Abstract
Purpose
Ras/MEK/ERK pathway activation is common in oral cavity squamous cell carcinoma (OCSCC). We performed a neoadjuvant (pre-operative) trial to determine biomarker and tumor response of OCSCC to MEK inhibition with trametinib.
Patients and Methods
Patients with Stage II–IV OCSCC received trametinib (2 mg/day, minimum 7 days) prior to surgery. Primary tumor specimens were obtained before and after trametinib to evaluate immunohistochemistry staining for p-ERK1/2 and CD44, the primary endpoint. Secondary endpoints included changes in clinical tumor measurements and metabolic activity (maximum Standardized Uptake Values [SUVmax] by F-18 fluorodeoxyglucose positron emission tomography/computed tomography), and in tumor downstaging. Drug-related adverse events (AEs) and surgical/wound complications were evaluated.
Results
Of 20 enrolled patients, 17 (85%) completed the study. Three patients withdrew because of either trametinib-related (n=2:nausea, duodenal perforation) or unrelated (n=1:constipation) AEs. The most common AE was rash (9/20 patients, 45%). Seventeen patients underwent surgery. No unexpected surgical/wound complications occurred. Evaluable matched pre- and post-trametinib specimens were available in 15 (88%) of these patients. Reduction in p-ERK1/2 and CD44 expression occurred in 5 (33%) and 2 (13%) patients, respectively. Clinical tumor response by modified World Health Organization criteria was observed in 11 of 17 (65%) evaluable patients (median 46% decrease, range 14 to 74%). Partial metabolic response (≥25% reduction in SUVmax) was observed in 6 of 13 (46%) evaluable patients (median 25% decrease, range 6 to 52%). Clinical-to-pathologic tumor downstaging occurred in 9 of 17 (53%) evaluable patients.
Conclusions
Trametinib resulted in significant reduction in Ras/MEK/ERK pathway activation and in clinical and metabolic tumor responses in OCSCC patients.
Keywords: trametinib, oral cavity squamous cell carcinoma, window clinical trials
Introduction
Oral cavity squamous cell carcinoma (OCSCC) is a global health problem that arises from the carcinogenic transformation of oral mucosa, primarily as a result of tobacco and alcohol abuse. OCSCC is clinically distinct from the human papillomavirus (HPV)–related oropharyngeal squamous cell carcinomas (OPSCC) (1, 2). Patients with HPV+ OPSCC have excellent outcomes with non-surgical or surgical therapy. In contrast, OCSCC is primarily treated with surgical approaches followed by adjuvant radiation therapy but has an overall poorer prognosis despite significant advances in surgical and radiation techniques. Thus, there is a clear rationale for integrating new therapeutic approaches within the primary surgical paradigm with the goals of reducing tumor burden and the extent of necessary surgical resection, and to lower relapse rates. Because of the ease of monitoring tumor response and performing biopsies for correlative biomarker studies in OCSCC, neoadjuvant “window-of-opportunity” studies provide an invaluable opportunity to assess novel therapeutic agents in this disease (3, 4).
The extracellular signal-regulated kinase 1 and 2 (ERK1/2) mitogen-activated protein kinase (MAPK) pathway orchestrates a central role in neoplastic disease with pleiotropic effects including proliferation, survival, apoptosis and migration (5, 6). Mutations in the Ras and Raf small GTPases act as key cancer cell-specific drivers of ERK activation via upstream MEK1/2 triggering and create pathway-specific targeting opportunities. However, data from COSMIC and The Cancer Genome Atlas (TCGA) analysis show that Ras and Raf are infrequently mutated in OCSCC; only 4–8% H-Ras isoform alterations and few K-Ras, N-Ras or BRAF mutations have been identified (4, 7). Alternative mechanisms exist to activate the ERK1/2 pathway. Specifically, wild-type Ras overexpression and alterations in numerous growth factor and other non-canonical pathways converge to activate ERK1/2 (8–12). In fact, immunohistochemical (IHC) analysis of phosphorylated ERK1/2 (p-ERK1/2) has shown that the majority of OCSCCs had activation of this pathway (8–12). Thus, OCSCC harbors a combination of alterations in Ras, growth factor and other non-canonical drivers of the ERK1/2 pathway that together stimulate tumor progression and suggest, as in other tumors, that this pathway may be an exploitable therapeutic target.
Our rationale for pursuing therapeutic targeting of MEK originated from a carcinogen-induced mouse model of OCSCC where we identified increased p-ERK1/2 activation to be associated with more aggressive tumor growth. We also linked activated ERK with increased cell surface CD44 expression, which together contributed to increased in vitro invasion and in vivo growth. Analysis of primary human OCSCCs confirmed an association between higher p-ERK1/2 levels and CD44 expression (13). We hypothesized that aggressive tumor growth mediated by these molecules may be due to their activity in putative cancer stem cells (CSCs) or cells undergoing an epithelial-to-mesenchymal (EMT) transition (14–17). Thus, previous work and our laboratory findings provide a firm rationale for therapeutic targeting of the MEK pathway in OCSCCs.
Trametinib (GSK1120212) is an allosteric MEK1/2 inhibitor that has a longer half-life than previous generation MEK inhibitors (18, 19). Trametinib is Food and Drug Administration (FDA) approved for use as single agent or in combination with dabrafenib for incurable BRAF mutant melanoma (20, 21). In these studies, trametinib was generally well tolerated with rash, nausea, vomiting, hypertension and diarrhea being the most common adverse events (AEs). MEK inhibitors have yet to be evaluated in head and neck squamous cell carcinoma (HNSCC), specifically in OCSCC. In this trial, we hypothesized that administration of the MEK inhibitor trametinib to patients with OCSCC would result in reductions in biomarkers of Ras/MEK/ERK pathway activation and in tumor size and metabolic activity, as measured by clinical examination and positron emission tomography/computed tomography with F18 -fluorodeoxyglucose (FDG-PET/CT). We chose the neoadjuvant setting to test this hypothesis because biopsies of the primary tumor site and surgical resection are standard of care diagnostic and therapeutic procedures for OCSCC and thus provided a convenient, unique “window-of-opportunity” to evaluate our hypotheses. Herein, we report the results of our translational trial.
Patients and Methods
Study Population
Eligible subjects were ≥18 years of age with stage II-IVa OCSCC (AJCC, 7th Edition), Eastern Cooperative Oncology Group performance status ≤ 1, and adequate organ function. Exclusion criteria included history of other active malignancy within the last 3 years, interstitial lung disease, pneumonitis, QTc ≥ 480 milliseconds, uncontrolled hypertension, and presence of a defibrillator. Baseline echocardiography or radionuclide ventriculography was performed to assess left ventricular ejection fraction as was ophthalmologic examination to evaluate for retinal abnormalities that predispose to retinal vein occlusion or central serous retinopathy.
The clinical trial and correlative studies were approved by the Washington University Human Research Protection Office and registered nationally (NCT01553851). All patients were required to provide written informed consent to participate.
Study Design
Each patient underwent an incisional biopsy of the primary tumor site and venipuncture to collect peripheral blood (30 mL). Tissue and blood specimens were immediately processed and used for correlative studies as described below. Patients were scheduled to take trametinib 2 mg orally once daily for 7–16 days prior to surgical resection. The range of doses permitted accommodation in the scheduling of surgery; however, a minimum of seven daily doses of trametinib was required with the last dose of trametinib given within 24 hours of surgery. Beginning on day 1 of study drug administration, patients were monitored for AEs by weekly history taking, physical examination, and laboratory testing (complete blood counts and metabolic panel), along with daily phone calls to the patient by the study coordinator or physician to assess for AEs. AEs were assessed using descriptions and grading scales found in the revised NCI Common Terminology Criteria for Adverse Events (CTCAE) version 4.0.
After at least seven daily doses of trametinib, patients underwent definitive surgical resection of the primary tumor site and regional neck dissection to remove involved or at-risk neck nodes. Some patients also underwent reconstruction of the primary surgical field by free flap or adjacent tissue transfer techniques. Tumor resection margins were defined by baseline assessments and were not altered based on response to trametinib therapy. Tissue from the primary tumor site was obtained at the time of surgery, as was additional peripheral blood, and immediately processed for correlative studies. Patients were monitored for AEs and for surgical/wound healing complications daily for the entire post-operative hospital stay and upon discharge, weekly through post-operative day 30.
Correlative Studies
Matched tumor biopsies obtained at baseline and on day of definitive surgery were divided and processed for IHC by immediate formalin fixation, and were processed for future genomic and proteomic studies by snap freezing in liquid nitrogen and xenografting into immunodeficient mice. Serum obtained at baseline and after trametinib was also stored.
IHC—Pre and post-treatment tumor biopsies were used to generate formalin fixed, paraffin embedded slide sections (FFPE, 5 micron). After antigen recovery using IHC-Tek Epitope Retrieval Solution for p-ERK1/2 (IHC World) and Retrievagen A for CD44 (BD Biosciences), these were immunostained for p-ERK1/2 (#9101, 1:200, Cell Signaling Technologies) or CD44 (Clone 1M7, 1:25, BD Biosciences) for 16 hours, at 4 °C. Detection was performed with an ABC kit developed with 3,3’-diaminobenzidine (DAB) for CD44 and VIP Peroxidase for p-ERK1/2 (Vector Labs) and slides were subsequently counterstained with Mayer’s hematoxylin. Slides were then independently evaluated by two dedicated head and neck pathologists (JSL and RDC) for percentage staining in quartiles (0 to 4 scale) and staining intensity (1–3 scale for weak, moderate, or strong). The sum of the intensity and quartile scaled score was expressed as the average expression score for each case. Cases with a ≥2 point change were considered as a significant reduction. In cases of discordance between pathologists, the two scores were summed to determine a mean score which was recorded as the consensus score that was used for the analysis.
Clinical Tumor Response Assessment
Assessment of tumor response at the primary site was performed by clinical examination and by FDG-PET/CT. For clinical assessment, we chose to measure the two largest dimensions of the tumor per modified World Health Organization (WHO) criteria (22) rather than RECIST, which is based on unidimensional measurement (23). Modified WHO criteria were used where partial responses (PR) were defined as ≥25% decrease in primary tumor size and progression was defined as ≥ 25% increase in primary tumor size. We used modified criteria because we only gave 2 weeks of study drug and chose to use a criteria model that would catch the early effect of short-term therapy with study drug. We reasoned that two-dimensional measurement would be a superior approach to assess clinical tumor response in the oral cavity as it is an anatomically complex region and tumors of this region are often of variable shapes. The primary tumor was measured in the two longest perpendicular axes within 7 days prior to starting trametinib and compared to intraoperative measurements at time of surgery. All baseline measurements were performed by the PI of the study (RU) and all post-treatment measurements were measured by the most senior surgeon involved at the time of surgical resection independent of the PI. Tumor response based on clinical examination was reported as the percentage change in the tumor area (product of two measurements) calculated as the difference between the pre- and post-trametinib tumor areas divided by the pre-trametinib tumor area, multiplied by 100.
Metabolic tumor response based on FDG-PET/CT was reported as the change in maximum Standardized Uptake Value (SUVmax) and was evaluated as previously described (24). Baseline FDG-PET/CT scans performed 2–3 weeks prior to starting trametinib were compared to a research-specific FDG-PET/CT performed the day before surgery and within 24 hours of the last dose of trametinib. Briefly, FDG-PET/CT was performed with one of several PET/CT scanners (Siemens Biograph 40HD (Siemens Medical Solutions USA, Inc., Malvern, PA), Siemens mCT (Siemens Medical Solutions USA, Inc.), and GE Discovery STE (GE Healthcare, Waukesha, WI). The post-trametinib FDG-PET/CT followed the same imaging procedure as the baseline study, except that imaging was limited to the head and neck region. FDG was administered intravenously (dose adjusted by weight per Division of Nuclear Medicine Body FDG-PET/CT imaging procedure), and imaging was begun 60 ± 10 min later. Non-contrast CT images used for attenuation correction and image fusion were acquired at 120 kVp with 111 mAs. The standard whole-body examination for the baseline study included images from the skull vertex to the upper thighs, acquired in two acquisitions. The first acquisition consisted of two bed positions from the skull vertex to the lung apices and the second acquisition encompassed the neck to the upper thighs. Only the head and neck region was imaged for the post-trametinib studies. Images were reconstructed at 5-mm slice thickness. FDG-PET/CT images were evaluated qualitatively as well as quantitatively by one of two experienced nuclear radiologists (FD or BAS). For quantitative analysis, SUVmax within the primary tumor site was determined within a volume of interest around the tumor using a Siemens eSoft workstation (Siemens Medical Solutions USA, Inc.). A decrease in SUVmax of ≥ 25% was used to define partial metabolic response (25).
Clinical and Pathologic Staging
Clinical staging was assessed before surgery by the Siteman Cancer Center multidisciplinary head and neck tumor board based on clinical examination and radiologic imaging using American Joint Committee on Cancer criteria (AJCC, 7th Edition). Primary site and nodal classification were determined using composite data extracted from clinical exam, neck CT and FDG-PET/CT scans. Pathologic staging was determined by standard primary tumor and lymph node assessments by dedicated head and neck surgical pathologists (JSL or RDC).
Baseline clinical staging and post-surgical pathologic staging was compared for each patient. Downstaging occurred when the clinical-to-pathologic stage decreased, placing the patient in a less advanced tumor stage which would improve prognosis and/or result in significant reduction in post-operative adjuvant treatment recommendation (for example, no chemotherapy or unilateral versus bilateral neck irradiation). Upstaging occurred when the clinical-to-pathologic stage increased, placing the patient in a more advanced tumor stage, which would worsen prognosis and/or result in significant increase in post-operative adjuvant therapy.
Statistical Analysis
Standard descriptive statistics were used to describe the demographic and clinical characteristics of the 20 subjects enrolled in the study. Frequency and relative frequency were used to describe distribution of data across levels of categorical variables. Median and range were used to describe distribution of continuous level variables with 95% confidence intervals calculated around the medians. A chi-square goodness-of-fit test was used to test the proportion of patients experiencing a clinical to pathological stage migration with the proportions from TCGA patients undergoing standard of care treatment.
Results
Patient and Tumor Characteristics
Twenty patients were enrolled and treated with trametinib (Table 1). Median age of patients was 59.5 years (range, 30 to 78 years), 95% were men, 90% were Caucasian and all but two had a history of smoking and/or alcohol abuse. The majority of patients had clinical Stage IV disease (70%). Tumor sub-sites were distributed throughout the oral cavity.
Table 1.
Patient demographics
| Characteristic | Endpoint | % |
|---|---|---|
| Patients Enrolled (#) | 20 | |
| Age (years) | ||
| Median | 59.5 | |
| Range | 30–78 | |
| Sex | ||
| Female | 1 | 5 |
| Male | 19 | 95 |
| Oral Cavity Sub-Site | ||
| Tongue | 7 | 35 |
| Floor of mouth | 7 | 35 |
| Retromolar trigone | 5 | 25 |
| Buccal | 1 | 5 |
| Clinical Stage | ||
| II (T2N0) | 3 (3) | 15 |
| III (T2N1, T3N1) | 3 (1,2) | 15 |
| IV (T2N2a, T2N2b, T3N2b, T4aN0, T4aN1,T4aN2b, T4aN2c) | 14 (1,3,1,2,1,3,3) | 70 |
Trametinib Drug Delivery and Adverse Events
All patients who received at least one dose of trametinib were evaluable for AEs. The median number of doses of trametinib taken by patients was 14 (range: 3–14). Seventeen patients (85%) received at least seven daily doses of trametinib. Sixteen patients (80%) received 12–16 daily doses of study drug.
Trametinib was well tolerated in most patients (Table 2). Seventeen of twenty patients tolerated trametinib therapy and completed surgical treatment. Six patients (30%) reported no drug-related AEs. The majority of AEs were mild (grades 1–2) and the most common AE was rash (45%). Two patients (10%) experienced trametinib-related AEs leading to discontinuation of the study drug. After seven doses of trametinib, one patient developed a duodenal perforation (grade 4) that required surgical intervention. After five doses of trametinib, a second patient developed nausea (grade 2) and withdrew from the study. One other patient developed trametinib-unrelated, narcotic-induced constipation (grade 2) and stopped trametinib after three doses.
Table 2.
Trametinib related adverse events
| Adverse Event | Grades 1–2 | Grades 3–4 | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Hematologic | ||||
| Neutrophil decrease | 1 | 5 | ||
| Thrombocytopenia | 1 | 5 | ||
| Gastrointestinal | ||||
| Colitis | 1 | 5 | ||
| Diarrhea | 3 | 15 | ||
| Mucositis | 1 | 5 | ||
| Nausea | 2 | 10 | ||
| Duodenal perforation | 1 | 5 | ||
| Stomach cramps | 1 | 5 | ||
| Infections | ||||
| Lung | 0 | 0 | 1 | 5 |
| Skin | ||||
| Rash, acneiform | 9 | 45 | ||
| Pruritis | 1 | 5 | ||
| Other | ||||
| Fatigue | 2 | 10 | ||
| Fever | 1 | 5 | ||
| Alkaline phosphatase | 3 | 15 | ||
| AST | 4 | 20 | ||
| ALT | 2 | 10 | ||
| Blurry vision | 1 | 5 | ||
| Hypotension | 1 | 5 | ||
Surgical Procedures and Complications
Nineteen patients (95%) underwent surgery. One patient’s treatment plan changed to a non-surgical approach because of slow recovery after duodenal perforation that occurred during trametinib dosing. The types of surgeries to remove the primary tumor and neck nodes and the reconstruction procedures performed are defined in Table 3. Surgical therapy involved local resections that were reconstructed with primary closure, skin graft, or regional flaps (42%) versus major composite resections that required microvascular free flap reconstructions (58%). All patients underwent either unilateral or bilateral neck lymph node dissections as dictated by the characteristics of the primary tumor.
Table 3.
Surgical treatment and complications
| Number | % | Complications | |
|---|---|---|---|
| Primary surgery | |||
| Glossectomy | 4 | 20 | None |
| FOM resection | 4 | 20 | None |
| Composite resection | 11 | 55 | None |
| Neck Dissections | |||
| Unilateral | 12 | 71 | None |
| Bilateral | 5 | 29 | None |
| Reconstruction | |||
| Primary closure/skin graft | 6 | 30 | None |
| Regional flap | 2 | 10 | None |
| Microvascular free flap | 11 | 55 | |
| Fibula | 1 | 5 | None |
| Scapula/latissimus dorsi | 1 | 5 | Flap failure, pectoralis flap salvage |
| Anterolateral thigh | 3 | 15 | None |
| Radial forearm | 6 | 30 | None |
Surgical outcomes were carefully monitored to assess for any unexpected AEs with tumor resections or reconstructions. During the operation, two patients (11%) were noted to have unusual edema of tissues with variable alterations of tissue planes. However, this observation did not adversely effect tumor resection or reconstruction, and analysis of resected tissue specimens revealed no correlative histopathologic abnormalities (data not shown). One patient (5%) experienced failure of a scapula/latissimus dorsi free flap due to a technical vessel geometry issue and was salvaged with a regional pectoralis flap reconstruction. The remaining patients (95%) had no post-operative surgical wound healing problems. One patient developed a pneumonia and sepsis following surgery and later expired. No clear relationship of these events to the study drug was established.
Biomarker Analysis
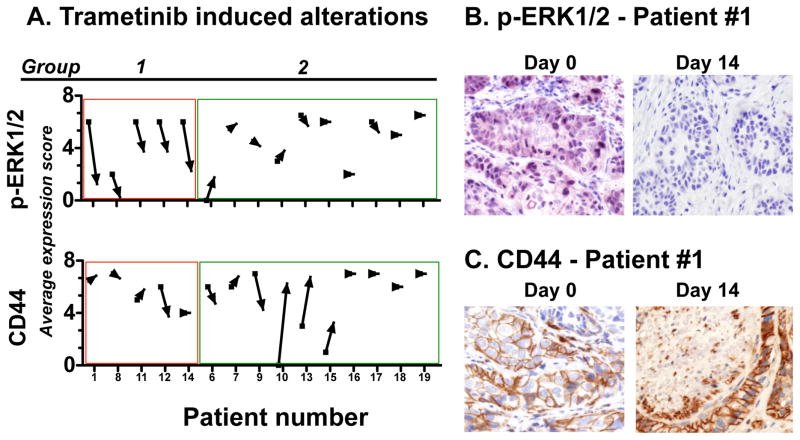
Fifteen patients had matched pre- and post-treatment biopsies with sufficient tumor content to be evaluable for biomarker assessment. These matched specimens were analyzed for p-ERK1/2 and CD44 expression using IHC (Figure 1). Tumor specimens from five of fifteen patients (33%, 95% CI: 9%–51%)) showed a decrease in p-ERK1/2 as determined by the average expression score which was the sum of the staining intensity and quartile distribution on IHC. These patients were designated as Group 1. The remaining 10 patients (Group 2) showed minimal change in p-ERK1/2 expression. Overall, reduction of p-ERK1/2 expression occurred in five patients and reduction of CD44 expression occurred in two patients. Only one patient (#12) displayed concordant decrease in both biomarkers with trametinib therapy.
Figure 1. p-ERK1/2 and CD44 immunohistochemistry of matched pre- and post-trametinib biopsy specimens identified 2 groups with differential response to trametinib.
(A) p-ERK1/2 (upper panel) and CD44 (lower panel) staining was quantitated and expressed as the average expression score which was the sum of the staining intensity and quartile distribution. The relative change of each from baseline to post-treatment is depicted with an arrow in direction of change and with groupings relative to p-ERK1/2. Group 1 patients showed a ≥2 point decrease in p-ERK1/2 staining and Group 2 showed equivocal change. Representative baseline and post-trametinib IHC stains of (B) p-ERK1/2 and (C) CD44 from patient 1 (400X magnification).
Clinical Tumor Responses
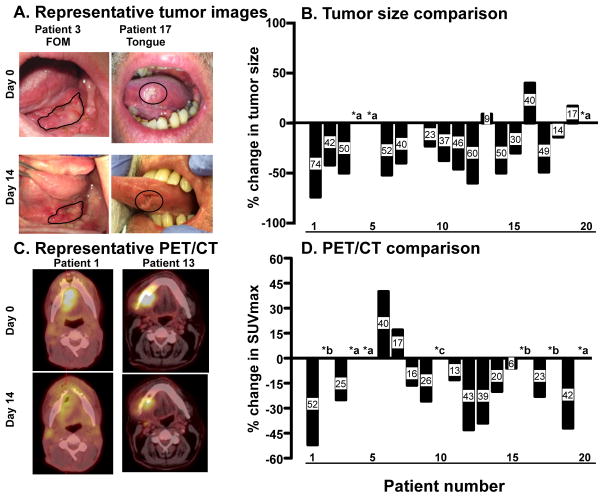
During trametinib therapy, measurable reductions in the primary tumor size occurred in many patients, along with concordant subjective decreases in tumor pain (Figure 2A). Quantitative changes in tumor size based on clinical examination were calculated by determining the area of the tumor at baseline and after trametinib based on two-dimensional measurements and expressed with modified WHO criteria. These data showed that 11/17 (65%) patients displayed PRs (≥ 25% reduction), 5/17 with stable disease, and 1/17 (6%) had PD (≥25% increase). The median reduction in tumor size for all patients with reductions was a 46% decrease (range 74 to 14%, Figure 2B). However, all surgical resections were completed using margins from the baseline tumor dimensions, thus encompassing the entire region where tumor was observed clinically prior to trametinib therapy.
Figure 2. Clinical and metabolic changes in trametinib-treated patients.
(A) Representative tumor photographs at baseline and post-treatment showing clinical changes in patient #3 and #17. (B) Percent change in tumor area across entire cohort. Tumor area was represented as the product of the two largest dimensions and percent change was calculated by ((Post area-Pre area)/Pre area) X 100. (*a represents patients who enrolled but did not complete the study). (C) Representative fused PET/CT images at baseline and post-treatment showing metabolic changes in patient #1 and #13. (D) Percent change in SUVmax of primary tumor in patients with available pre- and post-treatment PET/CT. The percentage change was calculated by ((PostSUVmax-PreSUVmax)/PreSUVmax) X 100. Patients 4, 5 and 20 did not complete the study (*a), patient 2, 16 and 18 (*b) did not have primary lesions that met size criteria for PET assessment and patient 10 chose not to undergo post-treatment PET/CT (*c).
Metabolic Tumor Responses
To define metabolic changes in the oral cavity tumor induced by trametinib, patients underwent a research-specific FDG-PET/CT performed after 12–14 days of starting trametinib and on the last day of trametinib that was compared to the baseline FDG-PET/CT (Figure 2C). Thirteen patients were evaluable for this endpoint. Seven patients were not evaluable because of either the absence of primary tumor lesions that met the protocol-defined size criteria (short axis ≥ 1.5 cm) for metabolic response assessment (n=3), patient withdrawal from the study (n=3), or patient declined the post-trametinib FDG-PET/CT (n=1). Assessing the change in SUVmax as the endpoint of interest in the 13 evaluable patients, 11 (85%) patients showed some decrease in the primary tumor site SUVmax (median 25%, range: 6–52%, Figure 2D), with six patients (46%) meeting criteria of a partial metabolic tumor response (≥ 25% reduction in SUVmax).
Clinical-to-Pathologic Tumor Downstaging after Trametinib
We examined whether the tumor responses to trametinib observed on clinical examinations and FDG-PET/CT were reflected in the final pathologic staging—that is, did the trametinib interval treatment alter the baseline clinical staging of the tumor? Of the 17 patients evaluable for this endpoint, downstaging occurred in 9 (53%) patients, no change in staging occurred in 7 (41%) patients, and upstaging occurred in 1 (6%) patient (Table 4A). Five of the nine patients had clinically staged (c)T2 tumors of which 4 showed size reductions after trametinib resulting in pathologically staged (p) T1 tumors (photographs of two of these patient’s tumors are in Figure 2A). Four patients had cT3 or cT4 and three of these showed reduction to either pT2 (2 patients) or to pT1 (1 patient) tumors. With respect to lymph node involvement, five of the nine patients who were cN+ were pathologically staged as either pN1 (1 patient) or pN0 (4 patients). Due to logistical/ethical issues, pathologic confirmation of lymph node involvement was not performed on patients prior to trametinib therapy. However, one patient did undergo fine needle aspiration biopsy of a suspicious lymph node confirming metastatic SCCA. Pathologic analysis of the neck dissection specimen in this patient did not show SCCA despite deeper step sectioning of lymph nodes (data not shown).
Table 4.
Trametinib downstaging and combined results summary
| A. Clinical versus pathologic staging | ||
|---|---|---|
| Patient | Clinical staging | Pathologic staging |
| Downstaged | ||
| 1 | IVa- T4aN2cM0 | III - T2N1M0 |
| 3 | IVa-T2N2bM0 | I-T1N0M0 |
| 6 | III- T2N1M0 | II-T2N0M0 |
| 9 | IVAa- T3N2bM0 | III-T3N0M0 |
| 10 | III -T3N1M0 | I-T1N0M0 |
| 11 | II-T2N0M0 | I-T1N0M0 |
| 16 | II-T2N0M0 | I-T1N0M0 |
| 17 | II-T2N0M0 | I-T1N0M0 |
| 18 | IVa-T4aN0M0 | II-T2N0M0 |
| Upstaged or no change | ||
| 2 | IVa-T2N2bM0 | IVa-T1N2bM0 |
| 7 | IVa- T4aN2cM0 | IVa-T4aN0M0 |
| 8 | III- T3N1M0 | IVa-T1N2bM0 |
| 12 | IVa - T4aN2bM0 | IVa - T4aN2bM0 |
| 13 | IVa-T4aN1M0 | IVa-T4aN0M0 |
| 14 | IVa-T2N2aM0 | IVa-T4aN0M0 |
| 15 | IVa- T4aN2bM0 | IVa-T4aN2bM0 |
| 19 | IVa-T4N2cM0 | IVa-T4N1M0 |
| B. TCGA versus trametinib staging | |||
|---|---|---|---|
| TCGA %(#) | Trametinib | Biron et al (2013) | |
| Same | 62.4 (147/237) | 41 (7/17) | 92.1 (128/139) |
| Down | 15.1 (37/237)* | 53(9/17)* | 7.9(11/139) |
| Up | 22.4 (53/237) | 6(1/17) | |
| C. Summary of two p-ERK patient groups | |||||
|---|---|---|---|---|---|
| Group 1 | Group 2 | ||||
| # | Size | PET/CT | # | Size | PET/CT |
| 1 | PR | PMR | 6 | PR | ↑ |
| 8 | NC | ↓ | 7 | ↓ | ↑ |
| 11 | PR | ↓ | 9 | ↓ | PMR |
| 12 | PR | PMR | 10 | PR | NA |
| 14 | PR | ↓ | 13 | ↑ | PMR |
| 15 | PR | ↓ | |||
| 16 | PD | NA | |||
| 17 | PR | ↓ | |||
| 18 | ↓ | NA | |||
| 19 | ↓ | PMR | |||
p=0.001
NC= no change
NA= not available
↓/↑= decrease or increase below level needed for PR/PMR or PD
To ascertain whether this observed stage migration effect was present in patients who underwent standard of care surgical therapy alone, we identified a large cohort of OCSCC patients from The Cancer Genome Atlas (TCGA) clinical database with documented clinical and pathologic staging. In contrast with the trametinib-treated patients in our study, only 36 of the 237 (16%) TCGA OCSCC patients were downstaged, with 148/237 (62%) unchanged and 53/237 (22%) upstaged (Table 4B). Thus, trametinib-treated patients had significantly increased downstaging compared to the standard of care TCGA cohort (p=0.001).
Comparison of p-ERK Expression and Clinical Tumor Response
A comparison of the changes in p-ERK1/2 expression with the clinical tumor responses as assessed by clinical examination and FDG-PET/CT (Table 4B) revealed that of the 5 patients in Group 1 (patients who had reduction in p-ERK), 2 patients showed concordant PRs and PMRs (patients 1 and 12). Patients 11 and 14 in Group 1 had reductions in p-ERK and clinical tumor size, and a non-significant reduction ( <25%) in SUVmax. Although several patients in Group 2 had either PRs or PMRs, none of these showed concordance with changes in p-ERK expression.
Discussion
So called “window-of-opportunity” clinical trials are an ideal model to assess therapeutic and/or biomarker alterations, and OCSCC is an excellent disease to apply this model given the ease of access for safe sequential tumor biopsies. The ability to compare a patient’s own baseline tumor biomarker signaling or FDG metabolic status to a post-treatment effect in sequential fashion represents a powerful model not afforded by isolated “snapshot” tumor biopsies. Herein, we completed a novel biomarker “window-of-opportunity” clinical trial with the MEK1/2 inhibitor trametinib in surgically treated OCSCC patients. Several key findings of this trial were encouraging with respect to future studies of trametinib in OCSCC. First, we were able to identify a substantial subset (33%) of evaluable patients whose tumor tissue displayed significant reduction of p-ERK1/2 expression with only 7–14 days of trametinib treatment. Second, decrease in tumor size (PRs) occurred in 65% of evaluable patients and metabolic tumor responses (PMRs) occurred in 46% of evaluable patients. These data show that trametinib has substantial anti-tumor activity in OCSCC. Finally, we noted an unexpected and robust tumor downstaging in 53% of evaluable patients with a brief interval of trametinib therapy that further supports exploration of MEK inhibition as a therapeutic strategy in OCSCC.
In this investigation, we focused on the ERK1/2 pathway because of its central role as a common downstream cascade in several oncogenic pathways and due to its importance in the biology of OCSCC. Although we did not annotate all of the proximal mechanisms of activation that could have been present in these patients, IHC analysis demonstrated that 5 of 15 evaluable patients (33%) displayed a significant decrease in p-ERK1/2 levels after up to two weeks of trametinib therapy. Thus, a significant proportion of patients with OCSCC may benefit with this novel therapeutic strategy demonstrating the importance of the Ras/MEK/ERK pathway in this disease. We speculate that tumors without p-ERK1/2 changes during trametinib therapy either do not have a p-ERK1/2 dependency or have an intrinsic bypass pathway that re-activates targeted MEK1/2.
Our laboratory findings in a mouse model of OCSCC and in primary human OCSCC led us to hypothesize a primary biomarker endpoint where targeted p-ERK1/2 reduction would be correlated with CD44 reduction. In our mouse model, we found that p-ERK1/2 transcriptionally regulated CD44 expression and this directly influenced cell migration. We extended these data to human tumor samples where we found a correlation of CD44 expression and ERK1/2 phosphorylation (13). Together, the mouse and human data represented the basis for the primary biomarker endpoint in the trametinib clinical trial. Although we observed a substantial subset of patients with p-ERK1/2 reduction, only one patient displayed concomitant tumor cell CD44 reduction. CD44 has several isoforms, and it is thus possible that specific CD44 isoforms that we did not detect were attenuated by MEK/ERK pathway targeting because we used a pan-CD44 antibody in IHC analysis. Also, IHC may not be a reliable method for quantification of changes in CD44 with therapies. Thus, it is also possible that a quantitative reduction in CD44 occurred in patients that we were not able to detect with this form of testing. Intra-tumoral heterogeneity, which likely was not captured by the biopsies, may also have contributed to our unexpected findings. Finally, our choice of CD44 as a target of the MEK/ERK pathway may not be valid and other biomarkers may be better correlated with inhibition of this pathway.
Trametinib was well tolerated in the majority of patients, with no significant surgical wound complication issues. As observed in other clinical contexts, the most common AEs due to trametinib were dermatologic, occurring in 45% of patients (20, 21). Seventeen of twenty patients (85%) completed the study as planned. Two patients withdrew from the study due to trametinib-related AEs (nausea; duodenal perforation) and one patient withdrew due to narcotic-related AE (constipation). Perforated duodenal ulcer occurred in one patient after 7 doses of trametinib. The patient had no history of peptic ulcer disease. Although this AE occurred during trametinib therapy, the cause of the AE is unclear. Duodenal ulcers are common in the general population (26). Two cases of perforated duodenal ulcer have been reported while taking trametinib (personal communication with Glaxo Smith Kline), and both cases occurred after greater than 50 doses. Thus, it is plausible that the perforated duodenal ulcer event that occurred in one patient in our study may have been causally unrelated to trametinib.
Given the short duration of trametinib therapy, we were surprised to observe reductions in tumor measurements based on clinical examinations in 65% of evaluable patients. These data, along with metabolic tumor responses and reductions in p-ERK expression, show that trametinib has substantial anti-tumor effects in OCSCC. An important caveat of this observation is that we used direct tumor measurement converted into modified WHO instead of unidimensional RECIST criteria because of the complex three-dimensional anatomy of the oral cavity. Thus, although we took steps to eliminate subjectivity (i.e. independent baseline and post-treatment measurements), this is a limitation of the finding of tumor size reduction. Additional studies with extended treatment are indicated to confirm our findings and further evaluate the clinical significance of these observations.
An intriguing observation from this trial was the tumor downstaging that occurred in 53% of evaluable patients. Upstaging only occurred in one patient (6%). Clinical staging was performed before surgery based on clinical examination and radiologic imaging in a multidisciplinary setting. Pathologic staging was performed postoperatively based on the findings in the pathology report. Clinical and pathology staging were compared for each patient. The downstaging effect of neoadjuvant trametinib observed in our trial is higher than that reported for patients undergoing standard-of-care therapy. Biron et al. (27) reported that downstaging occurred in 7.9% of patients with advanced OCSCC and our analysis of TCGA OCSCC patients showed a 16% stage decrease. With the limitation that our trial encompassed a small cohort of patients and that the TCGA data were not collected prospectively, this effect of trametinib given before surgery may be an important observation that has the capacity to impact the extent of surgical resection or the choice and intensity of adjuvant therapy. These hypotheses should be tested in appropriately designed clinical trials.
Limitations of this study include the small number of treated patients, the short duration of trametinib administration, and biopsy limitations that precluded analysis of all patients. Ongoing genomic and functional molecular correlative analysis of these respective tissues and accompanying autologous xenografts are directed at further understanding underlying tumor biology in this treatment setting and, ultimately, providing insight into identifiable determinants of response and resistance.
In conclusion, a brief duration of trametinib given to patients with OCSCC before surgery was well tolerated, and resulted in decreased expression of p-ERK in 33% of evaluable patients, reductions in tumor measurements in 65%, and metabolic tumor responses in 46%. Unexpectedly, tumor downstaging occurred in 53% of evaluable patients, an effect that could have a major impact on the extent of surgical resection and adjuvant therapy. Further studies of MEK inhibition with trametinib therapy are indicated in OCSCC.
Statement of Translational Relevance.
Because patients with advanced oral cavity squamous cell carcinoma (OCSCC) suffer from poor outcomes despite advances in multimodality approaches, there is an urgent need for novel therapeutic approaches. Based on emerging data on the crucial role of MAPK signaling in OCSCC, we hypothesized that the RAS/MEK/ERK pathway constitutes a central node where diverse signaling pathways may converge to drive OCSCC aggressiveness. However, there are no treatment data in OCSCC patients on the potential activity of MEK inhibitors such as trametinib in this disease. In this study, we completed a window of opportunity Phase II clinical trial with neoadjuvant trametinib in OCSCC patients and identified biomarker, metabolic and clinical changes in a large percentage of treated patients. Together, these data support further exploration of the clinical utility of trametinib and the mechanistic dissection of underlying molecular pathways.
Acknowledgments
We thank all patients and their families for participating in this study. We thank the Alvin J. Siteman Cancer Center at Washington University School of Medicine and Barnes-Jewish Hospital in St. Louis, Missouri for the use of the Clinical Trials Core, which provided protocol development and clinical trial support (including Franco Barbarescu, Kirsten Cady, Farley Johnson, Stephanie Myles and Casey Rowe), and for use of the Imaging and Response Assessment Core.
Grant Support This study was approved and funded by the National Comprehensive Cancer Network (NCCN) Oncology Research Program from general research support provided by Novartis Pharmaceutical Corporation (Novartis). RU is also supported by the NIH/NIDCR (DE024403). The Siteman Cancer Center is supported in part by NCI Cancer Center Support Grant #P30 CA91842, (Eberlein, PI).
Footnotes
Disclaimers: None
References
- 1.Bhatia A, Burtness B. Human Papillomavirus-Associated Oropharyngeal Cancer: Defining Risk Groups and Clinical Trials. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015;33(29):3243–50. doi: 10.1200/JCO.2015.61.2358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chinn SB, Myers JN. Oral Cavity Carcinoma: Current Management, Controversies, and Future Directions. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015;33(29):3269–76. doi: 10.1200/JCO.2015.61.2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gross ND, Bauman JE, Gooding WE, Denq W, Thomas SM, Wang L, et al. Erlotinib, erlotinib-sulindac versus placebo: a randomized, double-blind, placebo-controlled window trial in operable head and neck cancer. Clinical cancer research : an official journal of the American Association for Cancer Research. 2014;20(12):3289–98. doi: 10.1158/1078-0432.CCR-13-3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hammerman PS, Hayes DN, Grandis JR. Therapeutic insights from genomic studies of head and neck squamous cell carcinomas. Cancer discovery. 2015;5(3):239–44. doi: 10.1158/2159-8290.CD-14-1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fremin C, Meloche S. From basic research to clinical development of MEK1/2 inhibitors for cancer therapy. J Hematol Oncol. 2010;3:8. doi: 10.1186/1756-8722-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts PJ, Der CJ. Targeting the Raf-MEK-ERK mitogen-activated protein kinase cascade for the treatment of cancer. Oncogene. 2007;26(22):3291–310. doi: 10.1038/sj.onc.1210422. [DOI] [PubMed] [Google Scholar]
- 7.Cancer Genome Atlas N. Comprehensive genomic characterization of head and neck squamous cell carcinomas. Nature. 2015;517(7536):576–82. doi: 10.1038/nature14129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albanell J, Codony-Servat J, Rojo F, Del Campo JM, Sauleda S, Anido J, et al. Activated extracellular signal-regulated kinases: association with epidermal growth factor receptor/transforming growth factor alpha expression in head and neck squamous carcinoma and inhibition by anti-epidermal growth factor receptor treatments. Cancer research. 2001;61(17):6500–10. [PubMed] [Google Scholar]
- 9.Bancroft CC, Chen Z, Dong G, Sunwoo JB, Yeh N, Park C, et al. Coexpression of proangiogenic factors IL-8 and VEGF by human head and neck squamous cell carcinoma involves coactivation by MEK-MAPK and IKK-NF-kappaB signal pathways. Clinical cancer research : an official journal of the American Association for Cancer Research. 2001;7(2):435–42. [PubMed] [Google Scholar]
- 10.Hoover AC, Strand GL, Nowicki PN, Anderson ME, Vermeer PD, Klingelhutz AJ, et al. Impaired PTPN13 phosphatase activity in spontaneous or HPV-induced squamous cell carcinomas potentiates oncogene signaling through the MAP kinase pathway. Oncogene. 2009;28(45):3960–70. doi: 10.1038/onc.2009.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu SL, Herrington H, Reh D, Weber S, Bornstein S, Wang D, et al. Loss of transforming growth factor-beta type II receptor promotes metastatic head-and-neck squamous cell carcinoma. Genes Dev. 2006;20(10):1331–42. doi: 10.1101/gad.1413306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Molinolo AA, Amornphimoltham P, Squarize CH, Castilho RM, Patel V, Gutkind JS. Dysregulated molecular networks in head and neck carcinogenesis. Oral oncology. 2009;45(4–5):324–34. doi: 10.1016/j.oraloncology.2008.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Judd NP, Winkler AE, Murillo-Sauca O, Brotman JJ, Law JH, Lewis JS, Jr, et al. ERK1/2 Regulation of CD44 Modulates Oral Cancer Aggressiveness. Cancer research. 2012;72(1):365–74. doi: 10.1158/0008-5472.CAN-11-1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133(4):704–15. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ponta H, Sherman L, Herrlich PA. CD44: from adhesion molecules to signalling regulators. Nat Rev Mol Cell Biol. 2003;4(1):33–45. doi: 10.1038/nrm1004. [DOI] [PubMed] [Google Scholar]
- 16.Shin S, Dimitri CA, Yoon SO, Dowdle W, Blenis J. ERK2 but not ERK1 induces epithelial-to-mesenchymal transformation via DEF motif-dependent signaling events. Mol Cell. 2010;38(1):114–27. doi: 10.1016/j.molcel.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turley EA, Veiseh M, Radisky DC, Bissell MJ. Mechanisms of disease: epithelial-mesenchymal transition--does cellular plasticity fuel neoplastic progression? Nat Clin Pract Oncol. 2008;5(5):280–90. doi: 10.1038/ncponc1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilmartin AG, Bleam MR, Groy A, Moss KG, Minthorn EA, Kulkarni SG, et al. GSK1120212 (JTP-74057) is an inhibitor of MEK activity and activation with favorable pharmacokinetic properties for sustained in vivo pathway inhibition. Clinical cancer research : an official journal of the American Association for Cancer Research. 2011;17(5):989–1000. doi: 10.1158/1078-0432.CCR-10-2200. [DOI] [PubMed] [Google Scholar]
- 19.Yamaguchi T, Kakefuda R, Tajima N, Sowa Y, Sakai T. Antitumor activities of JTP-74057 (GSK1120212), a novel MEK1/2 inhibitor, on colorectal cancer cell lines in vitro and in vivo. Int J Oncol. 2011;39(1):23–31. doi: 10.3892/ijo.2011.1015. [DOI] [PubMed] [Google Scholar]
- 20.Flaherty KT, Infante JR, Daud A, Gonzalez R, Kefford RF, Sosman J, et al. Combined BRAF and MEK inhibition in melanoma with BRAF V600 mutations. The New England journal of medicine. 2012;367(18):1694–703. doi: 10.1056/NEJMoa1210093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flaherty KT, Robert C, Hersey P, Nathan P, Garbe C, Milhem M, et al. Improved survival with MEK inhibition in BRAF-mutated melanoma. The New England journal of medicine. 2012;367(2):107–14. doi: 10.1056/NEJMoa1203421. [DOI] [PubMed] [Google Scholar]
- 22.Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981;47(1):207–14. doi: 10.1002/1097-0142(19810101)47:1<207::aid-cncr2820470134>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 23.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. Journal of the National Cancer Institute. 2000;92(3):205–16. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 24.Adkins D, Ley J, Dehdashti F, Siegel MJ, Wildes TM, Michel L, et al. A prospective trial comparing FDG-PET/CT and CT to assess tumor response to cetuximab in patients with incurable squamous cell carcinoma of the head and neck. Cancer Med. 2014;3(6):1493–501. doi: 10.1002/cam4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Young H, Baum R, Cremerius U, Herholz K, Hoekstra O, Lammertsma AA, et al. Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron emission tomography: review and 1999 EORTC recommendations. European Organization for Research and Treatment of Cancer (EORTC) PET Study Group. Eur J Cancer. 1999;35(13):1773–82. doi: 10.1016/s0959-8049(99)00229-4. [DOI] [PubMed] [Google Scholar]
- 26.Lin KJ, Garcia Rodriguez LA, Hernandez-Diaz S. Systematic review of peptic ulcer disease incidence rates: do studies without validation provide reliable estimates? Pharmacoepidemiol Drug Saf. 2011;20(7):718–28. doi: 10.1002/pds.2153. [DOI] [PubMed] [Google Scholar]
- 27.Biron VL, O'Connell DA, Seikaly H. The impact of clinical versus pathological staging in oral cavity carcinoma--a multi-institutional analysis of survival. J Otolaryngol Head Neck Surg. 2013;42:28. doi: 10.1186/1916-0216-42-28. [DOI] [PMC free article] [PubMed] [Google Scholar]