Abstract
The aim of this study was to examine the influence of demographic variables and the interplay between collectivism and acculturation on breast and cervical cancer screening outcomes among Vietnamese American women. Convenience sampling was used to recruit 111 Vietnamese women from the Richmond, VA, metropolitan area, who participated in a larger cancer screening intervention. All participants completed measures on demographic variables, collectivism, acculturation, and cancer-screening-related variables (i.e., attitudes, self-efficacy, and screening behavior). Findings indicated that collectivism predicted both positive attitudes and higher levels of self-efficacy with regard to breast and cervical cancer screening. Collectivism also moderated the relationship between acculturation and attitudes toward breast cancer screening such that for women with low levels of collectivistic orientation, increasing acculturation predicted less positive attitudes towards breast cancer screening. This relationship was not found for women with high levels of collectivistic orientation. The current findings highlight the important roles that sociodemographic and cultural variables play in affecting health attitudes, self-efficacy, and behavior among Vietnamese women. The findings potentially inform screening programs that rely on culturally relevant values in helping increase Vietnamese women’s motivation to screen.
The epidemiological literature indicates that Vietnamese women in the United States experience higher rates of cervical cancer incidence and mortality than White women and other ethnic minority women (Bates, Hofer, & Parikh-Patel, 2008; McCracken et al., 2007; Miller, Chu, Hankey, & Ries, 2008). In addition, Vietnamese women experience poorer breast and cervical cancer prognosis, which is attributable to later stage diagnosis due to low rates of cancer screening (Gomez et al., 2005; Kagawa-Singer et al., 2007; Ma, Shive, Wang, & Tan, 2009). The continuing decline in national breast and cervical incidence and mortality rates reflect the impact of increased uptake in cancer screening in the general U.S. population (Edwards et al., 2013). Vietnamese women living in the United States have reported low levels of Pap testing and clinical breast examinations (CBEs), however, as compared with other racial/ethnic groups, even other Asian subgroups (De Alba, Ngo-Metzger, Sweningson, & Hubbell, 2005; Kandula, Wen, Jacobs, & Lauderdale, 2006; Wang, Sheppard, Schwartz, Liang, & Mandelblatt, 2008). Ho and colleagues (2005) conducted a survey of Vietnamese women living in one county in Texas. They found that 68% of the respondents had never had a Pap test and 45% had never had a CBE. Similar low rates of cancer screening among Vietnamese women have been reported in several other studies (Do et al., 2007; Lam et al., 2003; Nguyen et al., 2006; Taylor et al., 2004). Although cancer disparities may stem from structural barriers such as lack of insurance and access to care (Pourat, Kagawa-Singer, Breen, & Sripipatan, 2010), sociocultural factors also likely shape health beliefs and behaviors for Vietnamese American women (Ma et al., 2012).
The specific aim of this study was to examine sociodemographic correlates of breast and cervical cancer screening attitude, self-efficacy, and behavior among Vietnamese women. In addition, we were interested in examining the influence of cultural factors such as collectivism and acculturation on cancer-screening variables. For the present study, we recruited Vietnamese women from two local faith-based communities as part of a larger cancer screening intervention, Suc Khoe La Quan Trong Hon Sac Dep! Health Is More Important Than Beauty! In this article, the authors attempt to speak to an international forum to illustrate how health cannot be decontextualized from culture, whether measured at a distal level or proximal individual level. The present article seeks to elucidate the relationship between cultural factors and cancer relevant variables among Vietnamese women.
We rely on Andersen’s (1968, 1995) Behavioral Model of Health as our conceptual framework. The model posits that people’s use of health services (e.g., cancer screening) is a function of predisposition to use these services, enabling or impeding factors, and their need for care. Predisposing characteristics include demographic traits such as age, gender, social structures that determine status (e.g., education), and health beliefs such as beliefs of one’s capabilities in performing a task (i.e., self-efficacy for obtaining a Pap test or CBE; Bandura, 1986). Enabling factors also influence whether individuals engage in health behaviors and constitute both personal (e.g., income and health insurance status) and community factors (e.g., available health facilities and programs). Last, an individual’s perceived needs influence utilization of health services.
While some critics have suggested that the model neglects the role of culture, Andersen (1968, 1995) proposed that cultural variables help contribute to the development of social networks and guide social interactions; thus, they constitute social structures that shape an individual’s status. Acculturative processes exemplify cultural factors that shape one’s social class as they reflect the negotiation of ethnic identities for Vietnamese women. These negotiations include both the adoption of autonomous and independent traits valued in Western cultures and also the retaining of interdependent and caretaking traits valued in Eastern cultures. The interplay of these traits may influence how Vietnamese women perceive and evaluate issues surrounding preventive health. We further explore these cultural constructs below.
Acculturation
Acculturation occurs when a minority individual adopts the attitudes, beliefs, values, and behaviors of the dominant culture (Berry, 1980; Robbins, Chatterjee, & Canda, 2006). The process of acculturation is complex and lends itself to diametric roles in the domain of health. Among Vietnamese samples, the adoption of compromising and harmful health behaviors can result from acculturation as it has been linked to increased cigarette smoking (An, Cochran, Mays, & McCarthy, 2008), substance abuse (Reid, Higgs, Beyer, & Crofts, 2002), risky sexual behavior (Yi, 1998), and poor diet and sedentary lifestyle (Kaplan et al., 2003).
Conversely, higher levels of acculturation can also promote positive health behaviors. In comparison with their counterparts who report low levels of acculturation, Vietnamese women with higher levels of acculturation are more likely to endorse help-seeking behaviors for mental health (Luu, Leung, & Nash, 2009) and to undergo cancer screenings (Tang, Solomon, & McCracken, 2000; Yi & Reyes-Gibby, 2002). The intermediary between acculturation and the well-being of the ethnic minority individual lies within the type of normative behavior found in the dominant society. Acculturation influences the adoption of normative traits and behaviors found in the dominant culture; some of these behaviors may be harmful, while others may be health promoting. In the current study, we propose that acculturation will predict positive cancer screening outcomes as breast and cervical cancer screening constitute behaviors that are normative and generally valued in the United States.
Collectivism
Markus and Kitayama (1991) proposed two types of cultures: one that fostered an independent self-construal and one that fostered an interdependent self-construal. Members from individualistic Western cultures (e.g., United States, England, France) typically view the self as an independent being, whereas members from collectivistic Eastern cultures (e.g., Japan, China, Vietnam) view the self as an interdependent being (Markus & Kitayama, 1991; Triandis, 1995). Individualistic societies emphasize an independent self, which leads to the endorsement of values such as autonomy, egocentrism, separateness, self-containment, and uniqueness. Collectivistic societies emphasize an interdependent self, and this leads to the endorsement of values such as contextualism, allocentrism, relatedness, harmony, holism, and connectedness (Markus & Kitayama, 1991; Triandis, 1995).
The collectivistic orientation of Vietnamese culture provides a context in which people are seen within the family structure rather than as independent and autonomous individuals (Chung & Bemak, 1998). Ideally, members of a family are expected to subordinate their personal interests to those of the family or collective whole and to fulfill their duties to this larger unit (Bich, 1999). Because collectivist women are expected to be primary caretakers of home, children, and husband (Davis, 2000), understanding inherent cultural values is important as these values may influence a person’s motivation for maintaining health. We propose that collectivistic orientation will predict positive cancer screening outcomes as it may motivate Vietnamese women to adhere to screening guidelines in order to maintain their health so they can care for others.
In addition, we propose that having a collectivistic orientation will moderate the relationship between acculturation and cancer screening variables. Because possession of collectivist values may enhance motivations for screening, it is possible that for those who are high in collectivism, the relationship between acculturation and positive cancer screening outcomes will be stronger than for those who are low in collectivism.
The Study’s Hypotheses
This study was guided by the following hypotheses:
Acculturation will be positively associated with cancer screening variables.
Collectivism/interdependency will be positively associated with cancer screening variables.
Collectivism will moderate the relationship between acculturation and cancer screening variables such that for those who are high in collectivism, the relationship between acculturation and positive cancer screening outcomes will be stronger than for those who are low in collectivism.
METHODS
Although the design of the current study is cross sectional, it was part of a larger, longitudinal cancer-screening intervention study (results are not reported in the present article). Of the 111 Vietnamese women in our study sample, half of the participants were enrolled in a screening intervention group and the other half were enrolled in a control group. All measures for the current study came from pretest data.
Participants
The study sample comprised 111 Vietnamese women living in the Richmond, Virginia (United States), metropolitan area. This convenience sample was recruited from the Catholic Vietnamese Church of Martyrs (63%) and the Hue Quang Buddhist Temple (37%). Participants’ mean age was 39.06 years (SD = 13.64), ranging between 18 and 70 years. One participant was excluded from the analyses because her age (78 years) exceeded the inclusion age criterion of 70 years, yielding an analytic sample of 110 participants. Refer to Table 1 for additional information related to participants’ demographics.
TABLE 1.
Participant Demographics
| Characteristic | # | % |
|---|---|---|
| Education | ||
| Some high school | 30 | 28 |
| High school graduate/GED | 29 | 26 |
| Some college | 20 | 18 |
| College graduate | 28 | 25 |
| Postcollege graduate | 3 | 3 |
| Children | ||
| Yes | 80 | 73 |
| No | 30 | 27 |
| Household income | ||
| Less than $10,000 | 17 | 16 |
| $10,000–15,000 | 15 | 14 |
| $15,000–25,000 | 25 | 23 |
| $25,000–50,000 | 23 | 21 |
| $50,000–75,000 | 14 | 13 |
| Over $75,000 | 16 | 14 |
| Marital status | ||
| Single | 25 | 23 |
| Married | 74 | 67 |
| Divorced | 6 | 5 |
| Widowed | 4 | 4 |
| Employed | ||
| Yes | 79 | 72 |
| No | 31 | 28 |
| Regular physician | ||
| Yes | 67 | 61 |
| No | 43 | 39 |
| Health insurance | ||
| Yes | 76 | 69 |
| No | 34 | 31 |
Note: Numbers may not always add up to 110 due to missing responses.
Participant inclusion criteria
To be included in the study, participants had to be between the ages of 18 and 70 years, female, and self-identify with a Vietnamese ethnic background. Women whose medical histories included hysterectomy were eligible to participate in the educational session, but their data were excluded from analyses that involved cervical cancer screening. Based on this criterion, data from eight women were excluded from analyses involving cervical cancer screening variables.
Measures
All measures were available in both English and Vietnamese. Each measure was translated into Vietnamese by a native speaker then back-translated into English and reviewed for accuracy.
Predictor Variables
The measures used as predictors are listed below.
Demographic measures
Each woman provided information on her age, education, marital status, children status, income, employment, health insurance, whether she had a regular physician, and history of a hysterectomy.
Acculturation
The participants’ level of acculturation to United States culture was measured using the Suinn-Lew Asian Self-Identity Acculturation scale (SL-ASIA; Suinn, Rickard-Figueroa, Lew, & Vigil, 1987). The SL-ASIA is an 18-item scale that measures language, ethnic identity, friendship choices, behaviors, generational and geographic history, and attitudes. The items are rated on a 5-point Likert-type scale, ranging from 1 (low acculturation) to 5 (high acculturation). The SL-ASIA has been tested and validated with various Asian groups, including the Vietnamese, demonstrating associations with other relevant Eastern cultural variables such as social integrity and family attitude (Dao, Teten, & Nguyen, 2011). Cronbach’s alpha for the current study was .85.
Collectivism/interdependency
Collectivism/interdependency was measured using an adapted version of the Self-Construal Scale (Singelis, 1994). The Self-Construal Scale assesses two aspects of the self-construal construct using an interdependent subscale and an independent subscale. Responses are made using a 7-point Likert-type scale ranging from 1 (strongly disagree) to 7 (strongly agree). The current study used only the 11-item interdependent subscale; an example of an item from this subscale is, “It is important for me to maintain harmony within my group.” The Self-Construal Scale has been validated with previous Vietnamese samples, demonstrating associations with relevant Eastern cultural variables such as family cohesion and social support (Lam, 2005). Cronbach’s alpha for the current study was .75.
Outcome Measures
The following measures were used as cancer screening outcomes.
Attitudes toward breast and cervical cancer screening
We measured attitudes toward breast and cervical cancer screening based on a similar measure by Marteau and colleagues (2002). Participants responded to the four-item measure (e.g., “How important are regular Pap smears for women to remain healthy?”) using a Likert-type response format, ranging from 1 (not at all important) to 7 (extremely important). Cronbach’s alpha for attitudes toward Pap testing subscale scale was .73 and attitudes toward CBE subscale was .82.
Self-efficacy for breast and cervical cancer screening
We measured efficacy in screening based on a measure used by Champion and colleagues (2007). Participants responded to 20 items (e.g., “You can make an appointment for a Pap test”) using a Likert-response format, ranging from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s alpha for the Pap testing self-efficacy scale was .84 and for the CBE self-efficacy scale was .91.
Previous receipt of a CBE or Pap test
Cancer screening behavior was obtained by asking participants if they have ever received a Pap test or CBE (e.g., “Have you ever had a Pap test?” Yes = 1, No = 0).
Procedure
The authors obtained Institutional Review Board approval before recruitment began. With the help of community liaisons, participants were recruited through fliers, bulletin announcements, and service announcements. Individuals were also referred by community liaisons. Interested individuals contacted the principal investigator, who notified the women of the time and place of the group session. On session days, participants signed informed consent forms. Half of the women participated in a breast and cervical cancer-screening intervention (results not reported here). All participants completed baseline measures on demographic traits, cultural measures, and cancer-screening variables. Questionnaires took approximately 40 minutes to complete, and were administered by either the principal investigator or by trained community members. Participants were provided with a $30 thank-you/incentive gift for participation.
Data analytic plan
Descriptive statistics were calculated. Multiple hierarchical linear regression and logistic regression analyses were conducted to assess relationships among cultural variables and cancer screening variables. Based on evidence in the literature showing an association of certain covariates with cancer screening variables, we chose age, children status, educational attainment, household income, and health insurance status as covariates (Benyamini, Blumstein, Boyko, & Lerner-Geva, 2008; Couture, Nguyen, Alvarado, Velasquez, & Zunzunegi, 2008; DeNavas-Walt, Proctor, & Smith, 2012; Meissner et al., 2009; Somanchi, Juon, & Rimal, 2010).
RESULTS
Of the 110 women in the study sample, 65 (60%) participants reported having a CBE in their lifetime, and 72 (66%) participants reported having a Pap test in their lifetime. See Table 2 for descriptive statistics of the study’s measures.
TABLE 2.
Descriptives of Study’s Measures
| Measure | Min | Max | Mean | SD |
|---|---|---|---|---|
| Attitudes toward CBE | 6 | 14 | 13.28 | 1.34 |
| Attitudes toward Pap test | 5 | 14 | 12.95 | 1.91 |
| Self-efficacy for CBE | 25 | 50 | 45.09 | 6.17 |
| Self-efficacy for Pap test | 21 | 50 | 44.29 | 7.32 |
| Acculturation | 26 | 64 | 43.13 | 8.51 |
| Collectivism | 41 | 77 | 66.18 | 7.39 |
Attitudes Toward Breast Cancer Screening
We used hierarchical multiple regression analysis to predict scores in attitudes toward breast cancer screening. The analysis controlled for age, children status, educational attainment, household income, and health insurance status, which were entered in the first step. Centered scores for acculturation and collectivism were entered in the second step. Last, the higher order interaction effect between acculturation and collectivism was entered in the third step. The model accounted for a significant amount of variance in attitudes toward breast cancer screening, F (8, 101) = 4.81, p ≤ .001; R2 = .28. The addition of the interaction effect in Model 3 significantly improved prediction (R2 change = .04; F = 5.68, p = .02).
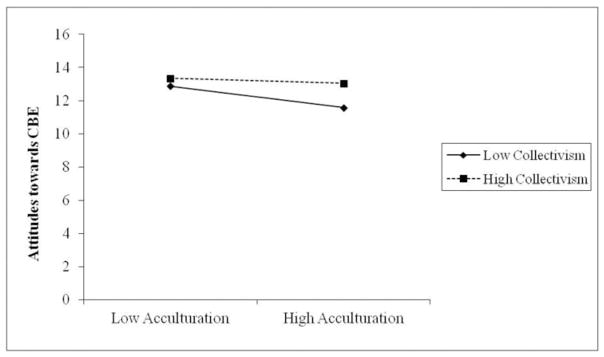
Increasing age was significantly associated with less positive attitudes toward breast cancer screening, β = −.24, t(108) = −2.07, p = .04. Having children was significantly associated with positive attitudes toward breast cancer screening, β = .28, t(108) = 2.23, p = .03. Higher levels of acculturation significantly predicted less positive attitudes, β = −.29, t(108) = −2.73, p = .01. Higher levels of collectivism significantly predicted more positive attitudes toward breast cancer screening, β = .36, t(108) = 4.20, p ≤ .001. Last, there was a significant interaction between acculturation and collectivism, β = .21, t(108) = 2.38, p = .02. For women who were low in collectivism, high levels of acculturation were associated with less favorable attitudes toward breast cancer screening. This relationship was not observed for women who were high in collectivism. Refer to Figure 1.
FIGURE 1.
The effect of collectivism on acculturation and attitudes toward CBE.
Attitude Toward Cervical Cancer Screening
Following identical blocking procedures in the previous regression analysis, the model accounted for a significant amount of variance in attitudes toward cervical cancer screening, F (7,92) = 2.90, p = .009; R2 = .18. The addition of cultural variables in Model 2 significantly improved prediction (R2 change = .10; F = 5.36, p = .006). Having children significantly predicted positive attitudes toward cervical cancer screening, β = .27, t(100) = 1.99, p = .05. Higher levels of collectivism significantly predicted more positive attitudes toward cervical cancer screening, β = .25, t(100) = 2.59, p = .01.
Self-Efficacy for Breast Cancer Screening
Following identical blocking procedures in the previous regression analysis, we found that the model accounted for a significant amount of variance in self-efficacy for breast cancer screening, F (7, 102) = 6.83, p ≤ .001; R2 = .32). The addition of cultural variables in Model 2 significantly improved prediction (R2 change = .08; F = 5.82, p ≤ .001).
Higher attainment of education was significantly associated with higher levels of self–efficacy for breast cancer screening, β = .22, t(108) = 2.18, p = .03. Having health insurance was significantly associated with higher levels of self-efficacy for breast cancer screening, β = .26, t(108) = 2.84, p = .005. Higher levels of collectivism significantly predicted higher levels of self-efficacy for breast cancer screening, β = .28, t(108) = 3.37, p ≤ .001.
Self-Efficacy for Cervical Cancer Screening
Following identical blocking procedures in the previous regression analysis, the model accounted for a significant amount of variance in attitudes toward cervical cancer screening, F (7,92) = 6.12, p ≤ .001; R2 = .32. The addition of cultural variables in Model 2 significantly improved prediction (R2 change = .07; F = 4.52, p = .01).
Higher attainment of education was significantly associated with higher levels of self–efficacy for cervical cancer screening, β = .24, t(100) = 2.24, p = .03. Having health insurance was significantly associated with higher levels of self-efficacy for cervical cancer screening, β = .25, t(100) = 2.55, p = .01. Higher levels of collectivism significantly predicted higher levels of self-efficacy for cervical cancer screening, β = .24, t(100) = 2.72, p = .008.
Previous Receipt of CBE
A logistic regression analysis was conducted to predict whether participants had received a CBE in their lifetime (0 = No, 1 = Yes). Using previous receipt of a CBE as the outcome, age, children status, educational attainment, household income, and health insurance status were controlled for and entered in the first step. Measures used to predict previous receipt of a CBE included centered scores in acculturation and collectivism and were entered into the second step. Last, the higher order interaction effect between acculturation and collectivism was entered in the third step.
Model 1 was significant, χ2(5) = 60.74, p ≤ .001; model fit did not improve with the addition of cultural variables or the interaction effect. The Nagelkerke R-square value equaled .58 and the Cox and Snell R-square value equaled .43. The variables correctly predicted 85% of the cases. The Hosmer and Lemeshow Test was nonsignificant, χ2(8) = 17.42, p = .12, indicating that the model did not differ from the observed data and was a good fit. According to the Wald criterion, age was significantly and positively associated with previous receipt of a CBE, β = .12, χ2(1) = 16.68, p ≤ .001. The change in log odds associated with a one-unit change in age was 1.12.
Previous Receipt of Pap Test
A logistic regression analysis was conducted to examine the relationship between the covariates and the probability of having had a Pap test in their lifetime (0 = No, 1 = Yes) using blocking procedures identical to those in the previous model. Model 2 was significant, χ2(7) = 54.78, p ≤ .001. The Nagelkerke R-square value equaled .55, and the Cox and Snell R-square value equaled .40. The variables correctly predicted 85% of the cases. The Hosmer and Lemeshow Test was non significant, χ2(8) = 8.41, p = .39, indicating that the model did not differ from the observed data and was a good fit.
According to the Wald criterion, age predicted previous receipt of a Pap test, β = .06, χ2(1) = 5.20, p = .02. The change in log odds associated with a one-unit change in age was 1.06. Having children also predicted having a previous Pap test, β = 1.58, χ2(1) = 3.65, p = .05. The change in log odds associated with having a child was 4.87. Last, acculturation predicted the outcome, β = .10, χ2(1) = 4.49, p = .03. The change in odds associated with a one-unit change in acculturation was 1.11.
DISCUSSION
The study findings revealed low rates of cancer screening among Vietnamese women that are consistent with those found in earlier research (Do et al., 2007; Lam et al., 2003; Nguyen et al., 2006; Nguyen, Beglrave, & Sholley, 2010; Taylor et al., 2004). We uncovered significant relationships between the demographic variables and cancer screening variables. Having health insurance was associated with women’s higher levels of self-efficacy for breast and cervical cancer screening. These findings are consistent with other studies that highlight the strong relationship between health insurance status and cancer screening behavior (Coughlin, Leadbetter, Richards, & Sabatino, 2008; Lee-Lin et al., 2007; Meissner et al., 2009) as insurance status is an enabling factor and a necessary component to health care access. Therefore, practitioners should assess all clients’ health insurance statuses. In addition, if needed, practitioners should link their clients with local and national resources, such as Medicaid, to help ensure that their clients have access to free or low-cost health insurance. Further, practitioners should continue to advocate for policies that would ensure that all Americans have access to quality health care.
In addition, higher levels of educational attainment predicted higher levels of self-efficacy for breast and cervical cancer screening; this is aligned with previous research that demonstrates ties between education and health promotion (Benyamini, Blumstein, Boyko, & Lerner-Geva, 2008; Couture et al., 2008). Education is potentially associated with cancer screening as a function of information seeking. That is, highly educated individuals are likely to obtain multiple sources of cancer-related information. Consequently, they may be more informed of the recommended preventive measures as well as consequences related to cancer (Walsh et al., 2010). As a result, practitioners should actively offer and engage in cancer awareness programs. Practitioners should ensure that cancer screening awareness programs are marketed via multiple methods, such as flyers distributed at local temples, radio, TV, and social media. In addition, practitioners should ensure that awareness programs are culturally sensitive (e.g., materials are written at an elementary education level).
When compared with participants without children, participants with children were more likely to have positive attitudes toward breast cancer and cervical screening. Participants with children were also more likely to have received a Pap test in their lifetime compared with their counterparts. These findings are in line with research that suggests that cancer survivors are more likely to fear progression of cancer if they are younger and have children in comparison with those who do not have children (Baucom, Porter, Kirby, Gremore, & Keefe, 2005–2006; Mehnert, Berg, Henrich, & Herschbach, 2009). Although our study examines women without a diagnosis of breast or cervical cancer, the link between having children and cancer screening outcomes is evident. These findings illustrate how emphasizing the salience of the Vietnamese woman’s caretaking role might serve as a motivator for cancer screening behavior. Therefore, practitioners should consider this finding when interacting with clients directly and developing procancer screening marketing materials. Further, this finding suggests that women who do not have children may potentially be at higher risk of not engaging in cancer screening behaviors than women who have children. Further research is needed to identify whether women who do not have children and women who do not intend to have children have less favorable attitudes toward cancer screening. Simultaneously, researchers and practitioners should assess other potential motivators as they relate to cancer screening behaviors for women who do not have children.
Age played diametric roles in cancer screening variables. As expected, increasing age was significantly associated with higher probability of having had a CBE and a Pap test. Surprisingly, increasing age was associated with less positive attitudes toward breast cancer screening. Several possibilities for this inconsistency are plausible. For example, it is possible that younger Vietnamese American women are more acculturated than older Vietnamese American women. These younger and more acculturated Vietnamese women may hold more favorable attitudes toward cancer screening than older Vietnamese women, as the younger Vietnamese women may perceive cancer screening as a “Western” behavior. Hence, more effort should be given to targeting older Vietnamese women in health promotion programs. During interactions with older Vietnamese women, practitioners should consider the significant finding of maternal status as an important predictor of cancer screening behaviors, as many of these older women are likely to be mothers and hold collectivistic orientations.
We also found proximal-level cultural correlates of cancer screening variables (i.e., acculturation and collectivism). Acculturation significantly predicted previous receipt of a Pap test. These findings are consistent with existing evidence showing acculturated Asian women are more likely to undergo cancer screening as compared with their less acculturated counterparts (Tang et al., 2000; Yi & Reyes-Gibby, 2002). In addition, collectivism predicted positive attitudes toward breast and cervical cancer screening and higher levels of self-efficacy for breast and cervical cancer screening. These relationships may be explained by two mechanisms. First, Vietnamese women may feel it is incumbent on them to take care of their health to ensure they can fulfill their responsibility of caring for their husband and children; thus, the women develop positive attitudes toward screening. Second, Vietnamese women with collectivist values may have higher efficacy for screening because the family unit plays a central role in the coping, healing, and health-related decisions among members of collectivistic societies (Braun, Mokuau, Hunt, Kaanoi, & Gotay, 2002; Davis, 2000). These findings suggest that individualist (presumably the primary orientation of women who are more acculturated) and collectivist orientations are associated with select positive cancer screening attitudes and behaviors.
We found, however, an unexpected effect; acculturation was negatively associated with positive attitudes toward breast cancer screening. This relationship was found only for women low in collectivistic orientation, but not for women high in collectivistic orientation. This partially confirms our initial predictions of the moderating role of collectivism on acculturation and cancer screening variables by suggesting a protective effort. Highly acculturated Vietnamese women may have less favorable attitudes toward Pap testing than less acculturated women due to anxiety related to being more familiar with cancer screening exams. In Vietnamese culture, a woman’s body is considered private. As a result, there is a strong tendency for Vietnamese women to experience embarrassment and hesitation when encountering issues such as breast and cervical examination (Donnelly, 2006). The motivations to stay healthy to fulfill responsibilities and duties inherent in collectivistic values, however, may help Vietnamese women to overcome their anxiety of screening. Practitioners should be sensitive to Vietnamese culture regardless of their clients’ acculturation status. In addition, practitioners who work in medical settings such as medical social workers should ask their clients whether they prefer a male or female physician to help reduce barriers to cancer screening. Moreover, all practitioners should engage in culturally sensitive and evidence-based practice by ensuring that they are integrating their clinical expertise and the best available evidence into their practice.
Limitations
To adequately interpret the findings, some limitations, such as a small sample size, must be acknowledged. Because participants were recruited from faith-based communities, the findings may not generalize to non faith-based Vietnamese samples. Another limitation is related to recall error that is an inherent challenge in the use of self-reports, such as participants’ self-reports of previous cancer. In addition, social desirability could potentially affect participants’ reporting of past cancer screenings. Studies of the accuracy of self-reported cancer screening procedures, however, suggest self-reports have relatively high agreement with actual behavior (Caplan et al., 2003; Thompson, Taylor, Goldberg, & Mullen, 1999). Future studies could request participants to bring documentation of their screening tests and provide incentives for complying.
Study Strengths
Despite the limitations, this study contributes to the knowledge base in several salient ways. First, previous research related to cancer screening in Vietnamese populations in the United States has primarily focused on West Coast samples (e.g., De Alba et al., 2005; Mock, Nguyen, Nguyen, Bui-Tong, & McPhee, 2006; Nguyen et al., 2006; Tung, Nguyen, & Tran, 2008). This study examined health outcomes of Vietnamese women on the East Coast. The experience of Vietnamese women living in areas with large Vietnamese communities (e.g., West Coast, Texas) is likely atypical for Vietnamese immigrants living elsewhere in the United States (D’Andrade, 2008).
Second, typical cancer screening interventions do not focus on the influence of cultural variables on health behaviors, especially among the Vietnamese population. The present study contributes to the literature by examining proximal-level cultural orientations and their potential role in motivating women to engage in cancer screening. For example, the study provides initial evidence that Vietnamese women’s perceptions of their caretaking roles and the dependence of others can serve as powerful motivators for engaging in cancer-screening behaviors. Our findings help shed light on the importance of studying cultural variables among ethnic minorities.
Although this study was conducted in the United States, we believe that the study’s findings on the interplay among culture, collectivist values, and health behaviors can be applied broadly. Research that has focused on Vietnamese migrants to other countries such as Britain, Canada, and Australia indicate that Vietnamese experience higher incidence and mortality rates of cancers of the liver, stomach, and cervix, while also suffering from disparities in cancer screening in comparison with the native population (Donnelly, McKellin, Hislop, & Long, 2009; Lesjak, Hua, & Ward, 1999; Swerdlow, 1991). The cultural orientations that Vietnamese immigrants bring with them can sometimes polarize differences found between Vietnamese practices and beliefs with those found in social systems, including that of health, of the native population. We believe our findings shed light on how differences in cultural values can act in tandem or against one another in the promotion of health. It is important to understand these cultural influences on health beliefs and behaviors and to build upon them to develop effective programs and health interventions for the Vietnamese.
Conclusions
Our findings illustrate the interplay among demographic, cultural, and cancer screening variables. These findings shed light on how culturally relevant values and roles can help motivate Vietnamese women to adhere to screening guidelines. Future research should examine the mechanisms by which cultural variables (e.g., collectivism and acculturation) influence attitudes toward and receipt of cancer screening by examining potential mediator variables such as health cognitions and perceptions of breast and cervical cancer risk. Interventions designed to increase rates of regular cancer screenings, especially breast and cervical, among Vietnamese women should consider these cultural variables as important tools.
Acknowledgments
The authors express their gratitude to the women who participated in this study and to the leaders of the Vietnamese Church of Martyrs and the Hue Quang Buddhist Temple for their invaluable work and help with this project.
FUNDING
This study was supported by a Ruth L. Kirschstein National Research Service Award (grant #5F31CA136235), the National Cancer Institute, National Institutes of Health, awarded to the first author.
Contributor Information
ANH B. NGUYEN, Division of Cancer Control and Population Sciences, The National Cancer Institute, Rockville, Maryland, USA
TRENETTE T. CLARK, School of Social Work, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, USA
References
- An N, Cochran SD, Mays VM, McCarthy WJ. Influence of American acculturation on cigarette smoking behaviors among Asian American subpopulations in California. Nicotine & Tobacco Research. 2008;10:579–587. doi: 10.1080/14622200801979126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen RM. Behavioral model of families use of health services. Chicago, IL: Center for Health Administration Studies, University of Chicago; 1968. (Rep. No. Research Series No. 25) [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Bates JH, Hofer BM, Parikh-Patel A. Cervical cancer incidence, mortality, and survival among Asian subgroups in California, 1990–2004. Cancer. 2008;113:2955–2963. doi: 10.1002/cncr.23752. [DOI] [PubMed] [Google Scholar]
- Baucom DH, Porter LS, Kirby JS, Gremore TM, Keefe FJ. Psychosocial issues confronting young women with breast cancer. Breast Disease. 2005–2006;23:103–113. doi: 10.3233/bd-2006-23114. [DOI] [PubMed] [Google Scholar]
- Benyamini Y, Blumstein T, Boyko V, Lerner-Geva L. Cultural and educational disparities in the use of primary and preventive health care services among midlife women in Israel. Women’s Health Issues. 2008;18:257–266. doi: 10.1016/j.whi.2007.12.009. [DOI] [PubMed] [Google Scholar]
- Berry JW. Acculturation as varieties of adaptation. In: Padilla AM, editor. Acculturation: Theory, models, and some new findings. Boulder, CO: Westview; 1980. pp. 9–26. [Google Scholar]
- Bich PV. The Vietnamese family in change: The case of the Red River Delta. Padstow, Cornwall: Curzon; 1999. [Google Scholar]
- Braun KL, Mokuau N, Hunt GH, Kaanoi M, Gotay CC. Supports and obstacles to cancer survival for Hawaii’s native people. Cancer Practice. 2002;10:192–200. doi: 10.1046/j.1523-5394.2002.104001.x. [DOI] [PubMed] [Google Scholar]
- Caplan LS, McQueen DV, Qualters JR, Leff M, Garrett C, Calonge N. Validity of women’s self-reports of cancer screening test utilization in a managed care population. Cancer Epidemiological Biomarkers and Prevention. 2003;12:1182–1187. [PubMed] [Google Scholar]
- Champion V, Skinner CS, Hui S, Monahan P, Juliar B, Daggy J, Menon U. The effect of telephone versus print tailoring for mammography adherence. Patient Education and Counseling. 2007;65:416–423. doi: 10.1016/j.pec.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung RC, Bemak F. Lifestyle of Vietnamese refugee women. Journal of Individual Psychology. 1998;54:373–384. [Google Scholar]
- Coughlin SS, Leadbetter S, Richards T, Sabatino SA. Contextual analysis of breast and cervical cancer screening and factors associated with health care access among United States women, 2002. Social Science & Medicine. 2008;66:260–275. doi: 10.1016/j.socscimed.2007.09.009. [DOI] [PubMed] [Google Scholar]
- Couture MC, Nguyen CT, Alvarado BE, Velasquez LD, Zunzunegi MV. Inequalities in breast and cervical cancer screening among urban Mexican women. Preventive Medicine. 2008;47:471–476. doi: 10.1016/j.ypmed.2008.07.005. [DOI] [PubMed] [Google Scholar]
- D’Andrade R. A study of personal and cultural values: American, Japanese, and Vietnamese. New York, NY: Palgrave Macmillan; 2008. [Google Scholar]
- Dao TK, Teten AL, Nguyen Q. Linear and orthogonal models of acculturation and its relations to cultural variables: An examination of the Suinn-Lew Asian Self-Identity Acculturation Scale (SL-ASIA) International Journal of Intercultural Relations. 2011;35:61–68. [Google Scholar]
- Davis RE. The convergence of health and family in the Vietnamese culture. Journal of Family Nursing. 2000;6:136–156. [Google Scholar]
- De Alba I, Ngo-Metzger Q, Sweningson JM, Hubbell FA. Pap smear use in California: Are we closing the racial/ethnic gap? Preventive Medicine. 2005;40:747–755. doi: 10.1016/j.ypmed.2004.09.018. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2012. Washington, DC: U.S. Government Printing Office; 2012. (Current Population Reports, P60-245) [Google Scholar]
- Do H, Taylor VM, Burke N, Yasui Y, Schwartz SM, Jackson J. Knowledge about cervical cancer risk factors, traditional health beliefs, and pap testing among Vietnamese American Women. Journal of Immigrant and Minority Health. 2007;9:109–114. doi: 10.1007/s10903-006-9025-7. [DOI] [PubMed] [Google Scholar]
- Donnelly TT. The health-care practices of Vietnamese-Canadian women: Cultural influences on breast and cervical cancer-screening. Canadian Journal of Nursing Research. 2006;38:82–101. [PubMed] [Google Scholar]
- Donnelly TT, McKellin W, Hislop G, Long B. Socioeconomic influences on Vietnamese-Canadian women’s breast and cervical cancer prevention practices: A social determinant’s perspective. Social Work in Public Health. 2009;24:454–476. doi: 10.1080/19371910802678772. [DOI] [PubMed] [Google Scholar]
- Edwards BK, Noone AM, Mariotto AB, Simard EP, Boscoe FP, Henley SJ, … Ward EM. Annual report to the nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2013 doi: 10.1002/cncr.28509. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez SL, Le GM, Miller T, Undurraga DM, Shema SJ, Stroup A, … Glaser SL. Cancer incidence among Asians in the Greater Bay area. Fremont, CA: Northern California Cancer Center; 2005. [Google Scholar]
- Ho V, Yamal JM, Atkinson EN, Basen-Engquist K, Tortolero-Luna G, Follen M. Predictors of breast and cervical screening in Vietnamse women in Harris County, Houston, Texas. Cancer Nursing. 2005;28:119–129. doi: 10.1097/00002820-200503000-00005. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Pourat N, Breen N, Coughlin S, Abend MT, McNeel TS, Ponce NA. Breast and cervical cancer screening rates of subgroups of Asian American women in California. Medical Care Research and Review. 2007;64:706–730. doi: 10.1177/1077558707304638. [DOI] [PubMed] [Google Scholar]
- Kandula NR, Wen M, Jacobs EA, Lauderdale DS. Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic whites: Cultural influences or access to care? Cancer. 2006;107:184–192. doi: 10.1002/cncr.21968. [DOI] [PubMed] [Google Scholar]
- Kaplan CP, Zabkiewicz D, McPhee SJ, Nguyen T, Gregorich SE, Disogra C, … Jenkins C. Health-compromising behaviors among Vietnamese adolescents: The role of education and extracurricular activities. Journal of Adolescent Health. 2003;32:374–383. doi: 10.1016/s1054-139x(03)00019-3. [DOI] [PubMed] [Google Scholar]
- Lam BT. Self-esteem among Vietnamese American adolescents: The role of self-construal, family cohesion, and social support. Journal of Ethnic & Cultural Diversity in Social Work: Innovation in Theory, Research & Practice. 2005;14:21–40. [Google Scholar]
- Lam TK, McPhee SJ, Mock J, Wong C, Doan HT, Nguyen T, … Luong TN. Encouraging Vietnamese-American women to obtain Pap tests through lay health worker outreach and media education. Journal of General Internal Medicine. 2003;18:516–524. doi: 10.1046/j.1525-1497.2003.21043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee-Lin F, Pett M, Menon U, Nail L, Itano J, Mooney K, Itano J. Cervical cancer beliefs and Pap test screening practices among Chinese American immigrants. Oncology Nursing Forum. 2007;34:1203–1209. doi: 10.1188/07.ONF.1203-1209. [DOI] [PubMed] [Google Scholar]
- Lesjak M, Hua M, Ward J. Cervical screening among immigrant Vietnamese women seen in general practice: Current rates, predictors and potential recruitment strategies. Australian and New Zealand Journal of Public Health. 1999;23:168–173. doi: 10.1111/j.1467-842x.1999.tb01229.x. [DOI] [PubMed] [Google Scholar]
- Luu TD, Leung P, Nash SG. Help-seeking attitudes among Vietnamese Americans: The impact of acculturation, cultural barriers, and spiritual beliefs. Social Work in Mental Health. 2009;7:476–493. [Google Scholar]
- Ma GX, Gao W, Lee S, Wang M, Tan Y, Shive SE. Health seeking behavioral analysis associated with breast cancer screening among Asian American women. International Journal of Women’s Health. 2012;4:235–243. doi: 10.2147/IJWH.S30738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Shive SE, Wang MQ, Tan Y. Cancer screening behaviors and barriers in Asian Americans. American Journal of Health Behavior. 2009;33:650–660. doi: 10.5993/ajhb.33.6.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markus HR, Kitayama S. Cultural variation of the self. In: Goethals GR, Strauss J, editors. Multidisciplinary perspectives on the self. New York, NY: Springer-Verlag; 1991. pp. 18–48. [Google Scholar]
- Marteau TM, Hankins M, Collins B. Perceptions of risk and cervical cancer and attitudes towards cervical screening: A comparison of smokers and non-smokers. Family Practice. 2002;19:18–22. doi: 10.1093/fampra/19.1.18. [DOI] [PubMed] [Google Scholar]
- McCracken M, Olsen M, Chen MS, Jemal A, Thun M, Cokkinides V, Deapen D, Ward E. Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA: A Cancer Journal for Clinicians. 2007;57:190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- Mehnert A, Berg P, Henrich G, Herschbach P. Fear of cancer progression and cancer-related intrusive cognitions in breast cancer survivors. Psycho-Oncology. 2009;18:1273–1280. doi: 10.1002/pon.1481. [DOI] [PubMed] [Google Scholar]
- Meissner HI, Yabroff R, Dodd KW, Leader AE, Ballard-Barbash R, Berrigan D. Are patterns of health behavior associated with cancer screening? American Journal of Health Promotion. 2009;23:168–175. doi: 10.4278/ajhp.07082085. [DOI] [PubMed] [Google Scholar]
- Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes and Control. 2008;19:227–256. doi: 10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mock J, Nguyen T, Nguyen KH, Bui-Tong N, McPhee SJ. Processes and capacity-building benefits of lay health worker outreach focused on preventing cervical cancer among Vietnamese. Health Promotion Practice. 2006;7:223s–232s. doi: 10.1177/1524839906288695. [DOI] [PubMed] [Google Scholar]
- Nguyen AB, Belgrave F, Sholley B. Development of a breast and cervical cancer screening intervention for Vietnamese American women: A community-based participatory approach. Health Promotion Practice. 2010;12:876–886. doi: 10.1177/1524839909355518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen TT, McPhee SJ, Bui-Tong N, Luong TN, Ha-Iaconis T, Nguyen T, … Lam H. Community-based participatory research increases cervical cancer screening among Vietnamese-Americans. Journal of Health Care for the Poor and Underserved. 2006;17:31–54. doi: 10.1353/hpu.2006.0091. [DOI] [PubMed] [Google Scholar]
- Pourat N, Kagawa-Singer M, Breen N, Sripipatan A. Access versus acculturation: Identifying modifiable risk factors to promote cancer screening among Asian American women. Medical Care. 2010;48:1088–1096. doi: 10.1097/MLR.0b013e3181f53542. [DOI] [PubMed] [Google Scholar]
- Reid G, Higgs P, Beyer L, Crofts N. Vulnerability among Vietnamese illicit drug users in Australia: Challenges for change. International Journal of Drug Policy. 2002;13:127–136. [Google Scholar]
- Robbins SP, Chatterjee P, Canda ER. Contemporary human behavior theory: A critical perspective for social work. 2. Boston, MA: Allyn and Bacon; 2006. [Google Scholar]
- Singelis TM. The measurement of interdependent and independent self-construal. Personality and Social Psychology Bulletin. 1994;20:580–591. [Google Scholar]
- Somanchi M, Juon H, Rimal R. Predictors of screening mammography among Asian Indian American women: A cross-sectional study in the Baltimore-Washington metropolitan area. Journal of Women’s Health. 2010;19:433–441. doi: 10.1089/jwh.2008.0873. [DOI] [PubMed] [Google Scholar]
- Suinn RM, Rickard-Figueroa K, Lew S, Vigil P. The Suinn-Lew Asian Self-Identity Acculturation Scale: An initial report. Education and Psychological Measurement. 1987;47:401–407. [Google Scholar]
- Swerdlow AJ. Mortality and cancer incidence in Vietnamese refugees in England and Wales: A follow-up study. International Journal of Epidemiology. 1991;20:13–19. doi: 10.1093/ije/20.1.13. [DOI] [PubMed] [Google Scholar]
- Tang TS, Solomon LJ, McCracken LM. Cultural barriers to mammography, clinical breast exam, and breast self-exam among Chinese American women 60 and older. Preventive Medicine. 2000;31:575–583. doi: 10.1006/pmed.2000.0753. [DOI] [PubMed] [Google Scholar]
- Taylor VM, Schwart SM, Yasui Y, Burke N, Shu J, Lam DH, Jackson JC. Pap testing among Vietnamese women: Health care system and physician factors. Journal of Community Health. 2004;29:437–449. doi: 10.1007/s11123-004-3393-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson B, Taylor V, Goldberg H, Mullen M. Mammography status using patient self-reports and computerized radiology database. American Journal of Preventive Medicine. 1999;17:203–206. doi: 10.1016/s0749-3797(99)00068-9. [DOI] [PubMed] [Google Scholar]
- Triandis HC. Individualism and collectivism. San Francisco, CA: Westview; 1995. [Google Scholar]
- Tung WC, Nguyen DHT, Tran DN. Applying the transtheoretical model to cervical cancer screening in Vietnamese-American women. International Nursing Review. 2008;55:73–80. doi: 10.1111/j.1466-7657.2007.00602.x. [DOI] [PubMed] [Google Scholar]
- Walsh MC, Trentham-Dietz A, Schroepfer TA, Reding DJ, Campbell B, Foote ML, … Cleary JF. Cancer information sources used by patients to inform and influence treatment decisions. Journal of Health Communication. 2010;15:445–463. doi: 10.1080/10810731003753109. [DOI] [PubMed] [Google Scholar]
- Wang JH, Sheppard VB, Schwartz MD, Liang W, Mandelblatt JS. Disparities in cervical cancer screening between Asian American and Non-Hispanic white women. Cancer Epidemiology, Biomarkers & Prevention. 2008;17:1968–1973. doi: 10.1158/1055-9965.EPI-08-0078. [DOI] [PubMed] [Google Scholar]
- Yi JK. Vietnamese American college students’ knowledge and attitudes toward HIV/AIDS. Journal of American College Health. 1998;47:37–42. doi: 10.1080/07448489809595617. [DOI] [PubMed] [Google Scholar]
- Yi JK, Reyes-Gibby CC. Breast cancer screening practices among low-income Vietnamese women. International Quarterly of Community Health Education. 2002;21:41–49. [Google Scholar]