Abstract
We report a case of exogenous lipoid pneumonia from chronic, extranasal use of petrolatum ointment (Vicks VapoRub in this case) for nasal decongestion in a young woman, presenting with cough, dyspnea and fever. Exogenous Lipoid pneumonia is a rare condition, underdiagnosed and is more prevalent in adults. Usually asymptomatic and diagnosed while evaluating predisposed patients who become clinically unstable or an abnormal lung shadow or during evaluation of rhinobronchial allergy. It is rarely reported from chronic use of petrolatum ointment extranasally and was diagnosed by transbronchial biopsy in the present case. She was found, retrospectively, to have been using petrolatum ointment, as an extranasal application since more than a year at bedtime. She didn't give history of using any other oil-based nasal topical vasoconstrictor preparations for sinusitis. Our patient was managed with discontinuation of further use of the petrolatum ointment and treatment with prednisolone apart from her regular treatment for chronic rhinobronchial allergy. Patient is stable without any further radiological deterioration during follow-up of one year.
Keywords: Exogenous lipoid pneumonia, Petrolatum ointment, Transbronchial lung biopsy, Prednisolone, Treatment
1. Introduction
Exogenous lipoid pneumonia (ELP) is an uncommon clinical condition, usually underdiagnosed in adults, and often results from either aspiration or inhalation of mineral or vegetable oils. Rarely, it was reported from chronic use of petroleum jelly, applied intranasally or extranasally as a decongestant. ELP was initially described by Laughlen in 1925 and can be either chronic from long term ingestion or inhalation of oily products or acute from accidental aspiration [1], [2]. The exact incidence was not known but reported as from 1 to 2.5% in an autopsy series [3]. In a retrospective study, it was noted in 34 patients (77%) from oil aspiration or inhalation and in 25% of the cases there is no discernible predisposing cause [2]. We report here a young patient suffering from chronic rhinobronchial allergy who was diagnosed as having ELP from chronic use of a petrolatum ointment, extranasally at bed time and successfully treated with prednisolone and discontinuance of usage of the same ointment. Previously reported cases were mostly from intranasal application of petroleum jelly and this case report emphasizes the fact that it can also be caused from the common practice of applying this product around the nose, externally [4].
2. Case report
23-year-old female, who was having history suggestive of chronic rhino bronchial allergy for the past five years, attended pulmonology outpatient with the complaint of cough, dyspnea and fever since more than four weeks. Vital signs were within normal range with SpO2 of 96%; her physical examination revealed bibasal lung crackles. Her past medical history revealed treatment with inhaled corticosteroids and fluticasone nasal spray on an irregular basis during exacerbations. She complains of recurrent headaches and underwent septoplasty with submucosal diathermy three years ago. Her routine blood work was within normal range with no peripheral eosinophilia and no sputum eosinophilia; her total serum IgE level was 731 ng/ml; her spirometry revealed mild restrictive ventilatory defect. Serum 25 hydroxy vitamin D3 was 9.12 ng/ml; chest radiograph showing bilateral infiltrates prompted for a computed tomography scan of chest (HRCT- Chest). The latter revealed multiple small well defined and ill-defined centrilobular nodules in both lungs, significantly in the left inferior lingula and in the basal segments of left lower lobe. The lesions show areas of tree-in-bud appearance and areas of confluence. Few small scattered centrilobular nodules were seen in the right lung in all the lobes (Fig. 1, Fig. 2).
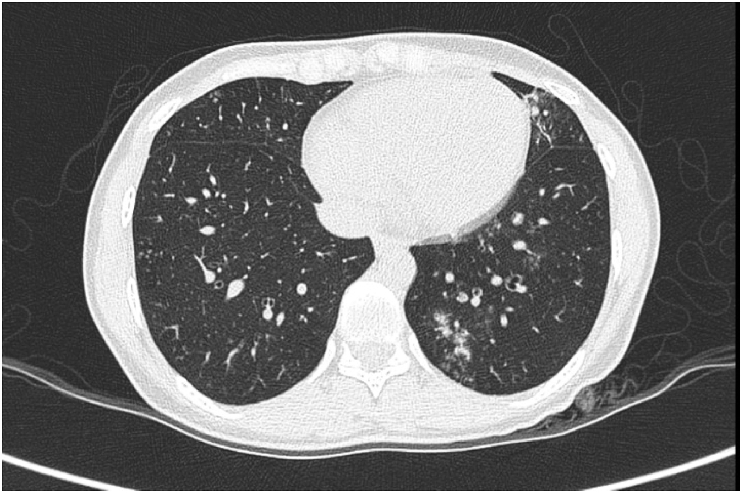
Fig. 1.
Axial HRCT section at the level of the lower chest reveals multiple tiny centrilobular nodules in the posterior basal segment of the left lower lobe and few nodules in the left lingula, right middle lobe and lateral basal segment of the right lower lobe.
Fig. 2.
Sagittal HRCT section of the left lung reveals foci of ground glass haziness and tiny nodules in the lower lobe and inferior lingula.
Clinicoradiological opinion was either atypical pneumonia or to rule out tuberculosis. She underwent fiberoptic bronchoscopy for bronchial wash and transbronchial lung biopsy; bronchial washings sent for smear for acid fast bacilli and fungal elements were negative, with gram stain showing occasional polymorphs; geneXpert MTB/RIF was not detected; 20 ml of bronchial washings which was hemorrhagic revealed an occasional alveolar macrophage with many neutrophils with a background of blood elements. Trans bronchial lung biopsy (TBLB) revealed histological features suggestive of Lipoid Pneumonia (Fig. 3).
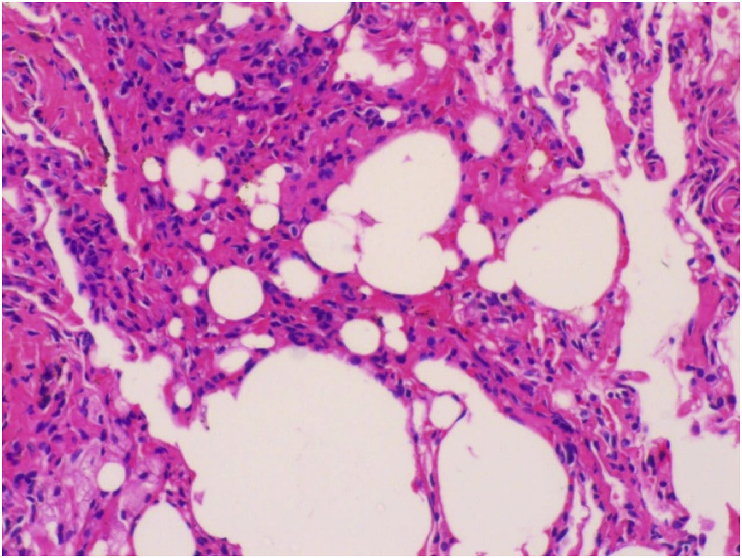
Fig. 3.
H&E section (200×) showing lung tissue composed of alveolar spaces with flattened lining, a few spaces show desquamation of the lining epithelium. Alveolar spaces are filled with macrophages with vacuoles of varying sizes.
Meticulous history, retrospectively, revealed patient habituated to applying a petrolatum ointment to the nose, externally, daily at night since more than a year. She was treated with oral prednisolone, tapered over a period of six months, apart from her regular inhaled corticosteroid and Fluticasone nasal spray. Her follow up HRCT-Chest at the end of one year showed partial resolution of the previous lesions, and patient is clinically stable without any relevant symptoms. (Fig. 4).
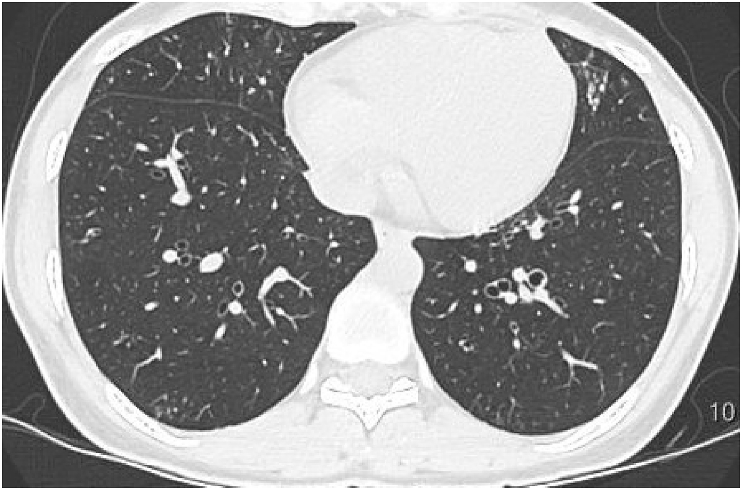
Fig. 4.
HRCT section at the level of the lower lobes reveals mild cylindrical bronchiectasis in the left lower lobe, faint tiny centrilobular nodules in the left lower lobe, right lower lobe and fibrotic lesions in the left lingula.
3. Discussion
Exogenous lipoid pneumonia is an uncommon entity without any pathognomonic clinical or radiological expressions. In adults, most of the cases emanate from usage of oil-based products as laxatives or for nasal application or instillations, especially for nasopharyngeal disorders. Medical literature contains many examples of exogenous lipoid pneumonia from intranasal instillation of petrolatum in the liquid form. A few case reports were found in the literature with examples of long-standing use of petroleum jellies applied intranasally [4], [5] and much rarer was external application causing ELP [6], [7], [8].
These reported cases were in patients who did not have underlying predisposing conditions for aspiration and mentholated topical ointments were used as nasal application for decongestant purpose, except for a case report of a female patient ingesting tablespoonful of cold Vaseline daily to induce soft daily bowel movement [9].
The predisposing factors are not obligatory for the mineral oil to penetrate the airways, as they were absent in 25% of cases [2]. It was noted that the petroleum jelly will liquefy at body temperature and lead to inhalation [5]. The oil finds its way into the alveoli of the lung, not only when directly introduced into the trachea but also at times when administered in sufficient quantities in the nose and throat [1]. The choice of liquid petrolatum as a “bland” vehicle for various medicaments used in the treatment of upper respiratory tract infections, is sufficiently light to enter the glottis without evoking the cough reflex. Then it is either aspirated or gravitates to the alveolar spaces [10]. Mineral oils can inhibit cough reflex and ciliary motility, thus facilitating inhalation [2]. Abanses JC et al. reported a case of an infant who presented with respiratory distress to the emergency after application of Vicks VapoRub directly under the nose. It was probably from the active ingredients of the aforementioned topical ointment which are noted to be ciliotoxic and mildly proinflammatory, thus increasing mucus secretion and decreasing mucus clearance [11].
The initial response of the oil in the alveoli, thus reached, is that of a foreign body reaction, from phagocytosis of emulsified oil by the alveolar macrophages. Thus, of the forty-four cases, the frequency of granulomatous form of inflammatory cell reaction was noted in 13 cases and the frequency of fibrotic lesions in 14 cases in the retrospective multicenter study by Gondouin A et al. [2]. Regardless of location, this inflammatory process can progress to fibrosis with destruction of alveoli and interstitium leading to chronic respiratory failure, end-stage lung disease and cor pulmonale [2], [12], [13].
Usually the diagnosis is not suspected at the first instance since the presentations are not characteristic and simulate wide array of disorders of interstitium or alveolar consolidation or lung tumors.
Several imaging patterns are identified on CT but none of them are specific to chronic ELP.
CT imaging showing areas of fat attenuation between −150 and −30HU, reinforced by a ‘positive CT angiogram sign’, inside the pulmonary consolidative and nodular opacities is consistent with lipoid pneumonia. But, these imaging features are not always seen in ELP. Other manifestations of chronic ELP are single or multiple nodules or masses that may or may not contain fat. In the absence of recognition of fat attenuation in these lesions, it is difficult to differentiate from other diseases, especially, malignancy [12].
Spickard and Hirschmann suggest that a consistent clinical history and roentgenographic abnormalities must accompany, apart from the demonstration of the lipid laden macrophages in the alveoli or interstitium of the lung tissue, for the diagnosis of ELP [13].
In the present case, we initially thought of excluding an infective condition including atypical pneumonia or tuberculosis. We performed bronchoalveolar lavage (BAL) and TBLB consecutively for diagnostic confirmation.
Hence, Exogenous Lipoid pneumonia can only be diagnosed with a high index of suspicion and a detailed historical review in patients presenting with chronic rhinobronchial allergy and infiltrative lesions on chest radiographs. In case of a negative yield of BAL fluid for free lipids or lipids in the alveolar cell vacuoles, a TBLB would confirm the diagnosis, rarely requiring an open lung biopsy.
In our patient, after the diagnosis of ELP, systemic corticosteroids were instituted for her persistent dyspnea, fever and cough, with diffuse infiltrative lesions on chest radiography. Patient was clinically stable without further radiological deterioration during follow up for a year.
In the literature, we could find the only reference of Ayvazian LF et al. for the treatment of ELP with prednisone [9]. Brown AC et al. treated their patient of ELP with prednisone unsuccessfully, due to significant fibrosis [4]. Another report of Chin NK et al., was of Idiopathic lipoid pneumonia treated with prednisolone [14].
4. Conclusion
Most of the therapeutic approaches available for the treatment of ELP, as of today, are from the experiences of the individual clinicians in the form of case reports.
Unsuspected causative agents, like Vicks VapoRub as in our case or any other agents containing mineral oils can silently or symptomatically lead to pulmonary fibrosis and even end-stage lung disease. Hence, high index of suspicion, early recognition, withdrawal of the offending agent and aggressive treatment of the underlying conditions like chronic rhinobronchial allergy, with a trial of oral corticosteroids, are the best therapeutic options available to date in the treatment of ELP, as in the present case.
Conflicts of interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Laughlin G.F. Studies of pneumonia following injections of oil. Am. J. Pathol. 1925;1:407–414. [PMC free article] [PubMed] [Google Scholar]
- 2.Gondouin A., Manzoni P.H., Ranfaing E., Brun J., Cadranel J., Sadoun D., Cordier J.F., Depierre A., Dalphin J.C. Exogenous lipid pneumonia: a retrospective multicentric study of 44 cases in France. Eur. Respir. J. 1996;9:1463–1469. doi: 10.1183/09031936.96.09071463. [DOI] [PubMed] [Google Scholar]
- 3.Volk B.W., Nathanson L., Losner S., Slade W.R., Jacobi M. Incidence of lipoid pneumonia in a survey of 389 chronically ill patients. Am. J. Med. 1951;10:316–324. doi: 10.1016/0002-9343(51)90276-8. [DOI] [PubMed] [Google Scholar]
- 4.Brown Andrew C., Slocum Philip C., Putthoff Stephen L., Wallace William E., Foresman Brian H. Exogenous lipoid pneumonia due to Nasal application of petroleum jelly. Chest. 1994;105(3):968–969. doi: 10.1378/chest.105.3.968. [DOI] [PubMed] [Google Scholar]
- 5.Varkey Basil. Lipoid pneumonia due to intranasal application of petroleum jelly. An old problem revisited. Chest. 1994;106(4):1311–1312. doi: 10.1378/chest.106.4.1311b. [DOI] [PubMed] [Google Scholar]
- 6.Cherrez Ojeda I., Calderon J.C., Guevara J., Cabrera D., Calero E., Cherrez A. Exogenous lipid pneumonia related to long-term use of Vicks VapoRub by an adult patient: a case report. BMC Ear, Nose Throat Disord. 2016;16:11. doi: 10.1186/s12901-016-0032-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kulkarni T., Pena T. A case of mistaken identity-lipoid pneumonia presenting as spiculated nodules after prolonged use of Vicks vaporub. Am. J. Respir. Crit. care Med. 2012;185:A6906. [Google Scholar]
- 8.Gattuso P., Reddy V.B., Castelli M.J. Exogenous lipoid pneumonitis due to Vicks Vaporub inhalation diagnosed by fine needle aspiration cytology. Cytopathology. 1991;2:3150316. doi: 10.1111/j.1365-2303.1991.tb00507.x. [DOI] [PubMed] [Google Scholar]
- 9.Ayvazian L.F., Steward D.S., Merkel C.G., Frederick W.W. Diffuse lipoid pneumonitis successfully treated with prednisone. Am. J. Med. 1966;43:930–934. doi: 10.1016/0002-9343(67)90251-3. [DOI] [PubMed] [Google Scholar]
- 10.Cannon P.R. The problem of lipid pneumonia. JAMA. 1940;115:2176–2179. [Google Scholar]
- 11.Abanses J.C., Arima S., Rubin B.K. Vicks VapoRub induces mucin secretion, decreases ciliary beat frequency and increase tracheal mucus transport in the ferret trachea. Chest. 2009;135(1):143–148. doi: 10.1378/chest.08-0095. [DOI] [PubMed] [Google Scholar]
- 12.Betancourt Sonia L., Martinez-Jimenez Santiago, Rossi Santiago E., Truong Mylene T., Carrillo Jorge, Erasmus Jeremy J. Lipoid pneumonia: spectrum of clinical and radiologic manifestations. Am. J. Roentgenol. 2010;194:103–109. doi: 10.2214/AJR.09.3040. [DOI] [PubMed] [Google Scholar]
- 13.Spickard A., Hirschmann J.V. Exogenous lipoid pneumonia. Arch. Intern Med. 1994;154:686–692. [PubMed] [Google Scholar]
- 14.Chin N.K., Hui K.P., Sinniah R., Chan T.B. Idiopathic lipoid pneumonia in an adult treated with prednisolone. Chest. 1994;105:956–957. doi: 10.1378/chest.105.3.956. [DOI] [PubMed] [Google Scholar]