Abstract
Objective
The study aims to examine gastrointestinal symptoms, quality of life and the risk of psychological symptoms after cholecystectomy.
Design
This is a prospective population-based cohort study based on the Nord-Trøndelag Health Study (HUNT) Norway. HUNT is a repeated health survey of the county population and includes a wide range of health-related items. In the present study, all 3 HUNT surveys were included, performed between 1984 and 2008. Selected items were scores on quality of life, the Hospital Anxiety and Depression Scale (HADS) and selected gastrointestinal symptoms. Participants who underwent cholecystectomy for gallstone disease between 1 January 1990 and until 1 year before attending HUNT3 were compared with the remaining non-operated cohort. Associations between cholecystectomy and the postoperative scores and symptoms were assessed by multivariable regression models.
Results
Participants in HUNT1, HUNT2 and HUNT3 were 77 212 (89.4% of those invited), 65 237 (69.5%) and 50 807 (54.1%), respectively. In the study period, 931 participants were operated with cholecystectomy. Cholecystectomy was associated with an increased risk of diarrhoea and stomach pain postoperatively. In addition, cholecystectomy was associated with an increased risk of nausea postoperatively in men. We found no associations between cholecystectomy and quality of life, symptoms of anxiety and depression, constipation, heartburn, or acid regurgitation following surgery.
Conclusions
In this large population-based cohort study, cholecystectomy was associated with postoperative diarrhoea and stomach pain. Cholecystectomy for gallstone colic was associated with nausea in men. There were no associations between quality of life, symptoms of anxiety and depression, constipation, heartburn, or acid regurgitation.
Keywords: QUALITY OF LIFE, CHOLECYSTECTOMY, GASTROINTESTINAL FUNCTION
Summary box.
What is already known about this subject?
-
▸
Previous studies have indicated an association between cholecystectomy and quality of life and gastrointestinal symptoms.
-
▸
The prevalence of postcholecystectomy diarrhoea has been reported to range from 0.9% to 35%.
-
▸
The psychological impact of cholecystectomy is largely unknown.
What are the new findings?
-
▸
There were no associations between cholecystectomy and quality of life, symptoms of anxiety and depression, constipation, heartburn, or acid regurgitation.
-
▸
Cholecystectomy was associated with postoperative diarrhoea and stomach pain. In addition, cholecystectomy for gallstone colic was associated with nausea in men.
-
▸
The prevalence of diarrhoea increased after cholecystectomy.
How might it impact on clinical practice in the foreseeable future?
-
▸
Both clinicians and patients should be aware of the increased risk of postcholecystectomy diarrhoea and stomach pain, before considering surgery. Other symptoms of anxiety, depression and gastrointestinal symptoms do not seem to be associated with cholecystectomy. However, one should not expect improvement in quality of life.
Introduction
Laparoscopic cholecystectomy for gallstone disease is one of the most common general surgical operations performed, but long-term outcomes are unknown.1 There are some limited and inconsistent information available about the long-term quality of life in these patients.2 In previous studies, female gender and cholecystectomy for gallstone colic correlated with low quality of life scores. Female gender also correlated with a higher risk of pain in the right upper stomach quadrant after cholecystectomy.3 Quality of life was significantly better with laparoscopic cholecystectomy compared with open cholecystectomy after 2 and 5 weeks. However, 10 weeks after surgery, there were no differences in total quality of life score between the groups.4 Specific gastrointestinal symptoms, like diarrhoea and stomach pain, have been reported to occur more prevalent after cholecystectomy.5 Patients with preoperative stomach pain for more than a year more often reported postoperative persistent pain, while patients with preoperative episodic right upper quadrant pain with a duration of less than a year more often were free of pain after the operation. However, 12 weeks after cholecystectomy, 92% of patients rated the postoperative outcomes as good to excellent.6
In this study, we aimed to assess the long-term changes in quality of life and psychological and gastrointestinal symptoms among patients who have had cholecystectomy performed for gallstone disease in a population-based setting.
Methods
Study population
This study is a cohort study based on the population of Nord-Trøndelag County, Norway. During January 1984 through February 1986, all citizens in Nord-Trøndelag aged 20 years and older were invited to participate in the first survey of the Nord-Trøndelag Health Study (HUNT1).7 The second survey (HUNT2) was performed from August 1995 through June 1997 and the third survey (HUNT3) was conducted from October 2006 through June 2008. The HUNT study includes data on a wide range of health-related items gathered from written questionnaires, interviews, clinical examinations and blood samples. Among these items were also quality of life scores, scores on psychological well-being and gastrointestinal symptoms. A full description of the questionnaires and measurements is available at http://www.ntnu.edu/hunt.
Assessment of exposure
All participants in HUNT who underwent acute or elective cholecystectomy at the two primary hospitals covering the county population (Levanger and Namsos Hospital) from 1 January 1990 until 1 year before attending HUNT3 were defined as exposed. The remaining participants were defined as unexposed. In this study, we made a distinction between elective surgery performed for repeated attacks of pain in the right upper stomach quadrant (gallstone colic) and surgery performed for acute or chronic gallstone-related cholecystitis or pancreatitis. The presence of gallstones was usually confirmed preoperatively with ultrasound imaging.
Assessment of quality of life
In all the three HUNT surveys, the general subjective well-being was measured by the question: ‘Thinking about your life at the moment, would you say that you by and large are satisfied with life, or are you mostly dissatisfied?’ A seven-point ordinal scale was used that ranged from ‘very satisfied’ (score=1) through ‘neither satisfied nor dissatisfied’ (score=4) to ‘very dissatisfied’ (score=7).8
Assessment of anxiety and depression
In HUNT2 and HUNT3 the Hospital Anxiety and Depression Scale (HADS) was used to indicate the general psychological well-being, anxiety disorders and depression. The scoring varied between 0 (no symptoms) and 42 (worst symptoms). HADS performs well in assessing the symptom severity in anxiety disorders and depression in somatic, psychiatric and primary care patients and in the general population.9 The subscales for anxiety (HADS-A) and depression (HADS-D) vary between 0 (no symptoms) and 21(worst symptoms). An optimal balance between sensitivity and specificity is achieved when illness is defined by a score of 8 or above on both subscales.9
Assessment of gastrointestinal symptoms
In HUNT2 and HUNT3, the questionnaires included assessments of gastrointestinal symptoms. In this study, seven gastrointestinal symptoms were selected. Four of these were assessed in HUNT2 and HUNT3 using the question: ‘To what degree have you had the following problems in the past 12 months?’; ‘diarrhoea’, ‘constipation’, ‘nausea’ and ‘heartburn or acid regurgitations’. All symptoms were assessed separately with the answers ‘no’, ‘yes, a little’ and ‘yes, much’. In addition, HUNT3 included assessments of stomach pain: ‘Have you had stomach pain or discomfort in the past 12 months?’ assessed with the answers ‘no’, ‘yes, a little’ and ‘yes, much’. If this question was answered with ‘yes, much’, the following questions were also included: ‘Is it localised in the upper stomach?’ assessed with the answers ‘no’ and ‘yes’, and ‘Do you have this pain/discomfort after eating?’ assessed with the answers ‘no’ and ‘yes’.
Assessment of confounders
As potential confounders, we selected sex, age, body mass index (BMI), waist circumference, physical activity and total HADS score. In HUNT, height, weight and waist circumference were objectively measured by trained personnel and BMI was calculated by dividing weight in kilograms by height in metres squared (kg/m2). Physical activity was assessed through questionnaires. In HUNT2, the participants reported that they were doing hard physical activity ‘less than one hour per week’ or ‘at least one hour per week’. In HUNT3, they reported ‘never’, ‘less than once a week’, ‘once a week’, ‘two to three times a week’ or ‘almost every day’.
Statistical methods
All analyses were performed for each sex separately.
The associations between previous cholecystectomy, performed at least 1 year before participation in HUNT3, and quality of life score at follow-up in HUNT3 were analysed using univariable and multivariable linear regression analyses. Adjustments were made for age, quality of life score in HUNT1, BMI in HUNT3, waist circumference in HUNT3 and physical exercise in HUNT3.
The associations between previous cholecystectomy, performed at least 1 year before participation in HUNT3, and HADS score at follow-up in HUNT3 were analysed using univariable and multivariable linear regression analyses. We adjusted for age, total HADS score in HUNT2, BMI in HUNT3, waist circumference in HUNT3 and physical exercise in HUNT3.
The associations between previous cholecystectomy, performed at least 1 year before participation in HUNT3 and gastrointestinal symptoms reported at follow-up in HUNT3 were analysed using logistic regression. Gastrointestinal symptoms were dichotomised into ‘no or a little’ and ‘much’. We adjusted for age, BMI, waist circumference, physical activity and total HADS score. The prevalence of the four gastrointestinal symptoms included in HUNT2 and HUNT3 was assessed before and after cholecystectomy among those operated between participation in HUNT2 and 1 year before participation in HUNT3.
We used multiple imputations to handle missing data. All variables used in the analyses were included in the imputation models. We imputed 100 data sets, as recommended by van Buuren.10 We did not impute missing data on ‘upper stomach pain’ and ‘stomach pain after meals’ on individuals who answered ‘no’ or ‘yes, a little’ to ‘Have you had stomach pain or discomfort in the past 12 months?’, as these values are missing by design.
Two-sided p values <0.05 were considered significant. We performed the analyses with SPSS V.23 (IBM, Armonk, New York, USA).
Ethical approval
The Regional Committee for Medical and Health Research Ethics, Central Norway, approved this study (2014/229). The participants in HUNT gave written informed consent for medical research, including linkage to patient records at the hospitals.
Results
Participants
The number of participants in HUNT1, HUNT2 and HUNT3 was 77 212 (89.4% of those invited), 65 237 (69.5%) and 50 807 (54.1%), respectively. In total, 27 992 persons have participated in all three surveys. Between 1 January 1990 and HUNT3, 931 HUNT participants (1.8%) were operated with cholecystectomy for gallstone disease and included in this study. Of these, 472 had elective cholecystectomy for gallstone colic and 459 had elective or acute cholecystectomy for gallstone-related cholecystitis or pancreatitis.
Table 1 shows the characteristics of the study participants in HUNT3. The majority of operated participants were women, especially those operated on for gallstone colic. The operated participants were older than the non-operated participants and those operated on for gallstone-related cholecystitis or pancreatitis were older than those operated on for gallstone colic. The BMI and waist circumference were higher among the operated than non-operated and the operated did less frequent physical exercise than the non-operated. There were no major differences in the quality of life scores or HADS scores among the operated and non-operated participants. The operated participants reported more symptoms with gastrointestinal symptoms than the non-operated and those operated on for gallstone colic reported more gastrointestinal symptoms than those operated on for gallstone-related cholecystitis or pancreatitis.
Table 1.
Characteristics of the study participants in HUNT3
| Cholecystectomy for gallstone colic | Cholecystectomy for gallstone-related cholecystitis or pancreatitis | No cholecystectomy | |
|---|---|---|---|
| Participants | |||
| N (%) | 472 (0.9) | 459 (0.9) | 49 874 (98.2) |
| Women | |||
| N (%) | 399 (84.5) | 295 (64.3) | 27 062 (54.3) |
| Age in years | |||
| Mean (SD) | 56.4 (14.1) | 62.9 (15.0) | 53.0 (16.1) |
| Body mass index | |||
| Mean (SD) | 29.7 (5.4) | 29.7 (5.0) | 27.1 (4.4) |
| Missing, n (%) | 3 (0.6) | 8 (1.7) | 388 (0.8) |
| Waist circumference | |||
| Mean (SD) | 98.4 (13.1) | 100.4 (13.0) | 93.5 (12.3) |
| Missing, n (%) | 8 (1.7) | 6 (1.3) | 432 (0.9) |
| Physical activity (exercise) | |||
| Never (%) | 28 (5.9) | 39 (8.5) | 2614 (5.2) |
| Less than once a week (%) | 64 (13.6) | 75 (16.3) | 8150 (16.3) |
| Once a week (%) | 135 (28.6) | 100 (21.8) | 10 493 (21.0) |
| 2–3 times a week (%) | 160 (33.9) | 163 (35.5) | 18 849 (37.8) |
| Almost every day (%) | 79 (16.7) | 74 (16.1) | 8851 (17.7) |
| Missing, n (%) | 6 (1.3) | 8 (1.7) | 917 (1.8) |
| Quality of life score | |||
| Mean (SD) | 2.6 (1.0) | 2.7 (1.1) | 2.6 (1.0) |
| Missing, n (%) | 77 (16.3) | 64 (13.9) | 14 043 (28.2) |
| Total Hospital Anxiety and Depression Scale score | |||
| Mean (SD) | 7.8 (5.8) | 7.5 (5.0) | 7.3 (5.4) |
| Missing, n (%) | 96 (20.3) | 102 (22.2) | 11 968 (24.0) |
| Diarrhoea | |||
| No or a little, n (%) | 297 (62.9) | 282 (61.4) | 34 269 (68.7) |
| Much, n (%) | 48 (10.2) | 29 (6.3) | 1465 (2.9) |
| Missing, n (%) | 127 (26.9) | 148 (32.2) | 14 140 (28.4) |
| Constipation | |||
| No or a little, n (%) | 304 (64.4) | 282 (61.4) | 33 758 (67.7) |
| Much, n (%) | 31 (6.6) | 35 (7.6) | 2257 (4.5) |
| Missing, n (%) | 137 (29.0) | 142 (30.9) | 13 859 (27.8) |
| Nausea | |||
| No or a little, n (%) | 329 (69.7) | 305 (66.4) | 35 106 (70.4) |
| Much, n (%) | 14 (3.0) | 1 (0.2) | 573 (1.1) |
| Missing, n (%) | 129 (27.3) | 153 (33.3) | 14 195 (28.5) |
| Heartburn or acid regurgitations | |||
| No or a little, n (%) | 315 (66.7) | 302 (65.8) | 34 117 (68.4) |
| Much, n (%) | 45 (9.5) | 32 (7.0) | 2588 (5.2) |
| Missing, n (%) | 112 (23.7) | 125 (27.2) | 13 169 (26.4) |
| Stomach pain or discomfort | |||
| No or a little, n (%) | 221 (68.4) | 227 (73.0) | 37 421 (74.6) |
| Much, n (%) | 51 (15.8) | 34 (10.9) | 2674 (5.3) |
| Missing, n (%) | 51 (15.8) | 50 (16.1) | 10 076 (20.1) |
| Upper stomach pain, if much stomach pain or discomfort | |||
| No, n (%) | 16 (31.4) | 9 (26.5) | 1113 (41.6) |
| Yes, n (%) | 33 (64.7) | 22 (64.7) | 1409 (52.7) |
| Missing, n (%) | 2 (3.9) | 3 (8.8) | 152 (5.7) |
| Stomach pain after meals, if much stomach pain or discomfort | |||
| No, n (%) | 14 (27.4) | 11 (32.4) | 1.249 (46.7) |
| Yes, n (%) | 36 (70.6) | 22 (64.7) | 1.307 (48.9) |
| Missing, n (%) | 1 (2.0) | 1 (2.9) | 118 (4.4) |
HUNT3, third Nord-Trøndelag Health Study.
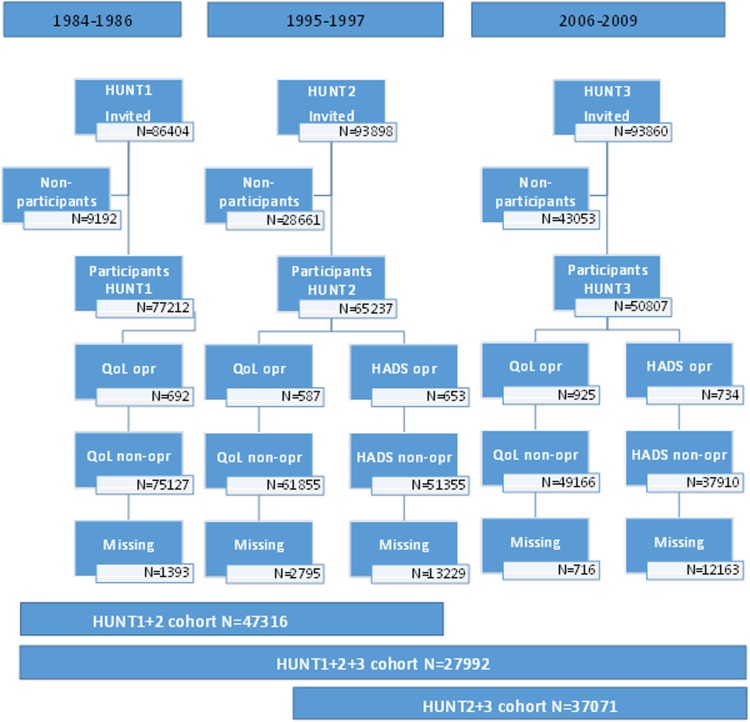
Quality of life after cholecystectomy
Figure 1 shows the flow of participants reporting quality of life. Quality of life was reported by 271 women and 54 men in HUNT3 who had cholecystectomy performed between 1 January 1990 and at least 1 year before HUNT3. The median observation time after cholecystectomy among these participants was 7.53 (range 1.02–18.13) years in women and 6.97 (range 1.38–17.66) years in men. Table 2 shows the association between cholecystectomy and quality of life postoperatively. The analysis did not show any association between cholecystectomy and quality of life postoperatively, neither unadjusted (not shown) nor adjusted. The results based on multiple imputations did not differ notably from complete case results (data not shown).
Figure 1.
Flow chart of participants reporting QoL score and HADS in HUNT1, HUNT2 and HUNT3, opr or non-opr with cholecystectomy for gallstone disease. HADS, Hospital Anxiety and Depression Scale; HUNT1, first Nord-Trøndelag Health Study; HUNT2, second Nord-Trøndelag Health Study; HUNT3, third Nord-Trøndelag Health Study; non-opr, non-operated; opr, operated; QoL, quality of life.
Table 2.
The associations between cholecystectomy and (a) quality of life score and (b) Hospital Anxiety and Depression Scale score postoperatively in HUNT3
| Unadjusted |
Adjusted* |
|||||||
|---|---|---|---|---|---|---|---|---|
| Women |
Men |
Women |
Men |
|||||
| β (95% CI) | p Value | β (95% CI) | p Value | β (95% CI) | p Value | β (95% CI) | p Value | |
| (a) Quality of life | ||||||||
| Non-operated | Reference | Reference | Reference | Reference | ||||
| Cholecystectomy for gallstone colic | 0.112 (−0.012 to 0.235) | 0.076 | 0.129 (−0.143 to 0.402) | 0.351 | −0.003 (−0.072 to 0.066) | 0.970 | 0.262 (0.121 to 0.403) | 0.063 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 0.060 (−0.081 to 0.202) | 0.404 | 0.045 (−0.150 to 0.239) | 0.653 | 0.094 (0.020 to 0.168) | 0.202 | 0.033 (−0.160 to 0.227) | 0.730 |
| (b) Hospital Anxiety and Depression Scale | ||||||||
| Non-operated | Reference | Reference | Reference | Reference | ||||
| Cholecystectomy for gallstone colic | 0.141 (−0.576 to 0.859) | 0.699 | −0.103 (−1.600 to 1.369) | 0.893 | −0.015 (−0.609 to 0.579) | 0.960 | −030 (−1.342 to 1.282) | 0.964 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 0.201 (−0.655 to 1.057) | 0.645 | 0.950 (−0.124 to 2.023) | 0.083 | −0.391 (−1.123 to 0.341) | 0.295 | 0.330 (−0.621 to 1.281) | 0.496 |
*Adjusted for (a) age, quality of life score in HUNT1 (baseline), body mass index in HUNT3, waist circumference in HUNT3 and physical exercise in HUNT3, and (b) age, Hospital Anxiety and Depression Scale score in HUNT2 (baseline), body mass index in HUNT3, waist circumference in HUNT3 and physical exercise in HUNT3.
HUNT1, first Nord-Trøndelag Health Study; HUNT3, third Nord-Trøndelag Health Study.
Anxiety and depression after cholecystectomy
Figure 1 shows the flow of participants reporting symptoms of anxiety and depression (HADS). The HADS questionnaire was answered by 182 women and 30 men in HUNT3 who had cholecystectomy performed between HUNT2 and at least 1 year before HUNT3. The median observation time after cholecystectomy among these participants was 6.23 (range 1.02–11.90) years in women and 5.03 (range 1.18–11.72) years in men. Table 2 shows the association between cholecystectomy and HADS postoperatively. The analysis did not show any association between cholecystectomy and HADS postoperatively, neither unadjusted (not shown) nor adjusted. The results based on multiple imputations did not differ notably from complete case results (data not shown).
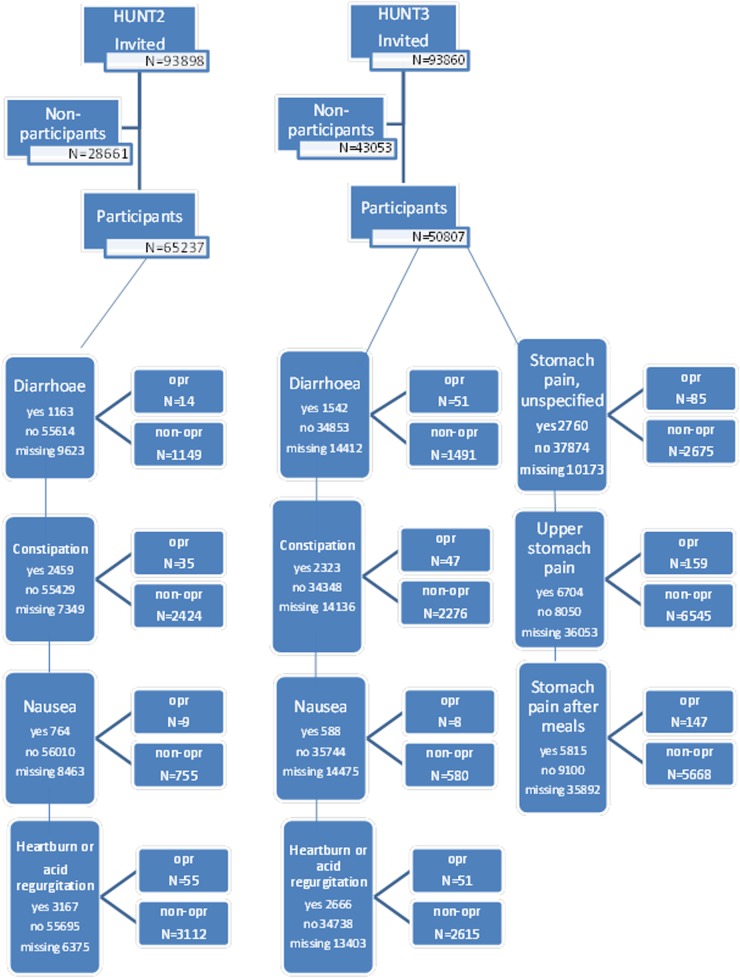
Gastrointestinal symptoms after cholecystectomy
Figure 2 shows the flow of participants reporting gastrointestinal symptoms. Gastrointestinal symptoms were reported by 396 women and 138 men in HUNT3 who had cholecystectomy performed between HUNT2 and at least 1 year before HUNT3. The median observation time among these participants was 6.59 (range 1.33–11.90) years in women and 5.44 (range 1.36–11.72) years in men.
Figure 2.
Flow chart of participants reporting gastrointestinal symptoms in HUNT2 and HUNT3, opr or non-opr with cholecystectomy for gallstone disease. HUNT2, second Nord-Trøndelag Health Study; HUNT3, third Nord-Trøndelag Health Study; non-opr, non-operated; opr, operated.
The participants reported more symptoms with diarrhoea after surgery than before surgery, and operated participants reported more symptoms with diarrhoea than non-operated participants did, especially women. Among the participants who later had a cholecystectomy, 3.4% (14/409) of the women and 0% (0/137) of the men reported much diarrhoea before surgery in HUNT2. This increased to 13.0% (45/345) of the women and 5.2% (6/116) of the men after surgery in HUNT3. Among the non-operated participants, 1.9% (345/17710) of the women and 1.9% (296/15367) of the men reported much diarrhoea in HUNT2 and 4.7% (686/14671) of the women and 3.1% (367/11996) of the men reported much diarrhoea in HUNT3.
The operated participants reported more symptoms with stomach pain or discomfort than did the non-operated participants. Among the participants operated on for gallstone colic, 19.5% (44/226) of the women and 14.9% (7/47) of the men reported much stomach pain at follow-up in HUNT3. Among the participants operated on for acute or chronic gallstone-related cholecystitis or pancreatitis, the corresponding numbers were 17.1% (29/86) and 5.5% (5/91), respectively. Among the non-operated participants, only 8.2% (1822/22329) of the women and 4.8% (853/17771) of the men reported much stomach pain.
Table 3 shows the associations between cholecystectomy and gastrointestinal symptoms postoperatively. After adjustments, previous cholecystectomy was associated with a 2.5-fold to 3-fold increased risk of diarrhoea postoperatively in women, irrespective of the indication for cholecystectomy. In men, the risk of diarrhoea increased by fourfold after cholecystectomy for gallstone colic, while cholecystectomy for gallstone-related cholecystitis or pancreatitis was not associated with diarrhoea. The risk of nausea was increased by about eightfold after cholecystectomy for gallstone colic in men, while the risk nausea was not increased after cholecystectomy for gallstone-related cholecystitis or pancreatitis or in women.
Table 3.
The associations between cholecystectomy and gastrointestinal symptoms postoperatively in HUNT3
| Unadjusted |
Adjusted* |
|||||||
|---|---|---|---|---|---|---|---|---|
| Women |
Men |
Women |
Men |
|||||
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Diarrhoea† | ||||||||
| Non-operated | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| Cholecystectomy for gallstone colic | 2.73 (1.77 to 4.20) | <0.001 | 2.96 (1.06 to 8.30) | 0.039 | 2.61 (1.62 to 4.21) | <0.001 | 4.39 (1.49 to 12.87) | 0.007 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 3.21 (1.77 to 4.20) | <0.001 | 0.85 (0.21 to 3.46) | 0.815 | 2.95 (1.71 to 5.08) | <0.001 | 1.46 (0.35 to 6.08) | 0.601 |
| Constipation† | ||||||||
| Non-operated | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| Cholecystectomy for gallstone colic | 1.16 (0.73 to 1.84) | 0.539 | 1.12 (0.18 to 7.11) | 0.901 | 1.09 (0.64 to 1.84) | 0.764 | 0.81 (0.11 to 6.19) | 0.835 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 1.68 (1.07 to 2.65) | 0.025 | 2.97 (0.89 to 9.90) | 0.076 | 1.66 (0.99 to 2.76) | 0.053 | 1.13 (0.44 to 3.86) | 0.634 |
| Nausea† | ||||||||
| Non-operated | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| Cholecystectomy for gallstone colic | 1.13 (0.46 to 2.75) | 0.794 | 6.06 (1.45 to 25.3) | 0.014 | 1.27 (0.46 to 3.55) | 0.646 | 7.95 (1.85 to 34.9) | 0.006 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 0.31 (0.04 to 2.18) | 0.237 | –‡ | –‡ | –‡ | |||
| Heartburn or acid regurgitation† | ||||||||
| Non-operated | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| Cholecystectomy for gallstone colic | 1.61 (1.03 to 2.52) | 0.036 | 1.33 (0.47 to 3.72) | 0.590 | 1.19 (0.72 to 1.97) | 0.501 | 1.24 (0.42 to 3.73) | 0.698 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 1.79 (1.10 to 2.90) | 0.018 | 1.09 (0.47 to 2.52) | 0.834 | 1.25 (0.73 to 2.12) | 0.417 | 0.82 (0.34 to 2.01) | 0.670 |
| Stomach pain or discomfort† | ||||||||
| Non-operated | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| Cholecystectomy for gallstone colic | 2.74 (1.96 to 3.82) | <0.001 | 3.48 (1.55 to 7.78) | 0.002 | 2.83 (2.01 to 4.00) | <0.001 | 3.57 (1.55 to 8.24) | 0.003 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 2.32 (1.55 to 3.46) | <0.001 | 1.15 (0.47 to 2.85) | 0.756 | 2.44 (1.61 to 3.69) | <0.001 | 1.10 (0.44 to 2.76) | 0.833 |
| Upper stomach pain§ | ||||||||
| Non-operated | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| Cholecystectomy for gallstone colic | 1.44 (0.76 to 2.73) | 0.260 | 4.62 (0.55 to 38.5) | 0.158 | 1.41 (0.74 to 2.68) | 0.307 | 4.59 (1.53 to 13.72) | 0.164 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 1.60 (0.72 to 3.58) | 0.250 | –‡ | 1.37 (0.62 to 3.01) | 0.453 | –‡ | ||
| Stomach pain after meals§ | ||||||||
| Non-operated | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | ||||
| Cholecystectomy for gallstone colic | 2.46 (1.23 to 4.90) | 0.011 | 1.66 (0.37 to 7.46) | 0.509 | 2.57 (1.30 to 5.08) | 0.008 | 1.68 (0.36 to 7.93) | 0.501 |
| Cholecystectomy for gallstone-related cholecystitis or pancreatitis | 1.52 (0.70 to 3.31 | 0.290 | 4.98 (0.55 to 44.7) | 0.152 | 1.63 (0.78 to 3.42 | 0.222 | 5.45 (1.76 to 16.85) | 0.133 |
*The first four symptoms were adjusted for the same symptom in HUNT2 (baseline). In addition, all seven symptoms were adjusted for age, body mass index, waist circumference, physical activity, and symptoms of anxiety and depression in HUNT3.
†Self-reported much symptoms in the last 12 months.
‡No or too few cases in these cells.
§Self-reported symptoms in the past 12 months in patients reporting much stomach pain or discomfort.
HUNT2, second Nord-Trøndelag Health Study; HUNT3, third Nord-Trøndelag Health Study.
In women, previous cholecystectomy was associated with a 2.5-fold to 3-fold increased risk of stomach pain or discomfort, irrespective of the indication for cholecystectomy. Cholecystectomy for gallstone colic was also associated with a 2.5-fold increased risk of stomach pain after meals in women. In men, cholecystectomy for gallstone colic was associated with a 3.5-fold increased risk of stomach pain or discomfort. However, men operated with cholecystectomy for gallstone-related cholecystitis or pancreatitis did not have any increased risk of postoperative stomach pain.
The adjusted analyses did not show any associations between cholecystectomy and constipation, heartburn, or acid regurgitation. The results based on multiple imputations did not differ notably from complete case results (data not shown).
Discussion
In this study, we found no association between cholecystectomy and quality of life, symptoms of anxiety and depression, constipation, heartburn, or acid regurgitation after at least 1 year of observation postoperatively. Cholecystectomy was associated with an increased risk of diarrhoea and stomach pain postoperatively. In addition, cholecystectomy for gallstone colic was associated with an increased risk of nausea in men postoperatively.
The population-based design with a large sample size, long observation period and a complete registration of all cholecystectomies are major strengths of this study, reducing the risk of chance findings and selection bias. Except for a slightly lower income and the absence of larger cities, the population of Nord-Trøndelag is stable and representative for Norway, which makes long-term follow-up possible and valid.11 12 The question about general subjective well-being was presented in exactly the same form throughout all the three HUNT studies, and the HADS questionnaire and the four specific gastrointestinal symptoms used in this study were presented in exactly the same form in HUNT2 and HUNT3, which makes comparison possible over time. HADS is an international and standardised score for anxiety and depression and is well validated.9
Some of the weaknesses of this study are the questionnaires on general subjective well-being and gastrointestinal symptoms. These questionnaires have not been externally validated, except the questions on heartburn or acid regurgitation, which has performed excellently in previous validations.13 14 The study also lacks records of participants operated with cholecystectomy before 1990. These participants were treated as unexposed in this study, together with all participants who actually have never had cholecystectomy performed. This could attenuate any association between cholecystectomy and quality of life and psychological and gastrointestinal symptoms. However, owing to the large number of unexposed, the effect of including individuals who underwent cholecystectomy before 1990 would be very small and probably not affect the outcome. Also, owing to large numbers of missing values for the outcomes, we used multiple imputations to handle the missing data. This reduces bias and avoids loss of sample size due to missing data, which in turn increases the precision of the results. The results with and without imputations did not alter the main results and conclusions of the study.
A non-participant study performed after HUNT3 showed that the population not captured were the youngest (aged 20 to 39 years) and the oldest (aged 80 years or more) residents. More men than women did not participate, and non-participants had lower socioeconomic status.11 This must be kept in mind when interpreting the results.
One must also keep in mind the differences in observation time when generalising the results. A short observation time may include only the short-term outcome and not represent the final outcome after cholecystectomy. A long observation time may conflict with other symptoms due to comorbidity. In studies with a long observation time, like this study, chronic long-term symptoms are included, but not temporary short-term symptoms. However, to avoid including symptoms related to the actual surgical procedure, we only evaluated symptoms that were present at least 1 year after cholecystectomy.
Previous research on long-term quality of life after cholecystectomy for gallstone disease is limited. A study comparing open and laparoscopic cholecystectomy in terms of quality of life and postoperative stomach pain found good quality of life after cholecystectomy regardless of method, but an increased prevalence of gastrointestinal symptoms compared with the background population.5
As far as we know, this is the first study to assess the association between cholecystectomy and symptoms of anxiety and depression postoperatively.
The prevalence of postcholecystectomy diarrhoea, one of the most distressing postoperative sequelae, has in previous studies been reported to range from 0.9% to 35%,15 with most studies reporting a prevalence between 12% and 20%.16–21 Differences in study groups, questionnaires and definitions of diarrhoea make comparison with other studies difficult. One study found that gastrointestinal transit time following cholecystectomy is shortened by 20% because of acceleration of colonic passage.15 However, other studies have found unchanged transit time and no significant difference in diarrhoea before and after surgery.19 22 The cause of postcholecystectomy diarrhoea is most likely multifactorial. This includes a continuous flux of hepatic bile into the duodenum combined with bile acid malabsorption due to saturation of the reabsorptive capacity in the distal ileum, resulting in increased amounts of bile acids presented to the large bowel causing secretory diarrhoea and acceleration of colonic passage. In addition, psychological and psychosomatic factors influence gut motility.15 23 24
In a previous study, treatment of symptomatic gallbladder stones with cholecystectomy resulted in cure or improvement of symptoms in about 90% of patients, but 20–30% of the patients reported significant pain and dyspeptic symptoms.25 Another study found that 7% of patients had persistent pain 3 months after cholecystectomy, but this was mostly caused by other diseases and was relieved after specific treatment. Three years postoperatively, only 4% reported that they still had stomach pain.21
In conclusion, this large prospective population-based cohort study showed no association between cholecystectomy and quality of life, symptoms of anxiety and depression, constipation, heartburn, or acid regurgitation postoperatively. However, cholecystectomy was associated with an increased risk of diarrhoea and stomach pain postoperatively. This should be kept in mind in the preoperative judgement and communicated to the patient.
Acknowledgments
The Nord-Trøndelag Health Study (the HUNT Study) is a collaboration between HUNT Research Centre (Faculty of Medicine, NTNU, Norwegian University of Science and Technology), Nord-Trøndelag County Council, Central Norway Health Authority and the Norwegian Institute of Public Health.
Footnotes
Contributors: AT planned the study together with KH, T-HE and EN-J. AT is the contributor responsible for the overall content together with EN-J. The statistical analysis was performed by AT, EN-J, T-HE and SL. AT, SL, T-HE, KH and EN-J contributed to the reporting of the manuscript.
Funding: Funded by Levanger Hospital, HNT Norway and NTNU, Norwegian University of Science and Technology.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Zapf M, Denham W, Barrera E, et al. Patient-centered outcomes after laparoscopic cholecystectomy. Surg Endosc 2013;27:4491–8. doi:10.1007/s00464-013-3095-0 [DOI] [PubMed] [Google Scholar]
- 2.Rydbeck D, Anesten B, Barje T, et al. Health-related quality-of-life in a cohort undergoing cholecystectomy. Ann Med Surg (Lond) 2015;4:22–5. doi:10.1016/j.amsu.2014.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wanjura V, Lundström P, Osterberg J, et al. Gastrointestinal quality-of-life after cholecystectomy: indication predicts gastrointestinal symptoms and abdominal pain. World J Surg 2014;38:3075–81. doi:10.1007/s00268-014-2736-3 [DOI] [PubMed] [Google Scholar]
- 4.Matovic E, Hasukic S, Ljuca F, et al. Quality of life in patients after laparoscopic and open cholecystectomy. Med Arh 2012;66:97–100. doi:10.5455/medarh.2012.66.97-100 [DOI] [PubMed] [Google Scholar]
- 5.Wanjura V, Sandblom G. How do quality-of-life and gastrointestinal symptoms differ between post-cholecystectomy patients and the background population? World J Surg 2016;40:81–8. doi:10.1007/s00268-015-3240-0 [DOI] [PubMed] [Google Scholar]
- 6.Lamberts MP, Den Oudsten BL, Gerritsen JJ, et al. Prospective multicentre cohort study of patient-reported outcomes after cholecystectomy for uncomplicated symptomatic cholecystolithiasis. Br J Surg 2015;102:1402–9. doi:10.1002/bjs.9887 [DOI] [PubMed] [Google Scholar]
- 7.Krokstad S, Langhammer A, Hveem K, et al. Cohort profile: the HUNT Study, Norway. Int J Epidemiol 2013;42:968–77. doi:10.1093/ije/dys095 [DOI] [PubMed] [Google Scholar]
- 8.Bowling A. Just one question: if one question works, why ask several? J Epidemiol Community Health 2005;59:342–5. doi:10.1136/jech.2004.021204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77. doi:10.1016/S0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 10.van Buuren S. Flexible imputation of missing data. Boca Raton, FL: CRC Press, 2012. [Google Scholar]
- 11.Langhammer A, Krokstad S, Romundstad P, et al. The HUNT study: participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol 2012;12:143 doi:10.1186/1471-2288-12-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Statistical Yearbook of Norway 2013. Oslo, Kongsvinger, Norway: Statistics Norway, 2013. [Google Scholar]
- 13.Nilsson M, Johnsen R, Ye W, et al. Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA 2003;290:66–72. doi:10.1001/jama.290.1.66 [DOI] [PubMed] [Google Scholar]
- 14.Ness-Jensen E, Lindam A, Lagergren J, et al. Changes in prevalence, incidence and spontaneous loss of gastro-oesophageal reflux symptoms: a prospective population-based cohort study, the HUNT study. Gut 2012;61:1390–7. doi:10.1136/gutjnl-2011-300715 [DOI] [PubMed] [Google Scholar]
- 15.Fisher M, Spilias DC, Tong LK. Diarrhoea after laparoscopic cholecystectomy: incidence and main determinants. ANZ J Surg 2008;78:482–6. doi:10.1111/j.1445-2197.2008.04539.x [DOI] [PubMed] [Google Scholar]
- 16.Lublin M, Crawford DL, Hiatt JR, et al. Symptoms before and after laparoscopic cholecystectomy for gallstones. Am Surg 2004;70:863–6. [PubMed] [Google Scholar]
- 17.Weinert CR, Arnett D, Jacobs D Jr, et al. Relationship between persistence of abdominal symptoms and successful outcome after cholecystectomy. Arch Intern Med 2000;160:989–95. doi:10.1001/archinte.160.7.989 [DOI] [PubMed] [Google Scholar]
- 18.Vander Velpen GC, Shimi SM, Cuschieri A. Outcome after cholecystectomy for symptomatic gall stone disease and effect of surgical access: laparoscopic v open approach. Gut 1993;34:1448–51. doi:10.1136/gut.34.10.1448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fort JM, Azpiroz F, Casellas F, et al. Bowel habit after cholecystectomy: physiological changes and clinical implications. Gastroenterology 1996;111:617–22. doi:10.1053/gast.1996.v111.pm8780565 [DOI] [PubMed] [Google Scholar]
- 20.Niranjan B, Chumber S, Kriplani AK. Symptomatic outcome after laparoscopic cholecystectomy. Trop Gastroenterol 2000;21:144–8. [PubMed] [Google Scholar]
- 21.Mjaland O, Hogevold HE, Buanes T. Standard preoperative assessment can improve outcome after cholecystectomy. Eur J Surg 2000;166:129–35. doi:10.1080/110241500750009474 [DOI] [PubMed] [Google Scholar]
- 22.Hearing SD, Thomas LA, Heaton KW, et al. Effect of cholecystectomy on bowel function: a prospective, controlled study. Gut 1999;45:889–94. doi:10.1136/gut.45.6.889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arlow FL, Dekovich AA, Priest RJ, et al. Bile acid-mediated postcholecystectomy diarrhea. Arch Intern Med 1987;147:1327–9. doi:10.1001/archinte.1987.00370070139021 [PubMed] [Google Scholar]
- 24.Sauter GH, Moussavian AC, Meyer G, et al. Bowel habits and bile acid malabsorption in the months after cholecystectomy. Am J Gastroenterol 2002;97:1732–5. doi:10.1111/j.1572-0241.2002.05779.x [DOI] [PubMed] [Google Scholar]
- 25.Borly L, Anderson IB, Bardram L, et al. Preoperative prediction model of outcome after cholecystectomy for symptomatic gallstones. Scand J Gastroenterol 1999;34:1144–52. doi:10.1080/003655299750024968 [DOI] [PubMed] [Google Scholar]