Abstract
Objectives. To examine the health-related quality of life among workers in 22 standard occupation groups using data from the 2013–2014 US Behavioral Risk Factor Surveillance System.
Methods. We examined the health-related quality of life measures of self-rated health, frequent physical distress, frequent mental distress, frequent activity limitation, and frequent overall unhealthy days by occupation group for 155 839 currently employed adults among 17 states. We performed multiple logistic regression analyses that accounted for the Behavioral Risk Factor Surveillance System’s complex survey design to obtain prevalence estimates adjusted for potential confounders.
Results. Among all occupation groups, the arts, design, entertainment, sports, and media occupation group reported the highest adjusted prevalence of frequent physical distress, frequent mental distress, frequent activity limitation, and frequent overall unhealthy days. The personal care and service occupation group had the highest adjusted prevalence for fair or poor self-rated health.
Conclusions. Workers’ jobs affect their health-related quality of life.
Health-related quality of life (HRQOL) addresses a wide range of public health priorities. The Centers for Disease Control and Prevention has defined HRQOL as “an individual’s or group’s perceived physical and mental health over time.”1(p4–6) HRQOL measures are designed to understand dysfunction and disability related to diseases, injuries, and health behaviors at an individual and community level.1 Reported perception of an individual’s health, overall psychological well-being, and ability to function physically can guide individual treatment of chronic illnesses and suggest effective interventions.2,3 The HRQOL measures provide needed health surveillance and measure beneficial impacts for analyses in public health policy, health care economics, psychology, sociology, environmental sustainability, and urban planning.1,2 Besides being reliable and valid,4,5 the Centers for Disease Control and Prevention HRQOL measures have been studied with other HRQOL measures, such as the Short Form-36 Health Survey, to test associations between these measures as well as to determine if they have value in surveys other than the Behavioral Risk Factor Surveillance System.6
The Centers for Disease Control and Prevention HRQOL measures have been studied with respect to various health outcomes and behaviors,7 sociodemographic factors,8 and environmental measures9 to determine if certain groups should receive interventions. Although employment status has been used as a covariate in some HRQOL studies,7,8 specific type of work performed (or occupation) has been only rarely included.
In a study of occupations among Washington State workers, those in protective services, those in cleaning and building services, and truck drivers reported significantly more frequent mental distress (≥ 14 mentally unhealthy days in the past 30 days) than did workers in management, even after controlling for potential confounders.10 Different occupations also involve different demands, both physical and mental, as well as differences in control that allows workers to meet those demands.11 For example, in the Netherlands, employees with high-demand but low-control jobs reported more emotional exhaustion, psychosomatic and physical health complaints, and job dissatisfaction than did other employees.12 In a British prospective cohort study, the Whitehall II study, employees with low decision latitude (job control) and high job demand (job strain) had the highest risk of coronary heart disease.13 Although job strain and job control have been linked to a number of health outcomes and HRQOL, occupation itself, which substantially determines these 2 factors, remains largely unstudied.
Among employed US adults, the prevalence of negative workplace psychosocial factors (job insecurity, work–family imbalance, and hostile work environment) and work organization characteristics (long work hours, temporary positions, etc.) varies by industry and occupation even after controlling for demographic variables.14,15 For example, the highest prevalence of a hostile work environment occurred among those working in protective services, whereas the highest prevalence of job insecurity occurred among those working in construction and extraction.14,15 Despite these few studies, the relationship between work-related psychosocial and work organization factors and HRQOL remains unclear because none of these studies attempted to connect these factors to HRQOL.
To our knowledge, we are the first to evaluate Behavioral Risk Factor Surveillance System HRQOL measures among occupation groups across several states. We hypothesized that, after adjusting for potential confounders including household income, currently employed workers in jobs that are physically demanding or that involve little autonomy such as production, health care support, and building and grounds cleaning and maintenance would have worse HRQOL than would workers in jobs that are traditionally office based, require little physical work, and offer more autonomy, such as legal, management, and life, physical, and social sciences.
METHODS
The Behavioral Risk Factor Surveillance System (BRFSS) is an annual government-funded survey conducted by state health departments over landline and cellular phones and administered to the US noninstitutionalized adult (aged ≥ 18 years) population.16 The BRFSS median response rate is 49.6% from landline phones and 37.8% from cellphones.16 BRFSS is composed of a standard core set of questions, a biannual rotating core, optional modules, and state-added questions that address topics related to health-risk behaviors, preventive health practices, and access to care.16 The National Institute for Occupational Safety and Health added optional industry and occupation questions to the 2013 and 2014 BRFSS for currently and recently employed adults to allow better understanding of work as a social determinant of health.
The BRFSS industry and occupation optional module is asked of respondents who report their employment status as “employed for wages,” “out of work for less than 1 year,” or “self-employed.” Only respondents who reported they were currently employed (“employed for wages” or “self-employed”) were included. Data from the 17 states that administered the BRFSS industry and occupation optional module during both 2013 and 2014 were used: Illinois, Louisiana, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Montana, Nebraska, New Hampshire, New Jersey, New Mexico, New York, North Dakota, Oregon, Utah, and Washington. Of the 412 829 BRFSS respondents in 2013 and 2014, 155 839 were currently employed among the 17 states and, therefore, were considered for analyses. In 2013, the total sample size of currently employed adults for all 17 states was 79 082, ranging from 15 071 in Massachusetts to 4292 in New York State. In 2014, the total sample size of currently employed adults for all 17 states was 76 757, ranging from 15 654 in Massachusetts to 3235 in New York State.
Measures
Respondents reported their current industry and occupation of employment on the basis of answers to 2 questions. “What kind of work do you do? (for example, registered nurse, janitor, cashier, auto mechanic)” ascertains a respondent’s occupation. “What kind of business or industry do you work in? (for example, hospital, elementary school, clothing manufacturing, restaurant)” ascertains a respondent’s industry. Respondents’ answers to the industry and occupational optional module are recorded as free text and later coded by the National Institute for Occupational Safety and Health’s Industry and Occupation Computerized Coding System or computer assisted coding17 to the 2002 US Census Bureau industry and occupation codes.18 Occupations were then recoded into 22 groups (excluding military) equivalent to the 2-digit Standard Occupational Classification System18 major occupation groups used by the Bureau of Labor Statistics. We examined HRQOL among these 22 occupation groups.
We determined HRQOL from BRFSS’s core Healthy Days measures, which comprise 4 questions on self-rated general health, recent physically unhealthy days, recent mentally unhealthy days, and recent activity limitation days.1 These Healthy Days measures have undergone validity and reliability testing with construct validity and retest reliability found to be moderate to excellent.1,4,5 The first HRQOL measure on self-rated health status asks, “Would you say that in general your health is ___?”19 and provides a 5-point Likert scale for responses: excellent, very good, good, fair, or poor. We dichotomized responses to this question into fair or poor health and excellent, very good, or good health.
The 3 HRQOL questions on physical health, mental health, and activity limitation reference respondents’ health during the previous 30 days: “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?”; “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?”; and “During the past 30 days, for about how many days did poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?”19 On the basis of clinicians’ use of 14 or more days as a guideline for clinical depression and anxiety disorders,20 we dichotomized the responses at 14 or more mentally unhealthy days as “frequent mental distress” and 13 or fewer days as “infrequent mental distress.” Consistent with previous research, we analogously dichotomized physically unhealthy days and recent activity limitation days using the same 14-day cut point, creating 2 more outcomes: “frequent physical distress” and “frequent activity limitation.”7,8
We created an outcome of overall unhealthy days by summing the numbers of physically unhealthy days and mentally unhealthy days, with a maximum of 30 days. Overall unhealthy days is a validated summary index of self-reported mental and physical health that allows researchers to examine trends in health over time and identify groups of people that may need attention.1,5 We also dichotomized overall unhealthy days using the 14-day cut point. Larger percentages of frequent distress, overall unhealthy days, and fair or poor self-rated health indicate worse HRQOL.
Because several sociodemographic characteristics, health-risk behaviors, and protective health behaviors are associated with both occupation group and these 5 HRQOL outcomes, we adjusted models assessing these relationships for the following independent characteristics and behaviors: age (18–34, 35–44, 45–54, 55–64, and ≥ 65 years), gender (men and women), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic multiple race or other race), education level (did not graduate from high school, graduated from high school, attended college or technical school, and graduated from college or technical school), marital status (married or member of an unmarried couple and divorced, widowed, separated, or never married), obesity on the basis of body mass index (< 30 kg/m2 and ≥ 30 kg/m2), smoking status (nonsmokers and current smokers), sleep duration (≤ 6 hours per day and ≥ 7 hours per day), physical activity performed outside of work (exercises outside of work and does not exercise outside of work), and household income (< $25 000, $25 000–$49 999, $50 000–$74 999, ≥ $75 000). We categorized all variables, and we excluded missing data from the analyses.
Statistical Analyses
We used SAS version 9.3 (SAS Institute Inc., Cary, NC) and SAS-callable SUDAAN (RTI International, Research Triangle Park, NC) to perform analyses that account for BRFSS’s complex survey design and use of respondent sampling weights. We used Proc RLOGIST in SAS-callable SUDAAN to calculate adjusted prevalence estimates and their respective 95% confidence intervals (CIs) for each HRQOL measure by occupation group. The SUBPOPX statement allowed us to specify the subpopulation of currently employed adults in the 17 states that used the industry and occupation optional module in both 2013 and 2014 and the NEST statement included the survey year. We considered adjusted prevalence estimates for HRQOL outcomes to differ statistically if their 95% CIs did not overlap. Using nonoverlapping 95% CIs as the test of statistical significance is approximately equivalent to setting the type 1 error for the null hypothesis at an α level of 0.006.21
RESULTS
The unadjusted prevalences of selected sociodemographic characteristics and health-risk behaviors vary across the 22 occupation groups (Table 1). The highest proportion of young (aged 18–34 years) employees occurs in food preparation and serving-related occupations (55.8%), whereas women are most prevalent in health care support occupations (86.9%). Nearly one third of employees in building and grounds cleaning and maintenance (33.9%) and farming, forestry, and fishing occupations (31.4%) are Hispanic. Additionally, the highest prevalences of smoking occur in construction and extraction (28.6%) and food preparation and serving (28.5%) occupations, whereas the highest prevalences of obesity occur in protective service (40.2%) and transportation and material moving (38.3%) occupations (Table 1).
TABLE 1—
Unadjusted, Weighted Sample Characteristics by Occupation Group Among Adults Aged 18 Years or Older: Behavioral Risk Factor Surveillance System, 17 US States, 2013–2014
| Occupation Group (SOC Code) | Frequencya | Aged 18–34 Years, % | Women, % | Hispanic, % | College Graduates, % | Married or Member of Unmarried Couple, % | Current Smokers, % | Annual Income < $25 000, % | BMI ≥ 30 kg/m2, % | Short Sleep (≤ 6 h/d), % | No Physical Activity Outside Work, % |
| Management (11) | 16 760 | 20.3 | 39.6 | 7.4 | 49.4 | 72.1 | 13.0 | 6.5 | 26.0 | 35.0 | 17.6 |
| Business and financial operations (13) | 6 005 | 25.1 | 55.7 | 5.0 | 60.2 | 68.3 | 11.5 | 3.8 | 26.3 | 31.2 | 13.9 |
| Computer and mathematical (15) | 4 436 | 30.9 | 23.4 | 4.4 | 61.6 | 71.4 | 10.6 | 3.8 | 27.6 | 34.1 | 14.1 |
| Architecture and engineering (17) | 3 792 | 26.9 | 12.3 | 3.8 | 62.8 | 72.1 | 10.8 | 2.6 | 27.1 | 34.1 | 13.4 |
| Life, physical, and social science (19) | 2 503 | 31.3 | 46.6 | 5.7 | 78.9 | 70.3 | 7.7 | 3.5 | 17.6 | 29.2 | 10.1 |
| Community and social services (21) | 3 193 | 30.0 | 65.1 | 9.8 | 70.0 | 66.0 | 14.1 | 9.0 | 29.6 | 34.5 | 16.3 |
| Legal (23) | 2 064 | 21.6 | 52.2 | 5.3 | 80.3 | 72.7 | 8.4 | 2.9 | 20.0 | 31.1 | 12.1 |
| Education, training, and library (25) | 11 622 | 25.1 | 73.5 | 5.9 | 75.7 | 69.3 | 7.1 | 8.3 | 23.2 | 29.8 | 14.8 |
| Arts, design, entertainment, sports, and media (27) | 3 147 | 30.9 | 47.2 | 10.9 | 57.2 | 63.4 | 11.8 | 14.6 | 18.1 | 29.5 | 13.0 |
| Health care practitioners and technical (29) | 11 519 | 26.9 | 76.7 | 4.3 | 59.6 | 68.8 | 10.2 | 4.4 | 24.9 | 38.0 | 16.5 |
| Health care support (31) | 3 249 | 41.9 | 86.9 | 12.3 | 15.5 | 46.7 | 20.5 | 38.5 | 33.4 | 44.6 | 22.9 |
| Protective service (33) | 2 536 | 31.8 | 21.9 | 9.8 | 23.6 | 59.5 | 12.5 | 13.1 | 40.2 | 45.4 | 14.9 |
| Food preparation and serving related (35) | 3 932 | 55.8 | 50.1 | 24.2 | 9.9 | 38.6 | 28.5 | 52.9 | 22.2 | 40.3 | 28.9 |
| Building and grounds cleaning and maintenance (37) | 4 440 | 34.6 | 39.8 | 33.9 | 6.7 | 53.3 | 26.0 | 46.8 | 28.8 | 38.2 | 30.7 |
| Personal care and service (39) | 4 504 | 36.8 | 78.3 | 14.0 | 15.6 | 51.7 | 16.9 | 36.6 | 29.1 | 40.0 | 20.1 |
| Sales and related (41) | 12 301 | 39.4 | 47.7 | 9.3 | 28.5 | 55.3 | 18.8 | 24.3 | 26.2 | 34.4 | 22.8 |
| Office and administrative support (43) | 16 151 | 29.0 | 74.1 | 9.4 | 24.7 | 60.6 | 16.4 | 14.9 | 31.0 | 35.8 | 21.9 |
| Farming, fishing, and forestry (45) | 1 074 | 38.7 | 16.8 | 31.4 | 9.2 | 56.8 | 17.7 | 34.9 | 30.0 | 36.6 | 37.2 |
| Construction and extraction (47) | 6 749 | 31.4 | 2.6 | 18.7 | 8.1 | 61.7 | 28.6 | 21.7 | 27.2 | 39.1 | 25.0 |
| Installation, maintenance, and repair (49) | 3 984 | 32.7 | 2.6 | 15.2 | 9.6 | 62.3 | 24.6 | 15.5 | 31.7 | 41.0 | 25.2 |
| Production (51) | 5 654 | 32.6 | 27.8 | 19.1 | 8.4 | 58.4 | 22.7 | 22.3 | 32.6 | 44.6 | 27.2 |
| Transportation and material moving (53) | 5 937 | 30.2 | 17.1 | 15.6 | 7.7 | 55.0 | 25.7 | 27.0 | 38.3 | 43.4 | 31.2 |
Note. BMI = body mass index; SOC = Standard Occupational Classification. The states in this study were IL, LA, MD, MA, MI, MN, MS, MT, NE, NH, NJ, NM, NY, ND, OR, UT, and WA.
Unweighted.
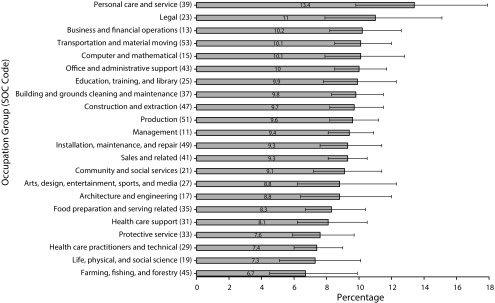
The 4 core HRQOL measures—frequent physical distress, frequent mental distress, frequent activity limitation, and fair or poor self-rated health—as well as the derived measure, frequent overall unhealthy days, vary across the occupation groups (Table 2; Figure 1).
TABLE 2—
Adjusted Prevalence of Frequent Physical Distress, Frequent Mental Distress, Frequent Overall Unhealthy Days, and Frequent Activity Limitation by Occupation Group Among Adults Aged 18 Years or Older: Behavioral Risk Factor Surveillance System, 17 US States, 2013–2014
| Occupation Group (SOC Code) | Frequent Physical Distress, % (95% CI) | Frequent Mental Distress, % (95% CI) | Frequent Overall Unhealthy Days, % (95% CI) | Frequent Activity Limitation, % (95% CI) |
| Management (11) | 6.5 (5.0, 8.4) | 8.7 (7.6, 10.1) | 13.3 (11.5, 15.3) | 2.3 (1.9, 2.8) |
| Business and financial operations (13) | 6.6 (4.8, 9.1) | 9.3 (6.7, 12.8) | 15.0 (11.8, 18.8) | 2.8 (2.2, 3.7) |
| Computer and mathematical (15) | 5.7 (4.4, 7.3) | 7.3 (5.5, 9.7) | 11.5 (9.4, 14.0) | 2.9 (1.6, 5.0) |
| Architecture and engineering (17) | 7.9 (5.6, 11.0) | 7.0 (5.1, 9.5) | 12.4 (9.7, 15.9) | 3.8 (2.3, 6.4) |
| Life, physical, and social science (19) | 6.0 (4.4, 8.1) | 7.9 (5.5, 11.1) | 12.8 (10.0, 16.2) | 2.2 (1.3, 3.7) |
| Community and social services (21) | 8.5 (5.7, 12.6) | 12.9 (6.6, 23.5) | 18.5 (11.6, 28.0) | 3.7 (2.5, 5.6) |
| Legal (23) | 8.3 (6.0, 11.4) | 10.3 (7.2, 14.6) | 14.5 (10.9, 18.9) | 4.0 (2.4, 6.6) |
| Education, training, and library (25) | 6.7 (5.4, 8.4) | 9.5 (7.7, 11.7) | 14.9 (12.7, 17.3) | 3.1 (2.3, 4.3) |
| Arts, design, entertainment, sports, and media (27) | 10.1 (7.2, 13.9) | 13.3 (10.2, 17.3) | 19.1 (15.6, 23.0) | 5.8 (3.8, 8.9) |
| Health care practitioners and technical (29) | 6.7 (5.2, 8.5) | 8.8 (7.3, 10.6) | 13.6 (11.7, 15.8) | 3.0 (2.2, 4.1) |
| Health care support (31) | 6.8 (5.3, 8.7) | 9.5 (7.1, 12.5) | 13.4 (10.8, 16.6) | 5.1 (3.0, 8.7) |
| Protective service (33) | 9.3 (7.1, 12.1) | 9.2 (7.2, 11.7) | 15.7 (12.9, 18.9) | 4.8 (3.3, 6.8) |
| Food preparation and serving related (35) | 6.4 (4.9, 8.4) | 10.0 (8.1, 12.4) | 13.5 (11.3, 16.1) | 3.3 (2.1, 5.1) |
| Building and grounds cleaning and maintenance (37) | 7.2 (5.6, 9.1) | 9.1 (6.8, 12.0) | 14.1 (11.5, 17.1) | 2.9 (1.9, 4.4) |
| Personal care and service (39) | 8.1 (6.5, 10.1) | 10.6 (8.1, 13.9) | 17.1 (13.2, 21.8) | 3.9 (2.6, 5.9) |
| Sales and related (41) | 6.5 (5.6, 7.4) | 8.8 (7.8, 9.9) | 14.2 (12.9, 15.7) | 3.3 (2.6, 4.2) |
| Office and administrative support (43) | 6.9 (5.8, 8.2) | 7.9 (7.0, 8.9) | 13.1 (11.7, 14.5) | 2.7 (2.2, 3.4) |
| Farming, fishing, and forestry (45) | 3.8 (2.2, 6.6) | 5.0 (2.9, 8.3) | 7.5 (4.8, 11.5) | 2.0 (1.0, 4.3) |
| Construction and extraction (47) | 6.5 (5.1, 8.2) | 8.9 (7.2, 11.0) | 12.3 (10.3, 14.6) | 3.0 (2.3, 3.9) |
| Installation, maintenance, and repair (49) | 6.1 (4.7, 7.8) | 9.7 (7.7, 12.2) | 13.2 (10.9, 15.7) | 3.0 (2.0, 4.4) |
| Production (51) | 6.1 (5.0, 7.5) | 9.2 (7.7, 11.0) | 13.0 (11.2, 15.0) | 3.0 (2.1, 4.2) |
| Transportation and material moving (53) | 7.0 (5.7, 8.7) | 10.2 (8.0, 12.8) | 14.1 (11.7, 16.9) | 3.6 (2.6, 5.0) |
Note. CI = confidence interval; SOC = Standard Occupational Classification. Adjusted for age, gender, race/ethnicity, education level, marital status, body mass index, smoking status, income, sleep duration, and physical activity performed outside work. We calculated the unhealthy days variable by adding the number of poor physical and mental health days with a logical maximum of 30 d. (Frequent overall unhealthy days dichotomizes the unhealthy days using the 14-d cut point.) The states in this study were IL, LA, MD, MA, MI, MN, MS, MT, NE, NH, NJ, NM, NY, ND, OR, UT, and WA.
FIGURE 1—
Adjusted Prevalences of Self-Rated Fair or Poor Health by Occupation Group: Behavioral Risk Factor Surveillance System, 17 US States, 2013–2014
Note. SOC = Standard Occupational Classification. The states in this study were IL, LA, MD, MA, MI, MN, MS, MT, NE, NH, NJ, NM, NY, ND, OR, UT, and WA.
The top 3 occupation groups for highest adjusted prevalences of frequent mental distress and the derived measure of frequent overall unhealthy days included (1) arts, design, entertainment, sports, and media; (2) community and social services; and (3) personal care and service (Table 2). Arts, design, entertainment, sports, and media employees also have the highest adjusted prevalence of frequent physical distress (10.1%), followed by protective service (9.3%) and community and social services (8.5%) employees (Table 2).
With regard to frequent activity limitation, arts, design, entertainment, sports, and media employees have the highest adjusted prevalence (5.8%), followed by health care support employees (5.1%) and protective service employees (4.8%; Table 2). Personal care and service employees have the highest adjusted prevalence of fair or poor self-rated health (13.4%), followed by legal (11.0%) and business and financial operations (10.2%) employees (Figure 1). Farming, fishing, and forestry employees have the lowest adjusted prevalences among all occupation groups for each of the HRQOL measures (Table 2; Figure 1).
DISCUSSION
Many studies have examined individual occupations and their relationships to certain injury and illness risks.22–24 Our study expanded on this previous research by evaluating and comparing 22 major occupation groups on HRQOL measures. Work exposures and organization may explain the observed differences among occupation groups. Although the arts, design, entertainment, sports, and media occupation group is large and diverse—it includes artists, actors, athletes, writers, the media, and communication equipment workers—limited research on their work-related health problems is available. To our knowledge, we are the first to demonstrate that this group has some of the highest prevalences of frequent physical distress, frequent mental distress, and frequent activity limitation of all major occupation groups. This group also has one of the highest adjusted prevalence rates of nonstandard work arrangements and alternative shift work among occupation groups.15 The creative work common in this group may have greater work demands and require more work–family multitasking than do other occupation groups.25 Because some media and communication equipment workers in this group carry and operate video cameras, sound equipment, and other gear, their job duties can involve heavy lifting, forceful manual exertions, nonneutral body postures, and insufficient recovery time, all risk factors for musculoskeletal disorders and physical distress.26
Personal care and service employees more commonly rated their health as fair or poor than did other occupation groups and reported higher prevalences for frequent mental distress. In a case–control study from the United Kingdom, hairdressers, a large part of this occupation group, reported significantly more musculoskeletal problems, including work-related shoulder, wrist, hand, and back pain.22 Occupational contact dermatitis, common among hairdressers, impairs quality of life by affecting self-perception and leading to negative psychosocial outcomes.23 Child care workers, another large segment of personal care and service employees, are also at risk for musculoskeletal disorders and burnout from job stressors.24 Working in a low-control environment with an effort–reward imbalance was associated with musculoskeletal disorders among the child care workers.24
Social workers, who account for a large percentage of community and social services employees, likely explain why these employees have one of the highest adjusted prevalences of frequent mental distress among all occupation groups. Social workers are often at risk for burnout because of job demands and stress such as staff shortages, unmanageable caseloads, emotional situations, and challenging clients.27,28 Nineteen percent of a sample of North Carolina social workers reported current depression, and 16% reported having seriously considered suicide at some point in their lives.28 In a sample of California social workers, high role stress and low job autonomy was associated with higher rates of burnout.27 Most previous research corroborates the high adjusted prevalence of frequent mental distress in community and social services employees in this study. Increased social support and changes to work organization may improve health among many of these employees.29
Health care support occupations, with the most female workers of the occupation groups, have one of the highest adjusted prevalence of frequent activity limitation among all occupation groups. According to the US Bureau of Labor Statistics, nursing, psychiatric, and home health aides, who account for approximately two thirds of all health care support occupations, ranked over a 10-year period among the top of occupation groups reporting the most cases of workplace injuries and illnesses.30 Health care support occupations also experience the highest risks of musculoskeletal disorders.31 Patient handling to provide basic care such as bathing, grooming, feeding, dressing, and moving assistance is a significant portion of health care support employees’ daily job tasks.30,31 Patient handling is also a major risk factor for musculoskeletal disorders and other injuries because it involves a significant amount of movement and different postures, from twisting and bending to whole body repetitive motion and lifting in addition to a fast work pace and ever-changing work environments.31,32
We found that certain occupation groups such as arts, design, entertainment, sports, and media, personal care, and service, community, and social services, and health care support should be further evaluated with regard to HRQOL because they have some of the highest prevalences of the negative core HRQOL measures. Although these groups frequently report HRQOL problems, this does not mean other occupation groups should be ignored. Although farming, fishing, and forestry employees reported the lowest adjusted prevalences of every adverse HRQOL measure, another study that was not limited by self-reporting bias found that farming, fishing, and forestry employees had the highest rate of suicide among occupation groups.33 Comparison of this study with that one suggests that farming, fishing, and forestry workers are reluctant to report poor HRQOL or that economic stress or workplace isolation may increase their suicide rates.
Stress-related illnesses, mental and physical, are costing the US economy more than $200 billion each year in the form of lost wages, absenteeism, and reduced productivity, and this has increased the interest in understanding how work affects health.34 Recent meta-analyses have attempted to answer the questions “Can work make you sick?” and “Can work make you mentally ill?” by examining work-related factors such as lack of control, workload, work hours, role ambiguity, and low social support.34,35 Organizational constraints, role conflict, interpersonal conflict, and workload were most strongly associated with physical symptoms such as headaches, fatigue, and appetite.34 More than 10 work-related factors, including low control and high demand, were associated with increased rates of certain mental health problems.35 Job characteristics are clearly linked to HRQOL. Some of our findings, however, are difficult to explain and did not support this hypothesis. For example, the physically demanding and often low autonomy occupations groups of installation, maintenance, and repair and production reported some of the lowest prevalences of frequent physical distress. Additionally, legal, business, and financial operations and computer and mathematical operations had some of the highest prevalences of fair or poor self-rated health. However, health care support and protective services had higher prevalences of frequent activity limitation, and this supports the hypothesis that physically demanding jobs are likely to have poorer HRQOL. Ultimately, the results indicate that the relationship between work and health is complex and multifactorial in nature. Our study suggests that occupation is relevant and important in this field and should not be overlooked. More research is needed to better assess differences among occupation groups for HRQOL measures as well as to understand how job characteristics are related to HRQOL.
Strengths and Limitations
We are the first, to our knowledge, to examine the association between occupation and HRQOL across multiple states. The HRQOL measures and the 22 occupation groups have been used in various previous studies. Besides using these validated and consistent HRQOL measures and occupation groups, the BRFSS, one of the nation’s largest and most established telephone surveys of behavioral health risks, provided information from nearly 156 000 US adults in 17 states on both HRQOL and several important confounding factors associated with HRQOL.
This study is subject to several limitations. Misclassification bias is possible because of errors during the coding of industry and occupation. The 22 broad occupation groups made it impossible to study more detailed occupation groups and still maintain statistical power. Because BRFSS data are cross-sectional, making causal inferences was not possible, although occupational choice probably preceded recent HRQOL outcomes. The accuracy of self-reported responses in BRFSS depends directly on a respondent’s memory as well as recall and social desirability biases. Adjusting for family income as a confounder excluded 13% of respondents, who likely differ markedly from respondents who reported their incomes. Because only 17 states used the BRFSS industry and occupation module in both 2013 and 2014, the study results may not be generalizable to the currently employed US population. BRFSS does not contain questions regarding work characteristics such as job demand and control, so it is not possible to measure any association between these factors, occupation group, or HRQOL. Lastly, even though we evaluated the confounders most commonly associated with HRQOL, because HRQOL is a complex set of measures, potentially unmeasured confounders, other potential confounders in the data set that we did not assess, and how we categorized our confounders may have affected our results.
Public Health Implications
Persistent variabilities in HRQOL exist among workers from different occupation groups even after adjustment for several sociodemographic and health behavior variables. No previous research has examined the BRFSS HRQOL measures among occupation groups at the multistate level, and more research is needed to understand these variabilities fully. Our research highlights the importance of considering occupation in HRQOL research as well as the need to collect information about occupation in large-scale health surveys such as the BRFSS. Interventions to improve HRQOL can be tailored to the needs of specific occupations and carried out in workplaces.
ACKNOWLEDGMENTS
This study was funded in part by the National Institute for Occupational Safety and Health (cooperative agreement PAR14-275).
We would like to acknowledge Jeff Purdin, Pam Schumacher, Susan Burton, and Jan Birdsey for preparing the Behavioral Risk Factor Surveillance System (BRFSS) industry and occupation module data for analyses. This article is grounded on module data contributed by 17 state BRFSS coordinators. We acknowledge the Washington State Department of Health for giving the Centers for Disease Control and Prevention (CDC) permission to include their state-added 2013 BRFSS industry and occupation data. We obtained data from the following institutions: Washington State Department of Health, Center for Health Statistics, and the module BRFSS, which is supported in part by the CDC (cooperative agreement U58/SO000047-1–3; 2011–2013).
Note. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
HUMAN PARTICIPANT PROTECTION
The CDC institutional review board determined this study to be exempt research activity (protocol #2988.0 under 45 CFR 46.101(b)(2)).
REFERENCES
- 1.Measuring Healthy Days: Population Assessment of Health-Related Quality of Life. Atlanta, GA: Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 2.Hennessy CH, Moriarty DG, Zack MM, Scherr PA, Brackbill R. Measuring health-related quality of life for public health surveillance. Public Health Rep. 1994;109(5):665–672. [PMC free article] [PubMed] [Google Scholar]
- 3.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118(8):622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 4.Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. 2003;57(5):339–343. doi: 10.1136/jech.57.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newschaffer CJ. Validation of Behavioral Risk Factor Surveillance System (BRFSS) HRQOL Measures in a Statewide Sample. Atlanta, GA: Centers for Disease Control and Prevention; 1998. [Google Scholar]
- 6.Barile JP, Horner-Johnson W, Krahn G et al. Measurement characteristics for two health-related quality of life measures in older adults: the SF-36 and the CDC Healthy Days items. Disabil Health J. 2016;9(4):567–574. doi: 10.1016/j.dhjo.2016.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abell JE, Hootman JM, Zack MM, Moriarty D, Helmick CG. Physical activity and health related quality of life among people with arthritis. J Epidemiol Community Health. 2005;59(5):380–385. doi: 10.1136/jech.2004.028068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Balsam KF, Mincer SL. Disparities in health-related quality of life: a comparison of lesbians and bisexual women. Am J Public Health. 2010;100(11):2255–2261. doi: 10.2105/AJPH.2009.177329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zullig KJ, Hendryx M. Health-related quality of life among central Appalachian residents in mountaintop mining counties. Am J Public Health. 2011;101(5):848–853. doi: 10.2105/AJPH.2010.300073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fan ZJ, Bonauto DK, Foley MP, Anderson NJ, Yragui NL, Silverstein BA. Occupation and the prevalence of current depression and frequent mental distress, WA BRFSS 2006 and 2008. Am J Ind Med. 2012;55(10):893–903. doi: 10.1002/ajim.22094. [DOI] [PubMed] [Google Scholar]
- 11.Clougherty JE, Souza K, Cullen MR. Work and its role in shaping the social gradient in health. Ann N Y Acad Sci. 2010;1186(1):102–124. doi: 10.1111/j.1749-6632.2009.05338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Jonge J, Bosma H, Peter R, Siegrist J. Job strain, effort-reward imbalance and employee well-being: a large-scale cross-sectional study. Soc Sci Med. 2000;50(9):1317–1327. doi: 10.1016/s0277-9536(99)00388-3. [DOI] [PubMed] [Google Scholar]
- 13.Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health. 2003;57(2):147–153. doi: 10.1136/jech.57.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alterman T, Luckhaupt SE, Dahlhamer JM, Ward BW, Calvert GM. Job insecurity, work-family imbalance, and hostile work environment: prevalence data from the 2010 National Health Interview Survey. Am J Ind Med. 2013;56(6):660–669. doi: 10.1002/ajim.22123. [DOI] [PubMed] [Google Scholar]
- 15.Alterman T, Luckhaupt SE, Dahlhamer JM, Ward BW, Calvert GM. Prevalence rates of work organization characteristics among workers in the US: data from the 2010 National Health Interview Survey. Am J Ind Med. 2013;56(6):647–659. doi: 10.1002/ajim.22108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System—Overview: BRFSS 2014. 2015. Available at: http://www.cdc.gov/brfss/annual_data/2014/pdf/overview_2014.pdf. Accessed July 1, 2016.
- 17.National Institute for Occupational Safety and Health. Industry and occupation coding. 2016. Available at: http://www.cdc.gov/niosh/topics/coding/how.html. Accessed August 31, 2016.
- 18.Bureau of Labor Statistics. Standard occupational classification. 2010. Available at: http://www.bls.gov/soc. Accessed July 1, 2016.
- 19.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system questionnaire. 2014. Available at: http://www.cdc.gov/brfss/questionnaires/pdf-ques/2014_brfss.pdf. Accessed July 1, 2016.
- 20.Strine TW, Chapman DP, Kobau R, Balluz L, Mokdad AH. Depression, anxiety, and physical impairments and quality of life in the US noninstitutionalized population. Psychiatr Serv. 2004;55(12):1408–1413. doi: 10.1176/appi.ps.55.12.1408. [DOI] [PubMed] [Google Scholar]
- 21.Knol MJ, Pestman WR, Grobbee DE. The (mis)use of overlap of confidence intervals to assess effect modification. Eur J Epidemiol. 2011;26(4):253–254. doi: 10.1007/s10654-011-9563-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bradshaw L, Harris-Roberts J, Bowen J, Rahman S, Fishwick D. Self-reported work-related symptoms in hairdressers. Occup Med (Lond) 2011;61(5):328–334. doi: 10.1093/occmed/kqr089. [DOI] [PubMed] [Google Scholar]
- 23.Cvetkovski RS, Zachariae R, Jensen H, Olsen J, Johansen JD, Agner T. Quality of life and depression in a population of occupational hand eczema patients. Contact Dermatitis. 2006;54(2):106–111. doi: 10.1111/j.0105-1873.2006.00783.x. [DOI] [PubMed] [Google Scholar]
- 24.Koch P, Stranzinger J, Nienhaus A, Kozak A. Musculoskeletal symptoms and risk of burnout in child care workers—a cross-sectional study. PLoS One. 2015;10(10):e0140980. doi: 10.1371/journal.pone.0140980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schieman S, Young M. The demands of creative work: implications for stress in the work–family interface. Soc Sci Res. 2010;39(2):246–259. [Google Scholar]
- 26.Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol. 2004;14(1):13–23. doi: 10.1016/j.jelekin.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 27.Kim H, Stoner M. Burnout and turnover intention among social workers: effects of role stress, job autonomy and social support. Adm Soc Work. 2008;32(3):5–25. [Google Scholar]
- 28.Siebert DC. Depression in North Carolina social workers: implications for practice and research. Soc Work Res. 2004;28(1):30–40. [Google Scholar]
- 29.Lloyd C, King R, Chenoweth L. Social work, stress and burnout: a review. J Ment Health. 2002;11(3):255–265. [Google Scholar]
- 30.Hoskins AB. Occupational Injuries, Illnesses, and Fatalities Among Nursing, Psychiatric, and Home Health Aides, 1995–2004. Washington, DC: Bureau of Labor Statistics; 2006. [Google Scholar]
- 31.Kim H, Dropkin J, Spaeth K, Smith F, Moline J. Patient handling and musculoskeletal disorders among hospital workers: analysis of 7 years of institutional workers’ compensation claims data. Am J Ind Med. 2012;55(8):683–690. doi: 10.1002/ajim.22006. [DOI] [PubMed] [Google Scholar]
- 32.Marras WS, Davis KG, Kirking BC, Bertsche PK. A comprehensive analysis of low-back disorder risk and spinal loading during the transferring and repositioning of patients using different techniques. Ergonomics. 1999;42(7):904–926. doi: 10.1080/001401399185207. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Suicide rates by occupational group—17 states, 2012. MMWR Morb Mortal Wkly Rep. 2016;65(25):641–645. doi: 10.15585/mmwr.mm6525a1. [DOI] [PubMed] [Google Scholar]
- 34.Nixon AE, Mazzola JJ, Bauer J, Krueger JR, Spector PE. Can work make you sick? A meta-analysis of the relationships between job stressors and physical symptoms. Work Stress. 2011;25(1):1–22. [Google Scholar]
- 35.Harvey SB, Modini M, Joyce S et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med. 2017;74(4):301–310. doi: 10.1136/oemed-2016-104015. [DOI] [PubMed] [Google Scholar]