Abstract
Thoracolumbar vertebral fracture incidents usually occur secondary to a high velocity trauma in young patients and to minor trauma or spontaneously in older people.
Osteoporotic vertebral fractures are the most common osteoporotic fractures and affect one-fifth of the osteoporotic population.
Percutaneous fixation by ‘vertebroplasty’ is a tempting alternative for open surgical management of these fractures.
Despite discouraging initial results of early trials for vertebroplasty, cement augmentation proved its superiority for the treatment of symptomatic osteoporotic vertebral fracture when compared with optimal medical treatment.
Early intervention is also gaining ground recently.
Kyphoplasty has the advantage over vertebroplasty of reducing kyphosis and cement leak.
Stentoplasty, a new variant of cement augmentation, is also showing promising outcomes.
In this review, we describe the additional techniques of cement augmentation, stressing the important aspects for success, and recommend a thorough evaluation of thoracolumbar fractures in osteoporotic patients to select eligible patients that will benefit the most from percutaneous augmentation. A detailed treatment algorithm is then proposed.
Cite this article: EFORT Open Rev 2017;2:293–299. DOI: 10.1302/2058-5241.2.160057
Keywords: osteoporotic vertebral fracture, kyphoplasty, vertebroplasty, bone cement
Introduction
Vertebral fractures in general, and thoracolumbar (TL) fractures in particular, are the second most frequent fractures after hip fractures.1,2 TL fractures at the TL junction (T11-L2) account for three-quarters of total spinal injuries.3 There are two peak incidences for vertebral fractures: at a young age with motor vehicle accidents as the most common cause and in the older population as one of the markers of osteoporosis.4 Osteoporotic vertebral fractures (OVF) affect 117 in 100 000 people1 and are often related to a minor trauma, such as a fall, or may even happen spontaneously, without relating to any minor trauma.5 OVF are generally type A1 or A3.1 fractures in the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification.6 OVF are associated with a greater impact on health-related quality of life than other fragility fractures.4 Standard therapy of these fractures consists of rest, analgesia and mobilisation, and is often poorly tolerated in elderly people, with the adverse effects of analgesia and immobilisation leading to associated health problems (poor cognition, increased risk of falls, constipation and nausea).7 MRI is of primary importance to show an area of hyperintensity signal on T2 scans, a marker of oedema that is correlated with pain levels and to non-surgical management success (Fig. 1).8 Percutaneous treatment of these types of fractures consists of bone cement augmentation with or without the use of posterior instrumentation.
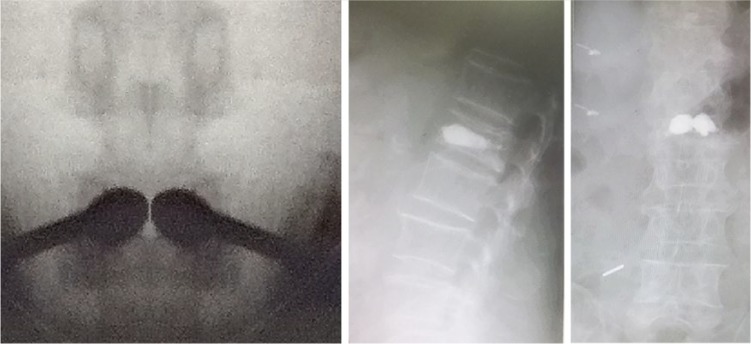
Fig. 1.
A 68-year-old woman with a history of a fall two months previously presented to our clinic for mid-back pain. Radiographs showed a T8 fracture (a). MRI confirmed the diagnosis with little hyperintensity on T2-weighted images (b, c). She was treated with a T8 kyphoplasty (d,e).
The objective of this paper, while analysing available evidence, is to answer the following questions: what is the best technique of cement augmentation through pedicle targeting? What is the efficacy of vertebral augmentation in treating OVFs? What is the best method of cement augmentation for OVFs?
Pedicle targeting
There are many described techniques for cement augmentation. Vertebroplasty was initially described for the treatment of aggressive haemangioma of the lumbar spine.9 In OVF, and via a transpedicular approach, cement is injected into the vertebra which helps stabilise the vertebral fracture with improvement of strength and stability. Balloon kyphoplasty is different in that it creates a cavity within the vertebra by an inflatable balloon, thus reducing the required injection pressure and restoration of vertebral body height.5 Newer techniques involve the introduction of a titanium device and represent the third generation of percutaneous vertebral augmentation procedures.10
No matter what the desired technique for augmentation of the OVF, posterior pedicle targeting is essential. We prefer bilateral pedicle targeting over cross-midline expansion via the unipedicular approach since evidence of the superiority of the unilateral approach is still lacking, even though some preliminary results are encouraging with the use of the latter in terms of radiation exposure and cost reduction.11,12
The patient is positioned in ventral decubitus on a Jackson frame or a radiolucent table. General or local anaesthesia is used depending on the surgeon’s preference. General anaesthesia offers less discomfort for the patient whereas local anaesthesia facilitates live neurologic monitoring. The use of two fluoroscopy machines renders the procedure faster (Fig. 2). Proper positioning of the fluoroscope is of primary importance as it must show a true anteroposterior (AP) and lateral view of the affected vertebra (parallel superior and inferior vertebral body end plates in both AP and lateral views and the spinous processes should be equidistant between vertebral body pedicles) (Fig. 3). This is especially important in patients with a small scoliotic curve or when the fracture is at the apex of a kyphosis.
Fig. 2.
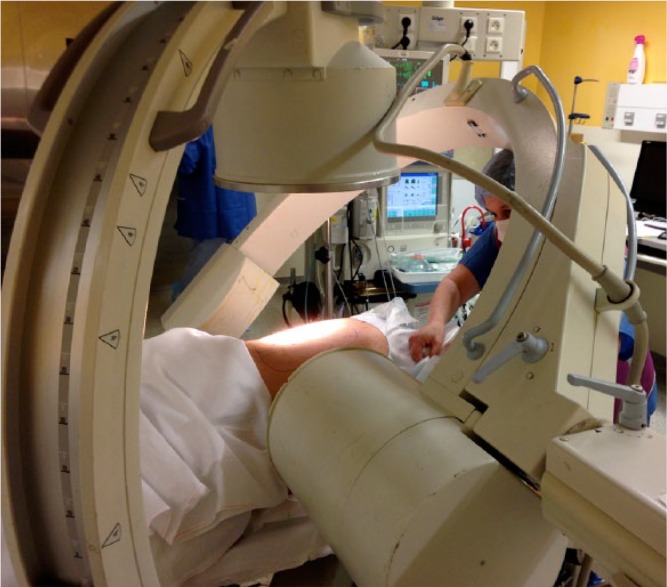
Positioning of the patient with two fluoroscopy machines for anteroposterior and lateral imaging.
Fig. 3.
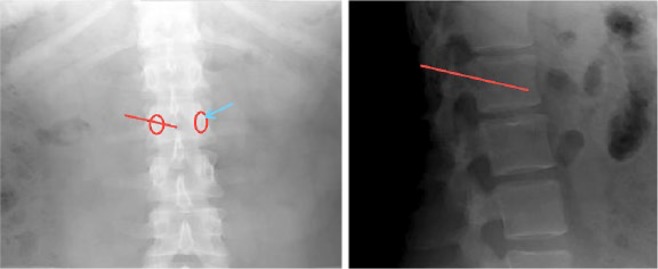
Anteroposterior (AP) and lateral radiographs of a normal lumbar spine showing the desired entry point (blue arrow on the AP) and the desired direction of the Jamshidi needle (red line on the lateral radiograph).
The pedicle targeting starting point is located in the superior-lateral part of the pedicle on the AP view (Fig. 3). Advancement of the Jamshidi needle is done in a convergent and descending direction. When the Jamshidi needle is in the middle of the pedicle on the AP view, it should be at the middle of pedicle. When the tip of the needle arrives at the posterior border of the vertebral body on the lateral radiograph, it should touch the inner border of the pedicle to have the best convergence of the needle while avoiding injury to the spinal cord (medial) or the lung (lateral). Then, the needle is advanced in the vertebral body on lateral fluoroscopy and stops 5 mm ahead of the anterior cortex (80% across the length of the vertebral body) to avoid penetration of the anterior cortex of the vertebral body and injury to the great vessels.
Cement is injected if a vertebroplasty is the desired technique. If kyphoplasty is done, a balloon is inflated to create a cavity for cement injection as well as for reduction of the kyphosis. Care must be taken not to increase pressures rapidly and not to breach the lateral cortex. This is achieved by a proper central placement of the balloon and checking for ‘kissing balloons’ on AP fluoroscopy (Fig. 4). Cement is then injected with low pressure insuring no leakage in the disc space, central canal and in the paravertebral muscles.
Fig. 4.
Anteroposterior fluoroscopy image showing the ‘kissing balloon’ image.
In the immediate post-operative period, no bracing is required. Pain is managed for a limited period with acetaminophen and narcotic medication. Most patients can be released from hospital on the same day if pain is acceptable and neurological examination is normal.
Pearls and pitfalls
True lateral and AP views should be obtained. The AP and lateral fluoroscopy images should be frequently checked to make sure of the entry point and trajectory. Care should be taken not to pierce the anterior cortex of the vertebra.
Cement should be of adequate consistency before it is injected (inject preferably after 30 seconds to 45 seconds of mixing) to minimise the risk of leak through the fissures or into the venous sinuses. The cement applicator should not be withdrawn early to decrease leakage in the paraspinal muscles.
Efficacy of vertebral augmentation
In 2009, two randomised controlled trials were published in the New England Journal of Medicine.13,14 Buchbinder et al13 and Kallmes et al14 compared vertebroplasty with a sham procedure. There was no difference in terms of pain (overall, at night, at rest) and quality of life at one week or at one, three, or six months after treatment, even though there was a trend towards a higher rate of clinically meaningful improvement in pain in the vertebroplasty group.14 This led the American Academy of Orthopedic Surgeons to strongly recommend against the use of vertebroplasty and kyphoplasty as an option for the management of painful osteoporotic compression fractures.15
Since then, several randomised controlled trials have been published.16-21 All but one16-19,21 reported the superiority of vertebral augmentation compared with optimal medical management. These studies included the FREE trial and the VERTOS and VERTOS II trials.16-21 Improvement of pain scores and quality of life scores were significantly better at early and late follow-up (up to 24 months).16 The authors also concluded that there was a mean gain of €30 000 per adjusted quality of life score.18 Thus, cement augmentation for the treatment of symptomatic OVF seems to have positive outcomes compared with optimal medical treatment or sham.22 Nonetheless, conclusions should be drawn cautiously as the results have a high likelihood of bias with most of these studies being sponsored by industry.5
One other finding is that cement volume seems to affect results. In fact, Röder et al23 recommended a minimal volume of 4.5 mL to achieve clinical efficacy as he found that lower cement-filling volumes contributed to inferior post-operative outcomes and clinical scores. Others found that higher volumes are associated with better compressive stiffness and recommend a volume of 4 mL to 6 mL to achieve acceptable physical properties.24 Yet there is ongoing controversy whether higher volumes are associated with higher cement extrusion.23,25 In brief, no definite evidence is present to support the use of a definitive volume of cement but 5 mL to 6 mL seems to be a good option.4
Early vertebroplasty has gained popularity in recent years. One study by Son et al26 was published analysing early versus delayed vertebroplasty. It showed no difference at final follow-up in terms of VAS, Odom’s criteria, and Oswestry disability index. The most important findings are the immediate improvement of VAS, which was more important in the early group, and less cement leakage.26 Recently, a randomised controlled trial comparing early vertebroplasty to placebo (the VAPOUR study) was published in The Lancet.27 It showed better early pain control, especially in the patient with initially very painful fractures. It also showed better return to daily activities. One last finding in this trial was the increased injected cement volume compared with other trials (7.5 mL versus 2 mL to 6 mL), possibly due to a shorter fracture duration. In summary, early cement augmentation seems to yield better early results and should be reserved for very painful patients (VAS ⩾ 7).
The best method of cement augmentation for OVFs
Balloon kyphoplasty relies on the fact that a cavity is created in the fractured vertebra to reduce the injection pressure (and cement leakage) and to improve the vertebral height (reduce the kyphosis) (Fig. 4).4 Recent meta-analyses have shown that kyphoplasty had a superior capability for intermediate-term (approximately three months) functional improvement while vertebroplasty was more effective in the short-term (no more than seven days) relief of pain with no difference in long-term function or pain relief.28,29 Kyphoplasty was associated with a decreased overall risk of cement leakage with a risk ratio of leakage of cement of 0.65 in kyphoplasty compared with vertebroplasty.30 Yet cement leakage in the ‘at-risk’ disc space was no different between the two methods of augmentation while the ‘safe’ paravertebral space showed reduction of leakage in the kyphoplasty.31
Stentoplasty is a recently described variation of balloon kyphoplasty where a titanium device creates the cavity within the vertebral body and is kept in place for cement injection.32,33 Many authors have found good to excellent results in terms of pain improvement, quality of life and kyphosis restoration.32,34,35 Few studies have compared stentoplasty with other modalities. When data are pooled together, a higher rate of adverse events related to material and cuff pressure was found in the stentoplasty group compared with kyphoplasty. There was no difference in terms of time of exposure to radiation, reduction of kyphosis or cement leakage, even if stentoplasty was associated with an improvement of restoration of vertebral height.36 Pain and functional disability were significantly improved at six- and 12-month follow-up.36 Results from these trials should be interpreted with caution since most of these studies are also sponsored by industry.5
Sagittal balance of the spine has become an important concept in understanding the spinal pathologies. Proponents of kyphoplasty and stentoplasty affirm that restoration of the vertebral height is important to restore the harmony and the global sagittal balance of the spine.37,38 Theoretically, improvement of the sagittal profile with restoration of the vertebral height will decrease the effort generated by the paraspinal muscles. Some authors found improvement in pulmonary function with restoration of the vertebral height39 while others noted significant improvement in the sagittal balance.40,41 Although there were significant improvements of kyphosis, this was not translated to an improvement of quality of life scores.29 On the other hand, restoring a balanced spine is protection against subsequent vertebral fracture especially in this ‘at-risk’ population (Fig. 5).4 However, based on the available literature, there can be no definitive recommendation to use one technique of vertebral cement augmentation over others.37
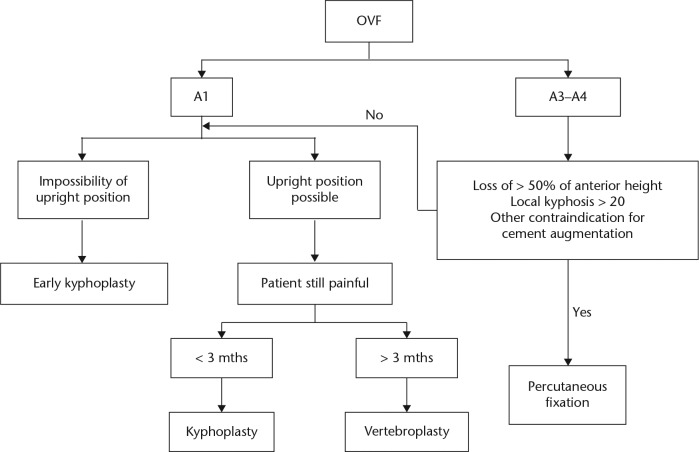
Fig. 5.
A 58-year-old woman with a non-specified mitochondrial pathology had a history of L1 vertebral fracture treated with kyphoplasty. She presented with pain in the lumbar region after a fall from her height. CT-scanner showed L2 fracture with a deformity in both sagittal and coronal planes (a, b). She was treated with a Spine Jack stentoplasty device with an unremarkable post-operative course. Post-operative scanning showed correction in both sagittal and coronal planes (c, d).
Treatment algorithm
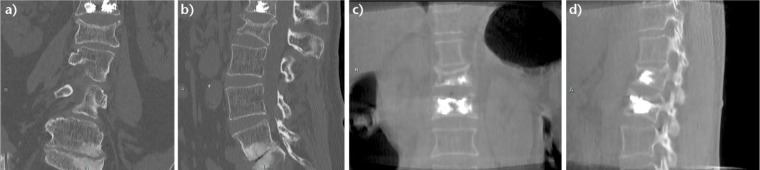
In 2010, a consensus of 160 expert practitioners of the indications and contraindications for cement augmentation in OVF was published.42 Absolute contraindications were: asymptomatic fractures; allergy to bone fillers; a history of vertebral body osteomyelitis; and irreversible coagulopathy. Relative contraindications were: presence of radiculopathy; bone retropulsion against neural structures; > 50% collapse of vertebral body height; and multiple pathological fractures. The retained indications for cement augmentations were: painful OVF that does not improve with one week of non-surgical care (impossibility for upright position); patient hospitalised as a result of painful OVF; painful pathological fracture; aggressive haemangioma; and Kümmell disease.
Based on this literature review, we propose a treatment algorithm for OVFs that are relatively stable fractures (the majority A1 or A3) (Fig. 6). Pain and maintaining an upright position are the most important indications for cement augmentations. Initial inability to maintain an upright position or contraindication to the use of a brace are the main indications for early kyphoplasty (to decrease cement extravasation). Pain at the longer-term follow-up is also an indication for cement augmentation. We prefer kyphoplasty in the early phase (less than three months) for its ability to restore the kyphosis and vertebroplasty after the third month. Finally, percutaneous fixation is the preferred method of treatment in this population when relative or absolute contraindications are present.
Fig. 6.
Algorithm for treating osteoporotic vertebral fractures (OVF).
Cement augmentation is an effective way to restore vertebral height as well as to decrease patient pain in osteoporotic fractures. The technique is relatively safe after the learning curve has passed. Therefore, a thorough evaluation of patients with thoracolumbar OVFs according to the proposed algorithm is needed to identify eligible patients for whom percutaneous cement augmentation is indicated.
Footnotes
ICMJE Conflict of interest statement: None declared.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Melton LJ, III, Kallmes DF. Epidemiology of vertebral fractures: implications for vertebral augmentation. Acad Radiol 2006;13:538-545. [DOI] [PubMed] [Google Scholar]
- 2. Wang H, Zhou Y, Li C, Liu J, Xiang L. Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg 2016;30:E239-E246. [DOI] [PubMed] [Google Scholar]
- 3. Irwin ZN, Arthur M, Mullins RJ, Hart RA. Variations in injury patterns, treatment, and outcome for spinal fracture and paralysis in adult versus geriatric patients. Spine (Phila Pa 1976) 2004;29:796-802. [DOI] [PubMed] [Google Scholar]
- 4. Sebaaly A, Nabhane L, Issa El, et al. Vertebral augmentation: state of the art. Asian Spine J 2016;10:370-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Savage JW, Schroeder GD, Anderson PA. Vertebroplasty and kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Am Acad Orthop Surg 2014;22:653-664. [DOI] [PubMed] [Google Scholar]
- 6. Reinhold M, Audigé L, Schnake KJ, et al. AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J 2013;22:2184-2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Goldstein CL, Chutkan NB, Choma TJ, Orr RD. Management of the elderly with vertebral compression fractures. Neurosurgery 2015;77:S33-S45. [DOI] [PubMed] [Google Scholar]
- 8. Takahashi S, Hoshino M, Takayama K, et al. Time course of osteoporotic vertebral fractures by magnetic resonance imaging using a simple classification: a multicenter prospective cohort study. Osteoporos Int 2017;28:473-482. [DOI] [PubMed] [Google Scholar]
- 9. Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987;33:166-168. (In French) [PubMed] [Google Scholar]
- 10. Vanni D, Pantalone A, Bigossi F, et al. New perspective for third generation percutaneous vertebral augmentation procedures: Preliminary results at 12 months. J Craniovertebral Junction Spine 2012;3:47-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yan L, Jiang R, He B, Liu T, Hao D. A comparison between unilateral transverse process-pedicle and bilateral puncture techniques in percutaneous kyphoplasty. Spine (Phila Pa 1976) 2014;39:B19-B26. [DOI] [PubMed] [Google Scholar]
- 12. Yan L, He B, Guo H, Liu T, Hao D. The prospective self-controlled study of unilateral transverse process-pedicle and bilateral puncture techniques in percutaneous kyphoplasty. Osteoporos Int 2016;27:1849-1855. [DOI] [PubMed] [Google Scholar]
- 13. Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009;361:557-568. [DOI] [PubMed] [Google Scholar]
- 14. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009;361:569-579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Esses SI, McGuire R, Jenkins J, et al. The treatment of symptomatic osteoporotic spinal compression fractures. J Am Acad Orthop Surg 2011;19:176-182. [DOI] [PubMed] [Google Scholar]
- 16. Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 2009;373:1016-1024. [DOI] [PubMed] [Google Scholar]
- 17. Voormolen MHJ, Mali WPTM, Lohle PNM, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol 2007;28:555-560. [PMC free article] [PubMed] [Google Scholar]
- 18. Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 2010;376:1085-1092. [DOI] [PubMed] [Google Scholar]
- 19. Farrokhi MR, Alibai E, Maghami Z. Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine 2011;14:561-569. [DOI] [PubMed] [Google Scholar]
- 20. Blasco J, Martinez-Ferrer A, Macho J, et al. Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up, controlled trial. J Bone Miner Res 2012;27:1159-1166. [DOI] [PubMed] [Google Scholar]
- 21. Boonen S, Van Meirhaeghe J, Bastian L, et al. Balloon kyphoplasty for the treatment of acute vertebral compression fractures: 2-year results from a randomized trial. J Bone Miner Res 2011;26:1627-1637. [DOI] [PubMed] [Google Scholar]
- 22. Anderson PA, Froyshteter AB, Tontz WL., Jr. Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. J Bone Miner Res 2013;28:372-382. [DOI] [PubMed] [Google Scholar]
- 23. Röder C, Boszczyk B, Perler G, et al. Cement volume is the most important modifiable predictor for pain relief in BKP: results from SWISSspine, a nationwide registry. Eur Spine J 2013;22:2241-2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Martinčič D, Brojan M, Kosel F, et al. Minimum cement volume for vertebroplasty. Int Orthop 2015;39:727-733. [DOI] [PubMed] [Google Scholar]
- 25. Ren H, Shen Y, Zhang YZ, et al. Correlative factor analysis on the complications resulting from cement leakage after percutaneous kyphoplasty in the treatment of osteoporotic vertebral compression fracture. J Spinal Disord Tech 2010;23:e9-e15. [DOI] [PubMed] [Google Scholar]
- 26. Son S, Lee SG, Kim WK, Park CW, Yoo CJ. Early vertebroplasty versus delayed vertebroplasty for acute osteoporotic compression fracture: are the results of the two surgical strategies the same? J Korean Neurosurg Soc 2014;56:211-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 2016;388:1408-1416. [DOI] [PubMed] [Google Scholar]
- 28. Han S, Wan S, Ning L, et al. Percutaneous vertebroplasty versus balloon kyphoplasty for treatment of osteoporotic vertebral compression fracture: a meta-analysis of randomised and non-randomised controlled trials. Int Orthop 2011;35:1349-1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Xing D, Ma J-X, Ma X-L, et al. A meta-analysis of balloon kyphoplasty compared to percutaneous vertebroplasty for treating osteoporotic vertebral compression fractures. J Clin Neurosci 2013;20:795-803. [DOI] [PubMed] [Google Scholar]
- 30. Ma XL, Xing D, Ma JX, et al. Balloon kyphoplasty versus percutaneous vertebroplasty in treating osteoporotic vertebral compression fracture: grading the evidence through a systematic review and meta-analysis. Eur Spine J 2012;21:1844-1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Xiao H, Yang J, Feng X, et al. Comparing complications of vertebroplasty and kyphoplasty for treating osteoporotic vertebral compression fractures: a meta-analysis of the randomized and non-randomized controlled studies. Eur J Orthop Surg Traumatol 2015;25:S77-S85. [DOI] [PubMed] [Google Scholar]
- 32. Shen GW, Wu NQ, Zhang N, et al. A prospective comparative study of kyphoplasty using the Jack vertebral dilator and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. J Bone Joint Surg [Br] 2010;92-B:1282-1288. [DOI] [PubMed] [Google Scholar]
- 33. Heini PF, Teuscher R. Vertebral body stenting / stentoplasty. Swiss Med Wkly 2012;142:w13658. [DOI] [PubMed] [Google Scholar]
- 34. Fan J, Shen Y, Zhang N, et al. Evaluation of surgical outcome of Jack vertebral dilator kyphoplasty for osteoporotic vertebral compression fracture-clinical experience of 218 cases. J Orthop Surg Res 2016;11:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Piazzolla A, De Giorgi S, Solarino G, Mori C, De Giorgi G. Vertebral body reconstruction system B-Twin® versus corset following non-osteoporotic Magerl A1.2 thoracic and lumbar fracture. Functional and radiological outcome at 12 month follow-up in a prospective randomized series of 50 patients. Orthop Traumatol Surg Res 2011;97:846-851. [DOI] [PubMed] [Google Scholar]
- 36. Martín-López JE, Pavón-Gómez MJ, Romero-Tabares A, Molina-López T. Stentoplasty effectiveness and safety for the treatment of osteoporotic vertebral fractures: a systematic review. Orthop Traumatol Surg Res 2015;101:627-632. [DOI] [PubMed] [Google Scholar]
- 37. Papanastassiou ID, Phillips FM, Van Meirhaeghe J, et al. Comparing effects of kyphoplasty, vertebroplasty, and non-surgical management in a systematic review of randomized and non-randomized controlled studies. Eur Spine J 2012;21:1826-1843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Papanastassiou ID, Filis A, Gerochristou MA, Vrionis FD. Controversial issues in kyphoplasty and vertebroplasty in osteoporotic vertebral fractures. BioMed Res Int 2014;2014:934206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sheng S, Zhenzhong S, Weimin J, et al. Improvement in pulmonary function of chronic obstructive pulmonary disease (COPD) patients with osteoporotic vertebral compression fractures (OVCFs) after kyphoplasty under local anesthesia. Int Surg 2015;100:503-509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Grohs JG, Matzner M, Trieb K, Krepler P. Minimal invasive stabilization of osteoporotic vertebral fractures: a prospective nonrandomized comparison of vertebroplasty and balloon kyphoplasty. J Spinal Disord Tech 2005;18:238-242. [PubMed] [Google Scholar]
- 41. Orler R, Frauchiger LH, Lange U, Heini PF. Lordoplasty: report on early results with a new technique for the treatment of vertebral compression fractures to restore the lordosis. Eur Spine J 2006;15:1769-1775. [DOI] [PubMed] [Google Scholar]
- 42. Röllinghoff M, Zarghooni K, Schlüter-Brust K, et al. Indications and contraindications for vertebroplasty and kyphoplasty. Arch Orthop Trauma Surg 2010;130:765-774. [DOI] [PubMed] [Google Scholar]