Abstract
Objectives. To investigate the validity of the apparent downward trend in the national case–fatality rate for gunshot wounds from assault.
Methods. We reanalyzed the estimated annual number of nonfatal firearm injuries the National Electronic Injury Surveillance System reported from 2003 to 2012. We adjusted the estimates for discontinuities created by the substitution of 1 hospital for another in the sample and for a downward trend in the percentage of gunshot injuries classified as “unknown circumstance.” Firearm homicide data are from the Centers for Disease Control and Prevention, Web-based Injury Statistics Query and Reporting System.
Results. The unadjusted National Electronic Injury Surveillance System estimate increased by 49%, yielding a decline in the case–fatality rate from 25% to 18%. Our adjustments eliminated these trends; the case–fatality rate was 22% in both 2003 and 2012.
Conclusions. With reasonable adjustments, the trend in nonfatal injuries from interpersonal firearms assault tracks the flat trend in firearms homicides, suggesting that there was no increase in firearms violence during this period. The case–fatality rate did not change, and trauma care improvements did not influence the firearms homicide trend.
Recent reports in the peer-reviewed literature and lay press1–3 have suggested what would be a very positive development: improvements in the survivability of assault-related gunshot wounds, as reflected by a decline in the case–fatality rate for firearm assault. These reports have relied on mortality data from the National Center for Health Statistics and nonfatal injury data from the National Electronic Injury Surveillance System (NEISS)-All Injury Program (AIP). The authors of these reports attribute the good news to improvements in emergency medical services and clinical care for severely injured patients.
But published analyses of other aggregated clinical data show that the case–fatality rate for firearm-related injuries has remained stable or increased in recent years.4–6 We assessed the validity of the reported estimates that the case–fatality rate for firearm-related assaults is decreasing. Our investigation focused on the NEISS.
METHODS
NEISS is a stratified probability sample of US hospitals that have more than 6 beds and provide 24-hour emergency care. Through an interagency agreement between the Consumer Product Safety Commission and the Centers for Disease Control and Prevention (CDC), information regarding all patients with gun-related injuries treated in NEISS hospital emergency departments (EDs) has been collected since June 1992.7
NEISS data are used to produce 2 sets of national estimates of the annual number of firearm gunshot injuries. The first is on the basis of a subsample of hospitals utilized in the NEISS-AIP. The CDC reports those estimates in their Web-based Injury Statistics Query and Reporting System.8 The second is on the basis of the complete sample, and results are available as the NEISS Firearms Injury Surveillance Study (FISS).8 We used FISS data for the decade 2003 to 2012. (At the time of this writing, 2012 was the most recent year available.) Besides the larger sample size, the FISS data provide a more detailed coding of circumstances than does the AIP.
Sample and Weights
The NEISS-FISS data are from a stratified sample of geographically defined primary sampling units (PSUs), with 4 strata on the basis of hospital size (as operationalized by the number of annual ED visits) and 1 children’s hospital stratum.9 We included at least 91 PSUs in each of the years under consideration. Further information about the sampling strategy used in NEISS-FISS is available in a CDC-issued codebook.10 NEISS employs sample weights to produce national estimates of the number of gunshot cases.
Each sample weight represents the inverse of the probability of the selection of the case. The average weight for assault cases in 2012 was 24.9 (53 293/2137). The sample weights are computed monthly and are adjusted for nonresponse; if an ED in the sample fails to report, other EDs in the same stratum are up-weighted for that month.11
Classification of Cases
Gunshot cases are included in NEISS-FISS if they are “nonfatal”; that is, the ED discharge code indicates that they are alive at the point of discharge. (It is relatively rare for a gunshot death to occur following discharge from the ED. Most deaths occur at the scene, during transport to the hospital, or in the ED.)12 Each case included in NEISS-FISS is coded for the intent of the shooting. The intent categories include assault, self-harm, unintentional, and legal intervention (caused by police or other legal authorities, including security guards). NEISS hospital coders work from medical-provider recorded information in the patient’s medical chart.
Each intent code is understood to be “confirmed or suspected.” “Unknown circumstance” is available as a distinct code and reported in FISS. (Conversely, unknown circumstances are merged with “unintentional” shootings in AIP.) Coders differ in the use of intent codes, and indeed, in some reporting hospitals and years all the gunshot cases were coded as “unintentional” or “unknown circumstance.” We do not know the source of these disparities in coding practice.
Statistical Analysis
We conducted the statistical analysis using Excel 2013 (Microsoft, Redmond, WA). The goal of the statistical analysis is to explore the possibility that the strong trend in firearm injuries from assaults and the corresponding trend in the assault case–fatality rate are artifacts of technical problems with the NEISS-FISS data series. Consumer Product Safety Commission staff provided the PSU-level raw data in personal communication. We found 2 possible problems. The first was that in several instances hospitals that withdrew from the sample were replaced with hospitals that had far more gunshot cases, including assault cases. The second was a strong downward trend in the number of cases classified as “unknown circumstance,” suggesting that cases that would have been identified as “unknown” in 2003 were assigned to one of the substantive categories (including “assault”) in 2012.
Our statistical analysis adjusted for both the “replacement” problem and the “unknown circumstance” problem. The adjustment for the replacement problem was confined to the instances in which NEISS replaced a sample hospital with another hospital in the same PSU. The adjustment for the replacement problem was simply to replace the firearm assault gunshot injury count from the new hospital with the count observed in the last complete year the original hospital was included in the sample. That substitution serves to adjust for the observed tendency (during the decade under consideration) for the substitute hospitals to report far more gunshot cases than did the original hospitals. This adjustment strategy reflects a reasonable expectation that there would typically be little year-to-year change in the number of gunshot cases in a PSU.
The adjustment for the declining number of “unknowns” in the national sample is to distribute all cases classified as “unknown” in proportion to the number of cases assigned to each of the other circumstances in each year nationwide. For example, if 40% of the nonfatal cases with known circumstance were classified as “assault,” we added 40% of the cases classified as “unknown” to the number of assaults. This adjustment is valid assuming that the true distribution of the “unknowns” is the same as the distribution of known intents in each year.
It is important to note that these adjustments do not serve to establish the true trend in assault firearms injuries or in the case–fatality rate. Rather they establish that the observed trends are heavily biased by evident problems with the NEISS time series.
Our statistical analysis followed the convention of reporting NEISS point estimates, without considering random sampling error. We focused on the possibility of systematic error, not of random sampling error (confidence intervals for the unadjusted estimates of assault-related nonfatal gunshot injuries are shown in Table A, available as a supplement to the online version of this article at http://www.ajph.org).
We extracted data for national counts of firearm injury deaths from CDC’s Web-based Injury Statistics Query and Reporting System, which in turn is derived from CDC’s National Vital Statistics System mortality data. The Web-based Injury Statistics Query and Reporting System provides annual national counts for deaths caused by “firearms,” classified by intent. For our purposes, the relevant intents are homicide, legal intervention, suicide, and unintentional. Each of these has a natural association with the NEISS-FISS intent codes, and in particular “assault” matches with “homicide.” We defined the case–fatality rate as the ratio of the relevant–intent death count to the sum of that death count and the estimate of nonfatal cases.
RESULTS
In 2012, the NEISS-FISS estimate of the number of nonfatal gunshot cases treated in EDs was 74 007. Of these, 72.0% were classified as assault, 17.8% as unintentional, 5.2% as self-harm, 1.2% as legal intervention, and 3.8% as unknown.
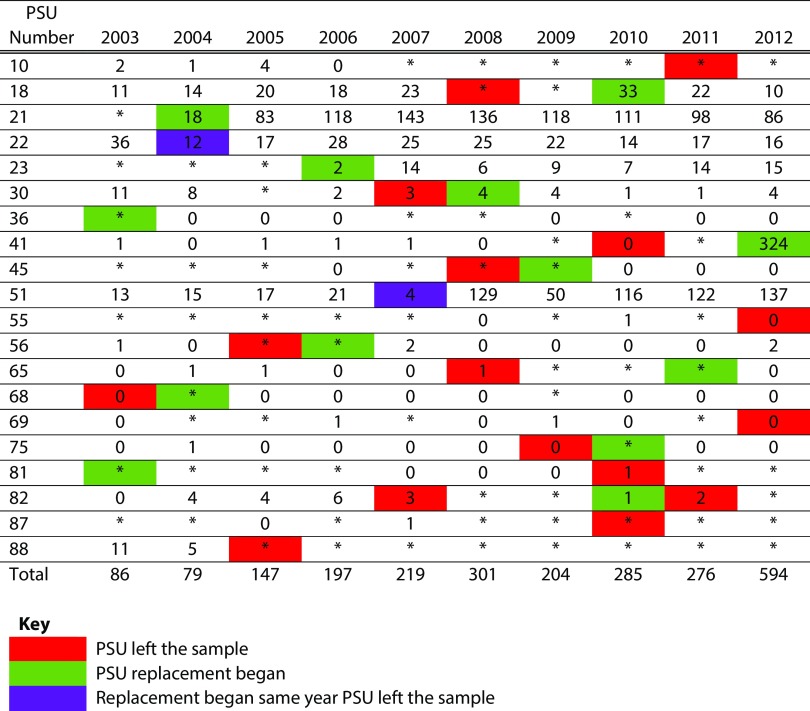
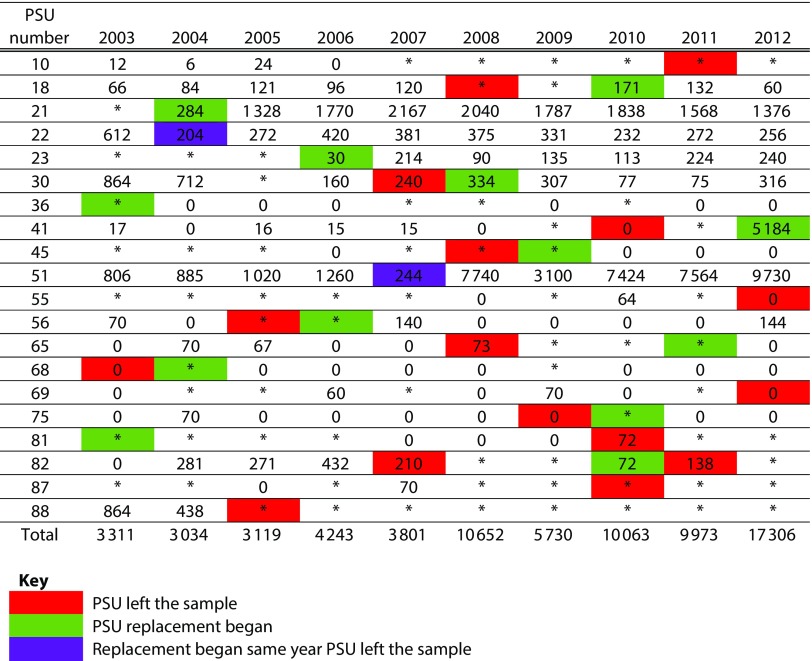
During the decade 2003 to 2012, the reporting hospital was replaced in 15 of the PSUs. In several cases the result was a sharp discontinuity in the estimated number of firearms gunshot cases. For PSU 51, NEISS-FISS reported that the number of cases increased from 7 in 2007 (the original hospital) to 149 in 2008 (the new hospital). Because of the sample weights, this replacement had the effect of adding 8513 cases to the estimated national total. Similarly, PSU 41 increased from 3 cases in 2010 to 358 cases in 2012 (the first year the replacement hospital reported to NEISS), adding almost 5679 cases to the national estimate. Focusing just on assault cases, the PSU 51 replacement added 7496 to the national total (an 18% increase), and the PSU 41 replacement added 5184 cases (an 11% increase). Data for all PSUs that incurred hospital replacement are included in Figures 1 and 2.
FIGURE 1—
Number of Persons With Nonfatal Firearm Injuries From Assault Treated in National Electronic Injury Surveillance System—All Injury Program–Sample Emergency Departments: United States, 2003–2012
Note. PSU = primary sampling unit. Sample emergency departments were PSUs in which the sample hospital was replaced sometime during 2003 and 2012. Unweighted. “0” indicates firearm-related injuries occurred but were not classified as assault.
*The hospital did not report any firearm-related injury.
FIGURE 2—
Number of Persons With Nonfatal Firearm Injuries From Assault Treated in National Electronic Injury Surveillance System—All Injury Program–Sample Emergency Departments: United States, 2003–2012
Note. PSU = primary sampling unit. Sample emergency departments were PSUs in which the sample hospital was replaced sometime during 2003 and 2012. Counts multiplied by National Electronic Injury Surveillance System—All Injury Program national weights. “0” indicates firearm-related injuries occurred but were not classified as assault.
*The hospital did not report any firearm-related injury.
A possible explanation for the implausible increase in gunshot cases for PSUs 41 and 51 is that the replacement hospital happened to be the lead treatment facility for gunshot cases. Note, however, that our adjustment process is not motivated by the belief that the old hospital is more representative than the new one. Rather, the adjustment is motivated by our goal of eliminating the distorting effect of the replacement on the observed 10-year trend.
As shown in Table 1, for the decade 2003 to 2012 the total NEISS-FISS estimate of the number of nonfatal cases classified as “assault” increased by 49% (from 35 768 to 53 293). During that time period the firearm homicide count actually declined slightly. The diverging trends resulted in a sharp decline in the implied case–fatality rate, from 25% to 18%, suggesting a considerable improvement in the survivability of gunshot wounds. But following the 2 adjustments, the trend was flat during that period, equal to 22% in both the first and last years with little variation in between.
TABLE 1—
National Estimates of the Number of Persons With Nonfatal Firearm Injuries for Assault Treated in Hospital Emergency Departments and Fatal Firearm Injuries for Homicides: United States, 2003–2012
| Nonfatal Injuries |
Fatal Injuries |
|||||
| Year | Unadjusted, No. | Adjusted for Hospital Replacement, No. | Adjusted for Replacement and Distribution of Unknowns, No. | Homicides, No. | Unadjusted Case–Fatality Rate, % | Adjusted Case–Fatality Rate, % |
| 2003 | 35 768 | 36 265 | 41 874 | 11 920 | 25 | 22 |
| 2004 | 38 303 | 39 350 | 44 374 | 11 624 | 23 | 21 |
| 2005 | 43 727 | 44 100 | 48 383 | 12 352 | 22 | 20 |
| 2006 | 43 799 | 43 552 | 47 162 | 12 791 | 23 | 21 |
| 2007 | 42 057 | 42 216 | 47 283 | 12 632 | 23 | 21 |
| 2008 | 47 659 | 40 952 | 45 575 | 12 179 | 20 | 21 |
| 2009 | 38 384 | 36 669 | 40 740 | 11 493 | 23 | 22 |
| 2010 | 45 966 | 39 848 | 41 813 | 11 078 | 19 | 21 |
| 2011 | 46 343 | 40 315 | 42 907 | 11 068 | 19 | 21 |
| 2012 | 53 293 | 39 932 | 41 996 | 11 622 | 18 | 22 |
Note. Includes nonfatal firearm-related gunshot wounds only.
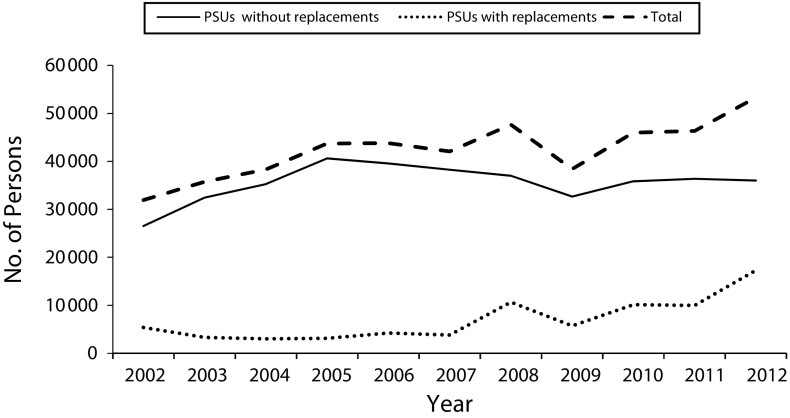
Figure 3 demonstrates the importance of the tendency for replacement hospitals to have more gunshot cases than do the hospitals they replace. The top line plots the unadjusted national estimates of assault cases, the first column of Table 1. The middle line plots the estimated total for PSUs with no replacement, and the bottom line is the estimated total for the 15 PSUs that did experience a replacement. The upward trend in the national total is entirely because of the strong upward trend in the PSUs with replacements.
FIGURE 3—
National Estimates of the Number of Persons With Nonfatal Firearm Injuries From Assault Treated in Hospital Emergency Departments in Primary Sampling Units (PSUs) With Replacements and PSUs Without Replacements: United States, 2003–2012
DISCUSSION
After adjusting for problematic features of the NEISS data, the case–fatality rate for firearm assault injuries remained stable from 2003 to 2012, suggesting that the recent decline in the firearm homicide rate is a result of the decline in the number of firearm assaults, rather than to improvements in trauma care for firearm injuries. Previous reports of an apparent declining case–fatality rate1–3 may be readily attributed to a few instances when the hospitals selected as replacements in the NEISS sample implausibly reported orders of magnitude more gunshot cases (despite representing the same PSU) and to a downward trend in the likelihood that assault cases were classified as “unknown circumstance.”
Our findings are supported by findings from other national and regional data sources. An analysis of the largest national sample of inpatient hospital discharges from 2003 to 2011 found that the case–fatality rate for firearm-related hospitalizations remained stable,5 whereas the national registry of trauma cases reported firearm-related trauma case–fatality rates from 2003 to 2014 that were virtually unchanged.4 Focusing particularly on firearm-related assault, a census of California hospital discharge records from 1992 to 2010 reported that case–fatality rates for firearm assault injuries increased from 1992 to 2002 and remained stable thereafter.6
We note that the case–fatality rates we have documented in this study (and others) are biased upward because some nonfatal gunshot cases are not treated in a hospital. However, the vast majority of nonfatal cases are treated,13 so the bias is small. More important for our purposes, there is no reason to expect that there is any trend in the proportion of nonfatal cases that go untreated over the decade under study.
PUBLIC HEALTH IMPLICATIONS
Our study suggests that the recent trend in firearm homicides is proportional to the number of firearm assaults resulting in gunshot injury and has not been noticeably influenced by changes in the lethality of firearm violence. Other national data on assault-related injuries and reports from individual trauma centers support that conclusion.14–16
ACKNOWLEDGMENTS
This work was supported by the National Institute on Drug Abuse (grant R21DA041154 to M. C.).
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary because the analysis was limited to secondary analysis of aggregate data.
REFERENCES
- 1.Fields G, McWhirter C. In medical triumph, homicides fall despite soaring gun violence. 2012. Available at: http://online.wsj.com/article/SB10001424127887324712504578131360684277812.html. Accessed March 10, 2016.
- 2.Jena AB, Sun EC, Prasad V. Does the declining lethality of gunshot injuries mask a rising epidemic of gun violence in the United States? J Gen Intern Med. 2014;29(7):1065–1069. doi: 10.1007/s11606-014-2779-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalesan B, Adhikaria A, Pressley JC et al. The hidden epidemic of firearm injury: increasing firearm injury rates during 2001–2013. Am J Epidemiol. 2017;185(7):546–553. doi: 10.1093/aje/kww147. [DOI] [PubMed] [Google Scholar]
- 4.American College of Surgeons. National Trauma Data Bank 2015: Annual Report. Chicago, IL: 2015. [Google Scholar]
- 5.Agarwal S. Trends and burden of firearm-related hospitalizations in the United States across 2001–2011. Am J Med. 2015;128(5):484–492.e1. doi: 10.1016/j.amjmed.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Office of Statewide Health Planning and Development. Trends in Firearm-Related Emergency Department Visits and Hospitalizations in California, 1992 to 2010. Sacramento, CA: 2013. [Google Scholar]
- 7.Centers for Disease Control and Prevention. Surveillance for fatal and nonfatal firearm-related injuries—United States, 1993–1998. MMWR Surveill Summ. 2001;50(SS02):1–32. [Google Scholar]
- 8.Centers for Disease Control and Prevention. Fatal injury reports, national and regional, 1999–2015. Available at: http://webappa.cdc.gov/sasweb/ncipc/mortrate10_us.html. Accessed June 13, 2016.
- 9.Centers for Disease Control and Prevention. Surveillance for fatal and nonfatal injuries—United States, 2001. MMWR Surveill Summ. 2004;53(7):1–57. [PubMed] [Google Scholar]
- 10.US Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Injury Prevention and Control. Firearm Injury Surveillance Study, 1993–2012. Ann Arbor, MI: Inter-University Consortium of Political and Social Research; 2015. ICPSR 36290. [Google Scholar]
- 11.Burney H, Schroeder T. Updated 2012 NEISS Weights Using the 2011 SDI Hospital Frame. Bethesda, MD: US Consumer Product Safety Commission; 2012. [Google Scholar]
- 12.Kellermann AL, Rivara FP, Lee RK et al. Injuries due to firearms in three cities. N Engl J Med. 1996;335(19):1438–1444. doi: 10.1056/NEJM199611073351906. [DOI] [PubMed] [Google Scholar]
- 13.May JP, Hemenway D, Hall A. Do criminals go to the hospital when they are shot? Inj Prev. 2002;8(3):236–238. doi: 10.1136/ip.8.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Efron DT, Haider A, Chang D, Haut ER, Brooke B, Cornwell EE., 3rd Alarming surge in nonsurvivable urban trauma and the case for violence prevention. Arch Surg. 2006;141(8):800–803. doi: 10.1001/archsurg.141.8.800. discussion 803–805. [Erratum in Arch Surg. 2006;141(10):1042. Haut, Elliot R corrected to Haut, Elliott R] [DOI] [PubMed] [Google Scholar]
- 15.Livingston DH, Lavery RF, Lopreiato MC, Lavery DF, Passannante MR. Unrelenting violence: an analysis of 6,322 gunshot wound patients at a level I trauma center. J Trauma Acute Care Surg. 2014;76(1):2–9. doi: 10.1097/TA.0b013e3182ab19e7. discussion 9–11. [DOI] [PubMed] [Google Scholar]
- 16.Sauaia A, Gonzalez E, Moore HB, Bol K, Moore EE. Fatality and severity of firearm injuries in a Denver trauma center, 2000–2013. JAMA. 2016;315(22):2465–2467. doi: 10.1001/jama.2016.5978. [DOI] [PubMed] [Google Scholar]