Abstract
Atrial fibrillation (AF) is a really uncommon arrhythmia in newborns. Here, we report the case of a 1-day-old infant who was recovered in Neonatal Intensive Care Unit for a twin-to-twin transfusion. The appearance of an unexpected AF was registered at his continuous electrocardiographic monitoring. Both chest X-ray and echocardiographic examination revealed the anomalous insertion of the tip of a central venous catheter (CVC) into the heart (‘umbilical artery → inferior vena cava → right atrium → patent foramen ovale → left atrium’). AF ceased as soon as the CVC was extracted from the heart. The mechanical irritation of both atria caused by the malposition of the CVC might be the underlying mechanism responsible for the triggering of AF in this unique case report.
INTRODUCTION
Atrial fibrillation (AF) is very uncommon in newborns and children.
Other possible even rarest causes of AF in this age range include severe rheumatic heart disease, cardiomyopathies, atrial tumours, infective endocarditis, lymphangiectasia, idiopathic paroxysmal forms, as well as endocardial fibroelastosis [1].
Uncontrolled AF may induce detrimental effects on the cardiovascular system, because it increases the risk of heart failure, thromboembolic events and prolongation of hospital stay.
Central venous catheters (CVCs) are usually inserted in critically ill newborns requiring intravenous therapy. During the placement of these catheters, sometimes their tip may advance into the heart, thereby increasing the risk of infection, thrombosis, cardiac perforation and not dangerous arrhythmias (extrasystolic atrial beats) [2]. The overall complication rate in positioning CVC is reported to be around 4% [2].
Here, we describe a case of AF induced by the malposition of CVC in a newborn, not previously reported in the literature.
CASE REPORT
One-day-old twin male newborns were admitted to the Neonatal Intensive Care Unit (NICU) of the University of Cagliari, Italy, because suffering from a twin-to-twin transfusion syndrome. The latter is a complication of aberrant placental blood vessels growth in monochorionic multiple pregnancies, when two or more fetuses share a chorion and hence a single placenta. This condition translates into an unbalanced blood flow distribution between the two fetuses, with consequent risk of death, which is 60–100% in the most severe forms [3].
The twins were born preterm at 30 weeks of gestational age after a caesarean delivery. The bigger of the twins weighed 2.4 kg, the smaller 1.2 kg. Their Apgar scores were 7–8 and 5–6 at 1 and 5 min, respectively.
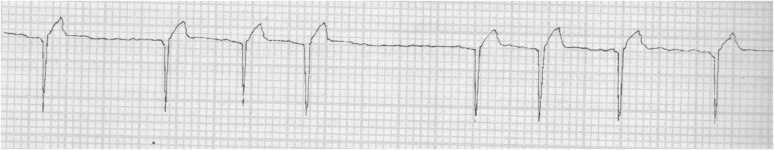
Immediately after the admission, a silicone CVC with diameter 3.5 French (Vygon Italia Srl, Padua, Italy) was inserted by NICU nurses into the twin's umbilical veins. After about half an hour, the appearance of an unexpected AF was registered at the continuous electrocardiogram (ECG) monitoring of the smaller twin (see Fig. 1).
Figure 1:
Single lead (D1) electrocardiographic monitoring shows the presence of AF in the monitored newborn.
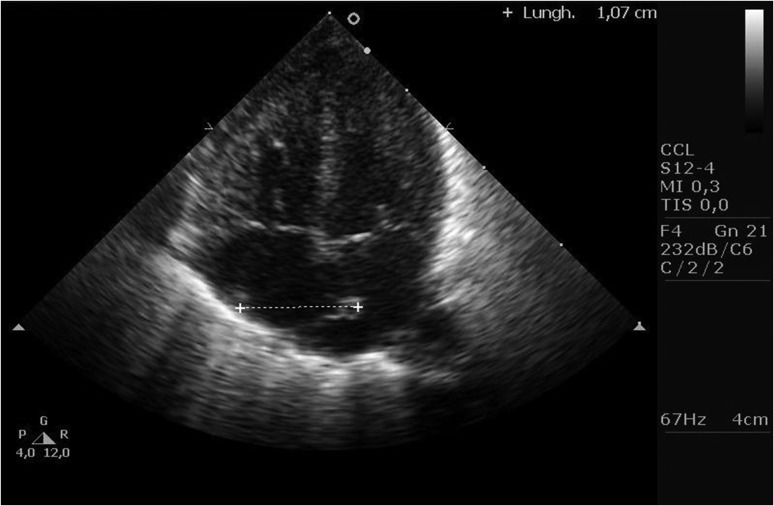
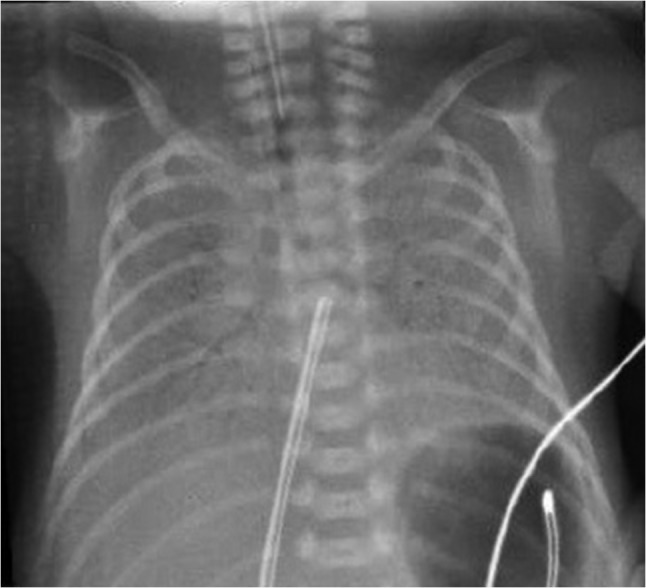
The malposition of the tip of CVC was shown by means of chest X-ray and confirmed at echocardiographic examination (see Figs 2 and 3). Specifically, ultrasound examinations showed the anomalous insertion of the tip of the CVC into the heart (‘umbilical artery → inferior vena cava → right atrium → patent foramen ovale → left atrium’). No cardiac malformations were found at ultrasounds examination.
Figure 2:
Chest X-ray shows the malposition of the tip of the CVC into the left atrium of the heart.
Figure 3:
The malposition of the tip of the CVC into the heart is confirmed at ultrasound examination.
On the basis of this finding, the CVC was withdrawn 2 cm and the conversion to sinus rhythm followed immediately. No further AF episodes were registered during newborn hospitalization.
DISCUSSION
This is the second report of the occurrence of AF in a preterm newborn with structurally normal heart [1].
In literature, the occurrence in a 1-month-old premature infant of another supraventricular tachycardia—i.e. atrial flutter with 2:1 block—had been reported as well. The possible contribution from an intracardiac catheter and the administration of broad spectrum antimicrobial agents in that arrhythmic event had been discussed as well. Regarding the latter, it had been previously discovered that some antimicrobial compounds may have a pro-arrhythmic effect proven in adults, but with limited data available in newborns [4].
A slightly increased risk of ventricular arrhythmias for CVC jugular and subclavian veins cannulation had been described as well [5].
As above stated, AF increases the risk of thromboembolic events. In addition, also CVC insertion may induce thrombus formation through the rupture of the endothelium and the interruption of the laminar blood flow induced by the local trauma from catheter insertion and the physical presence of the catheter itself. These events lead to the exposure of the blood to the venous intima lyer which, in turn, can lead to local activation of the coagulation cascade. In this respect, subcutaneous low-molecular-weight heparin is usually administered in NICU, in order to decrease the risk of CVC-related thrombi formation. In our little patient, no clot-induced adverse events have been observed.
About a pathophysiological interpretation of the AF occurrence in our baby, it can be hypothesized that the mechanical irritation of both atria caused by the malposition of the CVC might be the underling mechanism responsible for the triggering of this arrhythmia. In fact, when withdrawing the CVC, immediately AF disappeared. In this respect, the increased sympathetic tone due to the trauma may have triggered atrial automatic potentials and sustained them by lowering the atrial refractory period, thus resulting in anomalous multiple electrical microreentry circuits [5].
Other possible causes concurring to the occurrence of AF might have been low birth weight, prematurity at birth, low Apgar score, as well as hypovolaemia and anaemia [6].
In this case, due to the unique aetiology of AF, a pharmacological prophylaxis against supraventricular arrhythmias was not administered, without AF recurrences neither during recovery nor after discharge from the NICU [7].
Generally speaking, AF in paediatric age represents a strong indication for a complete investigation of the patient. When positioning CVCs, chest X-ray is usually mandatory to localize catheter tip [8]. The diagnosis of CVC malposition, with the precise localization of the tip, may be confirmed at echocardiographic examination. Echocardiography is a simple and unharmful tool for neonatologists in a number of clinical scenarios [9]. An ECG guidance when positioning CVC has been suggested as well [10].
In our NICU, CVCs are usually positioned by doctors. They had empirically chosen the length of the catheter on the basis of the child's measurement from umbilicus to shoulder, an old and with a limited reliability method. In a few minutes, the AF appeared at ECG monitoring.
The CVCs insertion check-list include a routinely performed chest X-ray. When the catheter malposition is put on evidence by the latter, an echocardiogram is usually performed for a better definition of the tip of the catheter.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL APPROVAL
Not required, since this is not an experiment involving humans or animal. Informed written consent to publish this case report has been obtained from the patient's parents.
GUARANTOR
Pier Paolo Bassareo.
REFERENCES
- 1. Estlin EJ, Bennett MK, Skinner JR, Milligan DW, Wren C. Atrial fibrillation with neonatal pulmonary lymphangiectasia. Acta Paediatr 1998;87:1304–6. [DOI] [PubMed] [Google Scholar]
- 2. Casado-Flores J, Barja J, Martino R, Serrano A, Valdivielso A. Complications of central venous catheterization in critically ill children. Pediatr Crit Care Med 2001;2:57–62. [DOI] [PubMed] [Google Scholar]
- 3. Dodge KL, Lynch CA, Moore CL, Biroscak BJ, Evans LV. Use of ultrasound guidance improves central venous catheter insertion success rates among junior residents. J Ultrasound Med 2012;31:1519–26. [DOI] [PubMed] [Google Scholar]
- 4. Obidi E, Toubas P, Sharma J. Atrial flutter in a premature infant with a structurally normal heart. J Matern Fetal Neonatal Med 2006;19:113–4. [DOI] [PubMed] [Google Scholar]
- 5. Polderman KH, Girbes AJ. Central venous catheter use. Part 1: mechanical complications. Intensive Care Med 2002;28:1–17. [DOI] [PubMed] [Google Scholar]
- 6. Kohut J, Durmala J, Rokicki W, Golba E, Goc B, Petelenz J. Analysis of the cardiac arrhythmias in premature infants throughout the 24 hours following birth using Holter method. Wiad Lek 2002;55:535–41. [PubMed] [Google Scholar]
- 7. Tavera MC, Bassareo PP, Neroni P, Follese C, Manca D, Montis S, et al. Supraventricular tachycardia in neonates: antiarrhythmic drug choice dilemma. J Matern Fetal Neonatal Med 2010;23:30–3. [DOI] [PubMed] [Google Scholar]
- 8. Kieran EA, Laffan EE, O'Donnell CP. Estimating umbilical catheter insertion depth in newborns using weight or body measurement: a randomised trial. Arch Dis Child Fetal Neonatal Ed 2016;101:10–5. [DOI] [PubMed] [Google Scholar]
- 9. Dodge KL, Lynch CA, Moore CL, Biroscak BJ, Evans LV. Use of ultrasound guidance improves central venous catheter insertion success rates among junior residents. J Ultrasound Med 2012;31:1519–26. [DOI] [PubMed] [Google Scholar]
- 10. Pittirutti M, La Greca A, Scoppettuolo G. The electrocardiographic method for positioning the tip of central venous catheters. J Vascul Access 2011;12:280–91. [DOI] [PubMed] [Google Scholar]