]
- 23.Moulakakis KG, Mylonas SN, Sfyroeras GS, et al. Hyperperfusion syndrome after carotid revascularization. J Vasc Surg. 2009;49:1060–1068. doi: 10.1016/j.jvs.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 24.van Mook WN, Rennenberg RJ, Schurink GW, et al. Cerebral hyperperfusion syndrome. Lancet Neurol. 2005;4:877–888. doi: 10.1016/S1474-4422(05)70251-9. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz RB. Hyperperfusion encephalopathies: Hypertensive encephalopathy and related conditions. Neurologist. 2002;8:22–34. doi: 10.1097/00127893-200201000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Aggarwal M, Khan IA. Hypertensive crisis: Hypertensive emergencies and urgencies. Cardiology Clin. 2006;24:135–146. doi: 10.1016/j.ccl.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Ono M, Joshi B, Brady K, et al. Risks for impaired cerebral autoregulation during cardiopulmonary bypass and postoperative stroke. Br J Anaesth. 2012;109:391–398. doi: 10.1093/bja/aes148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leonard MM, Agar M, Spiller JA, et al. Delirium diagnostic and classification challenges in palliative care: Subsyndromal delirium, comorbid delirium-dementia, and psychomotor subtypes. J Pain Symptom Manage. 2014;48:199–214. doi: 10.1016/j.jpainsymman.2014.03.012. [DOI] [PubMed] [Google Scholar]
- 29.Meagher DJ, Leonard M, Donnelly S, et al. A longitudinal study of motor subtypes in delirium: Relationship with other phenomenology, etiology, medication exposure and prognosis. J Psychosomatic Res. 2011;71:395–403. doi: 10.1016/j.jpsychores.2011.06.001. [DOI] [PubMed] [Google Scholar]