Abstract.
Household water treatment can reduce diarrheal morbidity and mortality in developing countries, but adoption remains low and supply is often unreliable. To test effects of marketing strategies on consumers and suppliers, we randomized 1,798 households in rural Haiti and collected data on purchases of a household chlorination product for 4 months. Households received randomly selected prices ($0.11–$0.56 per chlorine bottle), and half received monthly visits from sales agents. Each $0.22 drop in price increased purchases by 0.10 bottles per household per month (P < 0.001). At the mean price, each 1% drop in price increased purchases by 0.45% (elasticity = 0.45). There is suggestive evidence that household visits by some sales agents increased purchases at mid-range prices; however, the additional revenue did not offset visit cost. Choosing the lowest price and conducting visits maximizes chlorine purchase, whereas slightly raising the retail price and not conducting visits maximizes cost recovery. For the equivalent cost, price discounts increase purchases 4.2 times as much as adding visits at the current retail price. In this context, price subsidies may be a more cost-effective use of resources than household visits, though all marketing strategies tested offer cost-effective ways to achieve incremental health impact. Decisions about pricing and promotion for health products in developing countries affect health impact, cost recovery, and cost-effectiveness, and tradeoffs between these goals should be made explicit in program design.
INTRODUCTION
Worldwide, approximately 663 million people lack access to an improved water source1 and an estimated 1.2 billion more rely on microbiologically unsafe water.2 Household water treatment and storage (HWTS), which includes consumables such as chlorine solution and durables such as filters, can be a cost-effective means of improving drinking water quality3 and reducing diarrheal disease in low-income countries.4–6 One form of HWTS, chlorination, has been shown to reduce diarrhea by 22–84% in children and adults in randomized controlled trials.7–11
Despite these health benefits, only an estimated 33% of households in countries without reliable access to safe water self-report treating their drinking water.12 HWTS use increases with wealth quintile (20.4% in the poorest and 35.9% in the richest quintile), and self-reported use is higher in urban (36.6%) than rural areas (30.1%). Self-reported HWTS use in rural Haiti is higher than average (76%),13 possibly related to the fact that only 4.5% of the rural population has water piped onto the premises.1 The most commonly reported methods of HWTS in rural Haiti are chlorine tablets and chlorine solution (68% and 46%, respectively).13 However, a study in Haiti with similar levels of self-reported HWTS use (68.8%) found that total chlorine residual was actually present and confirmed (> 0.2 mg/L) in only 26% of rural Haitian households.14
A systematic review identified several key determinants of sustained use of HWTS products: perceived susceptibility and severity of disease, perceived benefits and barriers, injunctive and descriptive norms, and cost.15 Low willingness to pay (WTP) in developing countries is a barrier to use of many preventive health products,16 such as insecticide-treated bednets,17–20 deworming pills,21 soap,22 and condoms.23 Five randomized studies have been completed on WTP for chlorine solution, all of which demonstrated that demand for chlorine solution is sensitive to price (Table 1).24–28
Table 1.
Comparative results of some randomized studies on the price of chlorine solution
| Study | Country | Prior exposure of population to product | Market price of bottle* | Prices tested per 1,000 L | Elasticity at mean price† | Notes |
|---|---|---|---|---|---|---|
| Ashraf and others24 | Zambia | Varies; product launched 8 years prior to study | $0.25 | $0.09–$0.25 | −0.6 | |
| Ashraf and others28 | Zambia | Unfamiliar product | $0.30 | $0.00–$0.30 | −0.9 | Information |
| −0.6 | No information | |||||
| Blum and others25 | Kenya | Varies; product launched 4 years prior to study | $0.25 | $0.05–$0.25 | −0.9 | |
| Kremer and others26 | Kenya | Varies by household; 30% report prior use | $0.30 | $0.00–$0.30 | −1.2 | |
| Luoto and others27 | Bangladesh | 2 months | $0.12 | $0.00–$0.43 | −1.4 |
In Zambia and Kenya, one bottle treats 1,000 L; volume treated in Bangladesh was “more than 2 weeks.”
Elasticity values approximated from published data.
Since WTP for chlorine solution in low-income countries is below market prices in most cases,29 donor funding is often used to subsidize the price or to finance behavior change communication aimed at increasing WTP. One strategy is mass media campaigns, which increased use of handwashing with soap in Haiti and Burkina Faso,30,31 oral rehydration salts in Egypt and Burundi,32–34 zinc tablets in Nepal,35 and bednets in Tanzania.36 However, though mass media campaigns have increased awareness and other determinants of HWTS use, evidence for sustained behavior change at scale is mixed.37 For example, after years of mass media campaigns for chlorine solution in Kenya, use remained low38 and disparities between wealth quintiles persisted.39 Supplementation of mass media with school-based interventions40–42 increased chlorine use at home from 6% to 14%,40 and clinic-based interventions led to 71% confirmed chlorine use 1 year after receiving personal training from a nurse.38
Frequent, personal contacts with a health promoter over a period of time have been considered “the most influential program factors associated with sustained adoption” of water, sanitation, and hygiene behaviors.15 Household visits from health promoters increased handwashing with soap in Indonesia, Ghana, and India43,44 and latrine use in Bangladesh and Ethiopia.45,46 Interviews with mothers in Malawi indicated that “positive, ongoing contacts with health-care workers, especially during home visits, raised awareness of the need to treat water, encouraged trial use, and supported continuing use.”47 In cross-sectional surveys, households who received visits were more likely to use chlorine than those who had not received visits (68% versus 43% self-reported use in Zambia,48 68% versus 35% self-reported use 8 years after a campaign in Mozambique,49 and 14% versus 2% had purchased chlorine in Kenya).50
Household visits also provide opportunities to deliver messages on behavioral determinants. Providing information about water quality test results through visits increased self-reported HWTS use from 42% to 53% and annual HWTS expenditures by $7.24 in India.51 Health-oriented marketing scripts delivered during visits increased confirmed HWTS use from 47% to 54% in Kenya and from 10% to 14% in Bangladesh.52 “Motivational interviewing” by Zambian sales agents resulted in higher purchase rates and confirmed chlorine use than mass media alone (78% versus 14%).53
Incorporating these findings into marketing strategies for household chlorination programs involves negotiation between stakeholders with different values and interests, including donors, regulators, and for-profit and nonprofit chlorine suppliers that place varying degrees of emphasis on health impact and cost recovery. Strategies are designed best when informed by context-specific data on consumer demand. In Jolivert, a rural community in northwest Haiti, a household chlorination project began in 2002 and has been managed by the nonprofit social enterprise Deep Springs International (DSI) since 2008. Haitian staff manufactures and distributes sodium hypochlorite solution, branded “Gadyen Dlo” (“Water Guardian” in Haitian Creole). One 250-mL bottle treats 185 gallons (700 L) of water and lasts the average household 1–2 months. Users keep the bottle and purchase chlorine refills from community sales agents who conduct household visits.
Households who received a visit between 2002 and 2007 were more likely to purchase than those who had not been visited (78.9% versus 37.1%), and increased frequency of visits was associated with purchase consistency.54 Perceived affordability and household wealth were not correlated with having purchased or purchase consistency during 2002–2007.54 A 2010 evaluation found that 56% of participants (versus 10% of nonparticipants) had free chlorine residual in their water during an unannounced visit, and children under 5 years of age had 59% reduced odds of caregiver-reported diarrhea.55
As the program expanded to more households, the marketing strategy evolved. First, responsibility for visits shifted from three staff members to sales agents, who were trained how to test for total chlorine residual and provided test kits. Beginning in 2011, agents were offered contracts to visit their customers and record test results. Second, the product was advertised through radio, megaphone, signs, events, and branded giveaways. Finally, to improve cost recovery and align pricing with other products on the market, the retail price increased from 5 to 10 gourdes in 2008 ($0.11–$0.22) to 25 gourdes per bottle ($0.56) in 2013 in a stepwise process.
DSI sought to understand the current demand for chlorine and the relative impact of various marketing strategies on its goals of health impact, cost recovery, and cost-effectiveness. In this research, we aim to evaluate the causal impact of visits and prices on demand for chlorine and to identify optimal price and visit strategies in the context of rural Haiti.
MATERIALS AND METHODS
The study took place in five communes in the Northwest and Artibonite departments of Haiti. We conducted a census of participating households and randomized them, informed them of offer prices, collected data through monthly sales agent reports, and cleaned and analyzed data.
In June 2013, sales agents were provided paper forms to record localities and names of heads of households to whom they previously sold chlorine. Forms were returned to DSI supervisors, and household data were entered into Microsoft Excel (Microsoft Corporation, Redmond, WA) by the research team. Two numbers were generated per household using the random number generator function in Excel, one to assign visit status and one to assign price. After stratifying by sales agent, households were ranked based on the random number for visit status, and households in the bottom 50% of values for that sales agent were assigned to receive visits.
To increase transparency and prevent conflict between households and program staff, price was assigned via public lottery instead of directly by the research team. DSI Supervisors asked agents to organize community meetings with households who were listed on printed forms. During community meetings in August–September 2013, DSI Supervisors selected meeting participants from each of five groups that were determined by the second random number in Excel. Each group representative drew a price by raffle, and those prices were applied to all members of that group. The five prices offered were 5, 10, 15, 20, and 25 gourdes (the retail price). The exchange rate during the study was 1 USD = 45 gourdes, so prices offered were $0.11–$0.56 per bottle. Each randomized household, including those who did not attend the community meeting, was provided a card with their assigned price for reference during the duration of the study. To maintain the historical 10 gourdes wholesale-retail markup, DSI reimbursed sales agents for bottles they sold for less than 25 gourdes.
DSI paid sales agents to visit each household in the visit group once a month and conduct chlorine residual tests. Sales agents were trained to educate households about the importance of chlorinating their water, but they were not given a script for how to communicate during their visits. DSI supervisors collected monthly paper reports from sales agents from October 2013 to April 2014. Forms for households who did not receive visits included purchase date, volume of chlorine purchased, and price paid. Forms for households who received visits included date, volume, and price of chlorine purchases, as well as visit date, product used, and chlorine residual test result. Sales agents were not instructed to visit households in the nonvisit group, but they were instructed to record purchase data when a household came to purchase from them.
Sales agents turned in paper forms to DSI Supervisors, and DSI interns entered data into Excel. DSI provided deidentified data in Excel to Tufts researchers, and the Tufts University Institutional Review Board determined that secondary data analysis was excluded from review. The research team cleaned data in Excel, checked for data quality, and analyzed using Stata 14.1 (StataCorp LP, College Station, TX). Sales agents who did not turn in at least 4 months of forms were excluded from analysis.
Demand analysis.
Three outcome variables were constructed to measure demand at the household level: 1) purchased at least once, 2) purchased at least twice, and 3) bottles purchased per month. We tested relationships between all three outcome variables and visits (using Pearson’s χ2 tests and two-sample t tests) and price (using simple linear regression). Significance was considered at the P = 0.05 level, and we used heteroskedasticity-robust standard errors in regression models. Then we constructed multivariate linear regression models for each of the three outcome variables. We focus primarily on models of the third outcome variable:
| 1 |
Botpermthij is the number of bottles purchased per month by household i served by agent j. Priceij is the retail price per bottle (5, 10, 15, 20, or 25 gourdes). Visitsij is an indicator of whether the household received visits. Midpriceij • visitsij is an interaction term that captures heterogeneity in the effect of visits on purchase rates for households that received chlorine at 15 or 20 gourdes per bottle (compared with a reference group of 5, 10, or 25 gourdes).
Cost recovery analysis.
To explore implications on cost recovery for the chlorine supplier, we calculated monthly net revenue per month per household:
| 2 |
where p indexes the retail price per bottle and v indexes visits (visits or no visits). Botpermthpv is an estimate of monthly household bottle purchases using predicted values from Equation 1 for each of the 10 price–visit strategies. Marginp per bottle is equal to the wholesale price per bottle minus the cost of goods sold per bottle. We assumed the wholesale price was 10 gourdes less than the retail price, which is the markup that sales agents received during the study. Cost of goods sold included variable costs (raw materials, packaging, labor, delivery) and fixed costs directly related to production (capital equipment and production space). Other fixed costs such as monitoring and evaluation, administration, and advertising (radio spots, branded promotional merchandise, event sponsorships, etc.) were not included in this analysis. Data on costs of goods sold per bottle were provided by DSI and are confidential. Visitcostpermth is the compensation paid to agents to visit a household once per month (7.5 gourdes). We determined the optimal price for cost recovery by maximizing Equation 2 with respect to price, for cases with and without visits (assuming that the chlorine supplier yields enough market power to set price).
Incremental cost-effectiveness analysis.
We used two approaches to evaluate cost-effectiveness of marketing strategies from the perspective of donors that have a limited budget to create greater health impact than what is achieved by chlorine suppliers seeking to maximize cost recovery.
First, to illustrate how decisions could be made to best use donor funds in the current program, we compared cost-effectiveness of subsidies for visit-only versus price-only strategies. For the price-only strategy, we calculated the price without visits that results in the same net revenue as the visit-only strategy (conducting visits at the current retail price of 25 gourdes). Then we evaluated the ratio of purchase rates under these two equal-cost scenarios.
Second, to estimate cost-effectiveness of a wider range of potential strategies using a more generalizable metric, we evaluated the incremental cost-effectiveness ratio of marketing strategies relative to the net-revenue maximizing strategy:
| 3 |
Costpv is the marginal cost of the marketing strategy of offering price p and visit status v, calculated as the difference in net revenue between that strategy and the net-revenue maximizing strategy (p*v*). Benefits are the marginal health gains (expressed in disability-adjusted life years [DALYs]) that result from increased chlorine purchases relative to the net-revenue maximizing conditions. Estimates of the health impact of chlorine in Haiti (DALYs per bottle) were obtained using Population Services International (PSI)’s Impact Calculator,† which is based on data from the Lives Saved Tool, a multicause mortality model developed by Johns Hopkins Bloomberg School of Public Health. We adjusted PSI’s estimate that 16,200 chlorine tablets would need to be sold in Haiti to prevent the loss of 1 DALY by the relative amounts of water treated by chlorine tablets and one bottle of Gadyen Dlo.
RESULTS
For the census, 27 sales agents turned in 3,648 names. Seven agents subsequently chose not to participate in monthly visits and reporting. Of the 20 agents who turned in at least one report, 11 turned in forms for at least 4 months during the study period. We restricted all subsequent analysis to the 4 months (December 2013–March 2014) for which we had data for all 1,798 households served by these 11 agents.
During the 4-month analysis period, 58.5% of households purchased at least once and 37.0% purchased at least twice. The average household purchased 0.319 bottles per month (Table 2). Note that converting this to a percentage likely underestimates the number of households who possessed chlorine at any time, since one bottle lasts the average household up to 2 months.
Table 2.
Experimental data
| Offer price in Haitian gourdes per bottle of chlorine (45 gourdes/1 USD) |
||||||
|---|---|---|---|---|---|---|
| 5 | 10 | 15 | 20 | 25 | Pooled | |
| Purchased at least once | ||||||
| Visits | 72% (133/184) | 66% (120/182) | 66% (110/168) | 61% (109/179) | 52% (97/185) | 63% (569/898) |
| No visits | 71% (122/171) | 64% (119/187) | 56% (106/190) | 47% (84/178) | 45% (78/174) | 57% (509/900) |
| Pooled | 72% (255/355) | 65% (239/369) | 60% (216/358) | 54% (193/357) | 49% (175/359) | 60% (1,078/1,798) |
| Difference | * | *** | *** | |||
| Purchased at least twice | ||||||
| Visits | 52% (96/184) | 50% (91/182) | 46% (77/168) | 35% (62/179) | 27% (50/185) | 40% (376/898) |
| No visits | 46% (78/171) | 44% (82/187) | 33% (63/190) | 28% (50/178) | 18% (31/174) | 34% (304/900) |
| Pooled | 49% (174/355) | 47% (173/369) | 39% (140/358) | 31% (112/357) | 23% (81/359) | 38% (680/1,798) |
| Difference | ** | ** | *** | |||
| Purchases per household per month | ||||||
| Visits | 0.450 | 0.401 | 0.371 | 0.313 | 0.246 | 0.356 |
| No visits | 0.389 | 0.372 | 0.291 | 0.239 | 0.197 | 0.298 |
| Pooled | 0.420 | 0.386 | 0.328 | 0.276 | 0.222 | 0.327 |
| Difference | ** | ** | *** | |||
P < 0.10; ** P < 0.05; *** P < 0.01; for purchased at least once and twice, P values are for Pearson’s χ2 test of visits vs. no visits; for purchases per household per month, P values are for two-tailed t test for difference in means (visits vs. no visits).
Demand analysis.
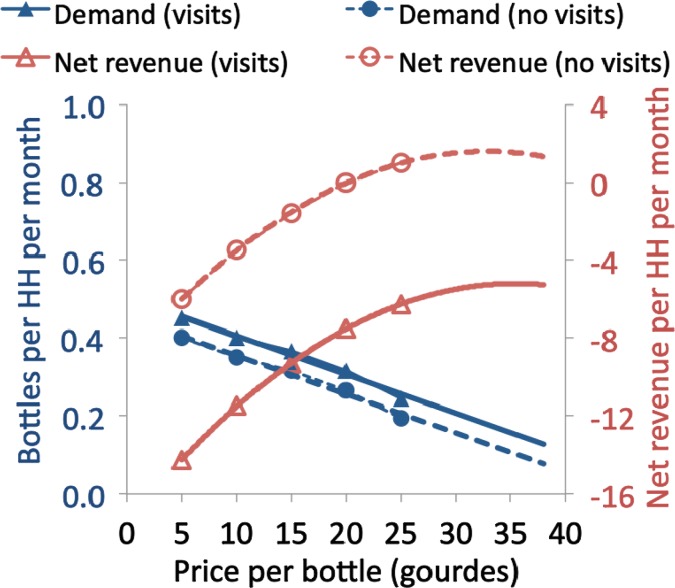
Pooling over 100% of price levels (5, 10, 15, 20, 25 gourdes), households who received visits were more likely to purchase at least once (61.1% versus 56.0%, P = 0.021), more likely to purchase at least twice (39.9% versus 34.2%, P = 0.009), and purchased more per month (0.340 versus 0.299 bottles per month, P = 0.004) than households who did not receive visits. Monthly purchases were greater for visited households than nonvisited households at all five prices (Figure 1B), but the difference is significant at the P = 0.05 level only at the 15 and 20 gourde price points (Table 2).
Figure 1.
(A) Three outcome variables vs. price. (B) Demand curve for visit and no-visit groups.
The number of bottles purchased per month ranged from 0.222 at 25 gourdes to 0.420 at 5 gourdes (Table 2 and Figure 1A). In simple linear regression models, price coefficients are negative and significant at the P < 0.001 level for all three outcome variables. On average, each 1-gourde drop in price increases the number of bottles purchased per month by 0.0101 (column 1, Table 3). The price elasticity of demand at the mean price (15 gourdes) and purchase rate (0.342 purchases per month) is 0.46, meaning that for every 1% drop in price, purchases increased by 0.46%.
Table 3.
Regression results: impact of price and visits on chlorine purchases
| Dependent variable | Bottles purchased per month |
At least once | At least twice | ||||
|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
| Price | −0.0101 | −0.0101 | −0.0103 | −0.0102 | −0.0118 | −0.0140 | |
| (0.0011)*** | (0.0011)*** | (0.0011)*** | (0.0021)*** | (0.0016)*** | (0.0016)*** | ||
| Visit | 0.0580 | 0.0581 | 0.0508 | 0.0522 | 0.0505 | 0.0697 | |
| (0.0163)*** | (0.0159)*** | (0.0185)*** | (0.0292) | (0.0262)* | (0.0258)*** | ||
| Midprice × visits | 0.0191 | 0.0127 | 0.0458 | 0.0295 | |||
| (0.0236) | (0.0149) | (0.0338) | (0.0332) | ||||
| Constant | 0.4788 | 0.2978 | 0.4498 | 0.4527 | 0.4513 | 0.7428 | 0.5476 |
| (0.0196)*** | (0.0113)*** | (0.0209)*** | (0.0209)*** | (0.0326)*** | (0.0295)*** | (0.0289)*** | |
| R2 | 0.043 | 0.007 | 0.050 | 0.050 | 0.084 | 0.033 | 0.047 |
| N | 1,798 | 1,798 | 1,798 | 1,798 | 1,798 | 1,798 | 1,798 |
| SER | 0.339 | 0.345 | 0.338 | 0.338 | 0.250 | 0.482 | 0.474 |
| Sales agent fixed effects? | No | No | No | No | Yes | No | No |
P < 0.1; ** P < 0.05; *** P < 0.01; heteroskedasticity-robust standard errors in parentheses.
In the model with both treatment variables, those who received visits purchased 0.0581 more bottles per month, and each 1-gourde ($0.02) drop in price increases bottles purchased per month by 0.0101 (column 3, Table 3). Interaction between visits and bottles purchased per month was modeled in seven different ways, and the model that explained the most variance was the one with midpriceij. The coefficient of this term was not statistically significant, but it was positive (βC = 0.019), implying that households that received visits at the 15 and 20 gourdes price point purchased 0.019 more bottles per month than households who were visited at lesser or greater prices (column 4, Table 3). Including sales agent fixed effects increases the percent of variation explained by the multivariate model from 5% to 8% without substantially changing the magnitude of the price and visit coefficients (column 5, Table 3). We used predicted values from Model 4 (Table 3), which includes the midpriceij interaction term, in all subsequent analyses.
Cost recovery analysis.
Only one of the 10 conditions tested experimentally (no visits, 25 gourdes) had positive monthly net revenue per household (Figure 2). At all prices tested, net revenue is greater when visits are not conducted than when they are. Net revenue for all conditions that include visits (minimum −14.3 to maximum −6.3 gourdes per household per month) was less than the lowest net revenue observed in the no-visit group (−6.0 gourdes per household per month). The prices that maximize net revenue are 31.9 gourdes per bottle if no visits are conducted and 35.3 gourdes per bottle if visits are conducted.
Figure 2.
Demand and net revenue curves. This figure appears in color at www.ajtmh.org.
Incremental cost-effectiveness analysis.
Relative to the current retail price and no visits, adding visits would increase purchases by 26.1% (0.194 to 0.245 bottles per month). Not conducting visits and lowering the price to 4.54 gourdes would result in the same net revenue per household and would increase purchases by 108.9% (0.194 to 0.406 bottles per month). Thus, the purchase increase for this level of price discount is 4.2 times greater than the purchase increase from adding visits at the current retail price.
Relative to the net-revenue maximizing conditions, the costs of strategies to increase demand through household visits range from $428 to $611 per DALY for the five prices tested (Figure 3). Of the five prices tested, the price that minimizes costs per DALY under scenarios that include visits is 15 gourdes per bottle, which costs $428 per DALY. This is greater than the costs for all strategies that do not include visits, which range from $66 to $260 per DALY. Thus, lowering the price to the lowest point tested (5 gourdes) is more cost-effective than adding visits at any price point. Costs per DALY for all strategies tested were less than the gross domestic product per capita in Haiti, which is used by some as a threshold for identifying “very cost-effective” interventions.
Figure 3.
Incremental cost-effectiveness relative to net-revenue maximizing strategy.
DISCUSSION
We randomly assigned 1,798 households in rural Haiti to receive or not receive monthly household visits and to receive one of five prices from $0.11 to $0.56 per bottle of chlorine solution. Each 1-gourde ($0.02) drop in price increases monthly household purchases by 0.010; at the mean price, each 1% drop in price increases purchases by 0.45%. Crude analysis indicates that household visits increase monthly household purchases by 19.7%, but this result is not statistically significant for all prices or for all agents. Net revenue is greater for households who do not receive visits than for those who do, even ignoring variation in sales agents, which is the more generous model specification with respect to the impact of visits at prices at which there is the strongest evidence of a positive effect. Choosing the optimal price and visit strategy depends on whether the program aims to maximize health impact, cost recovery, or cost-effectiveness (Table 4).
Table 4.
Summary of implications of model for managerial decisions
| Goal of program | |||
|---|---|---|---|
| Maximize demand (and health impact) | Maximize cost recovery | Maximize cost-effectiveness of a limited subsidy | |
| Price | Choose lowest price possible; of conditions tested, 5 gourdes maximized demand | 31.9 gourdes per bottle | Decrease price to lowest point possible, then add visits |
| Visits | Conduct visits | No visits | |
As expected, to maximize health impact through chlorine use, retail price should be set as low as possible and visits should be conducted. The Haitian government’s policy is that free distributions of HWTS products should be limited to emergency situations, so we did not test a 0 price point. By extrapolating the linear-linear model, we predict that the average household would acquire 0.45 or 0.50 bottles per month (for no visits and visits, respectively) if the price were zero. Note that this may underestimate demand for free chlorine solution because a constant elasticity (log-log) model may be a better fit at the tail ends.
To maximize cost recovery, household visits should not be conducted and the retail price should be 31.9 gourdes per bottle. This is not far from the retail price at the time of the study, indicating that DSI appears to have been acting rationally in its pursuit of sustainability, though these findings can help DSI fine-tune how it balances its dual goals of sustainability and health impact. Note that chlorine sales revenue still would not necessarily cover all of the costs to provide chlorine to households since we did not include all fixed costs in our analysis. This, as well as the fact that only one of the 10 conditions tested had positive net revenue, underscores the challenges in achieving full cost recovery for HWTS products in rural Haiti.
These results highlight the tradeoffs between health impact and cost recovery in populations with low WTP. In rural Haiti, there is a market for HWTS products, but strategies aimed solely at achieving cost recovery will likely result in missed opportunities to generate health impact. If resources exist to stimulate demand beyond such strategies, the most cost-effective use of a limited budget is to decrease retail price as much as possible and then add visits if funding still allows.
Historically, price interventions have been the least commonly used “P” in marketing strategies for HWTS consumables,37 including the DSI program, though price subsidies have been used for durable HWTS products56 and consumables in emergency contexts.57 Our results imply that shifting the focus to price subsidies for HWTS consumables in development contexts could lead to greater health gains. Designing price subsidies require donor flexibility but offer cost-effective opportunities to prevent morbidity and mortality.
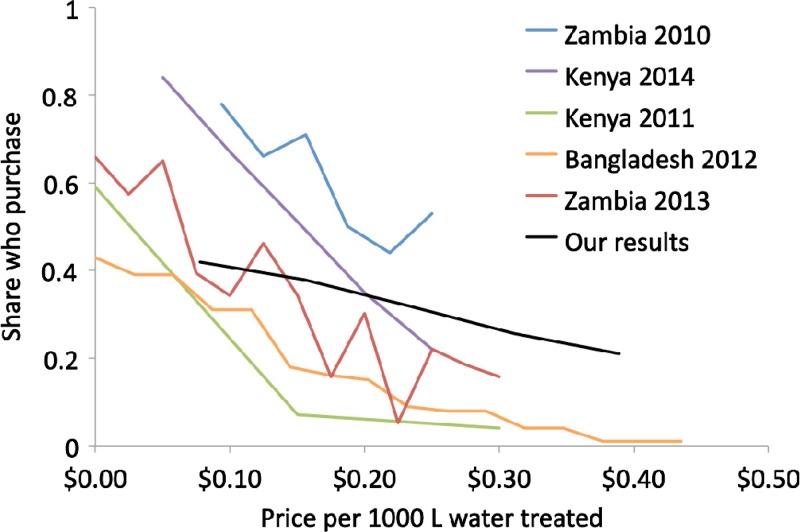
We found households in Haiti to be less sensitive to price than in other contexts.29 In five randomized studies, price elasticities of demand for chlorine solution ranged from 0.6 to 1.4 at mean prices (Table 1), whereas we found a price elasticity of 0.45 at mean price (approximated demand curves are shown in Figure 4). Since households were in the program up to 11 years prior to the study, we hypothesize that length of prior exposure to the product explains some of the variation in elasticities. High cholera rates58 may have decreased the Haitian population’s price sensitivity relative to other countries. Haitian households responded similarly to different prices to use community wells: for each gourde the monthly subscription fee increased, 0.6% of households stopped subscribing,59 which falls within the range we would predict based on the observed drop in demand for a bottle of chlorine solution that lasts 1–2 months.
Figure 4.
Comparative demand curves for chlorine solution. This figure appears in color at www.ajtmh.org.
Our findings are consistent with other studies that found statistically significant but modest effects of interpersonal communication on chlorine use. The estimate of the effect of household visits using previous data from this population was much larger.54 Some of the estimated effect may have been due to endogeneity, as program staff did not randomly select which households to visit, or to a decrease in households’ sensitivity to visits over time. Repeated exposure to messages and increased perceived risk due to the introduction of cholera are plausible explanations for this change. If marginal returns to visits are indeed decreasing, our results may underestimate the impact of visits on purchases in areas with less exposure to the product.
However, total costs of conducting visits may also be higher for other programs. DSI had existing program infrastructure for recruiting and managing sales agents, which minimized the marginal cost of administering the visit strategy. Those fixed costs were not included in our calculations but may be substantial for new programs that lack existing networks of sales agents. We note that less than half of agents who conducted a census followed the study protocol, underlining the potential for high agent turnover costs if the implementing partner seeks the level of data collection described here. After this experiment, DSI maintained a relatively stable cohort of agents that has continued doing visits for several years. This equilibrium supports the validity of our costing approach in making recommendations for DSI’s ongoing programs, but the cost of visit strategies may be higher for external programs, especially those in the agent recruitment phase and those that require high levels of reporting.
We found some evidence for interaction of household visits and price. Descriptive statistics indicated that visits had the greatest impact on purchase behavior at moderate prices (15 and 20 gourdes), which were the only two price points with a statistically significant difference in mean bottles purchased per month between visit and no-visit households. The interaction term was positive but not statistically significant in multivariate models. An interaction effect is consistent with a scenario in which households are most affected by interpersonal communication at prices at which they are indifferent between purchasing and not purchasing; at high prices, the extra push from visits is insufficient to overcome the price barrier, and at low prices, visits are not necessary to convince some households to buy and not relevant to other households who do not purchase even at low prices. Evidence for interaction between interpersonal communication and hygiene-related behavior was found in Zambia, where information scripts increased the effectiveness of chlorine price subsidies,28 and India, where shame-based campaigns increased the effectiveness of subsidies on latrine ownership60 and forced deliberation increased the effectiveness of low prices on soap purchases.22 However, no evidence was found for interaction between price discounts and marketing scripts on bednet purchases in Kenya17 or price discounts and information scripts on purchases of shoes, soap, and vitamins in Kenya, Guatemala, Uganda, and India.61 More research is needed to more fully understand the interaction of price subsidies and interpersonal communication.
One potential source of downward bias of our estimate of the visit effect is the possibility that agents visited households that were in the nonvisit group. This is unlikely, given the agents’ previous lack of interest in doing visits without compensation, the distance between houses, and the lack of instances of agents asking for additional compensation for doing “extra visits.”
Misclassification of sales toward lower price groups could bias our price elasticity estimate upward. Two factors may have led to such misclassification. First, agents had a financial incentive to record sales to households in lower price groups than the price that was actually paid. Second, households may have sold chlorine for a profit to neighbors who were in higher price groups. To monitor for potential fraud or arbitrage, DSI Supervisors conducted unannounced spot checks and asked households what price they paid. Spot checks did not provide evidence of misclassification, nor did the disaggregation of demand curves by sales agent, which were linear and homogenous.
Our study is limited by the lack of demographic data, which prevented us from verifying that the randomization process successfully eliminated any significant differences between treatment groups with respect to relevant variables. Additionally, we did not confirm whether households were aware of their price discount offers, but the information was provided equally to all treatment groups during community meetings.
Our results should be interpreted as providing a picture of chlorine purchase behavior among households served by the DSI program, but not necessarily among the population at large. The census conducted by DSI sales agents identified all “active program households” at the time, but the percentage of households located in communities served by a sales agent that were included in that agent’s census varies by locality, approaching 100% in some but not all cases.
The sample we analyzed was not representative of all households in the program because we excluded data from agents who failed to turn in at least four reports. Since excluded agents were geographically heterogeneous, it is unlikely that households they served would have responded differently to price variations than households in our sample. Agents who did not meet the reporting criteria may have been less invested in the program and less effective at persuading households to purchase chlorine, so we speculate that the effect of visits for the entire group of agents who conducted the census may be lower than our estimate. Limiting our sample to a 4-month period decreased our sample size but reduced missing data bias since not all twelve agents turned in reports during the rest of the study period. We completed a reanalysis using less stringent exclusion criteria (including data from November 2013 to April 2014). This resulted in the same coefficient estimate for price, a slightly higher estimate for visits, but did not change conclusions regarding relative net revenue and cost-effectiveness. Likewise, sensitivity analysis indicated that a 50% increase or decrease in cost per bottle did not change the relative cost-effectiveness of visits and price discounts.
Future research could analyze the distributional equity of HWTS marketing strategies by incorporating socioeconomic data and could identify whether factors such as length of exposure to the product determine the effectiveness of price subsidies or interpersonal communication. While many HWTS programs use interpersonal communication, few randomized studies have been conducted, and prior studies exhibit heterogeneity with respect to message content and role of the promoter. For example, we did not provide sales agents with a script as was done by Jalan and others,51 Luoto and others,27 and Quick and others.53 While it may be difficult to develop a precise but generalizable estimate of the effects of interpersonal communication on HWTS use, future research could explore ways to increase effectiveness of visits through targeting context-specific behavioral determinants or certain types of households. Implementing targeted approaches may be difficult and costly, though some HWTS programs in Haiti have constructed household wealth indices and are considering targeted subsidies.
Further investigations could also explore whether households used chlorine products as substitutes or complements to Gadyen Dlo, how this affected the competitiveness of Gadyen Dlo from a cost recovery perspective, and how best to attribute health impact to this program.
Finally, we note that purchase rates varied considerably between sales agents, and that treating sales agents as fixed effects increased the amount of variance explained and caused the coefficient of visits to lose its statistical significance. Future research could more fully explore models of the effect of agents on sales and seek to identify determinants of high performance among agents as salespeople and as persuasive visitors.
This research informs the evolving literature on how price affects demand for preventive health products in developing countries. We incorporated implications for the sustainability of supply, which is a critical but often missing element of these discussions. Decisions about behavior change campaigns and pricing for preventive health products in developing countries have implications for health impact, cost recovery, and cost-effectiveness, and tradeoffs between these goals should be quantified and made explicit in programmatic design.
Acknowledgments:
We thank the Deep Springs International field staff and sales agents in Jolivert; Jeff Zabel for comments on statistical methods; and Elizabeth Tenney and Maclain Borsich for entering and cleaning data.
Footnotes
Population Services International Impact Calculator can be accessed at http://impactcalculator.psi.org/intervention/261.
REFERENCES
- 1.World Health Organization, United Nations Children’s Emergency Fund (UNICEF) , 2015. Progress on Sanitation and Drinking Water: 2015 Update and MDG Assessment. Geneva, Switzerland: WHO; Available at: http://www.unicef.org/publications/files/Progress_on_Sanitation_and_Drinking_Water_2015_Update_.pdf. Accessed September 26, 2016. [Google Scholar]
- 2.Onda K, LoBuglio J, Bartram J, 2012. Global access to safe water: accounting for water quality and the resulting impact on MDG progress. Int J Environ Res Public Health 9: 880–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clasen T, Haller L, 2008. Water Quality Interventions to Prevent Diarrhoea: Cost and Cost-Effectiveness. Geneva, Switzerland: World Health Organization; Available at: http://www.who.int/water_sanitation_health/economic/prevent_diarrhoea.pdf. Accessed September 26, 2016. [Google Scholar]
- 4.Fewtrell L, Kaufmann RB, Kay D, Enanoria W, Haller L, Colford JM, 2005. Water, sanitation, and hygiene interventions to reduce diarrhoea in less developed countries: a systematic review and meta-analysis. Lancet Infect Dis 5: 42–52. [DOI] [PubMed] [Google Scholar]
- 5.Clasen T, Schmidt WP, Rabie T, Roberts I, Cairncross S, 2007. Interventions to improve water quality for preventing diarrhoea: systematic review and meta-analysis. BMJ 334: 782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clasen T, 2015. Household water treatment and safe storage to prevent diarrheal disease in developing countries. Curr Environ Health Rep 2: 69–74. [DOI] [PubMed] [Google Scholar]
- 7.Clasen T, Roberts I, Rabie T, Schmidt WP, Cairncross S, 2006. Interventions to improve water quality for preventing diarrhoea (review). Cochrane Database Syst Rev 3: CD004794 Available at: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004794.pub3/epdf. Accessed September 26, 2016. [DOI] [PubMed] [Google Scholar]
- 8.Quick R, Kimura A, Thevos AK, Tembo M, Shamputa I, Hutwagner L, Mintz E, 2002. Diarrhea prevention through household-level water disinfection and safe storage in Zambia. Am J Trop Med Hyg 66: 584–589. [DOI] [PubMed] [Google Scholar]
- 9.Quick R, Venczel LV, Mintz E, Soleto L, Aparicio J, Gironaz M, Hutwagner L, Greene KD, Bopp C, Maloney K, Chavez D, Sobsey MD, Tauxe RV, 1999. Diarrhoea prevention in Bolivia through point-of-use water treatment and safe storage: a promising new strategy. Epidemiol Infect 1222: 83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luby S, Agboatwalla M, Hoekstra RM, Rahbar MH, Billhimer W, Keswick B, 2004. Delayed effectiveness of home-based interventions in reducing childhood diarrhea, Karachi, Pakistan. Am J Trop Med Hyg 71: 420–427. [PubMed] [Google Scholar]
- 11.Crump JA, Otieno PO, Slutsker L, Keswick BH, Rosen DH, Hoekstra RM, Vulule JM, Luby SP, 2005. Household based treatment of drinking water with flocculant-disinfectant for preventing diarrhoea in areas with turbid source water in rural western Kenya: cluster randomised controlled trial. BMJ 331: 478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosa G, Clasen T, 2010. Estimating the scope of household water treatment in low- and medium-income countries. Am J Trop Med Hyg 82: 289–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cayemittes M, Busangu MF, Bizimana JdD, Barrere B, Severe V, Cayemittes V, Charles E, 2013. Enquete Mortalite, Morbidite et Utilisation des Services EMMUS-V. Petion-Ville, Haiti: Institut Haitien de l’Enfance and Calverton, MD: MEASURE DHS ICF International; Available at: http://www.mspp.gouv.ht/site/downloads/EMMUS V web.pdf. Accessed September 26, 2016. [Google Scholar]
- 14.Population Services International (PSI) , 2012. Enquete de suivi sur les determinants de l’utilisation des produits de traitement de l’eau au niveau des menages ayant des enfants de moins 5 ans en Haiti. Washington, DC: PSI; Available at: http://pdf.usaid.gov/pdf_docs/PA00JWZJ.pdf. Accessed September 26, 2016. [Google Scholar]
- 15.Hulland K, Martin N, Dreibelbis R, DeBruicker Valliant J, Winch P, 2015. What Factors Affect Sustained Adoption of Safe Water, Hygiene and Sanitation Technologies? A Systematic Review of Literature. London, United Kingdom: EPPI-Centre, Social Science Research Unit, UCL Institute of Education, University College London; Available at: https://eppi.ioe.ac.uk/cms/LinkClick.aspx?fileticket=FNNRVPIRw9g%3D&tabid=3475. Accessed September 26, 2016. [Google Scholar]
- 16.Dupas P, 2011. Health behavior in developing countries. Annu Rev Econ 3: 425–449. [Google Scholar]
- 17.Dupas P, 2009. What matters (and what does not) in households’ decision to invest in malaria prevention? Am Econ Rev 99: 224–230. [DOI] [PubMed] [Google Scholar]
- 18.Cohen J, Dupas P, 2010. Free distribution or cost-sharing? Evidence from a randomized malaria prevention experiment. Q J Econ 125: 1–45. [Google Scholar]
- 19.Dupas P, 2014. Short-run subsidies and long-run adoption of new health products: evidence from a field experiment. Econometrica 82: 197–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffmann V, 2009. Intrahousehold allocation of free and purchased mosquito nets. Am Econ Rev 99: 236–241. [Google Scholar]
- 21.Kremer M, Miguel E, 2007. The illusion of sustainability. Q J Econ 122: 1007–1065. [Google Scholar]
- 22.Spears D, 2014. Decision costs and price sensitivity: field experimental evidence from India. J Econ Behav Organ 97: 169–184. [Google Scholar]
- 23.Harvey P, 1994. The impact of condom prices on sales in social marketing programs. Stud Fam Plann 25: 52–58. [PubMed] [Google Scholar]
- 24.Ashraf N, Berry J, Shapiro JM, 2010. Can higher prices stimulate product use? Evidence from a field experiment in Zambia. Am Econ Rev 100: 2383–2413. [Google Scholar]
- 25.Blum A, Null C, Hoffmann V, 2014. Marketing household water treatment: willingness to pay results from an experiment in rural Kenya. Water 6: 1873–1886. [Google Scholar]
- 26.Kremer M, Miguel E, Mullainathan S, Zwane AP, Null C, 2011. Social Engineering: Evidence from a Suite of Take-up Experiments in Kenya. Available at: http://eml.berkeley.edu/~emiguel/pdfs/chlorinedispensers.pdf. Accessed September 26, 2016.
- 27.Luoto J, Mahmud M, Albert J, Luby S, Najnin N, Unicomb L, Levine DI, 2012. Learning to dislike safe water products: results from a randomized controlled trial of the effects of direct and peer experience on willingness to pay. Environ Sci Technol 46: 6244–6251. [DOI] [PubMed] [Google Scholar]
- 28.Ashraf N, Jack BK, Kamenica E, 2013. Information and subsidies: complements or substitutes? J Econ Behav Organ 88: 133–139. [Google Scholar]
- 29.Null C, Kremer M, Miguel E, Hombrados JG, Meeks R, Zwane AP, 2012. Willingness to pay for cleaner water in less developed countries: systematic review of experimental evidence. International Initiative for Impact Evaluation, Systematic Review 006. Available at: http://www.3ieimpact.org/media/filer_public/2012/05/28/sr006.pdf. Accessed September 26, 2016.
- 30.Contzen N, Mosler HJ, 2013. Impact of different promotional channels on handwashing behaviour in an emergency context: Haiti post-earthquake public health promotions and cholera response. J Public Health 21: 559–573. [Google Scholar]
- 31.Curtis V, Kanki B, Cousens S, Diallo I, Kpozehouen A, Sangare M, Nikiema M, 2001. Evidence of behaviour change following a hygiene promotion programme in Burkina Faso. Bull World Health Organ 79: 518–527. [PMC free article] [PubMed] [Google Scholar]
- 32.Kassegne S, Kays MB, Nzohabonayo J, 2011. Evaluation of a social marketing intervention promoting oral rehydration salts in Burundi. BMC Public Health 11: 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Levine R, 2007. Case 8: Preventing diarrheal deaths in Egypt. Case Studies in Global Health: Millions Saved. Sudbury, MA: Jones and Bartlett Publishers. [Google Scholar]
- 34.Hirschhorn N, 1985. Saving children’s lives: a communication campaign in Egypt. Dev Commun Rep 51: 13–14. Available at: http://files.eric.ed.gov/fulltext/ED288513.pdf. Accessed September 26, 2014. [PubMed] [Google Scholar]
- 35.Wang W, MacDonald VM, Paudel M, Banke KK, 2011. National scale-up of zinc promotion in Nepal: results from a post-project population-based survey. J Health Popul Nutr 29: 207–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Armstrong JRM, Abdulla S, Nathan R, Mukasa O, Marchant TJ, Kikumbih N, Mushi AK, Mponda H, Minja H, Mshinda H, Tanner M, Lengeler C, 2001. Effect of large-scale social marketing of insecticide-treated nets on child survival in rural Tanzania. Lancet 357: 1241–1247. [DOI] [PubMed] [Google Scholar]
- 37.Evans WD, Pattanayak SK, Young S, Buszin J, Rai S, Bihm JW, 2014. Social marketing of water and sanitation products: a systematic review of peer-reviewed literature. Soc Sci Med 110: 18–25. [DOI] [PubMed] [Google Scholar]
- 38.Parker AA, Stephenson R, Riley PL, Ombeki S, Komolleh C, Sibley L, Quick R, 2006. Sustained high levels of stored drinking water treatment and retention of hand-washing knowledge in rural Kenyan households following a clinic-based intervention. Epidemiol Infect 134: 1029–1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Freeman MC, Quick RE, Abbott DP, Ogutu P, Rheingans R, 2009. Increasing equity of access to point-of-use water treatment products through social marketing and entrepreneurship: a case study in western Kenya. J Water Health 7: 527–534. [DOI] [PubMed] [Google Scholar]
- 40.O’Reilly CE, Freeman MC, Ravani M, Migele J, Mwaki A, Ayalo M, Ombeki S, Hoekstra RM, Quick R, 2008. The impact of a school-based safe water and hygiene programme on knowledge and practices of students and their parents: Nyanza Province, western Kenya, 2006. Epidemiol Infect 136: 80–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Migele J, Ombeki S, Ayalo M, Biggerstaff M, Quick R, 2007. Diarrhea prevention in a Kenyan school through the use of a simple safe water and hygiene intervention. Am J Trop Med Hyg 76: 351–353. [PubMed] [Google Scholar]
- 42.Greene LE, Freeman MC, Akoko D, Saboori S, Moe C, Rheingans R, 2012. Impact of a school-based hygiene promotion and sanitation intervention on pupil hand contamination in Western Kenya: a cluster randomized trial. Am J Trop Med Hyg 87: 385–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wilson JM, Chandler GN, 1993. Sustained improvements in hygiene behaviour amongst village women in Lombok, Indonesia. Trans R Soc Trop Med Hyg 87: 615–616. [DOI] [PubMed] [Google Scholar]
- 44.Cairncross S, Shordt K, 2004. It does last! Some findings from a multi-country study of hygiene sustainability. Waterlines 22: 4–7. [Google Scholar]
- 45.Hanchett S, Krieger L, Kahn MH, Kullmann C, Ahmed R, 2011. Long-Term Sustainability of Improved Sanitation in Rural Bangladesh. New York, NY: World Bank; Available at: http://www.wsp.org/sites/wsp.org/files/publications/WSP-Sustainability-Sanitation-Bangladesh-Report.pdf. Accessed September 26, 2016. [Google Scholar]
- 46.Ross RK, King JD, Damte M, Ayalew F, Gebre T, Cromwell EA, Teferi T, Emerson PM, 2011. Evaluation of household latrine coverage in Kewot woreda, Ethiopia, 3 years after implementing interventions to control blinding trachoma. Int Health 3: 251–258. [DOI] [PubMed] [Google Scholar]
- 47.Wood S, Foster J, Kols A, 2012. Understanding why women adopt and sustain home water treatment: insights from the Malawi antenatal care program. Soc Sci Med 75: 634–642. [DOI] [PubMed] [Google Scholar]
- 48.Olembo L, Kaona F, Tuba M, Burnham G, 2004. Safe Water Systems: An Evaluation of the Zambia Clorin Program. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; Available at: http://www.ehproject.org/pdf/others/zambia report format.pdf. Accessed September 26, 2016. [Google Scholar]
- 49.Wheeler J, Agha S, 2013. Use of Certeza point-of-use water treatment product in Mozambique. J Water Sanit Hyg Dev 3: 341. [Google Scholar]
- 50.Harris JR, Patel MK, Juliao P, Suchdev PS, Ruth LJ, Were V, Ochieng C, Faith SH, Kola S, Otieno R, Sadumah I, Obure A, Quick R, 2012. Addressing inequities in access to health products through the use of social marketing, community mobilization, and local entrepreneurs in rural western Kenya. Int J Popul Res 2012: 1–9. [Google Scholar]
- 51.Jalan J, Somanathan E, 2008. The importance of being informed: experimental evidence on demand for environmental quality. J Dev Econ 87: 14–28. [Google Scholar]
- 52.Luoto J, Levine D, Albert J, Luby S, 2014. Nudging to use: achieving safe water behaviors in Kenya and Bangladesh. J Dev Econ 110: 13–21. [Google Scholar]
- 53.Quick R, 2003. Changing community behaviour: experience from three African countries. Int J Environ Health Res 13 (Suppl 1): S115–S121. [DOI] [PubMed] [Google Scholar]
- 54.Ritter M, 2008. Determinants of Adoption of Household Water Treatment Products in Rural Haiti. Atlanta, GA: Emory University; Available at: http://bit.ly/Ritter_MPH_Thesis. Accessed September 26, 2016. [Google Scholar]
- 55.Harshfield E, Lantagne D, Turbes A, Null C, 2012. Evaluating the sustained health impact of household chlorination of drinking water in rural Haiti. Am J Trop Med Hyg 87: 786–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yildizbayrak B, Moschos N, Tamar T, Le Tallee Y, 2004. Distribution of Arsenic Biosand Filters in Rural Nepal. Cambridge, MA: MIT Sloan School of Management; Available at: http://web.mit.edu/watsan/Docs/Student Reports/Nepal/NepalSloanABFReport2004.pdf. Accessed September 26, 2016. [Google Scholar]
- 57.Lantagne DS, Clasen TF, 2012. Use of household water treatment and safe storage methods in acute emergency response: case study results from Nepal, Indonesia, Kenya, and Haiti. Environ Sci Technol 46: 11352–11360. [DOI] [PubMed] [Google Scholar]
- 58.Barzilay EJ, Schaad N, Magloire R, Mung KS, Boncy J, Dahourou GA, Mintz ED, Steenland MW, Vertefeuille JF, Tappero JW, 2013. Cholera surveillance during the Haiti epidemic: the first 2 years. N Engl J Med 368: 599–609. [DOI] [PubMed] [Google Scholar]
- 59.Aliprantis D, 2014. What Is the Equity-Efficiency Tradeoff when Maintaining Wells in Rural Haiti? Working Paper, Federal Reserve Bank of Cleveland: Available at: https://www.clevelandfed.org/newsroom-and-events/publications/working-papers/2014-working-papers/wp-1424-what-is-the-equity-efficiency-tradeoff-when-maintaining-wells-in-rural-haiti.aspx. Accessed September 26, 2016. [Google Scholar]
- 60.Pattanayak SK, Yang J-C, Dickinson KL, Poulos C, Patil SR, Mallick RK, Blitstein JL, Praharaj P, 2009. Shame or subsidy revisited: social mobilization for sanitation in Orissa, India. Bull World Health Organ 87: 580–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Meredith J, Robinson J, Walker S, Wydick B, 2013. Keeping the doctor away: experimental evidence on investment in preventative health products. J Dev Econ 105: 196–210. [Google Scholar]