Abstract
Introduction:
Conventional two-dimensional (2D) laparoscopy systems have the drawback of poor depth perception and spatial orientation. Three-dimensional (3D) laparoscopic systems have stereoscopic vision in which depth perception is achieved by different unique images received by each eye. We evaluated 3D laparoscopy in comparison with conventional 2D laparoscopy in urological procedures in a prospective randomized study.
Materials and Methods:
Over a 19 month study period, 108 patients scheduled to undergo various urological procedures were randomized to either conventional 2D or 3D laparoscopy (2D n = 53; 3D n = 55). A single senior surgeon performed all the surgeries. Parameters such as total operative time, dissection and suturing time, blood loss, hospital stay, complications (Clavien-Dindo), and visual analog scale (VAS) score for pain were assessed. The subjective assessment of the operating surgeon of superiority and inferiority of either technology on parameters defining surgical skills was recorded using a Likert scale.
Results:
The total operative time (P < 0.0003), blood loss (P < 0.028), dissection, suturing and stenting time (P < 0.0001), and the State-Trait Anxiety Inventory for Adults score (P < 0.0001) was significantly in favor of 3D laparoscopy.
Conclusion:
Our study showed significant advantages of the 3D system over 2D laparoscopy. These advantages include enhanced operative performance and greater surgeon comfort.
INTRODUCTION
Laparoscopic procedures have been proven to be safe, less morbid, and very effective for various urological procedures. The main drawbacks of two-dimensional (2D) laparoscopy are a steep learning curve, lack of depth perception, and spatial orientation. To overcome these drawbacks, three-dimensional (3D) laparoscopic systems have been developed with stereoscopic vision, in which depth perception is achieved by combining different unique images received by each eye.
The first 3D systems became available for clinical use in the 1990s. Initially, surgeons were uncomfortable with the 3D system due to heavy active shutter glasses, poor quality image, and strain related to the view mode.[1] Advancement in 3D technology have made 3D vision more comfortable and acceptable. Comparative assessment of new generation 3D versus conventional 2D laparoscopy remains limited in clinical urology and only a few studies address this in the field of general surgery.[2,3] Literature regarding experience with 3D in comparison with 2D laparoscopic procedures in urology is scarce. We therefore evaluated 3D laparoscopy in comparison with conventional 2D laparoscopy in urological procedures.
MATERIALS AND METHODS
Study design
A prospective, randomized, comparative study was performed in our institution from January 2014 to July 2015. Totally, 111 patients were assessed for surgery. and 108 patients scheduled for commonly performed urological surgeries (simple nephrectomy, radical nephrectomy, and pyeloplasty) were randomized by block randomization method into two groups: 2D laparoscopy (n = 53) and 3D laparoscopy (n = 55). Three patients were excluded as they refused consent [Figure 1]. All patients provide informed, written consent and the study was cleared by the Ethics Committee. Of the 53 patients selected for 2D laparoscopy, 19 patients underwent laparoscopic pyeloplasty, 26 patients underwent laparoscopic simple nephrectomy, and eight patients underwent laparoscopic radical nephrectomy. In the group allotted for the 3D system (55 patients), laparoscopic pyeloplasty was performed in 21 patients, laparoscopic simple nephrectomy in 28 patients and laparoscopic radical nephrectomy in six patients.
Figure 1.
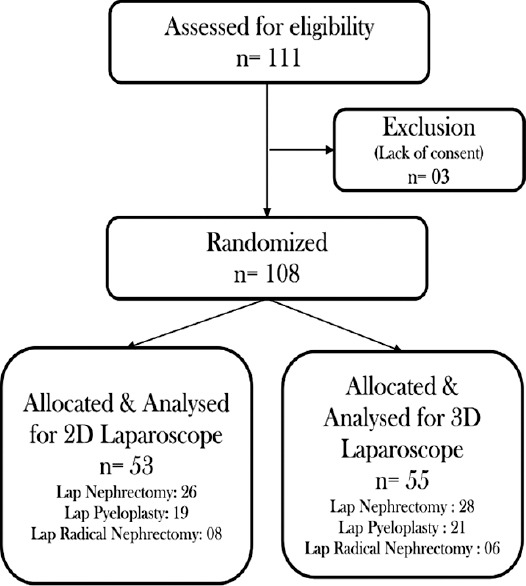
CONSORT flow diagram of study
A single senior surgeon with more than 17 years of experience in laparoscopic surgery in a tertiary health-care center performed all the surgeries. 2D laparoscopy was performed using Maxer 3 Chip HD system, and 3D laparoscopy using a Covidien Viking 3D HD vision system.
Parameters such as total operative time, blood loss during surgery, hospital stay, complications (Clavien-Dindo classification), and visual analog scale (VAS) score for pain were assessed. The surgeon's subjective assessment of image quality, depth perception, operative strain, ease of intra-corporeal suturing, and knotting, and hand–eye coordination was recorded using a Likert scale. The State-Trait Anxiety Inventory for Adults (STAI-6) Short Version of Spielberger et al.[4] was used to quantify emotional, physical, and cognitive aspects of stress experienced during each operative procedure. STAI is an introspective psychological inventory comprising a total of forty self-reporting items pertaining to anxiety affect and helps to measure anxiety at both poles of normal affect curve (state vs. trait). Short six-item STAI-6 scale was chosen as it is well validated and more suitable when time constraints prevent administration of longer version (forty-item). Total STAI score ranges between six (minimum) and 24 (maximum), with the higher scores indicating increased psychological stress experienced during the procedure. This method was used to measure the overall stress experienced by the operating surgeon during the procedure.
Subgroup analysis of time taken for critical surgical steps during the procedure was performed as follows: (a) for laparoscopic nephrectomy (simple and radical) – time taken for dissection of vascular pedicle, clipping of vessels, and cutting of vascular pedicle; (b) for laparoscopic pyeloplasty – time taken for dissection of ureteropelvic junction, the creation of anastomotic flaps, suturing, and stenting.
Statistical analysis was performed using the Student's t-test (GraphPad Analysis software, Inc. 2015, San Diego, California, USA).
RESULTS
Clinical parameters such as age, sex, surgery sides, and comorbidities showed no statistical significance between both groups. The total operative time was 150.19 min (2D) vs 111.18 min (3D) (P < 0.0003), blood loss was 203.21ml vs 149.64 ml (P < 0.028), dissection, suturing and stenting time was 68.58 min vs 46.11 min (P < 0.0001), and STAI score was 16.91 vs 13.33 (P < 0.0001). These parameters were significantly superior in the 3D system group compared with 2D. Posteoperative VAS score, hospital stay, and complications were similar between the two groups.
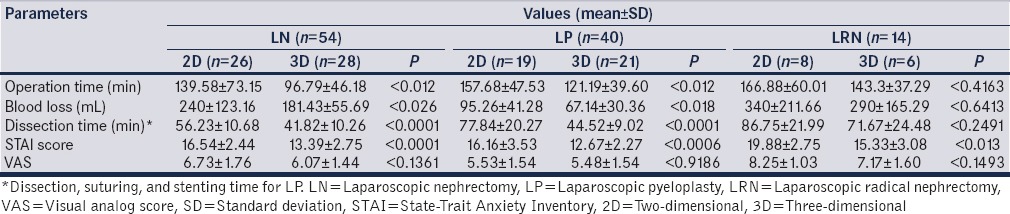
Data for individual procedures are given in Table 1, For simple nephrectomy, operative time (P < 0.012), blood loss (P < 0.026), dissection of pedicle (P < 0.0001), and STAI score (P < 0.0001) were statistically better for 3D system whereas VAS score (P < 0.1361) was similar. Laparoscopic pyeloplasty also showed similar results. For laparoscopic radical nephrectomy, only surgeon comfort was significantly better in 3D laparoscopy group with STAI score (P < 0.013), whereas other parameters such as VAS score (P < 0.1493), operative time (P < 0.4163), blood loss (P < 0.6413), and dissection of pedicle (P < 0.2491) did not show any difference between both groups.
Table 1.
Comparison between two- and three-dimensional
DISCUSSION
The conventional laparoscopic camera includes a 2D system, and although high-definition systems have improved the graphics, there is a lack of depth and spatial perception. This leads to increased learning curve as there is a need to interpret the secondary spatial cues such as shadow and motion parallax. 3D systems eliminate the need to overcome the loss of stereoscopic vision and thus improve laparoscopic skills. The stereoscopic vision in 3D laparoscopic systems is achieved by combining two separate images received by both eyes separately, thus overcoming the disadvantages rendered by the 2D system.
Surgeons can work faster and safer under 3D vision, especially during crucial and complicated surgical maneuvers during the procedure.[5] The initial study carried out by searching Cochrane database by Gurusamy et al.[6] and other studies[7] conducted for laparoscopic cholecystectomy failed to show any superiority of 3D system over 2D at that point of time due to primitive 3D systems. As the technology changed from heavy active shutter glasses to light polarizing glasses, several groups have described the subjective advantages of added depth perception, improved resolution, and easier manipulation during surgery.[8,9] Even though, 3D systems have improved a lot in terms of better ergonomics when compared to their predecessors, they are still plagued by certain shortcomings such as eye fatigue, motion blur and the need for special equipment increasing the cost involved in it. Although these limitations cannot be neglected, there is hope that with further advancement in technology, these things will be resolved.
Studies[2,10] have shown clear advantages of the 3D system in those who are in training, rather than in surgeons who have already obtained proficiency in advanced laparoscopic procedures, the reasons being improved co-ordination, spatial awareness, and timing in comparison to the traditional 2D imaging. 3D laparoscopy can reduce the time needed to learn laparoscopy and hence will be beneficial for the training of junior residents. Romero-Loera et al.[11] reported a comparative study including only newcomers who have no experience in laparoscopy and concluded that 3D is superior than 2D with the higher percentages of tasks completion, less time in performing them, and a shorter learning curve involved in 3D.
All procedures in our study were performed by a senior surgeon who had extensive experience in laparoscopic surgery. Experienced endoscopic surgeons may not always need 3D system as they can use shadow or movement parallax as depth cue instead of stereovision. However, studies carried out by Ohuchida et al.[12] and Cicione et al.[10] have, respectively, suggested that 3D system may contribute in reducing surgical accidents and could facilitate hand versatility in surgeon with preexisting laparoscopic skills. The latter prospective observational study involving standardized tasks in dry laboratory setting concluded that 3D imaging facilitated performance of Urological surgeons, mainly the beginners.[10]
Blood loss when compared to 2D was less in 3D due to better dissection and identification of vascular structures. Even control of bleeders was better for 3D due to better depth perception leading to prompt identification of bleeders. Due to clear vision, good depth perception, and proper hand–eye coordination, critical steps during surgery like dissection of renal pedicle and structure identification was much better with 3D systems when compared to 2D. During suture placement, tissue edge holding, needle direction, and suture picking were more precise and easier in 3D system due to better depth perception and good hand–eye coordination. This was, especially, appreciated during tissue approximation and suture placement for pyeloplasty wound closure. All these factors when taken together, account for reduced time taken for 3D laparoscopy when compared to conventional 2D laparoscopy.
3D systems at present are more expensive than 2D systems; however the advantages, they provide when compared to 2D makes them attractive. The 3D systems try to bridge the huge gap between 2D and robotics by providing certain advantages of robotic surgery at lower cost. The present 3D laparoscopic systems can be compared to robotic surgical systems in terms of good depth perception, reduced stress to surgeons along with advantages of being more cost-effective and ease of mobility.[1] Bhayani and Andriole[13] have expressed that it is unclear whether the robotic system offers any advantages over a smaller and less expensive 3D system. Although wristed instruments might seem to be a technological advance with an existing 3D view, it might be possible for surgeons to become proficient over an equally short learning curve. The cost savings for such proficiency, however, are overwhelmingly in favor of a 3D non-robotic tower, which costs less than one-tenth the price of a surgical robot. In addition, the nonrobotic tower is more mobile and might be used for any laparoscopic procedure. Park et al.[14] reported a comparative study between 2D, 3D, and robotic systems involving beginners and senior surgeons in the field of laparoscopy and concluded that robot was helpful in beginners, whereas experienced surgeons performed the task equally good in all the systems, even faster in 3D laparoscopy when compared to robot.
The likely shortcomings of our study may be counted as lack of blinding during data recording and the study being underpowered with less number of patients involved. Further, the, study was carried out for only three regularly done simple laparoscopic urologic procedures which were performed by single-experienced surgeon only and did not involve novice surgeons for comparison. Our results need to be confirmed with an adequately powered study and more complex procedures.
CONCLUSION
The use of 3D systems in laparoscopic urologic procedures resulted in shorter operative time, lower blood loss, and better surgeon performance with lower stress than with 2D systems. These systems may offer to fill the gap between 2D laparoscopy and robot assistance.
Footnotes
Financial support and sponsorship: Nil.
Conflicts of interest: There are no conflicts of interest.
REFERENCES
- 1.Izquiedo L, Peri L, Garcia-Cruz E, Musquera M, Ciudin A, Perez M, et al. 3D advances in laparoscopic vision. Eur Urol Rev. 2012;7:137–9. [Google Scholar]
- 2.Honeck P, Wendt-Nordahl G, Rassweiler J, Knoll T. Three-dimensional laparoscopic imaging improves surgical performance on standardized ex-vivo laparoscopic tasks. J Endourol. 2012;26:1085–8. doi: 10.1089/end.2011.0670. [DOI] [PubMed] [Google Scholar]
- 3.Tanagho YS, Andriole GL, Paradis AG, Madison KM, Sandhu GS, Varela JE, et al. 2D versus 3D visualization: Impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparoendosc Adv Surg Tech A. 2012;22:865–70. doi: 10.1089/lap.2012.0220. [DOI] [PubMed] [Google Scholar]
- 4.Spielberger CD, Gorssuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 5.van Bergen P, Kunert W, Bessell J, Buess GF. Comparative study of two-dimensional and three-dimensional vision systems for minimally invasive surgery. Surg Endosc. 1998;12:948–54. doi: 10.1007/s004649900754. [DOI] [PubMed] [Google Scholar]
- 6.Gurusamy KS, Sahay S, Davidson BR. Three dimensional versus two dimensional imaging for laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2011 Jan;19(1):CD006882. doi: 10.1002/14651858.CD006882.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Hanna GB, Shimi SM, Cuschieri A. Randomised study of influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet. 1998;351:248–51. doi: 10.1016/S0140-6736(97)08005-7. [DOI] [PubMed] [Google Scholar]
- 8.Pietrabissa A, Scarcello E, Carobbi A, Mosca F. Three-dimensional versus two-dimensional video system for the trained endoscopic surgeon and the beginner. Endosc Surg Allied Technol. 1994;2:315–7. [PubMed] [Google Scholar]
- 9.Yoshida T, Inoue H, Hara E, Umezawa A, Ohtsuka K, Endo S, et al. Newly developed 3D endoscopic system: Preliminary experience. Endoscopy. 2003;35:181–4. doi: 10.1055/s-2003-37015. [DOI] [PubMed] [Google Scholar]
- 10.Cicione A, Autorino R, Breda A, De Sio M, Damiano R, Fusco F, et al. Three-dimensional vs. standard laparoscopy: Comparative assessment using a validated program for laparoscopic urologic skills. Urology. 2013;82:1444–50. doi: 10.1016/j.urology.2013.07.047. [DOI] [PubMed] [Google Scholar]
- 11.Romero-Loera S, Cárdenas-Lailson LE, de la Concha-Bermejillo F, Crisanto-Campos BA, Valenzuela-Salazar C, Moreno-Portillo M. Skills comparison using a 2D vs. 3D laparoscopic simulator. Obes Surg. 2015;25:2120–4. doi: 10.1016/j.circir.2015.06.032. [DOI] [PubMed] [Google Scholar]
- 12.Ohuchida K, Kenmotsu H, Yamamoto A, Sawada K, Hayami T, Morooka K, et al. The effect of CyberDome, a novel 3-dimensional dome-shaped display system, on laparoscopic procedures. Int J Comput Assist Radiol Surg. 2009;4:125–32. doi: 10.1007/s11548-009-0282-5. [DOI] [PubMed] [Google Scholar]
- 13.Bhayani SB, Andriole GL. Three-dimensional (3D) vision: Does it improve laparoscopic skills? An assessment of a 3D head-mounted visualization system. Rev Urol. 2005;7:211–4. [PMC free article] [PubMed] [Google Scholar]
- 14.Park YS, Oo AM, Son SY, Shin DJ, Jung do H, et al. Is a robotic system really better than the three-dimensional laparoscopic system in terms of suturing performance? comparison among operators with different levels of experience. Surg Endosc. 2016;30:1485–90. doi: 10.1007/s00464-015-4357-9. [DOI] [PubMed] [Google Scholar]


