Highlights
-
•
Intraosseous cystic meningioma is a very rare.
-
•
There are no reports of similar cases in the last 30 years.
-
•
Primary intraosseous meningioma is a subtype of primary extradural meningioma.
-
•
Cystic meningioma is rare, 2–4% of all meningiomas.
-
•
A meningioma with both characteristics is an exceptional occurrence.
Keywords: Case report, Meningioma, Intraosseous, Intradiploic, Cystic, Osteolysis
Abstract
Introduction
This is a very rare case of intraosseous cystic meningioma. There have been no reports of similar cases in the last 30 years.
Presentation of case
A 62-year-old man, suffering from a swelling of the lateral wall of the left orbit was admitted to our hospital. MRI and CT scan showed a large intradiploic lesion involving the lateral wall of the orbit and the greater wing of the sphenoid. The lesion was cystic with a mural nodule. We operated the patient and removed completely the mural nodule and the fibrous wall of cyst. Histological examination showed that the mural nodule was a benign meningothelial meningioma.
Discussion
Primary intraosseous meningiomas represent a subtype of primary extradural meningiomas; they comprise about 2% of all meningiomas and are therefore rare entities. Cystic meningiomas are rare, their incidence compared to all other types of meningiomas is of 2–4%. The presence of a meningioma with both characteristics: cystic and intraosseous, like in our case, is an exceptional occurrence.
Conclusion
The surgical management of tumor was easy; its rarity means that the case is interesting.
1. Introduction
Having searched the main scientific Literature databases: Scopus, ISI Web, and Google scholar, we found that there haven’t been any reports of primary intraosseous cystic meningiomas for the last 30 years, therefore we think it useful to illustrate our experience. This work has been reported in line with the SCARE criteria [1].
2. Presentation of case
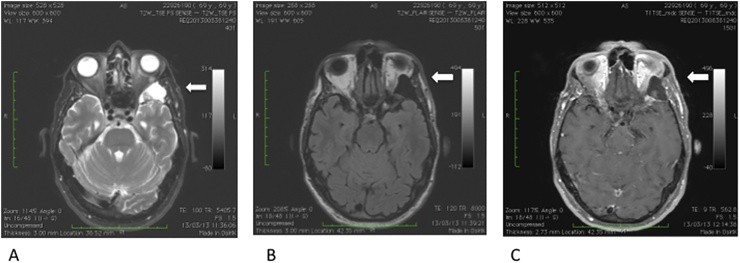
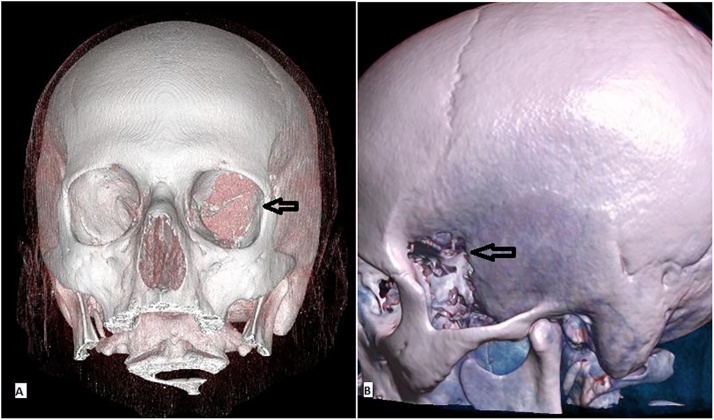
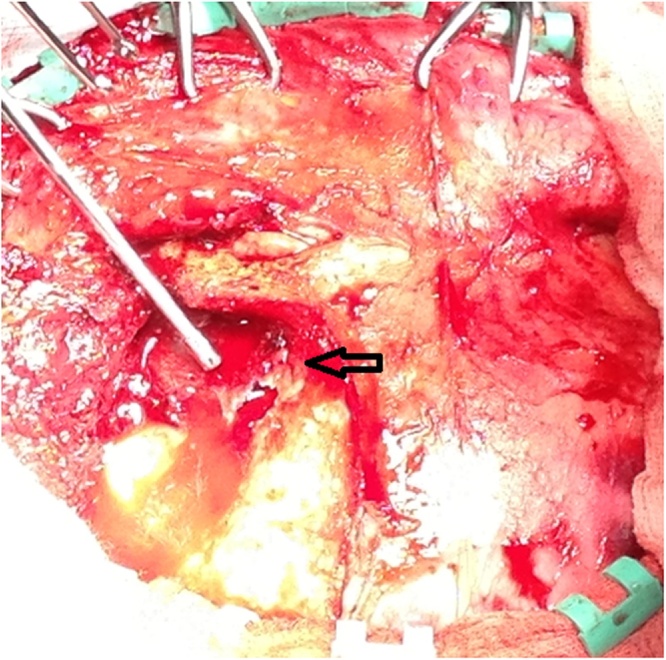
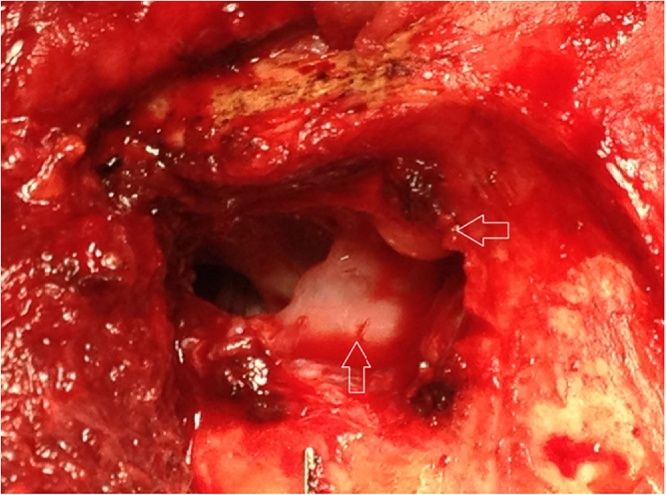
A 62-year-old man, suffering from a swelling of the lateral wall of the left orbit was admitted to our hospital in May 2013. The swelling had a hard consistency and was slightly painful on palpation. It had slowly grown over two years. The patient had a slight left proptosis. MRI (Fig. 1) showed a large intradiploic lesion involving the lateral wall of the orbit and the greater wing of the sphenoid in T2 weighted sequences. Within it, there was a non-homogenous and relatively hypointense round formation; in the FLAIR sequences the lesion looked hypointense. After contrast was administered the round formation showed increased signal intensity in a slightly non- homogenous way. CT scan (Fig. 2) showed an osteolytic lesion involving the lateral wall of the orbit and the greater wing of the sphenoid. It was near the suture between the sphenoid and zygomatic bones. The overall dimensions of the lesion were 23 × 32 mm; a large portion of the lesion was made up of fluid, whilst the dimensions of the solid part, highlighted by the dishomogenous contrast enhancement, were 8 × 9 mm. We operated the patient. We made a bi-coronal skin incision, using a left frontopterional approach. The bone bulged and was very thin. We opened it and were faced with a large cystic cavity with a thin fibrous wall, it was all contained inside the bone (Fig. 3). The cyst was full of yellow liquid; there was also a rather large mural nodule (Fig. 4), which was completely and easily removed. We also removed the fibrous wall. Once the tumor was removed, there was an evident dent where the bone was missing; for aesthetic purposes plastic surgery was carried out and a thin sheet of artificial bone, which was concurrently molded into the right shape, was applied. The patient was discharged from hospital after five days. The perioperative and postoperative course was uneventful. Histological examination (Fig. 5) showed that the mural nodule was a benign meningothelial meningioma (WHO Grade I) comprising cells with oval to round nuclei and small nucleoli, arranged in syncytial and lobular patterns, without atypical or malignant features. The cyst wall also did not include cancer cells; the tumor was attached to, but did not infiltrate the fibrous wall or the underlying bone.
Fig. 1.
A T2-weighted axial MRI: hyperintense signal alteration over a wide area in the diploic region in front of the temporal pole in the context of which is an nodular area heterogeneously hypointense. B. In the same layer, in the diploic region there is presence of an hypointense area in FLAIR sequences. C. T1-weighted MRI axial scan after administering paramagnetic contrast e.v.: slightly non- homogenous increase of signal of the globular formation in the intradiploic area.
Fig. 2.
3D CT reconstruction: osteolytic alteration of the orbital wall in the same location as the MRI showed.
Fig. 3.
The arrow in the photo shows the membrane of the cyst of the meningioma after removal of a very thing bone layer.
Fig. 4.
Vision from the operatory microscope of the surgical field: the horizontal arrow shows the cystic cavity, the vertical one the tumoral nodule.
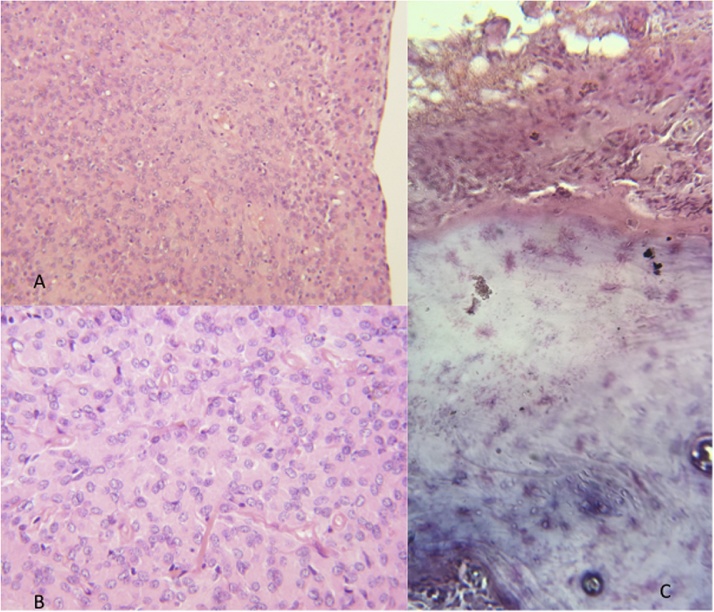
Fig. 5.
A Haematoxylin and Eosin stained sections of the mural nodule (A, B) show a benign meningothelial meningioma (WHO Grade I) comprising cells with oval to round nuclei and small nucleoli, arranged in syncytial and lobular patterns. There are no atypical or malignant features. An area (C) showing the interface between the tumor above and the bone matrix below with the intervening fibrous cyst wall. The tumor is attached to, but does not infiltrate the fibrous wall or the underlying bone.
3. Discussion
Primary intraosseous meningiomas [2], [3], [4], [5], [6] represent a subtype of primary extradural meningiomas. Typically, they originate within the bones of the skull, they comprise about 2% of all meningiomas and are therefore rare entities. Meningiomas that have within them, or in a surrounding area, a cyst filled with fluid are consequently defined as cystic [7]. They should not be confused with microcystic meningiomas, which are a histological variant of this tumor [8]. Nauta’s classification [9] divides cystic meningiomas into 4 groups: in types I and II the cysts are intratumoral, in types III and IV the cysts are extratumoral. In type III the cyst is bordered by both the tumor and brain parenchyma, which undergoes reactive gliosis; in type IV the meningioma is associated with a CSF cyst bordered by the arachnoid. Cystic meningiomas are quite rare, their incidence compared to all other types of meningiomas is of 2–4%. The presence of a meningioma with both characteristics: cystic and intraosseous, like in our case, is an exceptional occurrence. The tumor here illustrated was completely intradiploic and therefore fitted all the criteria to be defined as a primary intraosseous meningioma. Most intraosseous meningiomas favor osteoblastic activity, thus causing hyperostosis; but in literature there has also been a very small number of reports of osteolytic meningiomas, like ours [10], [11], [12].
As the wall of the cyst did not comprise tumoral tissue, we believe the meningioma to be of the third type according to Nauta’s classification. Since the tumor was not in contact with brain tissue, but with the bone, the cyst wall was not formed by reactive gliosis, but by reactive fibrosis. The tumor removal was easy, without complications.
The differential diagnosis needed to exclude the following patologies: meningoencefalocele [13], intradiploic arachnoid cyst [14], intradiploic dermoid or epidermoid tumor [15], intraosseous lipoma [16]. Meningoencefalocele presents as a combination of fluid-filled cyst and parenchyma, which, unlike tumor tissue, isn’t enhanced by the contrast agent; moreover in three-dimensional MRI reconstructions it is possible to note continuity between intracranial brain parenchyma and herniated parenchyma. In the case of an arachnoid cyst there are no mural nodules. The differential diagnosis between the lesion we operated on and a dermoid or epidermoid tumor as well as a lipoma is mainly ascribable to the difference of intensity of signal in the MRI and of density in a CT scan between the cholesterol or fat and the liquor-like fluid of the tumor cyst.
4. Conclusion
The rare occurrence of such tumor is what makes this case of particular interest. Even before surgery, having analyzed the MRI and CT scans findings, we had already suspected the lesion to be a benign one, but as is often the case in rare pathologies an exhaustive diagnosis was only possible after the histological examination was carried out.
Conflicts of interest
We wish to confirm that there are no known conflicts of interest associated with this publication.
Funding
We wish to confirm that there has been no significant financial support for this work that could have influenced its outcome.
Ethical approval
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
Riccardo Caruso: study concept, writing the paper, first surgical operator.
Giuseppina Fini: second surgical operator.
Alessandro Pesce: litterature data collection.
Venceslao Wierzbicki: third surgical operator, data analysis.
Luigi Marrocco: data collection.
Emanuele Piccione: radiological data analysis.
Paola Pasquini: histologic data analysis.
Registration of research studies
Registration is not required.
Guarantor
Riccardo Caruso.
Contributor Information
Riccardo Caruso, Email: riccardo.caruso@uniroma1.it.
Giuseppina Fini, Email: giuseppina.fini@uniroma1.it.
Alessandro Pesce, Email: ale_pesce83@yahoo.it.
Venceslao Wierzbicki, Email: wenzel@alice.it.
Luigi Marrocco, Email: lumarrocco@gmail.com.
Emanuele Piccione, Email: epiccione@sirm.org.
Paola Pasquini, Email: paspaol66@libero.it.
References
- 1.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Chen T.C. Primary Intraosseous Meningioma. Neurosurg. Clin. N. Am. 2016;27:189–193. doi: 10.1016/j.nec.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 3.Choi K.W., Chung K.J., Kim Y.H. Primary intraosseous meningioma. Arch. Plast. Surg. 2015;42:378–380. doi: 10.5999/aps.2015.42.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shamji M.F., Goyal M. Case of the month #178: intraosseous orbital meningioma presenting with diplopia and proptosis. Can. Assoc. Radiol. J. 2012;63:228–230. doi: 10.1016/j.carj.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Hussaini S.M., Dziurzynski K., Fratkin J.D. Intraosseous meningioma of the sphenoid bone. Radiol. Case Rep. 2010;5:357. doi: 10.2484/rcr.v5i1.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elder J.B., Atkinson R., Zee C.S. Primary intraosseous meningioma. Neurosurg. Focus. 2007;23:E13. doi: 10.3171/FOC-07/10/E13. [DOI] [PubMed] [Google Scholar]
- 7.Fortuna A., Ferrante L., Acqui M. Cystic meningiomas. Acta Neurochir. (Wien) 1988;90:23–30. doi: 10.1007/BF01541262. [DOI] [PubMed] [Google Scholar]
- 8.Bujok J., Bienioszek M. Microcystic variant of an intraosseous meningioma in the frontal area: a case report. Case Rep. Neurol. Med. 2014;2014:527267. doi: 10.1155/2014/527267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nauta H.J.W., Tucker W.S., Horsey W.J. Xanthochromic cysts associated with meningioma. J. Neu- rol. Neurosurg. Psychiatry. 1979;42:529–535. doi: 10.1136/jnnp.42.6.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vlychou M., Inagaki Y., Stacey R. Primary intraosseous meningioma: an osteosclerotic bone tumour mimicking malignancy. Clin. Sarcoma Res. 2016;6:14. doi: 10.1186/s13569-016-0054-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tokgoz N., Oner Y.A., Kaymaz M. Primary intraosseous meningioma: CT and MRI appearance. AJNR Am. J. Neuroradiol. 2005;26:2053–2056. [PMC free article] [PubMed] [Google Scholar]
- 12.Pearl G.S., Takei Y., Parent A.D. Primary intraosseous meningioma presenting as a solitary osteolytic skull lesion: case report. Neurosurgery. 1979;4:269–270. doi: 10.1227/00006123-197903000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Moudrous W., Boogaarts H.D., Grotenhuis J.A. Clinical Image A meningoencephalocele caused by a chronic growing skull fracture in a 76-year old patient. Word Neurosurg. 2016;16 doi: 10.1016/j.wneu.2016.08.052. [DOI] [PubMed] [Google Scholar]
- 14.Sachdeva R., Turell M.E., Meadows S.R. Congenital intradiploic arachnoid cyst presenting as painless proptosis. J. AAPOS. 2011;15:601–603. doi: 10.1016/j.jaapos.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 15.Berti A.F., Lovaas G.C., Santillan A. Primary intradiploic pterional epidermoid cyst. South. Med. J. 2010;103(January):87–89. doi: 10.1097/SMJ.0b013e3181c2a867. [DOI] [PubMed] [Google Scholar]
- 16.Jamrozik Z., Rosiak G., Kierdaszuk B. Intraosseous lipoma of the sphenoid: a case study. Case Rep. Neurol. Med. 2013;2013:519341. doi: 10.1155/2013/519341. [DOI] [PMC free article] [PubMed] [Google Scholar]