Highlights
-
•
There are few specific reports of late medial instability after TKA.
-
•
We described two cases of late medial instability of the knee due to hip disease after TKA, which required revision TKA.
-
•
Both cases required revision TKA with constrained knee prostheses due to the severe medial instability.
-
•
The late medial instability in current study was partially due to the same mechanism underlying the long-leg arthropathy and coxitis knee.
-
•
Constrained prostheses were applied for both patients, providing moderately good results.
Keywords: Late medial instability, Total knee arthroplasty, Constrained prosthesis
Abstract
Introduction
There are few specific reports of late medial instability after total knee arthroplasty (TKA). We described two cases of late medial instability of the knee due to hip disease with osteoarthritis or rheumatoid arthritis after TKA, which required revision TKA.
Presentation of cases
An 82-year-old woman experienced right femoral neck fracture due to a fall that required conservative treatment at age 77 years and underwent left TKA at age 80 years. A 68-year-old woman underwent left TKA at age 54 years, right TKA at age 64 years, and left THA at age 67 years. Both cases required revision TKA with constrained knee prostheses due to the severe medial instability. Hip-knee-ankle (HKA) angle, range of motion (ROM), Knee Society score (KSS) and functional score (FS) were evaluated pre- and postoperatively. Their respective HKA angle improved from 134° and 155° preoperatively to 184° and 179° postoperatively. KSS improved from −4 and 53 points to 59 and 100 points, respectively. FS improved from −10 and 58 points to 25 and 90 points, respectively. In the 82-year-old woman, ROM did not improve from −10–90° to −20–90°. On the other hand, in the 68-year-old woman, ROM improved from 0–110° to 0–125°. The late medial instability in the current case report was partly due to a similar mechanism underlying the long leg arthropathy and coxitis knee caused by hip joint degeneration.
Conclusions
Constrained prostheses were applied for both patients, providing moderately good short-term results.
1. Introduction
Total knee arthroplasty (TKA) is a procedure that generally results in successful outcomes and has a 10-year revision rate of 6.2% [1]. However, owing to the large number of procedures routinely performed, this apparently small percentage of failures constitutes a significant number of patients. It has been reported that most common causes for revision surgery include aseptic loosening, infection and wear [2] while polyethylene wear, component loosening, ligament or extensor mechanism attenuation, and patient factors such as connective tissue disorders or inflammatory arthritis make up some of the causes of late instability after TKA [3], [4]. Late instability is one of the most common causes of revision TKA [5], [6], [7]; nonetheless, there are very few specific reports of late medial instability after TKA. Thus, we describe here two cases of late medial instability of the knee due to hip disease after TKA, which required revision TKA. Additionally, we discuss the mechanism of late medial instability after TKA.
2. Presentation of cases
2.1. Case 1
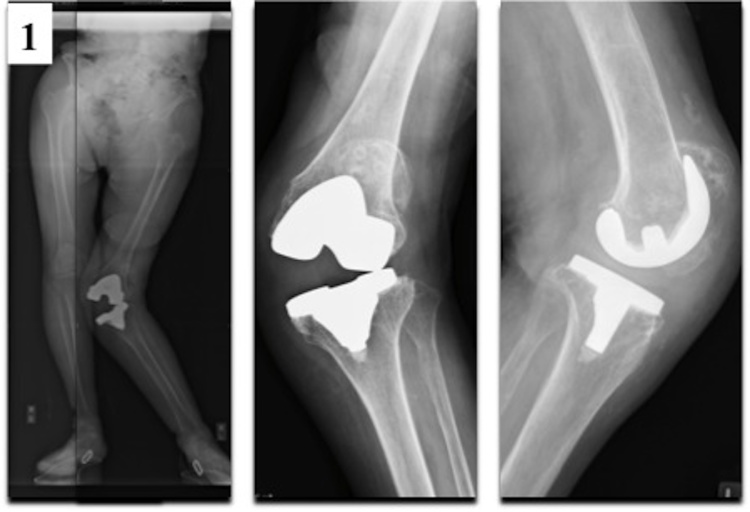
An 82-year-old woman was referred to our hospital with pain in the left knee and right hip. Her knee history began at age 78 years, when she first experienced left knee pain without an apparent cause. She was diagnosed with severe osteoarthritis (OA) of the left knee and underwent TKA using a cruciate-retaining (CR) design at age 80 years due to persistent knee pain (Table 1). Her hip history began at age 77 years, when she had right femoral neck fracture due to a fall that required conservative treatment. Post-treatment, the right femoral neck fracture was found to have deformed bony union with slight externally rotated healing. Subsequently, she was unable to walk, except with the aid of a wheelbarrow and had no pain in the right hip until 3 months prior to presentation for current case report when she experienced right hip pain again with no apparent cause. Physical examination of her left knee revealed decreased range of motion (ROM) from −10° in extension to 90° in flexion as well as severe medial instability. Preoperative radiographs showed severe valgus deformity, with a hip-knee-ankle (HKA) angle of 134° (46° valgus), and chronic patellar fracture of which she was unaware (Fig. 1). Her left leg was 3 cm longer than the contralateral side. Her Knee Society score (KSS) and functional score (FS) were −4 and −10 points, respectively. The late medial instability of the knee was developed a year after primary TKA of her left knee. In this case, total hip arthroplasty (THA) at the contralateral side was initially performed to resolve the severe hip OA and the leg length discrepancy. After the THA procedure, revision TKA was then performed. Intraoperative findings suggested that the late medial instability of the knee was caused by partial tear of the medial collateral ligament and polyethylene insert wear. The extensor mechanism was repaired using artificial ligament augmentation with partial patellectomy due to failure of the extensor mechanism caused by pseudarthrosis of the patella. Loosening of the femoral and tibial components was not observed. The lateral collateral ligament was intact. For this patient, we opted for a hinged prosthesis (NexGen Rotating Hinge Knee, Zimmer, Warsaw, Indiana) due to the fixed valgus deformity, severe medial instability, and persistent failure of the extensor mechanism even after repairing it with the artificial ligament. The postoperative hospital stay for rehabilitation lasted one and a half months, after which she was discharged with a pick-up walker. The physical or radiographic examination follow-up timings were 3, 6, 12, and 24 months post-surgery respectively. Two years after the surgeries, her HKA angle, KSS and FS improved to 184° (4° varus), 59 points, and 25 points, respectively, although her ROM had not improved (from −20° in extension to 90° in flexion) (Fig. 2).
Table 1.
Surgical history.
| Case | Age | Surgery |
|---|---|---|
| Case 1 | 80 | Left TKA |
| Case 2 | 56 | Left TKA |
| 64 | Right TKA | |
| 67 | Left THA |
TKA: total knee arthroplasty, THA: total hip arthroplasty.
Fig. 1.
Preoperative radiographs of Case 1 showed a severe valgus deformity of left knee joint, with a hip-knee-ankle angle of 134° (46° valgus).
Fig. 2.
In postoperative radiographs of Case 1, a hip-knee-ankle angle had improved to 184° (4° varus) by revision total knee arthroplasty with a hinged prosthesis.
2.2. Case 2
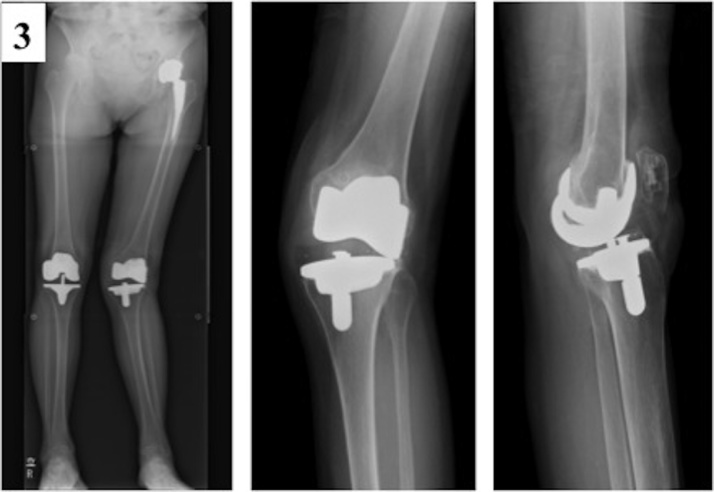
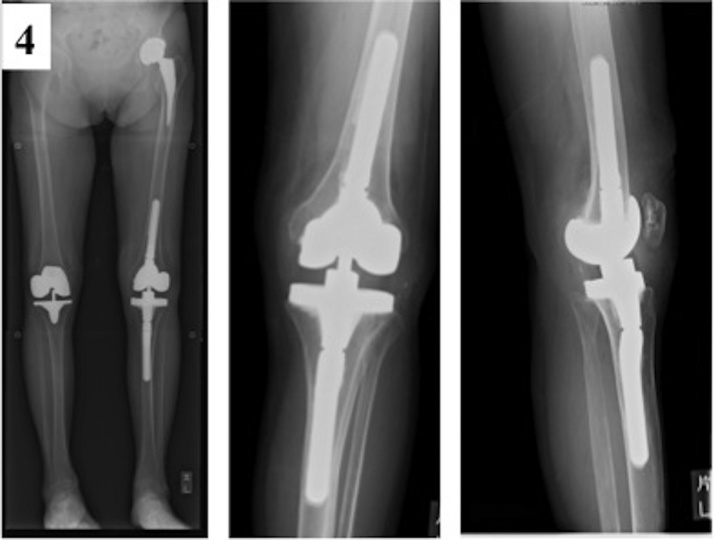
A 68-year-old woman was referred to our hospital with instability in the left knee. She had been diagnosed with rheumatoid arthritis (RA) 25 years prior. Her knee history began at age 55 years, when she first experienced left knee pain. She initially underwent left TKA using a CR design 12 years prior to presentation for the current case report. Then she underwent right TKA using a posterior stabilized (PS) design 8 years after the left TKA. Her hip history began at around 65 years of age, when she first experienced left hip pain with no apparent cause. She underwent left THA a year prior to presentation for the current case report (Table 1). Subsequently, she did not experience any left knee pain and instability until 6 months prior to presentation for the current case report. Physical examination of her left knee revealed slightly decreased ROM from 0° in extension to 110° in flexion as well as severe medial instability. Preoperative radiographs showed valgus deformity, with an HKA angle of 155° (25° valgus) (Fig. 3). There was no difference in the length of her legs. KSS and FS were 53 and 58 points, respectively. Her late medial instability of the left knee developed slowly for the 12 years following the primary TKA, after which revision TKA was performed. Intraoperative findings suggested that the medial instability was caused by partial tear of the medial collateral ligament and polyethylene insert wear. Loosening of the femoral and tibial components was not observed. The lateral collateral ligament was intact. For this patient, we opted for a constrained condylar knee prosthesis (NexGen Legacy Constrained Condylar Knee, Zimmer, Warsaw, Indiana) due to the fixed valgus deformity and severe medial instability. The postoperative hospital stay for rehabilitation lasted three weeks, after which she was discharged with a cane. The physical or radiographic examination follow-up timings were 3, 6, 12, and 24 months respectively post-surgery. Two years after the surgeries, her HKA angle, ROM, KSS and FS improved to 179° (1° valgus), from 0° in extension to 125° in flexion, 100 points, and 90 points, respectively (Fig. 4). Both surgeries were performed by the same surgeon, the senior author (T.M.). No complications were observed in both case descriptions; however, written informed consents were obtained from both patients before publishing this case report.
Fig. 3.
Preoperative radiographs of Case 2 showed a valgus deformity, with a hip-knee-ankle angle of 155° (25° valgus).
Fig. 4.
In postoperative radiographs of Case 2, a hip-knee-ankle angle had improved to 179° (1° valgus) by revision total knee arthroplasty with a constrained condylar knee prosthesis.
3. Discussion
The most important finding in the current case report was the late medial instability after TKA, which occurred following hip disease and could be treated with revision TKA using hinged or constrained prostheses.
It has been reported that common causes of TKA failure include infection, instability, stiffness, and polyethylene wear [8], [9], [10]. The instability after TKA could also be caused by polyethylene wear, component loosening, ligament or extensor mechanism attenuation, as well as patient factors (e.g. connective tissue disorders or inflammatory arthritis) [3], [4]. Late medial instability of the knee after primary TKA is relatively rare among the causes of revision TKA.
In both case descriptions of the current case report, the hip joint developed OA or RA changes prior to the development of the knee disorder. Previous studies have reported clinical knee conditions such as long leg arthropathy and coxitis knee. Long leg arthropathy is a degenerative joint disease that develops, after several years, in the hip and/or knee of the longer legs of people with unequal leg lengths. The knee of the longer leg is particularly prone to earlier and more severe damage. This pattern is exemplified in the case descriptions of varied etiology described here, including arthritis and arthrosis [11]. Coxitis knee is a severe disorder of the hip joint that leads to secondary osteoarthritis of the contralateral or ipsilateral knee joint. Generally, the femur rotates internally at the time of heel contact with the ground. However, the femur is unable to rotate after hip arthrodesis or contracture, leading to excessive stress on the contralateral or the ipsilateral knee joint, eventually resulting in valgus or varus knee deformity [12], [13]. The late medial instability after TKA in the current case report was partially due to the same mechanism as the long leg arthropathy or coxitis knee, which was caused by degenerative hip joint changes.
The treatment options for late medial instability of the knee were reported to include the use of constrained or unconstrained prostheses, ligamentous reconstruction, and augmentation [14], [15], [16]. However, there is no consensus on the management of medial instability of the knee following TKA. Several studies have reported successful management of the medial collateral ligament disruptions with either repair, augmentation or the use of unconstrained implant [15], [16]. Although it was reported that the use of increased constraint enhances coronal stability in cases of medial collateral ligament laxity or incompetence [17], [18], [19], it also resulted in increased stress on the implant-cement as well as implant-bone interfaces, which led to loosening [17], [18], [20]. Therefore, the use of constraints in routine primary TKA is inappropriate. However, a hinged prosthesis was used in Case 1 mainly due to failure of the extensor mechanism even after artificial ligament repair. Although the use of a hinged prosthesis in Case 2 was appropriate due to the severe medial instability, the loosening of the component was thought to have occurred in the early postoperative stage because of her weak bone quality. Therefore, the constrained condylar knee prosthesis was used in Case 2.
In the present study, we evaluated outcomes of patients with KSS and FS. These scoring systems are knee joint specific questionnaires originally developed and validated in 1989 for use in assessing the outcome of TKA [21]. KSS (0–100 points) is divided into pain (0–50 points) and a knee score that assesses range of motion, stability, and alignment (0–50 points). FS (0–100 points) is based on walking distance (0–50 points) and ability to climb stairs (0–50 points) with deductions for use of a gait aid (0–20 points). KSS includes range of motion and alignment measurements, and this may partially contribute to its popularity. Accurate coronal alignment of the knee implant is important for implant survival and function outcomes in TKA [22], and ROM is an important factor for many activities of daily living [23]. Both KSS and FS improved from preoperative to postoperative in both cases in current study. However, further long-term follow-up is needed. The present work has been reported in line with the SCARE criteria [24].
4. Conclusions
Late medial instability of the knee after primary TKA is a relatively rare cause of revision TKA. We observed two cases of late medial instability after TKA. This was partly due to a similar mechanism as that of long leg arthropathy or coxitis knee, caused by degenerative hip joint changes. There is no consensus on the management of medial instability of the knee following TKA. However, constrained prostheses were applied in the cases of fixed valgus deformity, severe medial instability or failure of the extensor mechanism of the knee, leading to relatively good short-term results in the current case report.
Conflict of interest
The authors have no conflict of interest.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical Approval
In our case report was not made no experimentation, you just described our clinical practice.
Consent
Written informed consents were obtained from the both patients for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in Chief of this journal on request..
Author’s contribution
All contributors who do not meet the criteria for authorship should be listed in an acknowledgements section. Examples of those who might be acknowledged include a person who provided purely technical help, writing assistance or a department chair who provided only general support.
Registration of Research Studies
My UIN is researchregistry 2365.
Guarantor
Dr. Tomoyuki Matsumoto.
Contributor Information
Masanori Tsubosaka, Email: masanori.tsubosaka@gmail.com.
Tomoyuki Matsumoto, Email: matsun@m4.dion.ne.jp.
Koji Takayama, Email: kojitakayama1978@gmail.com.
Naoki Nakano, Email: naokix1981@yahoo.co.jp.
Ryosuke Kuroda, Email: kurodar@med.kobe-u.ac.jp.
References
- 1.Pabinger C., Berghold A., Boehler N., Labek G. Revision rates after knee replacement: cumulative results from worldwide clinical studies versus joint resisters. Osteoarthr. Cartil. 2013;21(2):263–268. doi: 10.1016/j.joca.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 2.Sadoghi P., Liebensteiner M., Agreiter M., Leithner A., Böhler N., Labek G. Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J. Arthroplasty. 2013;28(8):1329–1332. doi: 10.1016/j.arth.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 3.Matthew A., Glenn D., Victor M. AAOS; 2014. Surgical Management of the Unstable Total Knee Arthroplasty. [Google Scholar]
- 4.Song S.J., Detch R.C., Maloney W.J., Goodman S.B., Huddleston J.l., 3rd Causes of instability after total knee arthroplasty. J. Arthroplasty. 2014;29(2):360–364. doi: 10.1016/j.arth.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 5.Vince K.G., Abdeen A., Sugimori T. The unstable total knee arthroplasty: causes and cures. J. Arthroplasty. 2006;21(4 Suppl. 1):44–49. doi: 10.1016/j.arth.2006.02.101. [DOI] [PubMed] [Google Scholar]
- 6.Parratte S., Pagnano M.W. Instability after total knee arthroplasty. J. Bone Joint Surg. Am. 2008;90(1):184–194. [PubMed] [Google Scholar]
- 7.Callaghan J.J., O'rourke M.R., Saleh K.J. Why knees fail: lessons learned. J. Arthroplasty. 2004;19(4 Suppl. 1):31–34. doi: 10.1016/j.arth.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 8.Fehring T.K., Odum S., Griffin W.L., Mason J.B., Nadaud M. Early failures in total knee arthroplasty. Clin. Orthop. Relat. Res. 2001;392:315–318. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 9.Hossain F., Patel S., Haddad F.S. Midterm assessment of causes and results of revision total knee arthroplasty. Clin. Orthop. Relat. Res. 2010;468(5):1221–1228. doi: 10.1007/s11999-009-1204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vessely M.B., Whaley A.L., Harmsen W.S., Schleck C.D., Berry D.J. Long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin. Orthop. Relat. Res. 2006;452:28–34. doi: 10.1097/01.blo.0000229356.81749.11. [DOI] [PubMed] [Google Scholar]
- 11.Dixion A.S., Campbell-smith S. Long leg arthropathy. Ann. Rheum. Dis. 1969;28(4):359–365. doi: 10.1136/ard.28.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smillie I.S. 2nd ed. Churchill Livingstone; Edinburgh, London: 1974. Angular Deformity. Diseases of the Knee Joint; pp. 311–312. [Google Scholar]
- 13.Ide S., Nishifuru K., Itoh J., Hotokebuchi T. Clinical study of coxitis knee. Orthop. Surg. Traumatol. 2002;51:749–752. [Google Scholar]
- 14.Hartford J.M., Goodman S.B., Schurman D.J., Knoblick G. Complex primary and revision total knee arthroplasty using the condylar constrained prosthesis. An average 5 year follow up. J. Arthroplasty. 1998;13(4):380–387. doi: 10.1016/s0883-5403(98)90002-x. [DOI] [PubMed] [Google Scholar]
- 15.Jung K.A., Lee S.C., Hwang S.H., Jung S.H. Quadriceps tendon free graft augmentation for a midsubstance tear of the medial collateral ligament during total knee arthroplasty. Knee. 2009;16(6):479–483. doi: 10.1016/j.knee.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 16.Leopold S.S., McStay C., Klafeta K., Jacobs J.J., Berger R.A. Primary repair of intraoperative disruption of the medial collateral ligament during total knee arthroplasty. J. Bone Joint Surg. Am. 2001;83-A:86–91. doi: 10.2106/00004623-200101000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Kim T.H., Kim J.S., Oh S.W. Total knee arthroplasty in neuropathic arthropathy. J. Bone Joint Surg. Br. 2002;84(2):216–219. doi: 10.1302/0301-620x.84b2.12312. [DOI] [PubMed] [Google Scholar]
- 18.Lachiewicz P.F., Soileau E.S. Ten-year survival of and clinical results of constrained components in total knee arthroplasty. J. Arthroplasty. 2006;21(6):803–808. doi: 10.1016/j.arth.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 19.Sculco T.P. Total condylar III prosthesis in ligament instability. Orthop. Clin. N. Am. 1989;20(2):221–226. [PubMed] [Google Scholar]
- 20.Koo M.H., Choi C.H. Conservative treatment for the intraoperative detachment of medial collateral ligament from the tibial attachment site during primary total knee arthroplasty. J. Arthroplasty. 2009;24(8):1249–1253. doi: 10.1016/j.arth.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 21.Insall J.N., Dorr L.D., Scott R.D., Scott W.N. Rationale of the knee society clinical rating system. Clin. Olthop. Relat. Res. 1989;1(248):3–4. [PubMed] [Google Scholar]
- 22.Choong P.F., Dowsey M.M., Stoney J.D. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J. Arthroplasty. 2009;24(4):560–569. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 23.Laubenthal K.N., Smidt G.L., Kettekamp D.B. A quantitative analysis of knee motion during activities of daily living. Phys. Ther. 1972;52(1):34–43. doi: 10.1093/ptj/52.1.34. [DOI] [PubMed] [Google Scholar]
- 24.Agha R.A., Fowler A.J., Seatta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]