Abstract
Introduction
Previous studies have shown that provider training and the tests performed play a role in the accuracy of diagnosis of anterior cruciate ligament (ACL) injuries. The specific aim of the current study is to determine the examiner proficiency and accuracy in performing the different proactive tests of ACL rupture before and after the induction of anesthesia prior to a definitive surgical procedure.
Materials and Methods
A case series was performed from January of 2015 through July of 2015. Two examiners were included (an experienced orthopaedic sports surgeon with more than 16 years in practice and an experienced orthopaedic physician assistant with 6 years of clinical experience in orthopaedic sports medicine). Three different physical examination tests were used before and after the induction of anesthesia to the patient: 1) Lachman test, 2) pivot shift test, and 3) Lelli test. Relevant patient demographic information such as BMI, thigh girth, and calf girth were recorded. Diagnosis of ACL rupture had been established pre-operatively.
Results
Thirty three patients met the inclusion criteria (males: 21 (64%), female: 12 (36%)). High percent of false negative was found with pivot shift test for both before and after anesthesia when compared to the other two tests. The Lelli test seemed to be most favorable to both the surgeon and the physician assistant with at least 67% favorable, while the pivot shift was least often felt to be the most useful test. No relationship was found for either patients’ thigh or patients’ calf girths with the physical examination test results for both examiners for any of the three tests (p = 0.110).
Conclusion
The diagnostic accuracy and limitations of the various tests for ACL injury need to be understood. Clinically, it is recommended performing at least two different examinations, as each test has its own specific limitations.
Level of Evidence: III- Prospective Cohort Study without blinding
Keywords: Lelli Test, Lachman Test, Pivot Shift Test, Arthroscopic Surgery, Anterior Cruciate Ligament
Introduction
Anterior cruciate ligament (ACL) injuries are common athletic injuries of the knee with an annual incidence of 68.6 per 100,000 person-years in the United States1. They largely occur in sports which require a sudden change of direction on a weight-bearing knee. Accurate diagnosis of ACL rupture relies on a combination of the patient’s history, a clinical examination, and by Magnetic Resonance Imaging (MRI) scanning and diagnostic arthroscopy if needed2,3. The initial presentation of ACL injuries often includes a history of non-contact injury and a hemorrhagic effusion4,5. The early diagnosis of an ACL injury is of importance as there is good evidence that a delay between ACL injury and reconstruction is associated with a higher risk of subsequent damage to the menisci, particularly the medial meniscus, and the articular cartilage6-18.
After ACL rupture, most patients have detectable signs and symptoms of excess knee laxity and instability19. There are several commonly used physical examination applied tests to determine an ACL injury such as the anterior drawer test, the Lachman test, the pivot shift test, and the Lelli test (“lever sign” test)20-23. It is, however, difficult to ascertain the benchmark for diagnostic accuracy following an ACL injury, and a significant percentage of subjects are misdiagnosed due to the limitations of each of these physical examination tests. Most of the literature has reported on the sensitivity, reliability, and specificity of these different physical examination tests to detect an ACL injury21-37, but most are reporting experienced surgeons performing the examination. There is limited data available in the literature on less-experienced physicians or surgeons or even physician assistants using these physical examination tests for the ACL lesion by their simplicity, reliability, and specificity. Geraets et al28 performed a study to assess the diagnostic value of ACL-specific medical history assessment and physical examination between primary and secondary care medical specialists, and found that a primary care physician was able to correctly identify 62% of chronic ACL injuries compared to 94% by an orthopaedic surgeon. This suggests that different providers with different training can have different interpretations with the same patients. The specific aim of the current study is to determine the examiner proficiency and accuracy in performing the different clinical diagnosis of ACL ruptures before and after the induction of anesthesia.
Patients and Methods
Institutional review board approval was obtained for the study and consent was obtained from the patients prior to enrollment in the study. A case series was performed looking at consecutive examiner’s proficiency and accuracy in performing the different clinical diagnosis of ACL ruptures before and after the induction of anesthesia from January 2015 through July 2016. The inclusion criteria for this study were patients who presented to the lead orthopedic surgeon with a unilateral knee injury that resulted in symptomatic instability at two selected facilities. There was no prior history of knee problems or injuries on the involved side, no prior ACL reconstruction or repair, the knee injury was not sustained within 72 hours prior to data collection, and there had been no surgical procedures on the involved knee in the six weeks prior to data collection.
The exclusion criteria for this study included all patients who presented with an ACL injury outside of the collection period, patients who had a previous knee surgery or infection on the affected side, patients presenting within 72 hours after injury, patients with chronic knee pain, patients with associated ligament injuries, and patients complaining of hip, ankle and foot symptoms.
Two examiners were included in this study: a sports medicine fellowship-trained orthopaedic surgeon with more than 16 years in practice and the other examiner was an orthopaedic physician assistant with 6 years of clinical experience in orthopaedic sports medicine. Three different physical examination tests (Figure 1) were used to evaluate for an ACL injury on both the affected and the non-affected extremities: 1) Lachman test, 2) pivot shift test, and 3) Lelli test. These tests were performed in the operating suite before and after the induction of anesthesia to the patient, and examinations were performed independently, without the other provider in the room and without discussing the results prior to recording the examination. All ACL injuries were confirmed arthroscopically.
Figure 1.
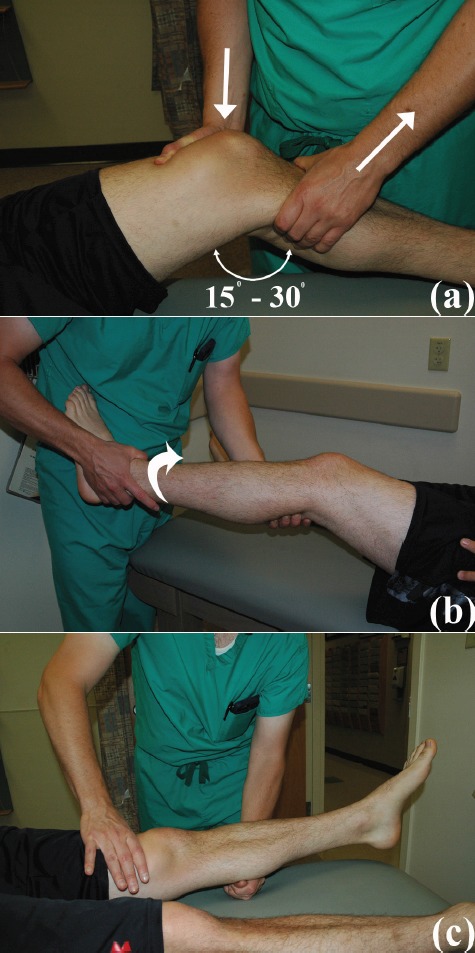
Physical Examination Test Performed. (a) Lachman Test, (b) Pivot Shift Test, and (c) Lelli Test
Lachman Test (Figure 1a)
The Lachman test was performed with the patient lying supine with the examiner on the side of the extremity to be examined. The knee was flexed between 15° and 30° while the heel remained on the table. The examiner placed one hand behind the tibia and with the other hand grasped the patient’s thigh. The examiner’s thumb was placed on the tibial tuberosity. With the femur thus stabilized, firm pressure was then applied to the posterior tibia in an attempt to translate it anteriorly. A positive test indicating disruption of the ACL is one in which there is proprioceptive and/or visual anterior translation of the tibia in relation to the femur with a characteristic “mushy” or “soft” end point. This is in contrast to the “hard” end point of an intact ACL36. The grades of laxity were defined by the amount of anterior tibial translation relative to contralateral knee: Grade I: 1-5mm; Grade II: 6-10mm; and Grade III: >10mm.
Pivot Shift Test (Figure 1b)
The pivot shift test was performed with the patient lying in the supine position. The leg was then picked up at the ankle with one of the examiner’s hands while the other hand was placed behind the fibula, over the lateral head of the gastrocnemius. The knee is initially flexed to 30° then slowly brought to full extension, with a slight valgus strain combined with 20° of internal rotation of the leg. The hand placed at the lateral portion of the leg at the level of the superior tibiofibular joint gives a strong valgus strain to prevent easy reduction of the tibia on the femur. If the tibia’s position on the femur reduces as the knee is flexed in the range of 30° to 40° or if there is an anterior subluxation felt during knee extension, the test is positive for instability.
Lelli Test (Figure 1c)
The Lelli test, or the lever sign test, was described by Lelli et al23. The patient was placed supine with the knee fully extended on a hard surface. The examiner placed a closed fist under the proximal third of the patient’s calf. The other hand of the examiner then applied a moderate downward force to the distal third of the quadriceps. An intact ACL allows the heel to lift off the examination table. Whereas an ACL deficient knee, the heel remain on the examination table.
Data Collection
The size of the examinees’ hand span from the tip of the thumb to the tip of the fifth digit (small finger) with the hand in maximal abduction was physically measured. The patient demographics including the patient’s age, gender, height, weight, body mass index (BMI), and side of injury were collected. The girth of the patient’s thigh and calf on the affected side (8cm above and below the midpoint of the patella) were also measured.
Statistical analysis
The independent sample t-test was performed using SPSS software (Version 19.0; SPSS Inc, Chicago, IL) and was used to determine if there were any observed differences between male and female with respect to patient demographics, thigh circumference and calf circumference. The level of significant difference was defined as p<0.05. The Kappa statistic using SPSS software (Version 19.0; SPSS Inc, Chicago, IL) was used to compare the inter- and intra-observer agreement for each of the three tests and for each provider. According to guidelines described by Landis and Koch38, a value of ≤0.2 indicates “poor” agreement, 0.21-0.40 is “fair” agreement, 0.41-0.60 is “moderate” agreement, 0.61-0.80 is “substantial” agreement, and >0.80 is “excellent” agreement. Sensitivity was calculated by dividing the number of true positives by the number of subjects with ACL injuries.
Results
Of the 33 patients that met the inclusion criteria, 21 patients (64%) were males and 12 patients (36%) were female. The mean age for the male and female groups were 30.9±14.3 years (range: 11-62 years) and 30.6±17.0 years (range: 15-60 years), respectively. The mean BMI for the male group (mean: 29.8±4.5 kg/m2; range: 20.6-36.9 kg/ m2) was statistically significantly higher than the female group (mean: 28.3±8.1 kg/m2; range: 19.9-45.3 kg/m2; p=0.024). Statistically, there was no significant difference detected between males and females in terms of thigh girth and calf girth (Table 1). Of the 33 patients with ACL injuries, 32 patients were found to have complete tears during diagnostic arthroscopy, and only one patient was found to have a partial tear with the anteromedial bundle intact and a torn posterolateral bundle.
Table 1.
Patient Demographics
| Male (N = 21) | Female (N = 12) | P value | |
|---|---|---|---|
| Age (Years) | 30.9 ± 14.3 (11 – 62) | 30.6 ± 17.0 (15 – 60) | 0.299 |
| Weight (kg) | 95.2 ± 19.5 (43.1 – 127.0) | 75.3 ± 19.8 (59.4 – 116.1) | 0.690 |
| Height (cm) | 178 ± 10 (145 - 193) | 163 ± 7 (150 - 175) | 0.247 |
| BMI (kg/m2) | 29.8 ± 4.5 (20.6 – 36.9) | 28.3 ± 8.1 (19.9 – 45.3) | 0.024 |
| Thigh girth (cm) | 45.0 ± 6.0 (35 - 58) | 43.7 ± 6.7 (35.1 – 60) | 0.918 |
| Calf girth (cm) | 35.8 ± 4.3 (30 - 51) | 37.8 ± 4.5 (31 - 46) | 0.888 |
For the experienced sports medicine orthopaedic surgeon, prior to the induction of anesthesia, there was 2 (6%) false negatives with notable during Lachman test, 24 (73%) false negative during pivot shift testing (22 (67%) were guarding reaction from the patient due to pain, and 2 (6%) were tested negative) and 4 (12%) false negatives during Lelli test (2 (6%) with a guarding reaction, and 2 (6%) were tested negative). On the other hand, there were no false positives with any of the three tests. The sensitivity of the Lachman test, pivot shift test, and Lelli test were 94%, 27%, and 88 %, respectively. With the patient under general anesthesia, there were no (0%) false negatives with Lachman test, 1 (3%) false negative with the pivot shift maneuver, and 1 (3%) false negative with the Lelli test (Figure 2). There were no false positives on the contralateral limb. The sensitivity of the Lachman test was then determined to be 100%, and 97% for both the pivot shift test and Lelli test.
Figure 2.
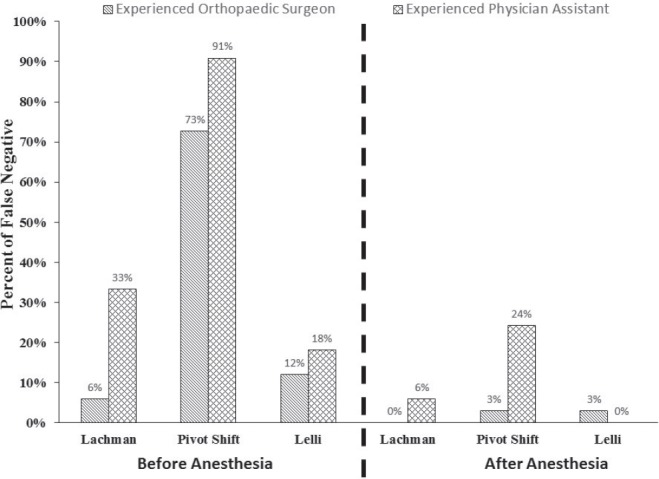
Validity For All Three Physical Examination ACL Tests Judgment of Negative Test
For the experienced orthopaedic physician assistant, prior to the induction of anesthesia, there were 11 (33%) false negatives with the Lachman test with guarding reaction noted in 10 (30%) patients, 30 (91%) false negatives with pivot shift testing with guarding reaction in 27 (82%) patients, and 6 (18%) false negatives with the Lelli test with guarding reaction in 2 (6%) patient. There were no false positives. The sensitivity for the Lachman test was 67%, for the pivot shift was 9%, and for the Lelli test was 82%. With the patient under general anesthesia, there were 2 (6%) false negatives with the Lachman test, 8 (24%) false negatives with the pivot shift with guarding in 1 (3%) patient, and no false negatives with the Lelli test (Figure 2). There were no false positives. The sensitivity for the Lachman test, pivot shift test and Lelli test was 94%, 76%, and 100%, respectively.
Inter-observer reliability testing prior to the induction of anesthesia for all the three tests showed “fair” agreement by using the guidelines described by Landis and Koch38. The Kappa coefficient for inter-observer agreement of judgments of positive or negative for the two examiners when using Lachman test was 0.23 with 72% agreement, when using pivot shift test was 0.23 with 76% agreement, and when using the Lelli test was 0.30 with 82% agreement. The inter-observer reliability with the patient under general anesthesia for the pivot shift test demonstrated “poor” agreement with the Kappa coefficient of 0.18 with 79% agreement. Unfortunately, the intra-observer value could not be computed for the Lachman test because there were no false negatives detected by the experienced surgeon,but there was 94% agreement. Similarly,the intra-observer value could not be calculated for the Lelli test because there were no false negatives for the experienced orthopaedic physician assistant but there was 97% agreement between the two observers (Table 2).
Table 2.
Inter-observer reliability for judgments based on all three different physical examination tests to determine an ACL injury
| Before Anesthesia | After Anesthesia | |||
|---|---|---|---|---|
| Kappa coefficient | Percent of agreement | Kappa coefficient | Percent of agreement | |
| Lachman test | 0.23 | 73 | N/A | 94 |
| Pivot shift test | 0.23 | 76 | 0.18 | 79 |
| Lelli test | 0.30 | 82 | N/A | 97 |
Intra-examiner reliability was calculated by comparing test results before and after the induction of anesthesia for each provider. Each of the three tests showed “poor” agreement except Lachman test for experienced physician assistant using the guidelines described by Landis and Koch38. For the experienced orthopaedic surgeon, the intra-observer Kappa value was 0.02 with 30% agreement for the pivot shift test,was 0.05 with 85% agreement for the Lelli test, and was not calculable for the Lachman test due to the lack of false negatives. For the experienced physician assistant, the Kappa coefficient for intra-observer agreement when using the Lachman test was 0.23 with 73% agreement,when using pivot shift test the Kappa value was 0.06 with 33% agreement,and when using Lelli test the Kappa value was not be able to computed as the physician assistant had no false negative results with the patient under anesthesia (Table 3).
Table 3.
Intra-examination test reliability for judgments based on before or after anesthesia
| Experienced Orthopaedic Surgeon | Experienced Physician Assistant | |||
|---|---|---|---|---|
| Kappa coefficient | Percent of agreement | Kappa coefficient | Percent of agreement | |
| Lachman test | N/A | 94 | 0.23 | 73 |
| Pivot shift test | 0.02 | 30 | 0.06 | 33 |
| Lelli test | 0.05 | 85 | N/A | 67 |
The Lelli test seemed to be most favorable to both the surgeon and the physician assistant with at least 67% favorable, while the pivot shift was least often felt to be the most useful test (Figure 3). The experienced surgeon felt the Lachman test was the most beneficial to detect injury in 42% of patients,while the experienced physician assistant only thought it was most beneficial in 18% of patients.
Figure 3.
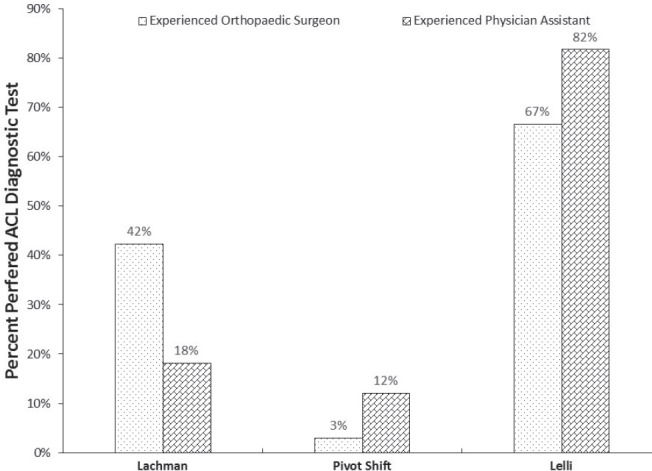
Examiners Preferred ACL Diagnostic Test
The hand span for the experienced orthopaedic surgeon and the experienced physician assistant was measured 21.5cm and 15.5cm,respectively (Table 4). The physician assistant stated that hand size was likely a factor in 2 false negative results while performing the Lelli test. No relationship was found for either patients’ thigh or patients’ calf girths with the physical examination test results for both examiners for any of the three tests (p=0.110).
Table 4.
Examiner Hand Span Size
| Left (cm) | Right (cm) | |
|---|---|---|
| Orthopaedic Surgeon | 21.5 | 21.5 |
| Experienced Physician Assistant | 15.5 | 15.5 |
Discussion
Despite the advent of MRI and its high sensitivity39, physical examination continues to play a major role in ACL diagnosis. In our study,we observed that all three physical examination tests (Lachman test,Pivot Shift test,and Lelli test) to determine an ACL injury have at least a trend towards increased false negative test results prior to the induction of anesthesia. This is consistent with previous studies that demonstrated that physical examination tests are more accurate with the patient under anesthesia25,30,40,41. Despite the increased sensitivity of the Lachman test compared to the pivot shift test and anterior drawer test in the literature, no single test has been consistently shown to detect all ACL injuries33,35,42. Scholten et al35 performed a meta-analysis of the physical diagnostic tests for ACL injuries and reported sensitivities of 62% and 86% for the anterior drawer test and Lachman test respectively, and between 18% and 48% for the pivot shift test. The sensitivity of the Lachman test, however, has been reported from other studies to range from 80% to 99%, with a specificity of 95%25,29-32,36,43. In meta-analyses, the sensitivity of the Lachman test is 0.85—0.871 with a specificity of 0.91—0.97, and the pivot shift had a sensitivity of 0.24—0.49 with a specificity of 0.98333542. Wagemaker et al37 assessed the diagnostic accuracy of a clinical history and physical examination in a primary care setting and found that a typical history for ACL injury combined with a positive anterior drawer test had a positive predictive value of between 36% and 80%.
To date, no physical exam maneuver has eliminated false negative test results. Guarding—the protective muscle action of the hamstrings secondary to joint pain—may be responsible for false negatives in some settings36. Others believe that some of these tests are not easily performed by examiners who have small hands or on patients with a large thigh girth or large calf girth26,44. In our study, even though the experienced physician assistant’s hand span was considered small (15.5cm),only reported 2 false negatives (6%) out of the 33 patients that may be due to small hand size.
The findings from our study further demonstrate that the Lelli test may be another useful physical examination maneuver for both physicians and physician assistants. The sensitivity for the Lelli test in our patient population was not significantly different from the Lachman test, and had fewer overall false negatives when combining the data for the providers. However,this test hold little value in distinguishing between partial and complete tears as this test is a binary test (positive or negative result)23. Both the Lachman test and pivot shift test are based on a grading system that measures the amount of translation of the tibia relative to the femur, and these tests undoubtedly continue to hold an important role in diagnosis of ACL injuries45.
Even though in our study both examiners preferred the Lelli test to diagnose ACL injuries in most patients, both examiners observed that soft cushions on the examination table can cause false negative results. Furthermore, if the examiner has a small fist size, or if the patient has a large, soft calf, this may have the potential to cause a false negative.
Several questions and limitations can be raised concerning the validity of our study and the applicability of these results to determine the examiner proficiency and accuracy in performing the different clinical diagnosis of ACL ruptures at clinic. We recognize that our study was performed with a relatively small number of patients, which decreased the chance of finding statistically significant results due to a low power. In addition, in this study we excluded patients who underwent examination within 72 hours of injury, which not only led to decreased enrollment but also prevents us from commenting on the usefulness of the Lelli test when guarding is likely most severe. The lack of blinding of the clinicians to the injury extremity was also another potential area of bias and may be responsible for the lack of any false positive test results in the study. Another weakness is the prevalence of male patients in the study, which may limit generalizability. Further expansion of the study to include more patients and more examiners is planned as future research.
Conclusion
A properly performed physical examination of the knee still holds a pivotal role in the diagnosis of ACL injury. The diagnostic accuracy and limitations of the various tests for ACL injury need to be understood. Clinically, in cases of suspicion of ACL injury, it is recommended performing at least two different physical examinations, as each test has its own specific limitations. The implementation of an acute ACL injury clinic may help minimize delays to surgery, which should result in better patient outcomes.
Acknowledgement
The authors wish to thank Dr. George Lucas for his assistance, revision, and critical comments on the paper.
References
- 1.Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, Stuart MJ, Krych AJ. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am J Sports Med. 2016 Feb 26 doi: 10.1177/0363546516629944. PMID: 26920430. [DOI] [PubMed] [Google Scholar]
- 2.Lee JK, Yao L, Phelps CT, Wirth CR, Czajka J, Lozman J. Anterior cruciate ligament tears: MR imaging compared with arthroscopy and clinical tests. Radiology. 1988 Mar;166(3):861–4. doi: 10.1148/radiology.166.3.3340785. PMID:3340785. [DOI] [PubMed] [Google Scholar]
- 3.Mink JH, Levy T, Crues JV., 3rd Tears of the anterior cruciate ligament and menisci of the knee: MR imaging evaluation. Radiology. 1988 Jun;167(3):769–74. doi: 10.1148/radiology.167.3.3363138. PMID:3363138. [DOI] [PubMed] [Google Scholar]
- 4.Bollen SR, Scott BW. Rupture of the anterior cruciate ligament--a quiet epidemic? Injury. 1996 Jul;27(6):407–9. doi: 10.1016/0020-1383(96)00033-2. PMID: 8881137. [DOI] [PubMed] [Google Scholar]
- 5.Noyes FR, Mooar PA, Matthews DS, Butler DL. The symptomatic anterior cruciate-deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983 Feb;65(2):154–62. doi: 10.2106/00004623-198365020-00003. PMID: 6687391. [DOI] [PubMed] [Google Scholar]
- 6.Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015 Feb;43(2):275–81. doi: 10.1177/0363546514559912. PMID: 25497145. [DOI] [PubMed] [Google Scholar]
- 7.Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, Dubrana F. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee. 2009 Aug;16(4):239–44. doi: 10.1016/j.knee.2008.11.004. PMID: 19097796. [DOI] [PubMed] [Google Scholar]
- 8.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007 Oct;35(10):1756–69. doi: 10.1177/0363546507307396. PMID: 17761605. [DOI] [PubMed] [Google Scholar]
- 9.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009 Jul;37(7):1434–43. doi: 10.1177/0363546509338827. PMID: 19567666. [DOI] [PubMed] [Google Scholar]
- 10.Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010 Nov;38(11):2201–10. doi: 10.1177/0363546510373876. PMID: 20713644. [DOI] [PubMed] [Google Scholar]
- 11.Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC. Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med. 2010 Mar;38(3):455–63. doi: 10.1177/0363546509350914. PMID: 20051501. [DOI] [PubMed] [Google Scholar]
- 12.Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA. Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999 Jan;358:188–93. PMID: 9973991. [PubMed] [Google Scholar]
- 13.Yüksel HY, Erkan S, Uzun M. The evaluation of intraarticular lesions accompanying ACL ruptures in military personnel who elected not to restrict their daily activities: the effect of age and time from injury. Knee Surg Sports Traumatol Arthrosc. 2006 Nov;14(11):1139–47. doi: 10.1007/s00167-006-0170-2. PMID: 169270. [DOI] [PubMed] [Google Scholar]
- 14.Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005 Dec;87(12):1639–42. doi: 10.1302/0301-620X.87B12.16916. PMID: 16326877. [DOI] [PubMed] [Google Scholar]
- 15.Chhadia AM, Inacio MC, Maletis GB, Csintalan RP, Davis BR, Funahashi TT. Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med. 2011 Sep;39(9):1894–9. doi: 10.1177/0363546511410380. PMID: 21705649. [DOI] [PubMed] [Google Scholar]
- 16.Granan LP, Bahr R, Lie SA, Engebretsen L. Timing of anterior cruciate ligament reconstructive surgery and risk of cartilage lesions and meniscal tears: a cohort study based on the Norwegian National Knee Ligament Registry. Am J Sports Med. 2009 May;37(5):955–61. doi: 10.1177/0363546508330136. PMID: 19251674. [DOI] [PubMed] [Google Scholar]
- 17.Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002 Nov-Dec;18(9):955–9. doi: 10.1053/jars.2002.36114. PMID: 12426537. [DOI] [PubMed] [Google Scholar]
- 18.Arastu MH, Grange S, Twyman R. Prevalence and consequences of delayed diagnosis of anterior cruciate ligament ruptures. Knee Surg Sports Traumatol Arthrosc. 2015 Apr;23(4):1201–5. doi: 10.1007/s00167-014-2947-z. PMID: 24671385. [DOI] [PubMed] [Google Scholar]
- 19.Shelbourne KD. The art of the knee examination: where has it gone? J Bone Joint Surg Am. 2010 Aug 4;92(9):e9. doi: 10.2106/JBJS.I.01691. PMID: 20686055. [DOI] [PubMed] [Google Scholar]
- 20.Solomon DH, Simel DL, Bates DW, Katz JN, Schaffer JL. The rational clinical examination. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA. 2001 Oct 3;286(13):1610–20. doi: 10.1001/jama.286.13.1610. PMID: 11585485. [DOI] [PubMed] [Google Scholar]
- 21.Makhmalbaf H, Moradi A, Ganji S, Omidi-Kashani F. Accuracy of lachman and anterior drawer tests for anterior cruciate ligament injuries. Arch Bone Jt Surg. 2013 Dec;1(2):94–7. PMID: 25207297. [PMC free article] [PubMed] [Google Scholar]
- 22.Thapa SS, Lamichhane AP, Mahara DP. Accuracy of Lelli Test For Anterior Cruciate Ligament Tear. Journal of Institute of Medicine. 2015 Aug;37(2):91–94. [Google Scholar]
- 23.Lelli A, Di Turi RP, Spenciner DB, Dòmini M. The “Lever sign”: a new clinical test for the diagnosis of anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2014 Dec 25 doi: 10.1007/s00167-014-3490-7. PMID: 25536951. [DOI] [PubMed] [Google Scholar]
- 24.Cooperman JM, Riddle DL, Rothstein JM. Reliability and validity of judgments of the integrity of the anterior cruciate ligament of the knee using the Lachman’s test. Phys Ther. 1990 Apr;70(4):225–33. doi: 10.1093/ptj/70.4.225. PMID:2315385. [DOI] [PubMed] [Google Scholar]
- 25.Donaldson WF, 3rd, Warren RF, Wickiewicz T. A comparison of acute anterior cruciate ligament examinations. Initial versus examination under anesthesia. Am J Sports Med. 1985 Jan-Feb;13(1):5–10. doi: 10.1177/036354658501300102. PMID:3976980. [DOI] [PubMed] [Google Scholar]
- 26.Draper DO, Schulthies SS. Examiner proficiency in performing the anterior drawer and Lachman tests. J Orthop Sports Phys Ther. 1995 Dec;22(6):263–6. doi: 10.2519/jospt.1995.22.6.263. PMID:8580954. [DOI] [PubMed] [Google Scholar]
- 27.Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980 Mar-Apr;147:45–50. PMID:7371314. [PubMed] [Google Scholar]
- 28.Geraets SE, Meuffels DE, van Meer BL, Breedveldt Boer HP, Bierma-Zeinstra SM, Reijman M. Diagnostic value of medical history and physical examination of anterior cruciate ligament injury: comparison between primary care physician and orthopaedic surgeon. Knee Surg Sports Traumatol Arthrosc. 2015 Apr;23(4):968–74. doi: 10.1007/s00167-013-2769-4. PMID: 25964958. [DOI] [PubMed] [Google Scholar]
- 29.Jonsson T, Althoff B, Peterson L, Renström P. Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparative study of the Lachman test and the anterior drawer sign. Am J Sports Med. 1982 Mar-Apr;10(2):100–2. doi: 10.1177/036354658201000207. PMID:7081521. [DOI] [PubMed] [Google Scholar]
- 30.Katz JW, Fingeroth RJ. The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries. Am J Sports Med. 1986 Jan-Feb;14(1):88–91. doi: 10.1177/036354658601400115. PMID:3752353. [DOI] [PubMed] [Google Scholar]
- 31.Kim SJ, Kim HK. Reliability of the anterior drawer test, the pivot shift test, and the Lachman test. Clin Orthop Relat Res. 1995 Aug;317:237–42. PMID:7671485. [PubMed] [Google Scholar]
- 32.Mitsou A, Vallianatos P. Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparison between the Lachman test and the anterior drawer sign. Injury. 1988 Nov;19(6):427–8. doi: 10.1016/0020-1383(88)90139-8. PMID:3267651. [DOI] [PubMed] [Google Scholar]
- 33.Ostrowski JA. Accuracy of 3 diagnostic tests for anterior cruciate ligament tears. J Athl Train. 2006 Jan-Mar;41(1):120–1. PMID: 16619105. [PMC free article] [PubMed] [Google Scholar]
- 34.Parwaiz H, Teo AQ, Servant C. Anterior cruciate ligament injury: A persistently difficult diagnosis. Knee. 2016 Jan;23(1):116–20. doi: 10.1016/j.knee.2015.09.016. PMID: 26552783. [DOI] [PubMed] [Google Scholar]
- 35.Scholten RJ, Opstelten W, van der Plas CG, Bijl D, Deville WL, Bouter LM. Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: a meta-analysis. J Fam Pract. 2003 Sep;52(9):689–94. PMID: 12967539. [PubMed] [Google Scholar]
- 36.Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976 Mar-Apr;4(2):84–93. doi: 10.1177/036354657600400206. PMID:961972. [DOI] [PubMed] [Google Scholar]
- 37.Wagemakers HP, Luijsterburg PA, Boks SS, Heintjes EM, Berger MY, Verhaar JA, Koes BW, Bierma-Zeinstra SM. Diagnostic accuracy of history taking and physical examination for assessing anterior cruciate ligament lesions of the knee in primary care. Arch Phys Med Rehabil. 2010 Sep;91(9):1452–9. doi: 10.1016/j.apmr.2010.06.012. PMID: 20801267. [DOI] [PubMed] [Google Scholar]
- 38.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. PMID: 843571. [PubMed] [Google Scholar]
- 39.Fischer SP, Fox JM, Del Pizzo W, Friedman MJ, Snyder SJ, Ferkel RD. Accuracy of diagnoses from magnetic resonance imaging of the knee. A multi-center analysis of one thousand and fourteen patients. J Bone Joint Surg Am. 1991 Jan;73(1):2–10. PMID: 1985991. [PubMed] [Google Scholar]
- 40.Lucie RS, Wiedel JD, Messner DG. The acute pivot shift: clinical correlation. Am J Sports Med. 1984 May-Jun;12(3):189–91. doi: 10.1177/036354658401200303. PMID:6742299. [DOI] [PubMed] [Google Scholar]
- 41.Deveci A, Cankaya D, Yilmaz S, Özdemir G, Arslantaş E, Bozkurt M. The arthroscopical and radiological corelation of lever sign test for the diagnosis of anterior cruciate ligament rupture. Springerplus. 2015 Dec 30;4:830. doi: 10.1186/s40064-015-1628-9. PMID: 26753117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang W, Zhang Y, Yao Z, Ma L. Clinical examination of anterior cruciate ligament rupture: a systematic review and meta-analysis. Acta Orthop Traumatol Turc. 2016;50(1):22–31. doi: 10.3944/AOTT.2016.14.0283. PMID: 26854045. [DOI] [PubMed] [Google Scholar]
- 43.DeHaven KE. Arthroscopy in the diagnosis and management of the anterior cruciate ligament deficient knee. Clin Orthop Relat Res. 1983 Jan-Feb;172:52–6. PMID:6822005. [PubMed] [Google Scholar]
- 44.Draper DO, Schulthies S. A test for eliminating false positive anterior cruciate ligament injury diagnoses. J Athl Train. 1993 Winter;28(4):355–7. PMID:16558252. [PMC free article] [PubMed] [Google Scholar]
- 45.Dejour D, Ntagiopoulos PG, Saggin PR, Panisset JC. The diagnostic value of clinical tests, magnetic resonance imaging, and instrumented laxity in the differentiation of complete versus partial anterior cruciate ligament tears. Arthroscopy. 2013 Mar;29(3):491–9. doi: 10.1016/j.arthro.2012.10.013. PMID: 23343713. [DOI] [PubMed] [Google Scholar]


