Abstract
Hepatitis B Virus (HBV) vaccination prevalence and its predictors were estimated among Asian, Pacific Islander, Native American, and Multiracial (A-PI-NA-M) adults. Using 2005 National Health and Nutrition Examination Survey data, estimates of HBV vaccination among A-PI-NA-M adults (N = 233) were compared all other racial/ethnic groups. Multivariable logistic regression was used to estimate predictors of vaccination. Among A-PI-NA-M adults 42% (95%CI 34, 50) were HBV immunized, higher than all other racial/ethnic groups. Some college was associated with a 31 % (95%CI 7, 55); a college degree with a 28% (95%CI 8, 49) increased probability of HBV vaccination relative to less education. Each 10-year increase in age was associated with an 11 (95%CI −18, −4) lower probability of HBV vaccination. Access to medical care and immigrant status were not associated with vaccination. Interventions to increase HBV vaccination should target less-educated and older A-PI-NA-M adults, as well as develop strategies so that access to care may increase vaccination.
Keywords: Hepatitis B virus, Asian or pacific islanders, Native Americans, Vaccination, National Health and Nutrition Examination Survey, Liver cancer
Introduction
An estimated 1–1.3 million people in the United States are chronically infected with hepatitis B virus (HBV). Asian and Pacific Islanders account for over half of these cases, with as many as 1 in 10 carrying the virus. HBV is closely linked to cirrhosis and death from liver failure and hepatocellular carcinoma (HCC) [1]. In 1999, Asian and Pacific Islanders were 6–13 times more likely to die from HBV-related cancers than non-Hispanic whites [2, 3]. In Asian and western Pacific countries, the estimated prevalence of chronic HBV infection ranges from 2 to 16% [4] and HBV -related cancers are among the three leading causes of death [5, 6].
The little data available for Native Americans suggest they too are at high risk of HBV infection. A study during the 1990s [7] suggested about 47 per 100,000 of urban and 25 per 100,000 of rural Native Americans were HBV positive, almost twice the rate of Anglo Americans. Native Americans are more likely to engage in activities that increase risk of infection such as excessive alcohol use [8] and injection drug use [9] that may increase proximate risks like sexual assault [10]. HBV -positive Native Americans are also at greater risk of HCC; the annual incidence rate of HCC was 387 for men and 63 for women [11], whereas the worldwide age-adjusted incidence rates were about 15 for men and 5 for women per 100,000 [12].
A recent release by the Office of Minority Health [13], claimed chronic hepatitis B, and liver cancer caused by hepatitis B in Asian Americans, Native Hawaiians, and other Pacific Islanders comprises one of the most serious but frequently neglected racial and ethnic health disparities in the U.S. While less serious, Native Americans might also be included.
Immunization with HBV vaccine is the most effective means of preventing HBV infection [14]. Originally developed in 1981, recommendations by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention (CDC) in 2008 identified several high priority adult populations, including persons born in geographic regions with HBsAg prevalence of ≥2%. Regions with high or intermediate prevalence of HBsAg include much of Eastern Europe, Asia, Africa, the Middle East, and the Pacific Islands [15].
Evaluations of immunization prevalence have been limited. Jain and colleagues [16] assessed immunization of high-risk adults (18–49 years old), defined as having an sexual transmitted disease in the past five years or engaging in a high-risk behavior such as trading sex for goods, and found 20% were vaccinated against HBV. Laboratory testing among adolescent and young adult men who have sex with other men in the U.S. suggest 9% were HBV immunized [17]. Trends in HBV vaccination are rarely reported. Koya and colleagues [18] showed that most of the increase in adult HBV immunization followed a cohort effect (vaccinated children have reached adulthood) rather than increases among high-risk adults not included in child vaccination campaigns. Unfortunately, these studies did not evaluate vaccination prevalence among Asian, Pacific Islanders or Native Americans.
There is a dearth of data on HBV vaccination prevalence among Asian, Pacific Islanders or Native Americans in the U.S. For example, our review found the most recent California Health Interview Studies, Behavioral Risk Factor Surveillance System, and The National Latino and Asian American Study did not include a single item on HBV vaccination. Our study fills this knowledge gap by identifying Asian American, Pacific Islander, Native American, and Multiracial (A-PI-NA-M) adults in the 2005 National Health and Nutrition Examination Survey (NHANES), adapting methods from Hightower and colleagues [19], to obtain population estimates of HBV vaccination prevalence and its predictors. A priori expectations consistent with the high risk of infection among A-PI-NA-M adults suggest a lower prevalence of HBV vaccination than among other racial/ethnic groups. Risk perception and structural inequalities suggest that less-educated, socially isolated, younger, and male adults have a greater risk of failure to vaccinate [20-22]. CDC recommendations suggest that A-PI-NA-M adults with a primary source of care, insurance, or who have seen a clinician in the past year are more likely to be vaccinated [23].
Methods
The NHANES is a probability sample of the non-institutionalized English and Spanish speaking civilian population in the US We used data from the most recently available NHANES (2005) to compare HBV vaccination prevalence among adults (age 18 years and older) in the “other” racial/ethnic group (all participants who self-identified as Asian, Pacific Islander, Native American, multiracial, or a race/ethnicity other than Black, non-Hispanic white, Mexican American, or Hispanic) with those in all other racial/ethnic groups. The “other” group is of interest because it includes people at potentially high risk for HBV infection such as Asian, Pacific Islanders, and Native Americans and no other national data is currently available. Disaggregating to lower levels of analysis was not possible since NHANES did not collect additional identifiers for subjects belonging to the A-PI-NA-M classification.
Among adults included in this analysis, 233 self-identified as Asian, Pacific Islander, Native American, or multiracial, 2,633 as non-Hispanic white, 1,341 as non-Hispanic black, 1,185 as Mexican American, and 171 as “other” Hispanics. About 4% of adult US residents were Asian or Pacific Islander, 1% Native American, and 2% Multiracial, according to the 2000 Census [24], collectively representing 7% of the entire U.S. population. Within the A-PI-NA-M classification, about 53% were Asian or Pacific Islander, 13% Native American, and 34% Multiracial. Among Multiracial, with only two racial/ethnic backgrounds, 44% had some Asian, Pacific Islander, or Native American heritage. No data were available on persons with three or more racial/ethnic identifications; however, more than 95% of Multiracial were biracial/biethnic. If we apply the 2000 Census [24] parameters to the sample, about 81 % of A-PI-NA-M subjects were either, at least in part, Asian, Pacific Islander, or Native American„ groups with assumed high risk of HBV infection. While 19% of respondents may belong to a separate category of multi-racial whose HBV risk is unknown, these are the best available data to assess HBV vaccination among Asian, Pacific Islander, or Native Americans.
Measures
HBV vaccination was measured by responses to “[Have you] ever received the 3-dose series of the hepatitis B vaccine?”; persons reporting “Yes all 3 doses” were coded as HBV vaccinated, and less than 3 doses were coded as not vaccinated. Immigrant status was measured as recent immigrant (5 or fewer years in the US), born in the US, other immigrant (as the reference category). Education was measured as college graduate, some college education, and less (as the reference category). Insured was measured by responses to “are [you] covered by health insurance or some other kind of health care plan?” coded insured or not. Having a source of primary care was indicated by having a place, including “Clinic or health center” or “Doctor’s office or HMO,” respondents “usually go/goes when [they are] sick or need advice about health.” Having seen a physician in the past year was dummy coded yes or no. Age was measured in years.
Analysis
First, prevalence for HBV vaccination by racial/ethnic classification was reported and statistically meaningful differences were appraised using two sample t-tests assuming unequal variances. Second, predictors of failure to immunize among A-PI-NA-M adults were evaluated by including all covariates in a single logistic regression equation (although results were consistent when relying on crude associations). Third, separate logistic regressions were specified for each covariate for a pooled sample of A-PI-NA-M and non-Hispanic white adults that included a dummy indicator for A-PI-NA-M and an interaction with the covariate to estimate differences in the association of predictors with HBV vaccination (results indicate the association for A-PI-NA-M minus association for non-Hispanic White adults). To ease interpretation, predicted probabilities (HBV vaccination or difference in HBV vaccination) were calculated using the estimates from the regression analysis by simulation, using 1,000 randomly drawn sets of estimates from a sampling distribution, with mean equal to the maximum likelihood point estimates and variance equal to the variance covariance matrix of the estimates, with covariates held at their mean [25]. Given the clustered sample design and nonrandom probability of participant inclusion, sample weights that matched the data with age by race/ethnicity by age population distributions were applied, following procedures described elsewhere [26], so estimates are reflective of the general population. Standard error estimates relied on a robust variance estimator [27] to assess hypotheses conservative to Type 1 errors and ensure conclusions are robust to possible violations unaccounted for in model diagnostics. All tests presented are two-tailed P < .05.
Results
Among A-PI-NA-M adults, 53% (95%CI 46,59) were born in the US; the remaining were immigrants, with 8% (95%CI4, 11) having immigrated in the last 5 years. About 30% (95%CI 24, 36) had some college education and 34% were college graduates (95%CI 24, 36). About 83% (95%CI 78, 88) were insured, 75% (95%CI 68, 79) had a source of primary care, and 82% (95%CI 77,87) had seen a clinician in the past year. About 10% (95%CI 6, 14) lived alone, 39% were male, and mean age was 40.57 years.
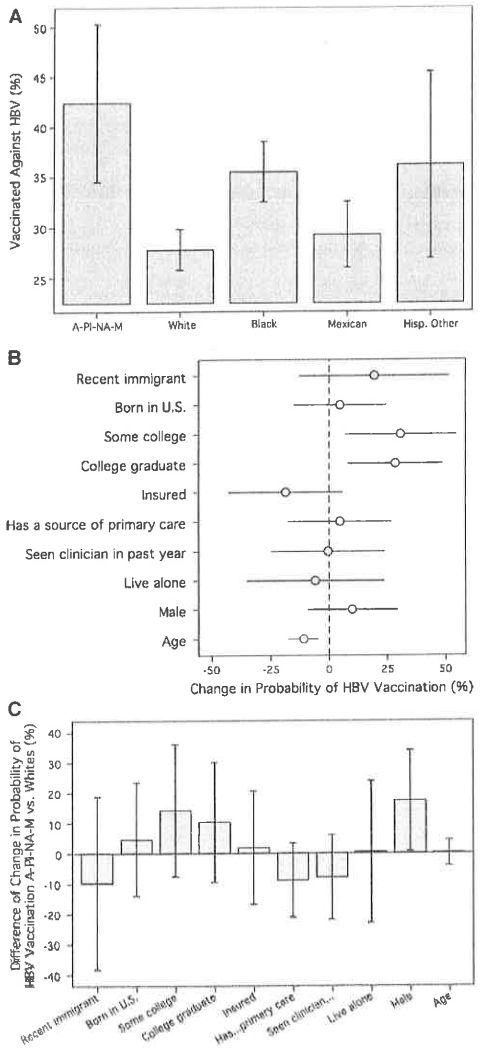
About 42% (95%CI 34, 50) of A-PI-NA-M adults reported receiving all three HBV vaccination shots, as displayed in Fig. 1a. Contrary to expectations, A-PI-NA-M adults had significantly greater vaccination prevalence than non-Hispanic Whites (28%, 95%CI 26, 30; t = 3.78, P < .01) and Mexicans (29%, 95%CI 26, 33; t = 3.16, P < .01). A-PI-NA-M adults also had greater vaccination prevalence than non-Hispanic Blacks (35%, 95%CI 32, 38; t = 1.65, P < .l0) and other Latinos (36%, 95%CI 27, 45; t = 1.00, P < .32), though these differences were statistically insignificant.
Fig. 1.
a HBV Vaccination Prevalence (Mean and 95% confidence interval). b Predictors of HBV Vaccination Among A-PI-NA-MG (n = 201). c Difference in Predictors of Vaccination: A-PI-NA-MG versus Whites
Education and age were significantly associated with HBV vaccination among A-PI-NA-M adults, as displayed in Fig. 1b. Some college was associated with a 31 % (95%CI 7, 55) and a college degree a 28% (95%CI 8, 49) increase in the probability of HBV vaccination relative to high school or less education. Each la-year increase in age was associated with an 11 % (95%CI −18, −4) lower probability of HBV vaccination. Immigrant status, insurance, having a source of primary care, seeing a clinician in the past year, social isolation, and gender were statistically unrelated to HBV vaccination.
Differences in predictors of vaccination for A-PI-NA-M versus non-Hispanic White adults are displayed in Fig. 1c. A-PI-NA-M men were statistically significantly more positively associated with HBV vaccination than White men (17%, 95%CI 1, 34); there was no statistical association for Asians but a significant negative association for Whites. Contrary to expectations, having a source of primary care or seeing a clinician in the past year was more negatively associated with HBV among A-PI-NA-M than White adults but neither difference was statistically significant. The association among insurance, education, immigrant status, or age and HBV vaccination did not significantly differ between A-PI-NA-M and White adults.
Discussion
This was the first study to use national data to estimate HBV vaccination prevalence among A-PI-NA-M adults. A-PI-NA-M adults were more likely than other racial/ethnic groups to be vaccinated against HBV. However, the paradox is this group still has among the highest rates of HBV infection. More than half of A-PI-NA-M adults remain unvaccinated against HBV and these are the adults feeling the brunt of HBV risk. A complete series of vaccinations as part of a secondary prevention program may reduce the disease burden.
The significant positive association between education and HBV vaccination may suggest that knowledge of HBV risks increases vaccination. The significant positive association of HBV vaccination with younger age suggests that attempts to vaccinate American youth are translating into increased vaccination among A-PI-NA-M adults.
The insignificant association of HBV vaccination with insurance status may suggest that economic-driven access to care is inconsequential to vaccination. Specific indicators of access to care suggest nearly all A-PI-NA-M adults have access to some form of care. About 82% of A-PI-NA-M adults had some form of clinician care in the past year, 74% had a source of primary care, and 89% had at least one or the other. However, vaccination rates were no higher for these than A-PI-NA-M adults with limited access to or no care. The association between access to care indicators and vaccination was stronger, though not statistically significantly, for non-Hispanic Whites, suggesting that A-PI-NA-M adults may be receiving the same care when they should be receiving more attentive HBV care. Many A-PI-NA-M adults meet the CDC criteria for immunization, so primary and emergency care clinicians should regularly screen them for HBV vaccination.
The non-association between immigrant status and immunization further exemplifies this need, as immigrants should already be screened for and vaccinated against HBV in the course of care, especially when originating from HBV -endemic nations such as those in Asia. An interaction term for seeing a clinician in the past year and recent immigrant status, was evaluated, and suggests that even among this population seeing a physician was not significantly associated with HBV vaccination (OR = 1.48, 95%CI .29, 7.41).
The reasons high-risk adults, like many A-PI-NA-M, enter into clinician care but remain unvaccinated is unknown. Three explanations may provide some insight. First, clinicians may not know HBV vaccination standards. This reasoning would have additional collateral consequences so that many A-PI-NA-M with clinician counseling would also be unaware of their need to vaccinate. Second, some clinicians may be aware of CDC guidelines but forget/ignore these based on their experiences in the usual course of care of adults at little or no risk of HBV infection. Nearly all adult patients fall outside the high-risk guidelines for HBV vaccination, so clinicians may need priming to ensure recall of CDC guidelines. Third, it may be that communication between clinicians and A-PI-NA-M patients is degraded. Without understanding patient cultural norms cross-communication may happen [28]. One UK study found that general practitioners believed Asian patients required longer consultations, were less compliant, and made excessive and inappropriate use of health services [29]. However, these views may be changing as Asian clinicians increase in number. A recent California study found that Asian clinicians comprised 26% of the physician workforce while the state’s Asian population was 11%. Some evidence from our ongoing qualitative assessments suggests that many clinicians do not recommend Asian Americans to have HBV screening tests. Similarly, in a recent study, many Asian American patients followed by Asian American primary care providers are not perceived as being at risk for chronic hepatitis B and are not screened [30]. Identifying mechanisms to increase screening and vaccination among A-PI-NA-M adults in the course of care should increase HBV screening and vaccinations.
Improved care of HBV risks would likely not infer complete vaccination, especially among the 18% of A-PI-NA-M adults receiving no care in the past year. Community interventions that target A-PI-NA-M adults are necessary. One such intervention by Juon and colleagues [31] was able to initiate vaccination among 99% and successfully vaccinate 79% of unvaccinated participants through Korean and Chinese American churches in the Washington, D.C. metro. The proportion of these persons, who would not have been vaccinated through existing medical care, if vaccination prescriptions for Asian populations were followed, is unknown. However, interventions to reach the most vulnerable, less-educated A-PI-NA-M adults may rely on targeting low skill work places that primarily employee these workers. The negative association between age and vaccination suggests that if A-PI-NA-M adults are not vaccinated early they are less likely to be vaccinated later in life. Expanding current standards that vaccinate adolescents to include all young adults may aid these efforts.
This study has several limitations. Data were not available to assess how behavioral risks for HBV infection, such as sexual activity and injection drug use, coincide with failure to vaccinate against HBV. Similarly, some vaccination-promoting factors could not be adjusted for in this analysis, such as working in a health care-related field. We assume that working in a health care field follows a stochastic pattern across racial/ethnic groups, so it did not interfere with evaluation of differences in vaccination across groups.
The administration of the survey in English may bias the conclusions for more vulnerable non-English-speaking populations. However, the absence of statistically meaningful associations between immigrant status and HBV vaccination· suggests that this unobserved confounding variable may not carry much weight; as additional analysis (Crude OR = .98, 95%CI .51, 1.90) suggested that speaking other languages at home was not associated with HBV vaccination. But these differences are likely a test of differences between fully and mostly acculturated A-PI-NA-M adults and how these data represent the need for HBV vaccination among recent immigrants or the most vulnerable populations is unknown.
It is possible that some respondents misreported their HBV vaccination status, but this should not be more/less likely among A-PI-NA-M than other adults, suggesting the cross-group comparison is not biased. Adults who receive a single HBV vaccine dose may differ from those who do not, but only six A-PI-NA-M adults had begun but not completed their vaccination. This low prevalence suggests that starting the vaccination process, not completing the process, is of concern among A-PI-NA-M adults. Given the aggregation of these data, assessment by specific racial/ethnic sub-group and country of origin was not possible, though the lowest point of aggregation possible was used.
In conclusion, the NHANES was not designed to identify small subgroups at risk, such as A-PI-NA-M adults, but given the limited data on HBV vaccination and the risk burden among this minority popUlation, it is imperative that available data be exploited to the greatest extent possible. This study provided the first population-based estimates of HBV vaccination for A-PI-NA-M adults, mostly comprised of Asian and Pacific Islanders and Native Americans, and suggests some avenues for increased vaccination. Clinicians and interventionists may need to alter current practices to recommend more HBV vaccination when caring for A-PI-NA-M adults. Furthermore, given current data limitations, improved surveillance strategies that include topics related to HBV among subsets of A-PI-NA-M adults are needed.
Acknowledgments
This research was supported by funds provided by the National Cancer Institutes (Grant number R25CA129042) to HSJ supplemented by Federal Student Work Study Aid and intra-departmental support to JWA. Those wishing to replicate this study may have all replication files upon request from JWA (jayers@jhsph.edu). We thank Gary Confessore and C. Richard Hofstetter for helpful criticisms.
Contributor Information
John W. Ayers, Department of Health, Behavior and Society, Johns Hopkins Bloomberg School of Public Health, 624 N. Broadway, Baltimore, MD 21205, USA; Center for Behavioral Epidemiology and Community Health, Graduate School of Public Health, San Diego Stale University, San Diego, CA, USA
Hee-Soon Juon, Department of Health, Behavior and Society, Johns Hopkins Bloomberg School of Public Health, 624 N. Broadway, Baltimore, MD 21205, USA.
Sunmin Lee, Department of Epidemiology and Biostatistics, University of Maryland School of Public Health, College Park, MD, USA.
Eunmi Park, Department of Geriatric Medicine and Gerontology, Johns Hopkins School of Medicine, Baltimore, MD, USA.
References
- 1.Ganem D, Prince AM. Hepatitis B virus infection-natural history and clinical consequences. N Engl J Med. 2004;350:1118–29. doi: 10.1056/NEJMra031087. [DOI] [PubMed] [Google Scholar]
- 2.Ghosh C. Healthy People 2010 and Asian Americans/Pacific Islanders: Defining a Baseline of Information. Am J Public Health. 2003;93:2093–8. doi: 10.2105/ajph.93.12.2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.USDHHS . 2010: National health promotion and disease prevention objectives. US Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 4.Custer B, Sullivan SD, Hazlet TK, Iloeje U, Veenstra DL, Kowdley KV. Global epidemiology of hepatitis B virus. J Clin Gastroenterol. 2004;38:S158–68. doi: 10.1097/00004836-200411003-00008. [DOI] [PubMed] [Google Scholar]
- 5.Asian Liver Center Hepatitis B in Asian American Statistics. 2005 http://livercancer.stanford.edu/Edu/Edu_stat.php.
- 6.Nguyen MH, Keeffe EB. Chronic hepatitis B and hepatitis C in Asian Americans. Rev Gastroenterol Disord. 2003;3:125–34. [PubMed] [Google Scholar]
- 7.Grossman DC, Krieger JW, Sugarman JR, Forquera RA. Health status of urban American Indians and Alaska Natives. J Amer Med Assoc. 1994;271:845–50. [PubMed] [Google Scholar]
- 8.Baldwin JA, Maxwell CJ, Fenaughty AM, et al. Alcohol as a risk factor for HIV transmission among American Indian and Alaska native drug users. Am Indian Alsk Native Ment Health Res. 2000;9:1–16. doi: 10.5820/aian.0901.2000.1. [DOI] [PubMed] [Google Scholar]
- 9.Beauvais P. Trends in drug use among American Indian students and dropouts, 1975 to 1994. Am J Public Health. 1996;86:1594–8. doi: 10.2105/ajph.86.11.1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manson S, Beals J, Klein S, Croy C, the AI-SUPERPFP Team Social epidemiology of trauma among 2 American Indian Reservation Populations. Am J Public Health. 2005;95:851–859. doi: 10.2105/AJPH.2004.054171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McMahon BJ, Alberts SR, Wainwright RB, Bulkow L, Lanier AP. Hepatitis B-related squeals: prospective study in 1400 hepatitis B surface antigen-positive Alaska Native carriers. Arch Intern Med. 1990;150:1051–4. doi: 10.1001/archinte.150.5.1051. [DOI] [PubMed] [Google Scholar]
- 12.Bosch FX, Ribes J, Borra J. Epidemiology of primary liver cancer. Semin Liver Dis. 1999;19:271–86. doi: 10.1055/s-2007-1007117. [DOI] [PubMed] [Google Scholar]
- 13.Office of Minority Health [16 Dec 2008];Goals and strategies to address chronic hepatitis B. http://www.omhrc.gov/templates/brawse.aspx?|v|=2&|v|id=190.
- 14.Poland GA, Jacobson RM. Prevention of hepatitis B with the hepatitis B Vaccine. N Engl J Med. 2004;351:2832–8. doi: 10.1056/NEJMcp041507. [DOI] [PubMed] [Google Scholar]
- 15.Weinbaum CM, Williams I, Mast EE, Wang SA, Finelli L, Wasley A, et al. Recommendations for identification and public health management of person with chronic hepatitis B virus infection. Morb Mortal Wkly Rep. 2008;57(RR08):1–20. [PubMed] [Google Scholar]
- 16.Jain N, Yusuf H, Wortley PM, Euler GL, Walton S, Stokley S. Factors associated with receiving hepatitis B vaccination among high-risk adults in the United States: an analysis of the National Health Interview Survey, 2000. Fam Med. 2004;36:480–6. [PubMed] [Google Scholar]
- 17.MacKellar DA, Valleroy LA, Secura GM, et al. Two decades after vaccine license: hepatitis B immunization and infection among young men who have sex with men. Am J Public Health. 2001;91:965–71. doi: 10.2105/ajph.91.6.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koya DL, Hill EG, Darden PM. The effect of vaccinated children on increased hepatitis B immunization among high-risk adults. Am J Public Health. 2008;98:832–8. doi: 10.2105/AJPH.2007.116046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hightower JM, O’Hare A, Hernandez GT. Blood mercury reporting in NHANES: identifying Asian, Pacific Islander, Native American, and multiracial groups. Environ Health Persp. 2006;114:173–5. doi: 10.1289/ehp.8464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choe JH, Taylor VM, Yasui Y, Burke N, Nguyen T, Acorda E, et al. Health care access and sociodemographic factors associated with hepatitis B testing in Vietnamese American men. J Immigr Minor Health. 2006;8:193–201. doi: 10.1007/s10903-006-9322-1. [DOI] [PubMed] [Google Scholar]
- 21.Ma GX, Fang CY, Shive SE, Toubbeh J, Tan Y, Siu P. Risk perceptions and barriers to hepatitis B screening and vaccination among Vietnamese immigrants. J Immigr Minor Health. 2007;9:213–20. doi: 10.1007/s10903-006-9028-4. [DOI] [PubMed] [Google Scholar]
- 22.Middleman AB. Race/ethnicity and gender disparities in the utilization of a school-based hepatitis B immunization initiative. J Adolescent Health. 2004;34:414–9. doi: 10.1016/j.jadohealth.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 23.Mast EE, Margolis HS, Fiore AE, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States. Morb Mortal Wkly Rep. 2005;55:1–25. [PubMed] [Google Scholar]
- 24.US Census Bureau Demographic Profiles: 100-percent and sample data. 2002 http://www.census.gov/Press-Release/www/2002/demoprofiles.html.
- 25.King G, Tomz M, Wittenberg J. Making the most of statistical analyses: Improving interpretation and presentation. Am J Pol Sci. 2000;44:341–55. [Google Scholar]
- 26.Continuous NHANES web tutorial: Specifying weighting parameters. http://www.cdc.gov/nchs/tutorials/Nhanes/SurveyDesign/Weighting/intro.htm.
- 27.White H. Maximum likelihood estimation of misspecified models. Econometrica: J Econometric Soc. 1982;19:1–25. [Google Scholar]
- 28.Kleinman A. Culture, illness and care: Clinical lessons from anthropological and cross-cultural research. Ann Intem Med. 1978;88:251–8. doi: 10.7326/0003-4819-88-2-251. [DOI] [PubMed] [Google Scholar]
- 29.Ahmad WIU, Baker MR, Kernohan EEM. General practitioners’ perceptions of Asian and non-Asian patients. Fam Pract. 1991;8:52–6. doi: 10.1093/fampra/8.1.52. [DOI] [PubMed] [Google Scholar]
- 30.Chu D, Lok ASF, Tran TT, et al. Hepatitis B virus (HBV) screening practices of Asian-American primary care physicians (PCPs) who treat Asian adults living in the United States; 13th international symposium on viral hepatitis and liver disease; Washington DC. 2009, March.pp. 20–4. [Google Scholar]
- 31.Juon HS, Strong C, Oh TH, Castillo T, Tsai G, Oh LDH. Public health model for prevention of liver cancer among Asian Americans. J Community Health. 2008;33:199–205. doi: 10.1007/s10900-008-9091-y. [DOI] [PubMed] [Google Scholar]