Abstract
Objective
Largest, single-centre study of clinical and functional outcomes of patients who underwent endoprosthetic replacement (EPR) for aggressive distal tibial bone tumours.
Method
Retrospective observational study of eight patients was undertaken.
Results
Median follow-up was 77 months (range 13–276). Cumulative five and ten year survival was 63% and 42% respectively. Three patients developed either disease recurrence or metastases post-surgery. One patient developed deep infection requiring washout and suppressive antibiotics. No patients required revision surgery. The median MSTS score at last follow up was 66%.
Conclusions
EPR of the distal tibia is a viable option and provides good function outcomes.
Keywords: Distal tibia, Primary, Osteosarcoma, Endoprosthetic replacement, Endoprosthesis
1. Introduction
Primary osteosarcomas of the tibia account for 20% of all osteosarcomas, with only 19% of these occurring in the distal tibia.1 Due to the subcutaneous nature of the distal tibia, as well as its close proximity to vital neurovascular and musculotendinous structures, adequate tumour excision with wide surgical margins can be difficult to achieve.2 Consequently, the traditional treatment offered to patients with malignant bone tumours of the distal tibia was amputation.3, 4, 5 However, with the subsequent development of new surgical techniques, modern imaging methods, and new chemotherapy regimens, limb salvage has become a more practical option compared to amputation for these patients.3 The various methods of limb salvage include free vascularised or non-vascularised fibula autograft with arthrodesis, osteo-articular allograft, and endoprosthetic replacement (EPR).6, 7, 8, 9 Although the long-term outcomes of EPR are currently unclear, it enables ankle motion preservation and earlier mobilisation, without significant risks of non-union and infection.6
We report the largest, single-centre retrospective study of clinical and functional outcomes in patients who underwent excision of distal tibia with subsequent EPR.
2. Patients and methods
Between 1977 and 2012, 508 patients were treated for aggressive malignant distal tibial bone tumour at our unit. Of these, eight consecutive patients (1.6%) underwent endoprosthetic replacement. There were four males and four females, with a median age of 33 years (range 14–76). There were four cases of osteosarcoma, one Ewings Sarcoma, one leiomyosarcoma, one giant cell tumour, and one dedifferentiated chondrosarcoma. Clinical data was retrospectively reviewed from all patients’ medical records and radiological imaging. Functional assessment was made according to the Musculoskeletal Tumour Society Functional Assessment Society (MSTS) criteria.2
All patients underwent diagnostic and staging studies including haematological and biochemical tests, plain x-rays and MRI scan of the lesion. Staging CT scan of the chest, abdomen, and pelvis, as well as whole body bone scan was also performed. The diagnosis was confirmed by needle biopsy or open biopsy in all cases.
2.1. Surgical technique
The prosthesis (Stanmore implants) consisted of a titanium tibial stem and shaft, as well as a chrome cobalt talar component which also had an ultra-high molecular weight polyethylene constituent.
A longitudinal incision was made lateral to the tibial crest, with skin flaps raised on medial and lateral sides deep to the deep fascia. Medial retraction of the anterior tibial vessels, deep peroneal nerve, and posterior tibial neurovascular bundle was performed. The tibia and interosseous membranes were subsequently divided approximately 5 cm proximal to the tumour site, enabling mobilisation and dissection of the lesion. The tumour was ideally excised completely en bloc with preservation of important tendons. The prosthesis was secured using methylmetacrylate bone cement after adequate preparation of the tibial medullary canal and the talus. A single suction drain was inserted before wound closure. Post-operative antibiotic prophylaxis consisted of 3 doses of intravenous cefuroxime in the earlier years, with Flucloxacillin used over the last 10 years. All patients were advised bed rest for 5 days in a Plaster of Paris backslab. They were subsequently allowed to mobilise non weightbearing for six weeks before their casts were removed, and gradual increased weightbearing was allowed. All patients were able to fully weight bear by three months following surgery (Fig. 1).
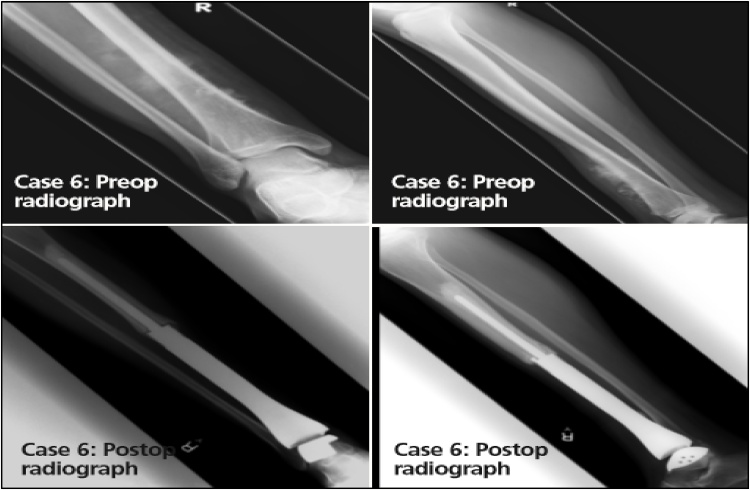
Fig. 1.
AP and lateral X-rays of right tibia and ankle of 14-year-old male with distal tibial osteosarcoma treated with excision and endoprosthetic reconstruction.
3. Results
The median follow-up for all cases was 77 months (range 13 to 276). Resection margins were clear in all eight patients, where only one was marginal. Two of eight patients (25%) died due to metastases at 10 and 41 months respectively following surgery. One patient (high grade osteosarcoma) already had lung metastases at presentation, and the other (Ewings sarcoma) had marginal resection margins. One patient developed local recurrence 6 months following resection of a dedifferentiated chondrosarcoma. This patient consequently underwent an above knee amputation, but later developed lung metastases 44 months following primary resection, leading to death.
All four patients (50%) who have survived the disease have not developed any recurrence or metastases following EPR. Two of these four patients have had high grade osteosarcomas, one had low grade osteosarcoma, and one had low grade leiomyosarcoma. All of these tumours were confined to the bone with minimal soft tissue extension. The median follow-up of patients who survived the disease was 120 months (range 72 to 276). The cumulative five and ten year survival was 63% and 42% respectively (95% CI: 37 to 100% and 16 to 100% respectively).
Significant complications developed in three of eight patients (37%). One patient developed a deep infection that required debridement, prolonged intravenous antibiotics, and implant retention. Another patient developed a superficial wound infection in the immediate post-operative period that resolved with oral antibiotics. The final patient developed aseptic loosening of the talar component 55 months post-surgery. This was evident on plain radiological imaging only, but no intervention was undertaken as he was asymptomatic. No patient has required surgical revision of their implants following EPR.
The median MSTS score at the last follow-up was 66% (50–90%) as shown in Table 1.
Table 1.
Details of clinical and functional outcomes of the eight patients included in the study.
| Case No. | Gender | Age | Diagnosis | Mets at Diagnosis | Follow-up (Months) |
Complications | MSTS (%) |
|---|---|---|---|---|---|---|---|
| 1 | F | 25 | Osteosarcoma | No | 44 | Deep infection Died from metastases |
50 |
| 2 | M | 40 | Osteosarcoma | No | 276 | Nil | 90 |
| 3 | F | 42 | Leiomyosarcoma | No | 262 | Asymptomatic loosening of talar component | 60 |
| 4 | F | 26 | Ewing’s sarcoma | No | 33 | Died from metastases | 67 |
| 5 | F | 46 | Giant Cell Tumour | No | 120 | Died from unrelated disease | 65 |
| 6 | M | 14 | Osteosarcoma | Yes (lung) | 82 | Superficial post-op infection | 87 |
| 7 | M | 19 | Osteosarcoma | No | 72 | Nil | 73 |
| 8 | M | 76 | Dedifferentiated Chondrosarcoma |
No | 13 | Local recurrence, later died from metastases | 50 |
4. Discussion
EPR offers an alternative method of management of aggressive distal tibial tumours to the traditional option of amputation. Although current literature suggests that amputation achieves the most reliable clinical and functional outcomes, it is associated with significant psychological and physical burdens.2, 9 Indeed, all patients in this study were initially offered amputation but refused. A number of studies have reported the most optimal functional outcomes and oncological results in patients treated with free vascularised or non-vascularised fibular autograft with arthrodesis, with mean MSTS between 75% and 80%.8, 10, 11 In comparison, however, EPR is less time-consuming to perform, and achieves better joint movement as well as a shorter recovery period.6
There have only been a small number of reports on the long-term outcomes of EPR so far as distal tibial tumours are extremely rare.6, 7, 9, 12, 13, 14 The medium and long term outcomes of these prostheses therefore still remain unclear. Of the 508 patients treated at our institute over a 30 year period for a malignant distal tibial lesion, only eight (1.6%) underwent EPR. This is still the largest study so far in the current literature describing clinical outcomes of EPR for distal tibial tumours. Table 2 compares the results of existing studies on EPR outcomes with those of our study. Evidently, we have one of the longest median follow-up periods of all studies, and we have shown a similarly low rate of local recurrence, infection, and amputation to existing studies.
Table 2.
Table compares published outcomes following distal tibial and ankle joint endoprosthetic replacement performed for bone tumours.
| Study | No. patients | Follow-up (yrs) | Local recurrence | Metastases | Wound infection | Amputation/Revision | Functional Outcome |
|---|---|---|---|---|---|---|---|
| Abudu et al. | 4 | 4.6 | 1 | 1 | 1 | 0 | 64% |
| Shekkeris et al. | 6 | 9.6 | 0 | 0 | 2 | 2 | 70% |
| Lee et al. | 6 | 5.3 | 0 | 0 | 1 | 0 | 80% (ISOLS) |
| Nataranjan et al. | 6 | 3.4 | 2 | 0 | 1 | 3 | 80% |
| Present study | 8 | 6.4 | 2 | 3 | 2 | 1 | 66% |
Our data reflects that patients with distal tibial bone tumour treated by wide resection and reconstruction with EPR do very well, provided that they do not develop local recurrence or metastases. This may be difficult to achieve in some cases due to the limitations of soft tissue cover, although the risks of disease recurrence may still be reduced by chemotherapy.12 Although marginal resection margins increase risks of metastases or local recurrence, our study enhances evidence that clear non-marginal resections can be achieved in the vast majority of patients undergoing EPR.7, 9 In our experience, patients with malignant tumours confined to bone with minimal soft-tissue extension, as well as those with benign-aggressive, or malignant lesions without metastases, should be considered for distal tibial EPR, as these lead to lower risks of local recurrence and improved survival. Abudu et al. has further documented that distal tibial tumours with extraosseous extension should also be considered for limb preserving surgery. However, involvement of major neurovascular bundles, the ankle joint, or main tendons of the foot, are contraindications to EPR.6
Our study further shows that patients who undergo EPR for Ewing’s sarcoma have worse prognosis than those with osteosarcoma. DTEPR has been used in only four cases of Ewing’s sarcoma in total according to the current literature so far. Local recurrence or metastases developed in three of these cases (75%), leading to death.6, 12 Contrarily, only 15% of the total 31 patients in current literature with distal tibial osteosarcomas who underwent EPR have had local recurrence or metastases following surgery.6, 12, 13, 18 This may be because in general, Ewing’s sarcoma has higher tendency to metastasise, compared to osteosarcoma.15, 16, 17 Patients with metastases at diagnoses are also unlikely to do well in the long-term, as supported by Lee et al. and Mavrogenis et al.9, 18 The one patient in our study with metastasis at diagnosis survived only 10 months following DTEPR. Evidently, limb salvaging does not alter the course of the initial malignancy and its tendency to metastasise.
In our experience, two patients developed wound infection following EPR. Although one patient required debridement and suppressive antibiotics, neither required revision surgery. There was only one case of mechanical failure in our study involving aseptic and asymptomatic loosening of talar component. This patient required regular close follow-up, but no further surgical intervention. Therefore, although EPR can have significant complications, these can be treated without having to result in need for further revision or amputation. Ultimately, function is adequate following EPR of the distal tibia and ankle, with median MSTS of 66%.
5. Conclusion
Many patients refuse amputation as treatment for their distal tibial tumour due to psychosocial reasons. With careful patient selection, EPR of the distal tibia is a viable alternative option, and provides good functional outcomes. We have demonstrated that the outcomes of EPR for distal tibial tumours are highly dependent on tumour histology, grade and stage of tumour, as well as resection margins. We believe that the complication rates overall are acceptable if amputation was to be the alternative option.
Conflict of interest
None.
References
- 1.Ottaviani G., Jaffe N. The epidemiology of osteosarcoma. Cancer Treat Res. 2009;152:3–13. doi: 10.1007/978-1-4419-0284-9_1. [DOI] [PubMed] [Google Scholar]
- 2.Enneking W.F., Spanier S.S., Goodman M.A. The surgical staging of musculoskeletal sarcoma. J Bone Joint Surg [Am] 1980;62:1027–1030. [PubMed] [Google Scholar]
- 3.Simon M.A., Aschiliman M.A., Thomas N., Mankin H.J. Limb-salvage treatment versus amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg [Am] 1986;68-A:1331–1337. [PubMed] [Google Scholar]
- 4.Bishop A.T., Wood M.B., Sheetz K.K. Arthrodesis of the ankle with a free vascularised autogenous bone graft: reconstruction of segmental loss of bone secondary to osteomyelitis, tumor or trauma. J Bone Joint Surg [Am] 1995;7-A:1867–1875. doi: 10.2106/00004623-199512000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Capanna R., van Horn J.R., Biagini R. Reconstruction after resection of the distal fibula for bone tumour. Acta Orthop Scand. 1986;57:290–294. doi: 10.3109/17453678608994394. [DOI] [PubMed] [Google Scholar]
- 6.Abudu A., Grimer R.J., Tillman R.M., Carter S.R. Endoprosthetic replacement of the distal tibia and ankle joint for aggressive bone tumours. Int Orthop. 1999;23:291–294. doi: 10.1007/s002640050374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Natarajan M.V., Annamalai K., Williams S., Selvaraj R., Rajagopal T.S. Limb salvage in distal tibial osteosarcoma using a custom mega prosthesis. Int Orthop. 2000;24:282–284. doi: 10.1007/s002640000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laitinen M., Hardes J., Ahrens H. Treatment of primary malignant bone tumours of the distal tibia. Int Orthop. 2005;29:255–259. doi: 10.1007/s00264-005-0656-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee S.H., Kim H.S., Park Y.B., Rhie T.Y., Lee H.K. Prosthetic reconstruction for tumours of the distal tibia and fibula. J Bone Joint Surg [Br] 1999;81-B:803–807. doi: 10.1302/0301-620x.81b5.9588. [DOI] [PubMed] [Google Scholar]
- 10.Bolton-Maggs B.G., Sudlow R.A., Freeman M.A. Total ankle arthroplasty: a long term review of the London Hospital experience. J Bone Joint Surg [Br] 1985;67:785–790. doi: 10.1302/0301-620X.67B5.4055882. 4. [DOI] [PubMed] [Google Scholar]
- 11.Casadei R., Ruggieri P., Giuseppe T., Biagini R., Mercuri M. Ankle resection arthrodesis in patients with bone tumours. Foot Ankle Int. 1994;15:242–249. doi: 10.1177/107110079401500503. [DOI] [PubMed] [Google Scholar]
- 12.Shekkeris A.S., Hanna S.A., Sewell M.D. Endoprosthetic reconstruction of the distal tibia and ankle joint after resection of primary bone tumours. J Bone Joint Surg Br. 2009;91:1378–1382. doi: 10.1302/0301-620X.91B10.22643. [DOI] [PubMed] [Google Scholar]
- 13.Natarajan M.V., Annamalai K., Williams S., Selvaraj R., Rajagopal T.S. Limb salvage in distal tibial osteosarcoma using a custom mega prosthesis. Int Orthop. 2000;24:282–284. doi: 10.1007/s002640000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zeytoonjian T., Mankin H.J., Gebhardt M.C., Hornicek F.J. Distal lower extremity sarcomas: frequency of occurrence and patient survival rate. Foot Ankle Int. 2004;25:325–330. doi: 10.1177/107110070402500509. [DOI] [PubMed] [Google Scholar]
- 15.O’Connor M.I., Pritchard D.J. Ewing’s sarcoma: prognostic factors, disease control, and the re-emerging role of surgical treatment. Clin Orthop Relat Res. 1991;262:78–87. [PubMed] [Google Scholar]
- 16.Shirley S.K., Askin F.B., Gilula L.A. Ewing’s sarcoma in bones of the hands and feet: a clinicopathologic study and review of the literature. J Clin Oncol. 1985;3:686–697. doi: 10.1200/JCO.1985.3.5.686. [DOI] [PubMed] [Google Scholar]
- 17.Bos G.D., Esther R.J., Scott Woll T. Foot tumours: diagnosis and treatment. J Am Acad Orthop Surg. 2002;10:259–270. doi: 10.5435/00124635-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Mavrogenis Andreas F., Abati Caterina Novella, Romagnoli Carlo, Ruggieri Pietro. Similar survival but better function for patients after limb salvage versus amputation for distal tibia osteosarcoma. Clin Orthop Relat Res. 2012;470:1735–1748. doi: 10.1007/s11999-011-2238-7. [DOI] [PMC free article] [PubMed] [Google Scholar]