Abstract
Background
The round window membrane (RWM) has become the preferred route, over cochleostomy, for introduction of cochlear implant electrode as it minimizes inner ear trauma. However, in absence of tool designed for creating precise perforation, current practices lead to tearing of the RWM and significant intracochlear pressure fluctuations. Based on the mechanical properties of the RWM, we have designed a multi-serrated needle to create consistent holes in the human RWM without membrane tearing or damaging inner ear structures.
Methods
A four and eight-serrated needle were designed and produced with wire electrical discharge machining (EDM). The needle’s ability to create RWM perforation was tested in de-identified temporal bones acquired commercially with the assistance of a micromanipulator. Subsequently, the specimens were imaged under light and scanning electron microscopy (SEM).
Results
The needles created consistent, appropriately sized holes in the membrane with minimal tearing. While a four-serrated crown needle made rectangular/trapezoid perforations, the octagonal crown formed smooth oval holes within the membrane. While designed for single use, the needle tolerated repeated use without significant damage.
Conclusions
The serrated needles formed precise perforations in the RWM while minimizing damage during cochlear implantation. The octagonal needle design created the preferred oval shaped perforation better than the quad needle.
Keywords: Round Window Membrane, Cochlear Implant Electrode, Electron Discharge Machining
INTRODUCTION
Cochlear implants are commonly used prosthetic devices that have been shown to effectively improve the hearing, vocalization, mood, and overall quality of life in patients with profound sensorineural hearing loss refractory to hearing aids. While traditional cochlear implants required the creation of a cochleostomy to reach the inner ear, in recent years, with newer, slimmer electrode designs and the introduction of small “hybrid” electrodes have allowed the use of the RWM as a portal for electrode placement [1]. It is estimated that as many as 75–85% of cochlear implants are now inserted via the RWM. Use of the RWM avoids traumatic disruption of the cochlea’s bony walls, along with the significant risk of hearing loss or vestibular dysfunction that comes with it.[2, 3]
However, to date, no device exists to create small, precise holes in the RWM to aid in electrode entry. In its absence, clinicians are forced to utilize needles or tools intended for other purposes that put the patient at risk for damage to the scala tympani walls, the auditory nerve, the cochlear aqueduct or the modiolar vein [4]. These include the use of a regular hypodermic needle tip, Beaver blade, Rosen needle, and rarely a laser to make an incision and/or perforation in the membrane. The resulting fenestration is an asymmetric oval or irregular shape, is often larger than necessary, and can have a floating hanging edge. As these tools are large, the tip of the instrument may traumatize the intracochlear structures during fenestration. Additionally, the force of the needle displaces fluid into the cochlea increasing inner ear pressure that may damage the fragile neuroepithelia of the hearing organ. As the surgeon tries to place the electrode through the resultant imprecise hole in the membrane, sometimes the hole is too small to allow the electrode to pass through it. He/She then has to decide to either remove the electrode and make a larger perforation or force the electrode through — either way risking tearing part of the membrane or missing and making a second hole altogether. The irregular shape of membrane around the electrode allows perilymph to leak out into the middle ear space or infection from the middle ear to extend into the inner ear. Thus, there is a real need for a tool specially designed to create a precise RWM perforation to facilitate electrode insertion that minimizes the risk of cochlear damage perilymph leakage into the middle ear space.
Based on our previous studies of the mechanical properties of the RWM, we have designed serrated, crown-shaped needle, with 4 or 8 serrations, for creating precise RWM perforation with one push of the needle [5] [6]. This needle would minimize trauma to the patient’s inner ear and minimize leakage of cochlear perilymph into the middle ear. In this study, we test the efficacy of the serrated needle, fabricated both in our lab (4 serrations) as well as by a commercial vendor (eight serrations) using good manufacturing practices (GMP), to make precise perforations in cadaveric human RWM.
MATERIALS AND METHODS
Needle Design and Preparation
Based on our previous studies of the anatomy and mechanical properties of the RWM and testing with larger prototype needles, we designed a needle to most effectively and reproducibly perforate the membrane while minimizing tearing of the membrane and intracochlear pressure. The serrated needle design was chosen to create RWM microperforations at the serrated tips that would interconnect to create a perforation while minimizing tear. The needle has a hollow shaft to allow some fluid to enter from the inner ear upon penetration, theoretically limiting the pressure increase seen in the cochlea and preventing turbulent damage to the scala tympani.
Two different designs, 4 and 8 serrated needles, were tested. The four-pronged needle had an outer diameter of 0.8 mm, with inner diameter 0.64 mm (Figure 1). It contained an arcuate bottom and trailing edge between each of the four points to minimize the force of perforation. Serrated crown tips were 2 mm in length before coalescence. The octagonal needle had the same diameter and contained the same arcuate bottoms and trailing edges as the quad needle (Figure 2). Crown tips were 0.5 mm in length.
Figure 1.
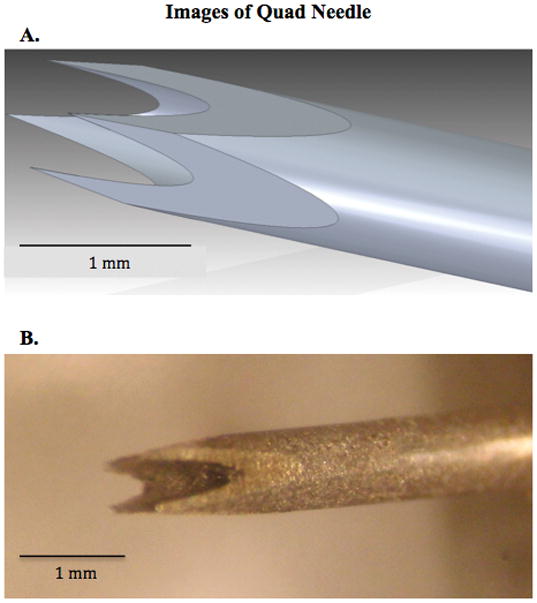
A. Graphic design of a 0.8 mm outer diameter four-pronged needle. Note the trailing edge and arcuate bottoms to the design. B. Photograph of a four-pronged single needle from an ultra-thin hypodermic needle, based on 1A. The use of EDM allowed the creation of a precise, symmetric needle that withstood multiple RWM perforations while forming a trapezoid-shaped hole.
Figure 2.
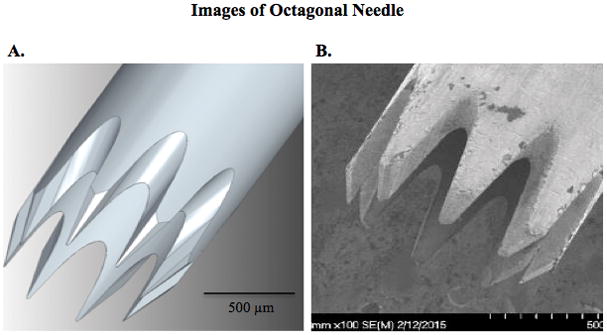
A. Graphic design of 0.8 mm octagonally-serrated, hollow needle. Trailing edge and arcuate bottoms are similar to quad needle in Figure 1, though individual points are closer to one another, with decreased angles for EDM cutting. Tip length is approximately 0.5 mm before coalescence. B. SEM image of 3D-CNC prototype octagonal needle. Minor blemishes can be seen along the needle shaft, but needle tips appear symmetric and closely resemble 2A.
For the quad prototype, the design specifications were entered into a local wire EDM program (Mitsubishi RA90, Tokyo, Japan) and produced in the Department of Mechanical Engineering, Columbia University. Octagonal needles were produced by 3D-CNC (Hutchinson, MN), using good manufacturing practices (GMP), with wire EDM. Needle tips were connected to the end of a Rosen needle handle with optically-fixed glue.
Tissue preparation and perforation
Fresh, frozen human temporal bones were purchased from a commercial vendor (Science Care, Phoenix, AZ). Samples were drilled in the Columbia University Department of Otolaryngology/H&NS temporal bone lab, as well as the Columbia University College of Physicians and Surgeons (P&S) Gross Anatomy lab. Temporal bones were dissected to expose the RWM from both the middle and inner ear sides, including removal of middle ear “false” membranous RWM coverings and separation of the basilar membrane. The RWM was isolated with a thin ring of surrounding bony niche, and transported in normal saline solution. Single perforations were performed under light microscopy with the assistance of a micromanipulator puncturing completely through the membrane, beyond the individual crown length. The needle was then slowly removed.
Imaging
Each RWM/RW niche was embedded in a plastic 3D-printed slide with the use of flowable dental composite. Slides were imaged with light microscopy under Z-stack mode, a composite of images every 5 μm for 300 μm (Olympus FSX-100, Toyko, Japan). Perforations were measured with ImageJ64 software. Samples were fixed in formaldehyde then serially dried with 10% increases in ethanol solutions, 50 to 100%. Membranes were soaked in 50% then 100% hexamethyldisilazane (HMDS), which was subsequently evaporated under a fume hood. Samples were coated with 10 nm gold-palladium (Cressington Sputter Coater 108auto, Watford, England) and imaged with SEM (Hitachi 4700, Tokyo, Japan).
RESULTS
Quad Needle Design
The EDM was successful in creating a symmetric needle prototype; Figure 1B shows a prototype of the quad needle. A given quad needle was able to perforate multiple samples while retaining its shape and created trapezoid shaped holes. Figure 3A shows the process of RWM perforation with the quad needle, while Figure 3B shows the hole made by the quad needle. Post-perforation visualization of such needles did not show substantial bending of the crown tips. While the needle remained sharp and undamaged with repeated use, contacting temporal bone or other hard surfaces did deform the needle tip.
Figure 3.

A. Middle ear view of quad needle in the process of perforating isolated human RWM. The bony niche can be seen surrounding the membrane, which is deflected inward from the force prior to perforation. B. Asymmetric, four-sided shape of RWM perforation from quad needle. A remaining attached flap containing the tissue can be seen folded over the top portion of the hole.
The four crown design was associated with irregular trapezoid perforation and size variability. Furthermore, the individual crowns were noted to be too long for the shallow scala tympani space. One trial in situ led to the crown tips striking the basilar membrane before a complete perforation was made; this observation was further supported by micro-CT analysis of human temporal bones.
Octagonal Needle Design
The octagonal design was refined based on the initial results with the quad needles; the needle tips were shortened to avoid intracochlear damage and serration angles were sharpened. The finer octagonal needle was manufactured by 3D-CNC, Inc. (Hutchinson, MN) as the in-house EDM was not suitable for its production. An SEM image of one prototype is seen in Figure 2B. Octagonal needles were subsequently tested on six commercially-acquired human temporal bones with the RWM isolated. The 0.8 mm outer diameter prototype created slightly elongated oval perforations in the RWM (Figure 4). Puncturing the membrane either removed that part of the RWM completely or produced a single flap that remained connected to the membrane. The average hole diameter was 0.96 x 0.70 mm (standard deviations 0.15 × 0.09 mm, respectively). The average area of these perforations was 1.1% different than the area of the microneedle device (0.5080 +/− 0.1071 mm2). Similar to the quad needle, a given octagonal needle prototype was tested on three temporal bone samples each (a total of two prototypes were used for an n=6). Each needle made smooth perforations and formed oval holes for all three samples tested. Post-perforation imaging via light microscopy did not show significant changes to the crown shape, though there was some dulling of the serrations (Images).
Figure 4.
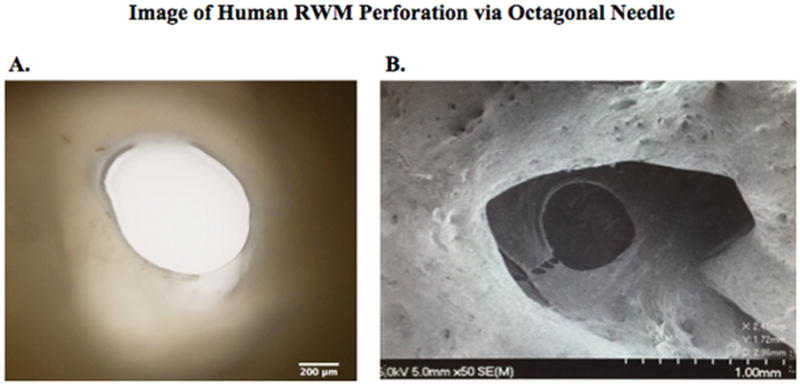
A. Light microscope image of oval RWM perforation formed by octagonal needle prototype. This portion of the membrane was completely removed, with no evidence of membrane tearing on visualization. B. SEM image of a RWM post-perforation with the octagonal needle. The hole is nearly circular, with a minor rip in the bottom right corner that would likely heal without effecting membrane structural stability.
DISCUSSION
In this report, we demonstrate that multi-serrated needle is capable of making precise holes in the RWM without tearing the membrane. The needle prototype in this study withstood repeated use; however, we envision that the needle would be a single-use device in the operating room. With single use, the sharp serrations will precisely and reliably perforated the RWM as demonstrated in this study. While both the quad and octagonal needles created precise holes, the octagonal needle created the preferred oval shape deemed more suitable for cochlear implant electrode insertion. The oval hole is slightly larger than the outer diameter of the needle and elongated in the membrane’s major axis. The elongated shape was expected based on the manner in which the RWM’s collagen fibers pull the remaining tissue along their major axis after perforation.
The design of the needle is responsible for both its precision and lack of tearing. The use of multiple small tips limits the force required for each prong to perforate the membrane, thus minimizing the risk of tearing, as the area in which the tension around a hole can be propagated into a tear is proportional to the size of the hole. That is why the use of a large, single-tip hypodermic or Rosen needle is universally associated with the tear of the RWM. Resultant slits give the electrode a very loose-fitting, leaky cover, or may not be large enough and lead to membrane tearing upon forced insertion. Furthermore, the hollow design of the needle should theoretically reduce intracochlear pressures during perforation seen with use of less precise tools [7].
In the current study, a needle with an outer diameter 0.8 mm was used, the diameter of several cochlear implant electrodes. The octagonal design is easily scalable to a needle with a diameter of 0.4 mm, 0.6 mm, or any other size to more precisely match any electrodes currently on the market. As technology changes the diameter can easily be adapted further to accommodate differences in electrode diameter between other cochlear implant models. As in these trials, future needles will be attached to the end of a long hand-held device similar to a Rosen needle. The device will be completely manual for the surgeon’s use, and will have a curved shape to match the anatomic approach to the RWM.
A variety of alternatives are available to surgeons to create RWN perforation for electrode insertion during cochlear implantation. These include hypodermic needles, Rosen needles, or Beaver blades — devices that were created for other purposes — to incise and perforate the membrane. The use of these instruments is associated with significant intracochlear pressures [7], and the resultant slits give the electrode a very loose-fitting, leaky cover, or may not be large enough and lead to membrane tearing upon forced insertion. A thin, hollow, symmetric, serrated needle should theoretically minimize the force needed for perforation and decrease the pressure change within the inner ear but remains to be demonstrated. Lasers have been proposed as a possible alternative method for RWM perforation. One obvious shortcoming of the use of lasers is the size and shape restriction of commercially available laser devices; both CO2 and YAG lasers are typically too large for our purposes [8, 9]. CO2, Argon, or KTP lasers can theoretically have smaller spot sizes, but the surgical lasers currently on the market cannot accomplish our goals. These devices are designed for wider orifices or open surgical fields, and some would not be able to effectively reach the anatomically hidden RWM. Lasers are inherently more expensive than a manual perforator such as tested in this study, costing tens of thousands of dollars or more for a hospital to purchase, and even more to design. Even then, there are various safety concerns with lasers, from accidental burning of non-targeted tissue, to the destruction of RWM tissue and limitation of the RWM’s intrinsic healing/formation of a well-sealed electrode post-implantation. Lastly, laser energy penetrating beyond the surface tissue may cause heat damage to the hair cells or other structures within the inner ear, or lead to significant perilymph evaporation [9].
In summary, the quad and octagonal serrated needle are effective in creating precise perforation of RWM with out tearing. Their efficacy in the operating room to create an appropriate size hole in the RWM during cochlear implant surgery, without deleterious increase in intracochlear pressure, remains to be demonstrated.
Acknowledgments
The research reported in this publication was supported by Columbia-Coulter Translational Research Partnership. Additional funding was provided by the National Institute On Deafness And Other Communication Disorders of the National Institutes of Health under Award Number R01DC014547. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Relevant Financial Disclosures: Dr. Anil Lalwani serves on the Medical Advisory Board of Advanced Bionics Corporation. The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1.Roland PS, Wright CG, Isaacson B. Cochlear implant electrode insertion: The round window revisited. Laryngoscope. 2007;117(8):1397–1402. doi: 10.1097/MLG.0b013e318064e891. [DOI] [PubMed] [Google Scholar]
- 2.Adunka O, et al. Cochlear implantation via the round window membrane minimizes trauma to cochlear structures: A histologically controlled insertion study. Acta Oto-Laryngologica. 2004;124(7):807–812. doi: 10.1080/00016480410018179. [DOI] [PubMed] [Google Scholar]
- 3.Briggs RJS, et al. Comparison of round window and cochleostomy approaches with a prototype hearing preservation electrode. Audiology and Neurotology. 2006;11(SUPPL 1):42–48. doi: 10.1159/000095613. [DOI] [PubMed] [Google Scholar]
- 4.Gaylor JM, et al. Cochlear implantation in adults: A systematic review and meta-analysis. JAMA Otolaryngology - Head and Neck Surgery. 2013;139(3):265–272. doi: 10.1001/jamaoto.2013.1744. [DOI] [PubMed] [Google Scholar]
- 5.Watanabe HKJ, Lalwani A. Microanatomic Analysis of the ROund Window Membrane by White Light Interferometry and Microcomputed Tomography for Mechanical Amplification. Otology and Neurotology. 2014;35(4):672–678. doi: 10.1097/MAO.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 6.Kelso CM, et al. Microperforations significantly enhance diffusion across round window membrane. Otology and Neurotology. 2015;36(4):694–700. doi: 10.1097/MAO.0000000000000629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mittmann P, Ernst A, Todt I. Intracochlear pressure changes due to round window opening: A model experiment. Scientific World Journal, 2014. 2014 doi: 10.1155/2014/341075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lumenis I, editor. Lumenis CO2 Laser Accesories. 2008. [Google Scholar]
- 9.Oswal V, et al. In: Principles and Practice of Lasers in Otorhinolaryngology and Head and Neck Surgery. 2. Oswal V, editor. Vol. 1. Amsterdam, The Netherlands: Kugler; 2014. p. 484. [Google Scholar]


