Abstract
Aim:
The aim of this study is to analyze the postoperative visual outcomes of fibrin glue-assisted, suture-less posterior chamber (PC) intraocular lens (IOL) implantation technique in eyes with inadequate capsule support at a tertiary eye care hospital in South India.
Setting and Design:
This is a retrospective, nonrandomized case series.
Patients and Methods:
This study analyzes 94 eyes which underwent PC-IOL implantation by fibrin glue-assisted, suture-less technique. All patients who had IOL implants by the fibrin glue-assisted PC-IOL technique from August 2009 to January 2014 were included in the study. Intra- and post-operative complications were analyzed. The postoperative best spectacle-corrected visual acuity (BSCVA) was evaluated and recorded at the end of 6 months.
Statistical Analysis:
The data were analyzed using SPSS version 16.1 (SPSS Inc., Chicago, Illinois, USA) using two sample paired t-test and independent t-test.
Results:
A total of 94 eyes of 92 patients that underwent glued IOL implantation over a period of 5 years were analyzed. Out of 94 eyes, 77 eyes (84.6%) maintained or improved on their preoperative BSCVA (P = 0.012).
Conclusion:
We conclude that glued IOL implantation is a feasible option in rehabilitating patients with aphakia without adequate capsular support.
Keywords: Fibrin glue, glued intraocular lens, inadequate capsular support
Intraocular lens (IOL) insertion after cataract surgery is one of the most frequently performed surgical procedures.[1,2] IOL implantation in eyes that lack posterior capsular support is problematic not only due to intraoperative problems but also due to complications seen postoperatively.[3] IOL implantation was achieved in the past by the following techniques[4] - iris-fixated IOL,[5,6] anterior chamber (AC) IOL,[5,6] sutured and suture-less transscleral-fixated IOL.[7] The limitations associated with sutured scleral-fixated IOL include tilting and decentration of the sutured posterior chamber (PC) IOL,[8,9] suture-induced inflammation, degradation, and delayed IOL subluxation.
A new procedure, the glued intrascleral fixation technique, was introduced in 2007.[10] This technique helps to implant a PC-IOL in eyes with a deficient posterior capsule using a quick-acting surgical fibrin sealant derived from human blood plasma.[11,12] This technique reduces the risk of suture-related complications in addition to increasing the speed and ease of surgery.[3] Suture-less intrascleral PC-IOLs have also been reported like y-fixation technique wherein the scleral flap is closed using a suture.[13,14,15]
In our current study, conducted at a tertiary eye care center in South India, the scleral flaps, and the conjunctiva were sealed using fibrin glue eliminating the need for sutures and its related complications in eyes with inadequate capsule support.
Patients and Methods
This study is a retrospective, nonrandomized case analysis of patients who underwent glued IOL implantation from August 2009 to February 2014. Case records of all patients who underwent glued IOL implantation were analyzed. The mean follow-up period for patients was 2 years. The male:female ratio of patients was 45:49. The age range of the patients was 13–90 years with a mean age of 58 years.
Indications for surgery were recorded as primary or secondary based on the implantation of the glued IOL as a primary or secondary procedure. Patients who had glued IOL implantation as a secondary procedure were further grouped into two based on whether the glued IOL was done as a single procedure after the primary surgery or whether combined with or preceded by other surgeries.
Group 1: Glued IOL implantation as a primary procedure.
Group 2: Glued IOL implantation as a secondary procedure which is further grouped into two:
Only glued IOL implantation after the primary procedure
Glued IOL implantation preceded by or combined with other procedures.
The study was approved by the Institutional Ethics Committee consisting of a nine-member team. All patients included in the study had undergone a complete ophthalmic evaluation, which included detailed history, preoperative visual acuity, intraocular pressure (IOP), keratometry, slit lamp, and fundus evaluation. IOL power was calculated by keratometry and A-scan under aphakic mode with SRK-T formula and an A-constant of 118.4.
Fibrin glue used in the procedure was Tisseel fibrin kit (Baxter AG, A-1220 Vienna, Industriestrasse 67, Austria). Tisseel lyophilized powder was mixed with aprotinin solution to prepare Tisseel solution. Thrombin lyophilized 500 containing thrombin 500 IU was mixed with calcium chloride solution to obtain thrombin solution. Reconstituted Tisseel solution and thrombin are then placed in the Fibrinotherm (machine provided by Baxter) to obtain the optimum viscosity and temperature before the solutions being loaded into two 1-ml sterile syringes and mounted onto the applicator for use.
All cases of glued IOL implantation were performed by a single surgeon under local anesthesia with assistance from the vitreoretinal surgeon in patients where retinal surgery was a requirement. Conjunctival peritomy was performed 180° apart. Two partial thickness flaps 2.5 mm × 2.5 mm exactly 180° diagonally apart were created. A 23-gauge infusion cannula was introduced at 3.5 mm from the limbus through the pars plana. AC maintainer was employed in few patients. Two sclerotomies were made 1.5 mm from the limbus with a 22-gauge needle/myringotomy knife under the scleral flaps. A scleral pocket/tunnel to hold the haptic was made at the edge of the partial thickness scleral flap with a 26-gauge needle [Fig. 1a]. A sclera-corneal tunnel incision for inserting a rigid IOL or a clear corneal tunnel for a foldable IOL was then made. Anterior vitrectomy with the help of triamcinolone acetonide for better visualization of the vitreous was done to remove any vitreous strands in the AC and in the pupillary area. Thereafter, the IOL was introduced through the limbal incision by means of a McPherson's forceps for a rigid IOL or an injector for a foldable IOL. An end gripping, 23-guage micro rhexis forceps (MicroSurgical Technology, Redmond, Washington, USA) was introduced through one of the sclerotomies to hold the leading haptic, which was then externalized under the partial thickness scleral flap [Fig. 1b]. Through the second sclerotomy, the trailing haptic was also externalized using a second 23-guage micro rhexis forceps after ensuring proper centering of the IOL. The two haptics were then tucked into the transscleral pockets/scleral tunnels [Fig. 2a]. Minimal anterior vitrectomy was done near the sclerotomies to prevent vitreous incarceration.
Figure 1.
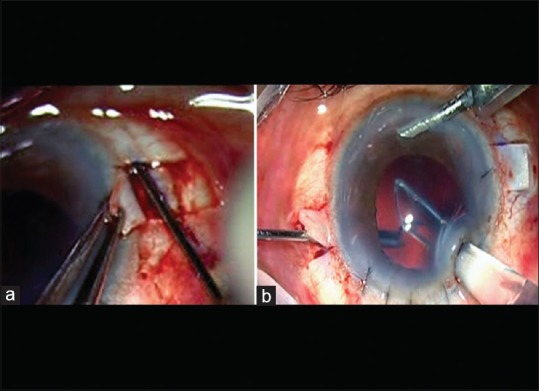
(a) Creation of scleral pocket under the scleral flap (b) leading haptic grasped with MST forceps
Figure 2.
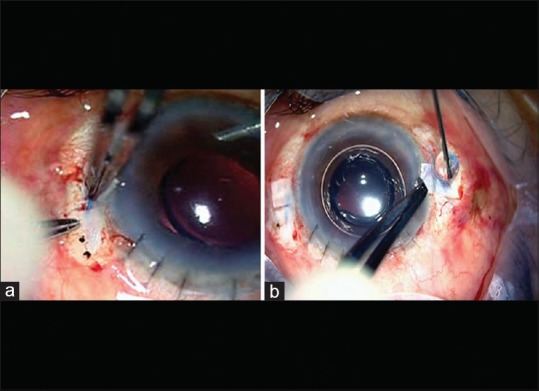
(a) Haptic tucked into scleral pocket (b) fibrin glue applied on scleral flap
The reconstituted fibrin glue was injected through the double syringe delivery system under the two scleral flaps which were sealed [Fig. 2b]. Minimal pressure was applied to the flaps for around 10–20 s until the fibrin polypeptides formed. The scleral flaps were thus closed with fibrin glue. Peritomy was also closed with fibrin glue. Patients who had a rigid IOL implanted had the limbal incisions closed with 10-0 nylon interrupted sutures. IOL used was either a rigid (PMMA-Aurolab) or a foldable acrylic (Alcon MA60 or Sensar), which are multipiece IOLs with optic diameter of 6.0 mm and modified “C” loop haptic design. There was no difficulty in performing either of procedure, and outcomes of both procedures were not affected. Intraoperative complications were noted if any. Antibiotic drops were administered to patients for 1 week, and steroid drops for 6 weeks in a tapering schedule. Postoperatively, the patients were followed up on day 1 (slit lamp examination and IOP assessment only) and later at 1 week, 1 and 6 months best spectacle-corrected visual acuity (BSCVA), IOP, slit lamp, and fundus examination were performed. Only BSCVA was measured by means of Snellen's visual acuity charts.
Data were entered in a Microsoft Excel spreadsheet (Microsoft Corp, Redmond, Washington, USA) and analyzed using SPSS version 16.1 (SPSS Inc., Chicago, Illinois, USA) using two sample paired t-test and independent t-test. P < 0.05 was considered statistically significant. Snellen's visual acuity was converted to logMAR scale for statistical analysis.
Results
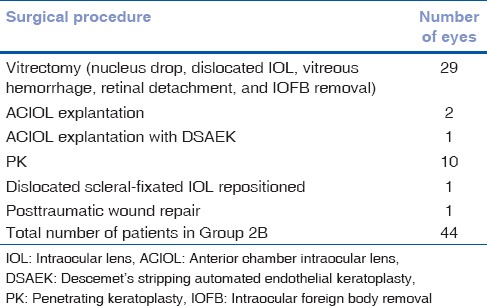
The total number of glued IOL implantations evaluated in the study was 94 (92 patients). Out of the 92 patients evaluated, the surgical procedure was performed in both the eyes in two patients. Glued IOL implantation was performed as a primary procedure along with lensectomy or phacoemulsification in seven eyes. It was performed as a secondary procedure in 87 eyes. Among the 87 eyes, 43 eyes received glued IOLs as a single procedure after the primary procedure while 44 eyes had complicated procedures [Table 1] either preceding the glued IOL implantation or in combination with the glued IOL implantation. The age range of the patients was from 13 to 90 years with a mean age being 58 years. The average duration between the primary surgery and the glued IOL implantation was 3 months.
Table 1.
Eyes receiving intraocular lens as a complicated procedure
Rigid IOLs were implanted in 32 eyes, and foldable IOLs were implanted in 62 eyes. The preoperative BSCVA ranged from 6/6 to < 6/60 in many patients [Fig. 3]. Intraoperative complications encountered were a broken haptic, ciliary body bleeding, and uveal exposure following a deep scleral flap.
Figure 3.
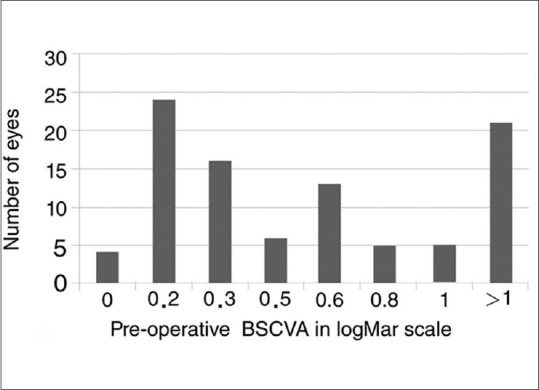
Preoperative (best spectacle-corrected visual acuity in logMar scale)
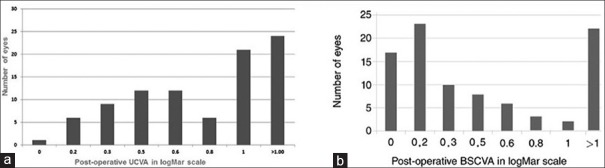
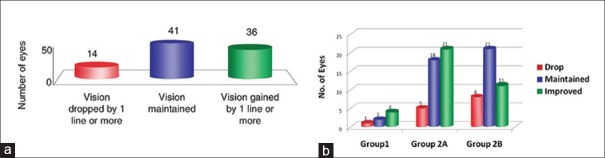
The postoperative uncorrected visual acuity (UCVA) is shown [Fig. 4a]. The postoperative BSCVA showed a statistically significant improvement (P = 0.012) with 77 eyes maintaining or improving on their preoperative BSCVA as shown [Fig. 4b]. Three eyes were lost during follow-up and were excluded from the study. Comparing the pre- and post-operative BSCVA using logMAR, 41 eyes maintained their preoperative visual acuity, 36 eyes improved, 14 Patients had drop in vision by 1 line or more [Fig. 5a]. Analysis of pre- and post-operative BSCVA between the three groups demonstrates that patients in Groups 1 and 2a achieved greater gains in visual acuity than patients in Group 2b [Fig. 5b].
Figure 4.
(a) Postoperative uncorrected visual acuity (uncorrected visual acuity in logMar scale) (b) postoperative best spectacle-corrected visual acuity (best spectacle-corrected visual acuity in logMar scale)
Figure 5.
(a) Postoperative gain or loss of lines (b) comparison between preoperative best spectacle-corrected visual acuity and postoperative best spectacle-corrected visual acuity between the three groups
Implantation of glued IOLs was stable in most of the eyes. Although IOL tilt was noted in three eyes on slit lamp examination, (no specific method of measurement of IOL tilt was done) visual acuity dropped in only one compared to the preoperative visual acuity. Glued IOL removal had to be done in two eyes where the IOL dislocated. Out of these two, one eye had recurrent dislocation of PC-IOL before the glued IOL implantation; the patient had a larger white-to-white horizontal diameter. The IOL used in this case was a Sensar acrylic IOL by AMO, the overall diameter was smaller than MA60AT Alcon lenses, so this resulted in dislocation at later date and subsequently underwent AC-IOL implantation. In the second case, glued IOL dislocation resulted from trauma associated with retinal detachment. Two eyes that were implanted went in for pseudophakic bullous keratopathy due to traumatic primary surgery and multiple surgeries preceding glued IOL implantation. Graft decompensation, secondary to rejection, was noted in two eyes.
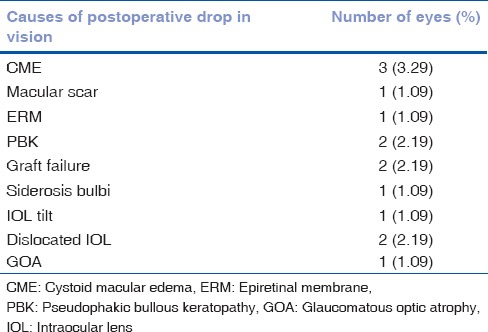
Postoperative increase in intraocular pressure was noted in four eyes, of which one required trabeculectomy, two eyes required cyclodiode, and one developed glaucomatous optic atrophy. Siderosis bulbi developed in one of the eyes, in which lensectomy along with vitrectomy, and intraocular foreign body removal was done during the primary procedure. Fundus examination revealed cystoid macular edema (CME) in three eyes and epiretinal membrane (ERM) in one eye that had uneventful glued IOL surgery but which had undergone multiple complicated surgeries such as vitrectomy/silicone oil removal (SOR), nucleus removal, and IOL removal. The causes for postoperative drop in vision are shown in [Table 2]. Dispersed vitreous hemorrhage, not affecting visual acuity secondary to minimal bleeding during insertion of the micro vitreo retinal (MVR) blade/forceps, was also seen in four eyes.
Table 2.
Causes of postoperative drop in vision
Discussion
Different techniques have been developed for IOL implantation in the absence of capsular support such as PC-IOL and AC-IOL, but each has their own set of limitations. A study published by the American Academy of Ophthalmology comparing AC-IOLs, iris-fixated, and sclera-fixated IOLs showed that they were comparable in all the aspects.[16,17]
Agarwal et al. in 2008 were the first to describe glued IOL implantation. In this technique, a single-piece nonfoldable IOL was used. This procedure has undergone numerous modifications and advances since then.
The advantages associated with glued IOL implantation are the short learning curve, absence of suture-related complications, ability to fix the IOL in aphakic eyes as well as under any complex situations such as subluxated cataract, dislocated IOL, AC-IOL with corneal decompensation and postvitrectomy, and SOR,.[12] In this technique, the PC-IOL was fixated without suture to the sclera by inserting the haptics into the sclera pockets. The sclera and conjunctival flaps were sealed with the fibrin glue eliminating the need for sutures, and no special instrumentation was required apart from a microforceps.
This study was conducted with the purpose of evaluating the safety and effectiveness of this relatively new procedure. The primary factor analyzed in our study was the improvement in BCVA after the surgery, measured with Snellen visual acuity chart and converted into LogMar units. Eighty-four percent (84.6%) maintained or improved BCVA which compares well with the study done by Kumar et al.[12] In their retrospective analysis of 735 eyes, there was a significant improvement in the UCVA and BCVA of 486 patients with rigid IOLs (paired t-test P = 0.000) with the mean postoperative UCVA and BCVA being 0.19 ± 0.19 and 0.38 ± 0.27, respectively. In 191 patients with foldable IOLs, the mean postoperative BCVA and UCVA were 0.39 ± 0.29 and 0.22 ± 0.23, respectively.
About 15.38% of eyes implanted in our study lost BCVA due to comorbid conditions such as corneal decomposition, ERM, and CME, which were not directly related to the glued IOL surgery, but worsened over the postoperative period. These patients lost lines due to the extremely complicated surgeries done before glued IOL.
The best results in our series were seen in patients who had undergone glued IOL implantation as a primary procedure along with patients who were uncomplicated aphakes following a phacoemulsification or extracapsular cataract extraction.
Less favorable results were obtained in patients who had multiple surgeries or had complicated prior surgeries with resultant compromised corneas, vitreous in the AC, CME, and ERMs. The need for adequate protection of the cornea with viscoelastics and a thorough wound toileting cannot be more emphasized in the presence of complications during cataract surgery.
In our study, three eyes exhibited IOL tilt, and two showed dropped IOL (5.4%). This was comparable to the study published by Agarwal et al. where the decentration rate was 5.6%.[18] IOL tilt was observed in eyes with horizontal white-to-white diameter >12 mm, resulting in stretching of the haptic and dislocation from the scleral pocket due to the movement of the eye. Therefore, in all the surgeries, it is mandatory to measure the horizontal white-to-white distance. Eyes with the white-to-white distance beyond 12 mm are best fixated vertically. In patients with conjunctival scarring and large horizontal corneal diameter, a vertical placement of the IOL was done with ease. Another finding from our study is that eyes that had dislocation and tilt had been implanted with the Sensar acrylic IOL, which has a shorter overall diameter and smaller haptic.
There was no precipitation of glaucoma after the glued IOL surgery in any of the patients, which clearly demonstrates that the procedure did not compromise the angles. However, in patients with preexisting glaucoma, aggressive treatment was necessary.
Glued IOL implantation can be combined with other procedures such as penetrating keratoplasty (PK), Descemet's stripping automated endothelial keratoplasty (DSAEK), Descemet's membrane endothelial keratoplasty, iridoplasty, vitrectomy, and trabeculectomy.[18] In our study, twenty eyes had glued IOL implantation combined with other procedures such as PK, DSAEK, lensectomy, and vitrectomy. The implantation procedure was performed with ease even in these combined surgeries. Patients with large dislocation of lens, such as traumatic dislocation, Marfan's syndrome did very well with a combined primary procedure of lensectomy with glued IOL.
There was no major sight-threatening complication such as retinal detachment or endophthalmitis noted during the study. We also did not have scleral problems or extrusion of the haptics through the scleral pockets. The patients who developed corneal decompensation depicted low endothelial counts to begin with due to traumatic surgeries done before glued IOL.
Limitation of the study is that there is no comparison with other methods of IOL implantation such as Iris claw and sutured sclera-fixated IOL's.
Conclusion
Glued IOL implantation is an excellent surgical procedure for implantation of IOL in the absence of capsular support. The technique is completely suture-less in both securing the haptic and sealing the sclera flaps and conjunctiva. The excellent approximation allows sealing of the sclerotomy without leakage ensuring prevention of wound-related complications and endophthalmitis. In addition, it is possible to combine it with other techniques where suturing is not essential. The technique has a short learning curve and requires minimal instrumentation. Glued IOL implantation is a relatively new procedure with published reports from handful of institution. This study provides information from our institution.
Ethics approval
Ethics Committee approval for analysis of the patients case records who underwent glued IOL surgery was obtained from the Institutional Ethics Committee. The research adhered to the tenets of the Declaration of Helsinki.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Woodcock M, Shah S, Smith RJ. Recent advances in customising cataract surgery. BMJ. 2004;328:92–6. doi: 10.1136/bmj.328.7431.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leung TG, Lindsley K, Kuo IC. Types of intraocular lenses for cataract surgery in eyes with uveitis. Cochrane Database Syst Rev. 2014:CD007284. doi: 10.1002/14651858.CD007284.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Narang P, Narang S. Glue-assisted intrascleral fixation of posterior chamber intraocular lens. Indian J Ophthalmol. 2013;61:163–7. doi: 10.4103/0301-4738.112160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Por YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv Ophthalmol. 2005;50:429–62. doi: 10.1016/j.survophthal.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 5.Donaldson KE, Gorscak JJ, Budenz DL, Feuer WJ, Benz MS, Forster RK. Anterior chamber and sutured posterior chamber intraocular lenses in eyes with poor capsular support. J Cataract Refract Surg. 2005;31:903–9. doi: 10.1016/j.jcrs.2004.10.061. [DOI] [PubMed] [Google Scholar]
- 6.Holt DG, Young J, Stagg B, Ambati BK. Anterior chamber intraocular lens, sutured posterior chamber intraocular lens, or glued intraocular lens: Where do we stand? Curr Opin Ophthalmol. 2012;23:62–7. doi: 10.1097/ICU.0b013e32834cd5e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parekh P, Green WR, Stark WJ, Akpek EK. Subluxation of suture-fixated posterior chamber intraocular lenses a clinicopathologic study. Ophthalmology. 2007;114:232–7. doi: 10.1016/j.ophtha.2006.10.037. [DOI] [PubMed] [Google Scholar]
- 8.Hayashi K, Hayashi H, Nakao F, Hayashi F. Intraocular lens tilt and decentration, anterior chamber depth, and refractive error after trans-scleral suture fixation surgery. Ophthalmology. 1999;106:878–82. doi: 10.1016/S0161-6420(99)00504-7. [DOI] [PubMed] [Google Scholar]
- 9.Moawad AI, Ghanem AA. One-haptic fixation of posterior chamber intraocular lenses without scleral flaps. J Ophthalmol. 2012;2012:891839. doi: 10.1155/2012/891839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34:1433–8. doi: 10.1016/j.jcrs.2008.04.040. [DOI] [PubMed] [Google Scholar]
- 11.Price MO, Price FW, Jr, Werner L, Berlie C, Mamalis N. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 2005;31:1320–6. doi: 10.1016/j.jcrs.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 12.Kumar DA, Agarwal A, Agarwal A, Prakash G, Jacob S. Glued intraocular lens implantation for eyes with defective capsules: A retrospective analysis of anatomical and functional outcome. Saudi J Ophthalmol. 2011;25:245–54. doi: 10.1016/j.sjopt.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ohta T, Toshida H, Murakami A. Simplified and safe method of sutureless intrascleral posterior chamber intraocular lens fixation: Y-fixation technique. J Cataract Refract Surg. 2014;40:2–7. doi: 10.1016/j.jcrs.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 14.Rodríguez-Agirretxe I, Acera-Osa A, Ubeda-Erviti M. Needle-guided intrascleral fixation of posterior chamber intraocular lens for aphakia correction. J Cataract Refract Surg. 2009;35:2051–3. doi: 10.1016/j.jcrs.2009.06.044. [DOI] [PubMed] [Google Scholar]
- 15.Yamane S, Inoue M, Arakawa A, Kadonosono K. Sutureless 27-gauge needle-guided intrascleral intraocular lens implantation with lamellar scleral dissection. Ophthalmology. 2014;121:61–6. doi: 10.1016/j.ophtha.2013.08.043. [DOI] [PubMed] [Google Scholar]
- 16.Bellucci R, Pucci V, Morselli S, Bonomi L. Secondary implantation of angle-supported anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 1996;22:247–52. doi: 10.1016/s0886-3350(96)80227-6. [DOI] [PubMed] [Google Scholar]
- 17.Wagoner MD, Cox TA, Ariyasu RG, Jacobs DS, Karp CL American academy of ophthalmology. Intraocular lens implantation in the absence of capsular support: A report by the American academy of ophthalmology. Ophthalmology. 2003;110:840–59. doi: 10.1016/s0161-6420(02)02000-6. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal A, Prakash G, Jacob S, Saravanan Y, Kumar DA. Glued posterior chamber IOL in eyes with deficient capsular support retrospective analysis of 1-year post-operative outcomes. Eye. 2010;24:1143–8. doi: 10.1038/eye.2010.10. [DOI] [PubMed] [Google Scholar]