Abstract
Although a robust literature has linked stable, high levels of fear across childhood to increased risk for anxiety problems, less is known about alternative pathways to anxiety. We tested two putatively normative developmental pathways of early fearfulness for their distinct associations with behavioral (anxiety related behaviors and symptoms) and biological (diurnal cortisol) markers of anxiety risk in middle childhood in a community-based sample (n=107). Steeper increases in fear from six to 36 months predicted more parent-reported anxiety symptoms at age eight years. Additionally, children who exhibited steep increases in fear during infancy were over-represented among children with diagnoses of separation anxiety disorder at age eight years. Finally, we showed that steeper increases in fearfulness in infancy predicted flatter slopes of diurnal cortisol at age eight years for girls. Thus, differences in stranger fear across infancy may indicate varying degrees of risk for anxious behaviors in later childhood.
Keywords: Stranger Fear Development, Cortisol, Anxiety Risk, Infancy
Heterogeneity in the developmental origins and outcomes of anxiety disorders presents a challenge to both clinical and developmental psychologists. Anxiety disorders are notable for their early onset (Beesdo, Knappe, & Pine, 2009; Egger & Angold, 2006; Mian, Godoy, Briggs-Gowan, & Carter, 2012) and lifetime persistence (Beesdo et al., 2007; Pine, Cohen, Gurley, Brook, & Ma, 1998), but heterogeneity in symptom presentation and in pathways to disorder is an impediment to identifying early markers of risk (Bell-Dolan, Last, & Strauss, 1990). Thus, delineating multiple pathways to risk may prove useful for preventing chronic mental health problems. Here, we examine developmental profiles of infant fearfulness elicited by strangers for distinct associations with later biological and behavioral markers of anxiety risk. We have previously identified these developmental profiles of infant fearfulness (Brooker, Buss, Lemery-Chalfant, Aksan, Davidson, & Goldsmith, 2013).
Developing Stranger Fear and Behavioral Markers of Anxiety Risk
Fear of unfamiliar conspecifics promotes adaptive behaviors and decreases the threat of physical harm to vulnerable, young offspring (Bowlby, 1973; Marks, 1987). Beginning mainly in the early 20th century (e.g., Bridges, 1932), researchers began to systematically measure negative reactions to strangers during the second half-year of life. Although the ubiquity and interpretation of this fear of strangers has been questioned (Rheingold & Eckerman, 1973), at about 7 months of age, human infants commonly display fear when confronted with unfamiliar adults (e.g., Sroufe, 1977). The magnitude of this fear response increases during the infant and toddler years (Andersson, Bohlin, & Hagekull, 1999; Hill-Soderlund & Braungart-Rieker, 2008) before dissipating at about 30 months of age (Cox & Campbell, 1968; Gershaw & Schwarz, 1971; Marks, 1987).
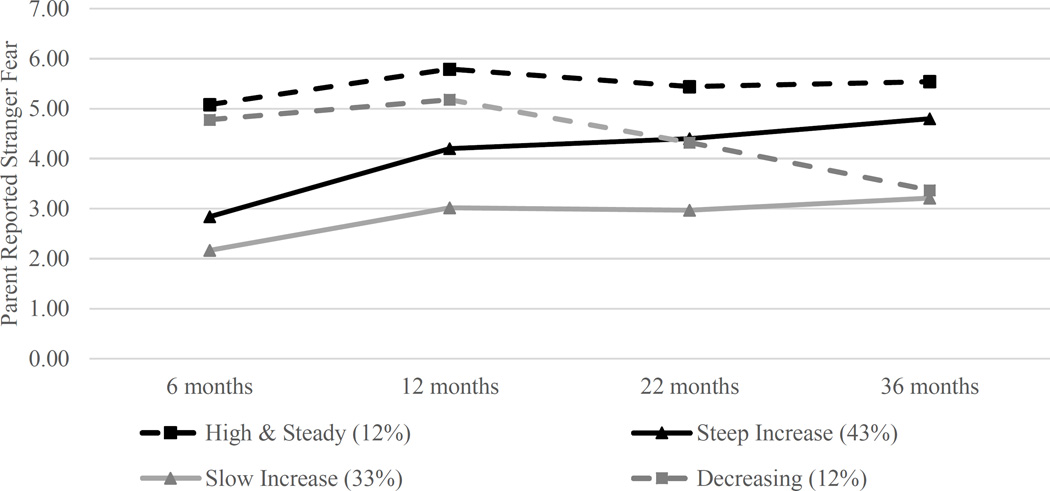
Recently, we demonstrated substantial heterogeneity in the development of stranger fear across infancy and toddlerhood. Using latent class analysis, we identified four different trajectories of developing stranger fear: a profile of infants who showed the expected slow, steady increases in stranger fear between 6 and 36 months of age; a second profile of infants whose levels of stranger fear also showed the expected increase but at steeper rate relative to the first profile; a third profile of infants who evinced high, steady levels of stranger fear over time; and a fourth profile of infants whose high levels of early stranger fear decreased across development (Brooker et al., 2013). Figure 1 [adapted from Brooker et al.’s (2013) Figure 1] shows these four profiles of stranger fear.
Figure 1.
Latent Profiles of Stranger Fear Development During Infancy
Note: Figure modified from Brooker et al., 2013, Developmental Science; Percentages indicate the proportion of individuals included in each class.
Consistent with prior research (Hirshfeld et al., 1992), we showed that infants who displayed high, steady levels of stranger fear over time also showed high levels of behavioral inhibition observed during a structured laboratory temperament assessment (Preschool Lab-TAB; Goldsmith, Reilly, Lemery, Longley, & Prescott, 1999) at age 36 months (Brooker et al., 2013). Behavioral inhibition is a robust risk factor for social anxiety across childhood and adolescence (Biederman et al., 2001; Chronis-Tuscano et al., 2009; Clauss & Blackford, 2012; Muris, Van Brakel, Arntz, & Schouten, 2011; Schwartz, Snidman, & Kagan, 1999). The slow-increase and steep-increase profiles in Brooker et al. (2013) both followed the presumptive normative pattern of increasing stranger fear from ages 6 to 36 months, but only the steep-increase profile showed elevated behavioral inhibition. Thus, while stable, high levels of stranger fear over time were verified as a risk for the development of anxiety problems, steeper than expected increases in stranger fear across infancy may reflect a second pathway that exacerbates risk for clinical conditions over time. We now extend our analyses with a longitudinal follow-up at age eight years, with a focus on the two largest profiles (steep increase and slow increase) that included 86% of the follow-up sample.
Although stranger fear is conceptually and empirically related to behavioral inhibition and fear more broadly, it is a distinct construct. Empirical evidence for relations between infant stranger fear and disorder-specific symptoms in childhood is lacking. Contributing to this lack of evidence are developmental fluctuations in prevalence rates for different anxiety symptoms (Beesdo et al., 2009). For example, extreme fearfulness in early childhood may be most readily apparent as acute distress in the presence of strangers or during separation from caregivers; this acute distress maps readily onto symptoms of separation anxiety disorder (American Psychiatric Association, 2013). Later in childhood, social evaluative fears become more common (Westenberg, Gullone, Bokhorst, Heyne, & King, 2007) so that by adolescence, extreme fearfulness may be more common in social contexts and overlap more fully with symptoms of social phobia. Indeed, separation and social anxiety constitute two separable, albeit moderately correlated, constructs as early as three to five years of age (Spence, Rapee, McDonald, & Ingram, 2001). In our view, a developmentally sensitive perspective allows that anxiety risk related to stranger fear might be associated chiefly with symptoms of separation anxiety in early childhood, with a potential shift to association with symptoms of social phobia over time. Therefore, we sought to identify the degree to which steep increases and slow increases in stranger fear during infancy are linked with specific anxious behaviors during middle childhood.
Stranger Fear Development and Putative Biological Markers of Anxiety Risk
Given the aforementioned heterogeneity in fear-related behaviors associated with early risk for anxiety problems, researchers have tried to isolate biological markers of risk for anxiety in young children. These markers typically signal disruptions in the regulation of biological systems in contexts that are likely to elicit anxious responses. One such biological system is the stress response of the hypothalamic-pituitary-adrenocortical (HPA) axis, which is discernable as early as 6 weeks of age (Larson, White, Cochran, Donzella, & Gunnar, 1998). HPA axis activity can be measured via its primary end product, cortisol, a glucocorticoid that increases available energy for action and plays a role in the maintenance of homeostasis by modulating activity in other stress-sensitive systems (see Gunnar, 1992, for a full review of the physiological and affective effects of cortisol).
In addition to fluctuations associated with specific stressors, cortisol follows a predictable diurnal cycle. Frequent pulses of cortisol release in the morning become less frequent over the course of the day, producing peaks in basal cortisol levels near morning wake times and nadirs near bedtime. These basal levels are not entirely independent from the experience of stressors, as chronic stress early in life can produce disruptions in the diurnal rhythm of cortisol such that cortisol levels increase (Vermeer & van IJzendoorn, 2006) or flatten across the day (Gunnar & Quevedo, 2007).
While blunted cortisol rhythm and high afternoon cortisol levels are associated broadly with psychopathology comorbidity and general mental health symptom severity (Essex, Klein, Cho, & Kalin, 2002; Shirtcliff & Essex, 2008), these cortisol measures are also linked specifically to anxiety problems and social wariness (Greaves-Lord et al., 2007; Smider, Essex, Kalin, Buss, Klein, Davidson, & Goldsmith, 2002; Van den Bergh, Van Calster, Pinna Puissant, & Van Huffel, 2008). Additionally, the negative impact of stress experienced in early infancy on observed overanxious behaviors during middle childhood is mediated through a flatter slope of diurnal cortisol (Brooker, Davidson, & Goldsmith, 2016). Thus, heightened HPA axis activity may exacerbate early individual differences in fear and precede subsequent maladaptive anxious behaviors (Rosen & Schulkin, 1998; Schulkin, McEwen, & Gold, 1994).
The Role of Gender in Anxiety Risk
Findings regarding gender differences in fear and anxiety are not uniform. In one meta-analysis examining temperament, girls displayed a modestly but significantly higher level of fear than did boys (Else-Quest, Hyde, Goldsmith, & Van Hulle, 2006). Most relevant to our study, Gartsein and colleagues (2010) found that, relative to males, female infants showed steeper increases in mother-reported, but not observed, fear across infancy. Similarly, an examination of teacher-reported trajectories of fearfulness across the elementary school years demonstrated that more females than males were placed in the “high fear” trajectory (Côté, Tremblay, Nagagin, Zoccolillo, & Vitaro, 2002). In our own work (Brooker et al., 2013), females were more likely than males to be in the high/steady fear trajectory and less likely to be in the slow-increase trajectory.
Although the mean age of onset for anxiety disorders does not differ between males and females, girls develop anxiety disorders more quickly (Lewinsohn, Gotlib, Lewinsohn, Seeley, & Allen, 1998). Evidence for gender differences in anxiety disorders during the preschool years is lacking (Spence et al., 2001), but in at least one study, twice as many girls qualified for a diagnosis of an anxiety disorder by age six years (Lewinsohn et al., 1998). This gender difference persists into adolescence and adulthood (Lewinsohn, Zinbarg, Seeley, Lewinsohn, & Sack, 1997; Mclean, Asnaani, Litz, & Hofman, 2011; Poulton, Milne, Craske, & Menzie, 2001). Results regarding gender differences in the prevalence of specific anxiety diagnoses are mixed, with some findings supporting a greater preponderance of females in cases of both separation and social anxiety and other studies failing to find such an association (reviewed in Albano, Chorpita, & Barlow, 2003). One large longitudinal study reported no significant sex differences in the prevalence rates of either separation or social anxiety during mid- to late childhood (Copeland, Angold, Shanahan, & Costello, 2014).
Hypotheses
Although we have previously demonstrated important individual differences in stranger fear development (Brooker et al., 2013), two seemingly prototypical trajectories of stranger fear during infancy may evince differential associations with early anxiety-relevant behavioral (anxious behaviors and anxiety diagnoses) and biological (diurnal cortisol) measures. Differences in infant stranger fear trajectories were tested in association with behavioral and biological measures of anxiety risk obtained five years after the final infant assessment. The longitudinal study design provides a robust test of associations between two infant trajectories of stranger fear development and emerging risk for the development of anxiety problems.
We expected that steep increases in stranger fear during infancy would be associated with increased risk for anxiety problems over time as indexed by both behavioral and biological measures, and we anticipated that this risk would be greatest for symptoms of separation anxiety disorder, based on the age of the children being studied. In addition, we hypothesized that infants who showed steeper increases in stranger fear would show more dysregulated childhood cortisol responses manifested as flattened diurnal slopes (Gunnar et al., 1992; Shirtcliff & Ruttle, 2010).
Methods
Participants
The sample was drawn from a longitudinal twin study examining genetic and environmental influences on emotional development between 6 and 36 months of age (Schmidt et al., 2013). Participants for the infant/toddler study were recruited from the greater Madison, Wisconsin, area via the following methods and sources: state birth records, recruiting at Mothers of Multiples clubs, television publicity, birth announcements in newspapers and materials left at doctors’ offices. Ongoing recruitment procedures allowed families to enter the study at any time prior to children reaching 36 months of age. Our sample included a subset of children classified as one of the four stranger fear profiles during infancy who also participated in a separate study (Schmidt et al., 2013) at age eight years (N = 129; 54.3% female). Of the 129 children who participated in both studies, 51 (40%) children scored at or above 1.5 standard deviation above the mean on at least one of eight parent-reported symptom scales of the Health and Behavior Questionnaire (Armstrong, Goldstein, & The MacArthur Working Group on Outcome Assessment, 2003). Fourteen of these children were elevated on pure internalizing symptoms, fifteen children were elevated on externalizing symptoms (CD/ODD) and ADHD, thirteen children were elevated on externalizing symptoms only, and nine children were elevated on ADHD only. The remaining participants were part of a low-symptom group who scored below the mean on all symptom scales (n=40) or were co-twins of a high-scoring child or a low-symptom child (n=38).
Demographic information from the follow-up assessment are provided in Table 1. Consistent with the demographics of the recruitment area, 95% of mothers and 92.5% of fathers self-reported as Caucasian. Mothers and fathers most frequently reported a college degree as their highest level of education (45.0% and 40.4% respectively). Median family income was in the $70,000 to $80,000 range. Ninety-five percent of children lived with both biological parents at the time of initial participation, and 90% of children lived with both biological parents at the follow-up assessment.
Table 1.
Family demographics at the age eight years.
| Age | Mean | (SD) | Min | Max |
|---|---|---|---|---|
| Maternal | 39.1 | 4.4 | 30 | 50 |
| Paternal | 41.9 | 5.4 | 34 | 61 |
| Child (in years) | 8.0 | 0.5 | 7 | 11 |
| Parent Education | Maternal % | Paternal % | ||
| High School diploma | 5.8 | 15.4 | ||
| Some college | 14.4 | 23.0 | ||
| College degree | 45 | 40.4 | ||
| Some post-college training | 18.3 | 7.7 | ||
| Post-college degree | 16.3 | 13.5 | ||
| Family Income Level | % | |||
| <$50,000 | 11.2 | |||
| $50,000-$60,000 | 12.2 | |||
| $60,000-$70,000 | 16.3 | |||
| $70,000-$80,000 | 6.1 | |||
| $80,000-$90,000 | 10.2 | |||
| $90,000-$100,000 | 11.2 | |||
| $100,000-$150,000 | 21.4 | |||
| >$150,000 | 11.2 | |||
Procedure
Parents completed questionnaire-based assessments that included items about stranger fear when children were 6, 12, 22, and 36 months of age. When children were eight years old, families participated in an in-depth study that included parent interviews and questionnaires, and an in-home observational child assessment (Schmidt et al., 2013). Samples of diurnal cortisol were collected by parents for three days (3 samples per day) prior to the home visit and frozen until transported back to the laboratory for storage and later assay.
Measures
Profiles of stranger fear during infancy
Details on stranger fear profile formation can be found in Brooker et al. (2013). Briefly, mothers and fathers completed age-appropriate temperament questionnaires for each infant during the 6-, 12-, 22-, and 36-month assessments (the Infant Behavior Questionnaire, Rothbart, 1981; the Toddler Behavior Assessment Questionnaire, Goldsmith, 1996, and the Children’s Behavior Questionnaire, Rothbart, Ahadi, Hershey, & Fisher, 2001; respectively).
We constructed a stranger fear scale for each questionnaire by selecting items that asked about infants’ interactions with unfamiliar people. Relevant items from each questionnaire were analyzed via principal components; items with low component loadings were removed. In addition, items with low item-total correlations were removed. We averaged remaining items to create a scale score for stranger fear. A complete list of items composing scales of stranger fear is provided by Brooker et al. (2013). To reduce reporter bias, scores of stranger fear obtained from maternal and paternal reports were mean composited to produce a single score for stranger fear at each age.
Stranger fear scores were then entered into a latent class growth analysis (Muthén & Muthén, 2006) to identify latent profiles of individuals whose trajectories of stranger fear development from 6 to 36 months of age differed from the overall group (Jung & Wickrama, 2008; Muthén, 2004). As previously reported (Brooker et al., 2013), a 4-class solution provided the best fit to the data. The two least common classes showed consistently elevated levels of stranger fear (High/Steady; 10%) or an unusual pattern of decreasing levels of stranger fear (Decreasing; 5%). We would expect these two classes to predict later anxious behaviors; however, we were constrained by the limited number of children in these classes for whom longitudinal data were available (n = 12 for High/Steady and n = 10 for Decreasing). The two most common classes identified in infancy both showed low levels of stranger fear at 6 months and increases in stranger fear over time. These two classes were differentiated by their rates of increase, with one group showing steeper (Steep Increase; 43%) and the other showing slower (Slow Increase; 33%) increases in stranger fear. We focused analyses on individuals with Steep Increase (n = 57) and Slow Increase profiles (n = 50) for whom parent-reported behaviors were available at age eight years.
Anxious behaviors
Mothers and fathers reported on children’s anxiety-relevant behaviors at age 8 using the MacArthur Health and Behavior Questionnaire (HBQ; Armstrong & Goldstein, 2003). The HBQ requires respondents to rate, using a three-point scale (0 = rarely, 2 = certainly applies), the degree to which different behaviors are characteristic of their child in the past six months. Given our hypotheses, analyses focused on the scales of separation anxiety symptoms and inhibition. Mother and father reports were moderately correlated for both separation anxiety ratings (r = 0.34, p < 0.01) and inhibition ratings (r = 0.34, p < 0.01) and results did not differ when examining mother- and father-reported behaviors separately, so parent ratings were mean composited to reduce possible rater bias.
Primary caregivers also reported on clinically-relevant child mental health symptoms at child age eight years using the Diagnostic Interview Schedule for Children, Version IV (DISC-IV; Shaffer, Fisher, Lucas, Dulcan & Schwab-Stone, 2000). Interviews were administered orally over the telephone by trained research assistants, who asked parents to rate whether symptoms were or were not characteristic of their child. Primary caregiver responses were then used to create symptom counts for each clinical condition and to identify children who met diagnostic thresholds consistent with Diagnostic and Statistical Manual of Mental Disorder criteria (DSM-IV-TR; American Psychiatric Institute, 2000) for individual conditions. Given our hypotheses, analyses were focused on both past year diagnoses and symptoms of separation anxiety disorder and social phobia. Eleven children displayed a sufficient number of symptoms to qualify for a diagnosis of either separation anxiety disorder or social phobia. Primary caregivers endorsed on average 1.5 (SD = 2.7) symptoms of separation anxiety disorder and 1.4 (SD = 2.8) symptoms of social phobia. DISC symptom counts were analyzed using a Poisson distribution.
Salivary cortisol
As part of the middle childhood study, parents were mailed prelabeled Salivette collection tubes (Starstedt) and instructions. Parents were asked to collect saliva 30 minutes after waking, in the late afternoon, and 30 minutes prior to bedtime on three consecutive days prior to the home visit. Ninety-five percent of morning samples were collected between 6:30 AM and 9:45 AM, 95% of afternoon samples were collected between 2:00 PM and 6:00 PM, and 95% of evening samples were collected between 7:30 PM and 10:00 PM. Families were instructed not to eat or drink one hour prior to saliva collection and to store samples in the freezer immediately after collection. Parents recorded the date and time of collection in addition to waking time, nap schedule (if applicable), medication use, primary activity during a half hour prior to saliva collection, and general health for each twin on each collection day.
The research team transported all saliva samples back to the laboratory on ice. Samples were then stored at −80°C until assayed. Saliva samples were thawed, then centrifuged at 5000 rpm for 10 minutes to remove impurities. Cortisol was assessed in duplicate with a salivary enzymeimmunoassay kit (Salimetrics, State College, PA). Two non-blind internal controls were included in each assay. For the low control, the average value was 0.082 µg/dL with inter-and intra-assay Coefficient of Variations (CVs) of 7.2% and 6.1%, respectively. For the high control, the average value was 0.84 µg/dL with inter- and intra-assay CVs of 8.1% and 5.3% respectively. Results were considered acceptable if the CV of the duplicate samples was < 20%. Repeat assays were performed on any samples not meeting this requirement. Families were assayed across one or two batches. Outlying samples were windsorized to a value two standard deviations above the mean. Raw cortisol values averaged across the three sample collection days are: morning M = .42 µg/dL (SD = .22), afternoon M = .14 µg/dL (SD = .10), evening M = .10 µg/dL (SD = .12). We showed in a previous study that medication use did not predict cortisol levels (Van Hulle, Shirtcliff, Lemery-Chalfant, and Goldsmith, 2012); therefore, we did not control for medication use in this study. Activity level was not related to cortisol level after correcting for multiple testing, nor was activity level related to gender, stranger fear profile, or the interaction between them; thus, we did not control for activity level in subsequent analyses.
We converted all sample collection times into time-since-waking. Hierarchical linear modeling (HLM) was then used to extract Empirical Bayes estimates of basal cortisol levels and diurnal rhythm scores. HLM offers several advantages. First, HLM captures the inherent dependency of repeated samples collected on the same participant. Empirical Bayes estimates extracted only the stable, correlated cortisol component separate from uncorrelated moment-to-moment or day-to-day cortisol fluctuations (Shirtcliff, Granger, Booth, & Johnson, 2005). Second, HLM does not require complete data, but rather uses all the samples provided to calculate basal cortisol and diurnal rhythm scores. Third, HLM allows for time-varying predictors of cortisol levels (e.g. time-since-waking), thereby permitting individualized estimation of HPA functioning at the specific collection times for each individual and for each sample rather than necessitating that all samples be collected at equivalent intervals. This advantage is important for estimations of the diurnal slope when several hours pass between sample collections.
Empirical Bayes scores were extracted from a three-level HLM model centered on 7 hours post- awakening (i.e., in the afternoon). Level 1 and Level 2 modeled within-person (within day and day-to-day) variation in cortisol measures. Level 3 measured the between-person variation in level and slope. Centering on the afternoon enabled us to simultaneously predict afternoon cortisol level and two separate slopes—morning-to-afternoon slope and afternoon-to-evening slope—for each individual. Detailed information on the formation of the basal cortisol composites is provided by Van Hulle et al. (2012). To determine whether anxiety was related to overall cortisol level, change in diurnal slope, or both, we analyzed each of these components separately.
Socioeconomic status
Given previous evidence for associations between socioeconomic status (SES) and mental health, SES was also included in the analyses. We created a mean composite of SES from standardized parent education (mother and father) and family’s gross annual income at the follow-up occasion.
Plan for analysis
We first examined descriptive statistics and raw associations among the variables. Following this, we tested profile-based differences in the presence of anxiety symptoms at age 8. These analyses included both an exploratory examination of associations between profiles of stranger fear and the presence of diagnoses at age eight years and also tests of profile-based differences in symptoms of separation anxiety and social phobia/inhibition. Finally, we tested for profile-based differences in diurnal cortisol. We used generalized estimating equations (GEE) to control for clustering within families.
Missing data
A test of patterns of missing data including all variables suggested that data were missing completely at random (Little’s MCAR χ2 = 50.55, p > 0.10). Missing data were imputed using SAS PROC MI (SAS Institute Inc., 2011). The maximum proportion of missing values for any single variable was 8.2%. Data were imputed using a fully conditional Markov Chain Monte Carlo imputation model (n imputations = 100). Sex, race, and child age were included in the imputation model along with family SES as auxiliary variables (Enders, 2010). Analyses presented below reflect the pooled parameter estimates from all imputed data sets.
Results
Descriptive Statistics and First-order Associations
Descriptive statistics for all primary variables are shown in Table 2 by stranger profile. We present behavioral and biological measures for all four stranger fear profiles; however, we lacked power to test group effects for the high/steady and decreasing fear profiles due to low samples size. Correlations among the primary variables are shown in Table 3. Separation and social inhibition were correlated within and across parent-reported measures. However, anxiety measures were mostly unassociated with basal cortisol measures. DISC separation anxiety symptoms alone was significantly, positively correlated with afternoon-evening cortisol slope. Consistent with the literature, GEE models suggested sex differences in parent-reported symptoms of social phobia and inhibition. As is frequently observed, parents reported significantly more inhibited behaviors for girls than boys on the HBQ (MFemale = 0.68, SD = 0.30 and MMale = 0.43, SD = 0.33; d = 0.79) and significantly more social phobia symptoms on the DISC interview (M Female = 1.9 SD = 3.3 and MMale = 0.81, SD = 1.9.; d = .40). Sex was also significantly related to profile membership (χ2[1] =10.0, p = 0.002), with girls comprising a larger proportion of the steep increase profile (67%) and boys comprising a larger proportion of the slow increase profile (62%). We examined participant sex as a moderator of the relationship between stranger fear profiles and the outcomes of interest.
Table 2.
Descriptive statistics and tests of sex differences for primary variables by Stranger Fear Profile
| MHS (SD) | MST (SD) | MSL (SD) | MD (SD) | |
|---|---|---|---|---|
| Family SES | 0.09 (.68) | 0.09 (.82) | 0.23 (.62) | −0.11 (.63) |
| HBQ Separation Anxiety | 0.39 (.27) | 0.31 (.29) | 0.24 (.25) | 0.22 (.17) |
| HBQ Social Inhibition | 0.99 (.42) | 0.60 (.33) | 0.52 (.35) | 0.60 (.48) |
| DISC Separation Anxiety | 1.60 (2.3) | 2.05 (2.7) | 0.93 (1.5) | 0.60 (0.5) |
| DISC Social Phobia | 2.40 (2.4) | 1.84 (3.0) | 0.92 (2.4) | 0.20 (.42) |
| Home cortisol Afternoon Levela | 3.08 (.20) | 3.07 (.24) | 3.06 (.24) | 2.90 (.26) |
| Home cortisol Morning-Afternoon slopea | −0.13 (.01) | −0.13 (.01) | −0.12 (.02) | −0.12 (.02) |
| Home cortisol Afternoon-Evening slopea | −0.11 (.04) | −0.09 (.04) | −0.10 (.04) | −0.08 (.08) |
Note. HS = High & Steady (n = 12), ST = Steep Increase (n = 57), SL = Slow Increase (n = 50), D = Decrease (n = 10).
Due to missing data sample sizes dropped by n=5 participants for the High & Steady and Decrease groups, and by n=10 for the Steep Increase and Slow Increase groups.
Table 3.
Bivariate associations among primary variables, other than Stranger Fear Profiles
| 1. | 2. | 3. | 4. | 5. | |
|---|---|---|---|---|---|
| 1. Family SES | |||||
| 2. HBQ Separation Anxiety | −.05 | ||||
| 3. HBQ Social Inhibition | −.05 | .35** | |||
| 4. DISC Separation Anxiety | −.18* | .67** | .10 | ||
| 5. DISC Social Phobia | −.03 | .32** | .24** | .35** | |
| 6. Cortisol (afternoon level) | −.04 | −.05 | −.01 | .01 | .14 |
| 7. Cortisol (morning-afternoon slope | −.01 | .04 | −.08 | .10 | .12 |
| 8. Cortisol (afternoon-evening slope) | −.16 | .08 | −.18† | .26** | .07 |
Note: n = 129,
p < 0.01,
p < 0.05,
p < 0.10;
SES = socioeconomic status; HBQ = Health & Behavior Questionnaire; DISC = Diagnostic Interview Schedule for Children; Cortisol measures derived from slopes-as-outcome HLM model.
Profile-Related Differences in Parent-Reported Anxious Behaviors
First, using the generalized estimating equations approach, we tested associations between stranger fear profiles and parent-reported anxious behaviors. Given the well-known association between SES and anxiety symptoms and significant sex differences in both parent-reported symptoms and profile status, SES and sex were included in tests of group differences. The profiles did not differ in parent-reported HBQ separation anxiety (estimate (EST) = .04, t = 0.69, p = .48) or inhibition (EST = .004, t = .07, p = .94). Profile group differences were observed, however, for parent-reported DISC separation anxiety symptoms (EST = .63, t = 3.42, p < .001) and social phobia symptoms (EST = .46, t = 2.1, p = .04). Children in the steep increase group showed more separation anxiety behaviors (M = 2.1, SD = 2.7) than did children in the slow increase group (M = 0.94, SD = 1.5, d = 0.53). Children in the steep increase group also scored higher than children in the slow increase group on symptoms of social phobia (M = 1.8, SD = 3.0 vs. M = 0.92, SD = 1.8, d = .32), although the magnitude of this effect was smaller than that for separation anxiety. Stranger fear profile and child sex did not interact in predicting anxious behaviors or symptoms.
To determine if the shape of stranger fear behaviors across infancy and toddlerhood added information beyond toddler stranger fear levels alone, we conducted post-hoc analyses specifically focusing only on stranger fear measured at age 36 months. For these analyses we included individuals in the high/steady and decreasing fear groups. The 36-month stranger fear score predicted DISC separation anxiety symptoms (EST = .29, t = 3.2, p = .002), but not social phobia symptoms (EST = .18, t = 1.6, p = .13). Thus, the shape of infant fear appears to be more predictive of social phobia than the most recent stranger fear assessment alone.
Consistent with prevalence rates in the population (American Psychiatric Association, 2013), four children met diagnostic criteria for social phobia. These children were evenly split between the slow increase and steep increase stranger fear profiles. Eight children met diagnostic criteria for Separation Anxiety disorder. One of the eight children was in the high/steady profile, one was in the slow increase profile, and the other six children (75%) followed trajectories of steep increases in stranger fear between 6 and 36 months of age.
Profile-related Differences in Later Cortisol Measures
Our final set of analyses used a series of GEEs to test for a neuroendocrine correlate of anxiety problems indexed by afternoon cortisol level and diurnal cortisol slope. As with previous analyses, child’s sex and family SES were included in the model.
We observed no main effects of stranger fear profile on afternoon cortisol level (EST = .02, t = .27, p = .78) or slope across the day (EST = .004, t = .1.5, p = .13 for morning-afternoon slope and EST = .004, t = .49, p = .61 for afternoon-evening slope).
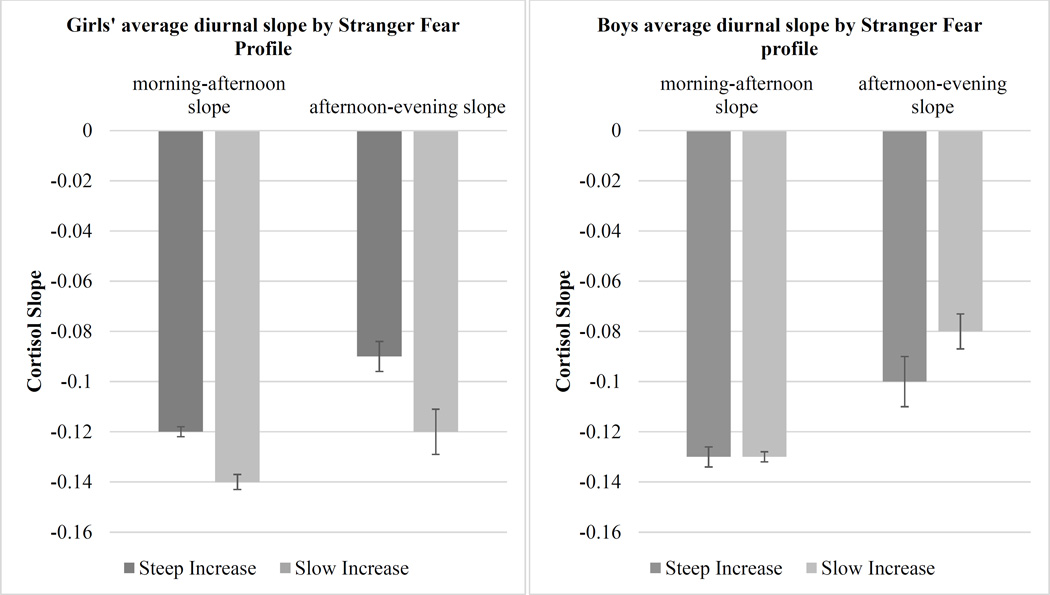
The anticipated profile differences in the slope of diurnal cortisol were moderated by sex of child. The interaction between sex and profile did not predict afternoon cortisol level (t = .11, p = .90). However, child sex interacted with both morning-afternoon slope (t = 2.7, p=.02) and afternoon-evening slope (t = 2.5, p=.01). Figure 3 shows the stranger fear profile difference in morning-afternoon and afternoon-evening slopes by sex. For boys, cortisol declined across the day as expected and this pattern did not differ between profiles (t = .81, p = .42 for morning-afternoon slope and t = 1.5, p = .14 for afternoon-evening slope). For girls, significant changes in cortisol levels across the day were modulated by profile membership (t = −2.9, p = .01 for morning-afternoon slope and t = −2.2, p = .02 for afternoon-evening slope). Specifically, female infants who showed steep increases in stranger fear later showed flatter cortisol levels across the day.
Because concurrent DISC Separation Anxiety symptoms were correlated with afternoon-evening cortisol slope (r = .26, p <.001), we repeated these analyses including separation anxiety symptoms as a covariate to ensure that profile-based differences in cortisol were not sure solely to the presence of concurrent anxiety symptoms. The pattern of results held when concurrent separation anxiety symptoms were added to the model.
Finally, as we did when the outcome was parent-reported anxiety, we conducted post-hoc analyses with age 36 month stranger fear instead of the stranger fear profiles as the predictor. We did not find a main effect for 36-month stranger fear on middle childhood cortisol levels and slope, nor did we find an interaction with child sex. Both of these analyses support the centrality of the pattern of infant stranger fear development in the analyses.
Discussion
Summary of key findings
Two relatively common trajectories of stranger fear development across infancy were differentially related to risk for anxiety symptoms during middle childhood. Children with steeper increases in stranger fear between 6 and 36 months showed more anxious symptoms relative to children for whom stranger fear increased more gradually across infancy. This finding held for more overt clinical symptoms of separation anxiety and social phobia captured by the DISC interview, but not the dimensional perspective captured by the HBQ. For girls, infant trajectories of stranger fear were also uniquely related to daily cortisol patterns later in childhood; girls who showed steep increases in stranger fear during infancy had flatter slopes of diurnal cortisol at 8 years of age.
Integration of detailed findings with the literature
We and others (e.g., Chronis-Tuscano et al., 2009; Essex et al., 2002; Hirshfeld et al., 1992) have suggested that chronically high levels of fear constitute a facet of risk for the development of anxiety problems. Although very early identification may be plausible for children who show extreme stranger fear during infancy (i.e., those in the high/steady profile), identifying at-risk individuals only during the first year of life would fail to detect those children whose stranger fear is not atypical until the toddler years (i.e., those in the steep increase group). Both groups begin to exhibit inhibited behaviors as early as age two to three years (Brooker et al., 2013; Gartstein et al., 2010). And, as we demonstrate here, children in the steep increase group also experience more separation and social anxiety during middle childhood. Thus, the findings are consistent with notions of multiple pathways to disorder (Cichetti & Rogosch, 1996).
Our hypothesis that infant fear would be more closely related to separation anxiety than social phobia was partially supported. Although group differences were not apparent in HBQ symptoms, children in the stranger fear steep increase profile showed more clinical symptoms of separation anxiety and qualitatively more frequent DISC diagnoses of separation anxiety relative to children who showed slow increases in stranger fear across infancy. Likewise, children in the steep increase group had more DISC symptoms of social phobia than children in the slow increase group.
These results must be qualified by one important caveat. Given the significant correlation between parent-reported HBQ separation anxiety behaviors and DISC separation anxiety symptoms, it is unclear why profile differences emerged only for the DISC symptoms. The most likely explanation is that the overt clinical orientation of the DISC identifies more severe or impairing anxious behaviors than does the HBQ, with its more dimensional perspective. Similarly, only DISC-reported separation anxiety symptoms were correlated with diurnal cortisol slope, additionally suggesting these DISC symptoms might represent more critical anxious behaviors.
The notion that children following steeply increasing trajectories of stranger fear between 6 and 36 months of age were at greater risk for later anxiety problems than were children who followed slowly increasing trajectories was corroborated, in part, by analyses of diurnal cortisol levels and slopes. Girls with steeply increasing stranger fear across infancy showed smaller declines in diurnal cortisol across the day four years later than did girls with slowly increasing infant fear.
As discussed by Klein and colleagues (2012), this overlap between biological and behavioral indicators of early risk supports the presence of more than one etiological pathway toward anxiety problems. Early fearfulness may lead to a dysregulated stress response system. Alternatively, dysregulated psychophysiology may, itself, reflect a predisposition toward the development of anxiety disorders. Indeed, we found differences in diurnal cortisol slope between the two fear profiles after statistically accounting for concurrent symptoms of separation anxiety. These alternatives cannot be disentangled with our data, as we could not control for early diurnal cortisol. Nevertheless, we identified risk factors in children who might previously have been considered to be at low risk for the development of anxiety problems.
Our neuroendocrine results were confined to change in diurnal cortisol across the day. Early experiences may lead to the reorganization of baseline biological processes that may be immediately adaptive, but that become maladaptive as contexts change across development (Gunnar & Quevedo, 2007; Shirtcliff & Ruttle, 2010). From this perspective, dysregulated patterns of diurnal cortisol may be a product of allostatic load, or the wear and tear of constant efforts to adapt, built up as a result of consistent and long-standing over-reactive fear responses in young children. This possibility is supported in part by our post-hoc analyses wherein 36-month stranger fear alone did not predict diurnal cortisol.
Our findings regarding the relationship between diurnal cortisol and concurrent anxious behaviors were mixed, as only afternoon-evening cortisol slope was significantly correlated with concurrent anxiety, and this result was specific to DISC Separation Anxiety. We also note that atypical diurnal cortisol patterns are associated with a wide variety of negative outcomes across development, including internalizing problems during the preschool years (Saridjan, Velders, Jaddoe, Hofman, Verhulst, & Tiemeier, 2014), an increase in conduct problems and aggressive behavior across middle childhood (Salis, Bernardm Black, Dougherty, & Klein, 2016), and adolescent alcohol use (Ruttle, Maslowsky, Armstrong, Burk, & Essex, 2015). Thus, it remains unclear to what extent our results are specific to anxiety or may generalize to a broader range of mental health symptoms, as in Shirtcliff & Essex (2008), for example.
Our results of profile-based differences in diurnal cortisol only for eight-year-old girls are consistent with previous work demonstrating that adolescent girls with higher levels of internalizing behaviors do not show the typical pattern of decreasing cortisol levels across the day (Klimes-Dougan, Hastings, Granger, Usher, & Zahn-Waxler, 2001). However, some other research in younger samples has failed to find gender differences in the relationship between flat diurnal cortisol slope and internalizing problems (Saridjan et al., 2014).
Temperament-based theories of early risk for anxiety problems suggest that the biological and behavioral contributions to early anxiety risk may be different for boys and girls (Kagen, 1994). This problem may be compounded by the fact that girls show higher prevalence rates for anxiety problems overall (Altemus, Sarvaiya, and Epperson, 2014; Mash & Barkley, 2003). For example, girls may be more physiologically aroused (i.e. elevated heart rate) than boys under conditions of interpersonal distress (Zahn-Waxler, Klimes-Dougain & Slattery, 2000). Kagan (1994) described how high heart rates appear to distinguish between levels of behavioral reactivity (low vs. high) more accurately for girls, while low heart rates were better predictors of behavior for boys. Thus, an alternative psychophysiological index may provide insight into boys’ risk status. Although our results do suggest the utility of diurnal cortisol as a marker of risk for anxiety differences for girls, our study does not explain how these sex differences evolve over time as the brain develops and children interact with their social world.
A variety of potential factors may mediate the relationship between early stranger fear and later anxiety and cortisol rhythms. For example, bidirectional relationships between parent behaviors and offspring fear/anxiety are likely (see Dadds & Roth, 2001, for one model). Fearful children may elicit protective or intrusive parenting in novel environments, which then serves to reinforce withdrawal tendencies and internalizing behaviors (Bayer, Sampson, & Hemphill, 2006; Kiel & Buss, 2011). Children with more rapid increases in fear during infancy tend to have mothers who are less sensitive (Braungart-Rieker, Hill-Soderlund, & Karrass, 2010) and who experience more anxiety-specific negative affect (Brooker et al., 2013). Parenting practices are also associated with altered psychophysiology; mothers whose parenting is characterized by low involvement and warmth, for instance, tend to have children with flat diurnal cortisol patterns (Pendry & Adam, 2007).
Cognitive-based emotion regulation strategies also represent a possible mediating factor. For example, an attentional bias toward threat moderates the relationship between early fear and social withdrawal in childhood and adolescence (Pérez-Edgar, Bar-Haim, McDermott, Chronis-Tuscano, Pine, & Fox, 2010; Pérez-Edgar, Reeb-Sutherland, McDermott, White, Henderson, & Fox, 2011). Relatedly, preschool children with chronically elevated cortisol score lower on measures of attentional and inhibitory control (Gunnar, Tout, de Haan, Pierce, & Stansbury, 1997). Moreover, weak emotion regulation is associated with HPA axis dysfunction in children (Scher, Hall, Zaidman-Zait, & Weinberg, 2010).
We may speculate that experiencing fear in situations that occur often in young childhood (meeting new adults) may itself constitute a stressor for some children (Gilissen, Koolstra, van IJzendoorn, Bakermans-Kranenburg, & van der Veer, 2007). Chronic exposure to such ordinary and necessary fear-eliciting stimuli early in life, when accompanied by over-protective parenting, high levels of parental negative affect, and limited opportunities to learn adaptive coping strategies, may lead to poor emotion regulation, increased anxiety, and disrupted HPA axis functioning. The role of these possible mediating factors in the context of our findings remains speculative. However, when viewed in conjunction with our results, these potential mediators do suggest potential intervention points for preventing and managing children’s anxious tendencies.
Limitations
Potential limitations include the overall sample size, which was fairly small, although we had adequate power (99%) to detect expected moderate to large main effects. The small sample size is of more concern when interpreting the results regarding gender because we have less power to examine statistical interactions. An additional limitation is the inability to examine outcomes associated with the two less frequent stranger fear profiles (i.e., the high/steady and decreasing profiles) given the limited number of children in these groups for whom follow-up data were available. Thus, we do not know the extent to which these other atypical stranger fear profiles may be associated with risk for later mental health symptoms or dysregulated psychophysiology.
Although the group of individuals selected for follow-up was mildly enriched for psychopathology prior to the middle childhood assessments, our sample included only the small number of diagnoses that would be expected in a largely community sample at age eight years. While unsurprising, the small number of cases does limit our ability to examine the relationship between early stranger fear and specific diagnoses.
Both the stranger fear profiles and later anxious behaviors were based on mother and father reports, which have both strengths and weaknesses. Although using both mother and father reports helps to decrease bias (Stanger & Lewis, 1993), our results may pertain as much to parent perceptions of their child as to the child’s actual behavior. However, these concerns are mitigated somewhat by our previous work showing that observational measures of behavioral inhibition varied by stranger fear profile (Brooker et al., 2013). Our results also converge with those of Gartstein and colleagues (2010), who found that steep increases in early mother-reported and observed fear predicted anxious behaviors during the toddler years. Thus, our results add to a growing body of evidence that early atypical fear is a potent risk factor for later anxiety problems.
Conclusions
Despite limitations, our results support theoretical and empirical work suggesting multiple developmental trajectories that place infants at risk for future anxiety problems. Here, profiles of stranger fear assessed when infants were between 6 and 36 months of age predicted neuroendocrine markers of anxiety risk and anxiety symptoms during childhood. Infants who showed steep increases in the trajectory of fear during infancy had more anxiety symptoms, and possibly more diagnoses, at age eight years than infants whose fearfulness increased more slowly across infancy.
Figure 2.
Diurnal Cortisol Slopes for Girls (left panel) and Boys (right panel) by Stranger Fear Profile.
Note: Slopes are negative because basal cortisol levels decline across the day.
Table 4.
Results from fitting generalized linear model (controlling for clustering within families) to anxiety at age 8 years.
| Separation Anxiety (DISC) |
Separation Anxiety (HBQ) |
Social Phobia (DISC) |
Social Inhibition (HBQ) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EST | t | p | EST | t | p | EST | t | p | EST | t | p | |
| Intercept | .60 | 4.0 | .0001 | .25 | 4.9 | <.001 | .10 | 0.5 | .59 | .43 | 7.2 | <.001 |
| Sex | .16 | 1.0 | .35 | .10 | 1.8 | .06 | .72 | 3.6 | .001 | .27 | 4.1 | <.001 |
| SES | −.29 | −2.8 | .007 | −.01 | −0.3 | .77 | −.10 | −0.9 | .39 | −.07 | −1.6 | .10 |
| Stranger Profile | .63 | 3.4 | .001 | −.04 | −0.7 | .49 | .46 | 2.1 | .04 | .01 | 0.2 | .88 |
Note: Model results are combined across n=50 multiply imputed data sets; significant predictors are shown in bold.
Table 5.
Results from fitting generalized linear models (controlling for clustering within families) to cortisol measured at age 8 years.
| Level | Morning-Afternoon Slope |
Afternoon-Evening Slope |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| EST | t | p | EST | t | p | EST | t | p | |
| Intercept | 3.1 | 45.9 | <.001 | −.13 | −37.3 | <.001 | −.10 | −.98 | <.001 |
| Sex | −.03 | −0.4 | .67 | .01 | 1.6 | .12 | .01 | 1.1 | .27 |
| SES | −.02 | −0.6 | .54 | .00 | 0.1 | .95 | −.01 | −.16 | .11 |
| Stranger Profile | .07 | 0.9 | .36 | .003 | 0.8 | .45 | .02 | 1.6 | .11 |
| Stranger Profile * Sex | −.12 | 1.0 | .31 | .02 | 2.5 | .01 | .05 | 2.7 | .01 |
Note: Model results are combined across n=50 multiply imputed data sets; significant predictors are shown in bold.
Acknowledgments
Data collection was supported by R37 MH50560 (PI: Goldsmith) and R01 MH59785 (PIs: Goldsmith & Lemery-Chalfant) from the National Institute of Mental Health. The writing of this manuscript was partially supported by T32 MH018931 (Program Director, Davidson), K01 MH100240 (PI: Brooker), and P50 MH100031 (Center Director, Davidson) from the National Institute of Mental Health. Infrastructure support was provided by the Waisman Center via P30 HD03352 from the National Institute of Child Health and Human Development. We thank the families who participated in this study and the staff members who helped with the recruitment and data collection.
References
- Albano AM, Chorpita BF, Barlow DH. Childhood anxiety disorders. In: Mash EJ, Barkley RJ, editors. Child psychopathology. second. New York, NY: The Guildford Press; 2003. pp. 279–329. [Google Scholar]
- Altemus M, Sarvaiya N, Epperson CN. Sex differences in anxiety and depression clinical perspectives. Frontiers in neuroendocrinology. 2014;35(3):320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: Author; 2013. [Google Scholar]
- Andersson K, Bohlin G, Hagekull B. Early temperament and stranger wariness as predictors of social inhibition in 2-year-olds. British Journal of Developmental Psychology. 1999;17(3):421–434. http://doi.org/10.1348/026151099165375. [Google Scholar]
- Armstrong J, Goldstein LH. The MacArthur Working Group on Outcome Assessment: Manual for the MacArthur Health and Behavior Questionnaire (HBQ 1.0) Pittsburgh: University of Pittsburgh.: MacArthur Foundation Research Network on Psychopathology and Development; 2003. [Google Scholar]
- Bayer JK, Sanson AV, Hemphill SA. Parent influences on early childhood internalizing difficulties. Journal of Applied Developmental Psychology. 2006;27:542–559. [Google Scholar]
- Beesdo K, Bittner A, Pine DS, Stein MB, Hofler M, Lieb R, Wittchen H-U. Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Archives of General Psychiatry. 2007;64(8):903–912. doi: 10.1001/archpsyc.64.8.903. http://doi.org/10.1001/archpsyc.64.8.903. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics in North America. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell-Dolan DJ, Last CG, Strauss CC. Symptoms of anxiety disorders in normal children. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29(5):759–765. doi: 10.1097/00004583-199009000-00014. http://doi.org/10.1097/00004583-199009000-00014. [DOI] [PubMed] [Google Scholar]
- Biederman J, Hirshfeld-Becker DR, Rosenbaum JF, Herot C, Friedman D, Snidman N, … Faraone SV. Further evidence of association between behavioral inhibition and social anxiety in children. American Journal of Psychiatry. 2001;158(10):1673–1679. doi: 10.1176/appi.ajp.158.10.1673. http://doi.org/10.1176/appi.ajp.158.10.1673. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss. Vol. 2. New York: Basic; 1973. [Google Scholar]
- Bridges KMB. Emotional development in early infancy. Child Development. 1932;3:324–341. [Google Scholar]
- Brooker RJ, Buss KA, Lemery-Chalfant K, Aksan N, Davidson RJ, Goldsmith HH. The development of stranger fear in infancy and toddlerhood: normative development, individual differences, antecedents, and outcomes. Developmental Science. 2013;16(6):864–878. doi: 10.1111/desc.12058. http://doi.org/10.1111/desc.12058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooker RJ, Davidson RJ, Goldsmith HH. Maternal negative affect during infancy is linked to disrupted patterns of diurnal cortisol and alpha asymmetry across contexts during childhood. Journal of Experimental Child Psychology. 2016;142:274–290. doi: 10.1016/j.jecp.2015.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Degnan KA, Pine DS, Perez-Edgar K, Henderson HA, Diaz Y, Fox NA. Stable early maternal report of behavioral inhibition predicts lifetime Social Anxiety Disorder in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48(9):928–935. doi: 10.1097/CHI.0b013e3181ae09df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clauss JA, Blackford JU. Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:1066e1075. doi: 10.1016/j.jaac.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal patterns of anxiety from childhood to adulthood: The Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(1):21–33. doi: 10.1016/j.jaac.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Côté S, Tremblay RE, Nagin D, Zoccolillo M, Vitaro F. The development of impulsivity, fearfulness, and helpfulness during childhood: Patterns of consistency and change in the trajectories of boys and girls. Journal of Child Psychology and Psychiatry. 2002;43(5):609–618. doi: 10.1111/1469-7610.00050. [DOI] [PubMed] [Google Scholar]
- Cox FN, Campbell D. Young children in a new situation with and without their mothers. Child Development. 1968;39:123–131. [PubMed] [Google Scholar]
- Dadds MR, Roth JH. Family processes in the development of anxiety problems. In: Vasey MW, Dadds MR, editors. The developmental psychopathology of anxiety. New York, NY: Oxford University Press, Inc; 2001. pp. 278–303. [Google Scholar]
- Egger HL, Angold A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry. 2006;47(3–4):313–337. doi: 10.1111/j.1469-7610.2006.01618.x. http://doi.org/10.1111/j.1469-7610.2006.01618.x. [DOI] [PubMed] [Google Scholar]
- Else-Quest NM, Hyde JS, Goldsmith HH, Van Hulle CA. Gender differences in temperament: A meta-analysis. Psychological Bulletin. 2006;132(1):33–72. doi: 10.1037/0033-2909.132.1.33. [DOI] [PubMed] [Google Scholar]
- Enders CK. Analyzing longitudinal data with missing values. Rehabilitation Psychology. 2011;56(4):267–288. doi: 10.1037/a0025579. [DOI] [PubMed] [Google Scholar]
- Essex MJ, Klein MH, Cho E, Kalin NH. Maternal stress beginning in infancy may sensitize children to later stress exposure: effects on cortisol and behavior. Biological Psychiatry. 2002;52(8):776–784. doi: 10.1016/s0006-3223(02)01553-6. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Bridgett DJ, Rothbart MK, Robertson C, Iddins E, Ramsay K, Schlect S. A latent growth examination of fear development in infancy: Contributions of maternal depression and the risk for toddler anxiety. Developmental Psychology. 2010;46(3):651–668. doi: 10.1037/a0018898. [DOI] [PubMed] [Google Scholar]
- Gershaw NJ, Schwarz JC. The effects of a familiar toy and mother’s presence on exploratory and attachment behaviors in young children. Child Development. 1971;42(5):1662–1666. [PubMed] [Google Scholar]
- Gilissen R, Koolstra C, van IJzendoorn MH, Bakermans-Kranenburg MJ, van der Veer R. Physiological reactions of preschoolers to fear-inducing film clips: Effects of temerapmental fearfulness and the quality of the parent-child relationship. Developmental Psychobiology. 2007;49(2):187–195. doi: 10.1002/dev.20188. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH. Studying temperament via construction of the Toddler Behavior Assessment Questionnaire. Child Development. 1996;67(1):218–235. [PubMed] [Google Scholar]
- Greaves-Lord K, Ferdinand RF, Oldehinkel AJ, Sondeijker FEPL, Ormel J, Verhulst FC. Higher cortisol awakening response in young adolescents with persistent anxiety problems. Acta Psychiatrica Scandinavica. 2007;116(2):137–144. doi: 10.1111/j.1600-0447.2007.01001.x. [DOI] [PubMed] [Google Scholar]
- Gunnar MR. Reactivity of the Hypothalamic-Pituitary-Adrenocortical system to stressors in normal infants and children. Pediatrics. 1992;90(3):491–497. [PubMed] [Google Scholar]
- Gunnar MR, Larson MC, Hertsgaard L, Harris ML, Brodersen L. The stressfulness of separation among nine-month-old infants: Effects of social context variables and infant temperament. Child Development. 1992;63(2):290–303. [PubMed] [Google Scholar]
- Gunnar M, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58(1):145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Gunnar M, Tout K, de Haan NM, Pierce S, Stansbury K. Temperament, social competence, and adrenocortical activity in preschoolers. Developmental Psychobiology. 1997;31:65–85. doi: 10.1002/(sici)1098-2302(199707)31:1<65::aid-dev6>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- Hill-Soderlund AL, Braungart-Rieker JM. Early individual differences in temperamental reactivity and regulation: Implications for effortful control in early childhood. Infant Behavior and Development. 2008;31(3):386–397. doi: 10.1016/j.infbeh.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Hirshfeld DR, Rosenbaum JF, Biederman J, Bolduc EA, Faraone SV, Snidman N, Kagan J. Stable behavioral inhibition and its association with Anxiety Disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(1):103–111. doi: 10.1097/00004583-199201000-00016. [DOI] [PubMed] [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. [Google Scholar]
- Kagan J. Galen’s Prophecy: Temperament in Human Nature. New York: Basic Books; 1994. [Google Scholar]
- Kiel EJ, Buss KA. Prospective relations among fearful temperament, protective parenting, and social withdrawal: The role of maternal accuracy in a moderated mediation framework. Journal of Abnormal Child Psychology. 2011;39(7):953–966. doi: 10.1007/s10802-011-9516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Dyson MW, Kujawa AJ, Kotov R. Temperament and internalizing disorders. In: Zentner M, Bates JE, editors. Handbook of Temperament. New York, New York: Guilford Press; 2012. pp. 541–561. [Google Scholar]
- Klimes-Dougan B, Hastings PD, Granger DA, Usher B, Zahn-Waxler C. Adrenocortical activity in at-risk and normally developing adolescents: Individual differences in salivary cortisol basal levels, diurnal variation, and responses to social challenges. Development and Psychopathology. 2001;13(03):695–719. doi: 10.1017/s0954579401003157. [DOI] [PubMed] [Google Scholar]
- Larson MC, White BP, Cochran A, Donzella B, Gunnar M. Dampening of the cortisol response to handling at 3 months in human infants and its relation to sleep, circadian cortisol activity, and behavioral distress. Developmental Psychobiology. 1998;33(4):327–337. [PubMed] [Google Scholar]
- Lewinsohn PM, Gotlib IH, Lewinsohn M, Seeley JR, Allen NB. Gender differences in anxiety disorders and anxiety symptoms in adolescents. Journal of Abnormal Psychology. 1998;107(1):109–117. doi: 10.1037//0021-843x.107.1.109. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Zinbarg R, Seeley JR, Lewinsohn M, Sack WH. Lifetime comorbidity among anxiety disorders and between anxiety disorders and other mental disorders in adolescents. Journal of Anxiety Disorders. 1997;11(4):377–394. doi: 10.1016/s0887-6185(97)00017-0. [DOI] [PubMed] [Google Scholar]
- Marks I. The Development of Normal Fear: A Review. Journal of Child Psychology and Psychiatry. 1987;28(5):667–697. doi: 10.1111/j.1469-7610.1987.tb01552.x. [DOI] [PubMed] [Google Scholar]
- Mash EJ, Barkley RA. Child psychopathology. Guilford Press; 2003. [Google Scholar]
- McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research. 2011;45(8):1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mian ND, Godoy L, Briggs-Gowan MJ, Carter AS. Patterns of anxiety symptoms in toddlers and preschool-age children: Evidence of early differentiation. Journal of Anxiety Disorders. 2012;26(1):102–110. doi: 10.1016/j.janxdis.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, van Brakel AM, Arntz A, Schouten E. Behavioral inhibition as a risk factor for the development of childhood anxiety disorders: a longitudinal study. Journal of Child and Family Studies. 2011;20(2):157–170. doi: 10.1007/s10826-010-9365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of quantitative methodology for social sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- Pendry P, Adam EK. Associations between parents’ marital functioning, maternal parenting quality, maternal emotion and child cortisol levels. International Journal of Behavioral Development. 2007;31(3):218–231. [Google Scholar]
- Pérez-Edgar K, Bar-Haim Y, McDermott JM, Chronis-Tuscano A, Pine DS, Fox NA. Attention biases to threat and behavioral inhibition in early childhood shape adolescent social withdrawal. Emotion. 2010;10(3):349. doi: 10.1037/a0018486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Edgar K, Reeb-Sutherland BC, McDermott JM, White LK, Henderson HA, Degnan KA, Fox NA. Attention biases to threat link behavioral inhibition to social withdrawal over time in very young children. Journal of Abnormal Child Psychology. 2011;39(6):885–895. doi: 10.1007/s10802-011-9495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. 1998;55(1):56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Poulton R, Milne BJ, Craske MG, Menzies RG. A longitudinal study of the etiology of separation anxiety. Behaviour Research and Therapy. 2001;39(12):1395–1410. doi: 10.1016/s0005-7967(00)00105-4. [DOI] [PubMed] [Google Scholar]
- Rheingold HL, Eckerman CO. Fear of the stranger: A crticial examination. In: Reese HW, editor. Advances in Child Development and Behavior. Vol. 8. New York: Academic Press; 1973. [DOI] [PubMed] [Google Scholar]
- Rosen JB, Schulkin J. From normal fear to pathological anxiety. Psychological Review. 1998;105(2):325–350. doi: 10.1037/0033-295x.105.2.325. [DOI] [PubMed] [Google Scholar]
- Rothbart MK. Measurement of temperament in infancy. Child Development. 1981;52(2):569–578. [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, Fisher P. Investigations of temperament at three to seven years: The Children’s Behavior Questionnaire. Child Development. 2001;72(5):1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- Ruttle PL, Maslowsky J, Armstrong JM, Burk LR, Essex MJ. Longitudinal associations between diurnal cortisol slope and alcohol use across adolescence: A seven-year prospective study. Psychoneuroendocrinology. 2015;56:23–28. doi: 10.1016/j.psyneuen.2015.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salis KL, Bernard K, Black SR, Dougherty LR, Klein D. Examining the concurrent and longitudinal relationship between diurnal cortisol rhythms and conduct problems during childhood. Psychoneuroendocrinology. 2016;71:147–154. doi: 10.1016/j.psyneuen.2016.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saridjan NS, Velders FP, Jaddoe VW, Hofman A, Verhulst FC, Tiemeier H. The longitudinal association of the diurnal cortisol rhythm with internalizing and externalizing problems in pre-schoolers. The Generation R Study. Psychoneuroendocrinology. 2014;50:118–129. doi: 10.1016/j.psyneuen.2014.08.008. [DOI] [PubMed] [Google Scholar]
- Schmidt NL, Van Hulle CA, Brooker RJ, Meyer LR, Lemery-Chalfant K, Goldsmith HH. Wisconsin Twin Research: Early development, childhood psychopathology, Autism, and Sensory over-responsivity. Twin Research and Human Genetics. 2013;16(Special Issue 01):376–384. doi: 10.1017/thg.2012.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulkin J, McEwen BS, Gold PW. Allostasis, amygdala, and anticipatory angst. Neuroscience & Biobehavioral Reviews. 1994;18(3):385–396. doi: 10.1016/0149-7634(94)90051-5. [DOI] [PubMed] [Google Scholar]
- Schwartz CE, Snidman N, Kagan J. Adolescent social anxiety as an outcome of inhibited temperament in childhood. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(8):1008–1015. doi: 10.1097/00004583-199908000-00017. [DOI] [PubMed] [Google Scholar]
- Scher A, Hall WA, Zaidman-Zait A, Weinberg J. Sleep quality, cortisol levels, and behavioral regulation in toddlers. Developmental Psychobiology. 2010;52:44–53. doi: 10.1002/dev.20410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirtcliff EA, Essex MJ. Concurrent and longitudinal associations of basal and diurnal cortisol with mental health symptoms in early adolescence. Developmental Psychobiology. 2008;50(7):690–703. doi: 10.1002/dev.20336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirtcliff EA, Granger DA, Booth A, Johnson D. Low salivary cortisol levels and externalizing behavior problems in youth. Development and Psychopathology. 2005;17(01):167–184. doi: 10.1017/s0954579405050091. [DOI] [PubMed] [Google Scholar]
- Shirtcliff EA, Ruttle P. Immunological and neuroendocrine dysregulation following early deprivation and stress. In: Brisch KH, editor. Attachment and Early Disorders of Development. Munich: Klett-Cotta; 2010. [Google Scholar]
- Smider NA, Essex MJ, Kalin NH, Buss KA, Klein MH, Davidson RJ, Goldsmith HH. Salivary cortisol as a predictor of socioemotional adjustment during kindergarten: A prospective study. Child Development. 2002;73(1):75–92. doi: 10.1111/1467-8624.00393. [DOI] [PubMed] [Google Scholar]
- Spence SH, Rapee R, McDonald C, Ingram M. The structure of anxiety symptoms among preschoolers. Behaviour Research and Therapy. 2001;39(11):1293–1316. doi: 10.1016/s0005-7967(00)00098-x. [DOI] [PubMed] [Google Scholar]
- Sroufe LA. Wariness of strangers and the study of infant development. Child Development. 1977;48(3):731–746. [Google Scholar]
- Stanger C, Lewis M. Agreement among parents, teachers, and children on internalizing and externalizing behavior problems. Journal of Clinical Child Psychology. 1993;22(1):107–116. [Google Scholar]
- Van den Bergh BRH, Van Calster B, Pinna Puissant S, Van Huffel S. Self-reported symptoms of depressed mood, trait anxiety and aggressive behavior in post-pubertal adolescents: Associations with diurnal cortisol profiles. Hormones and Behavior. 2008;54(2):253–257. doi: 10.1016/j.yhbeh.2008.03.015. [DOI] [PubMed] [Google Scholar]
- Van Hulle CA, Shirtcliff EA, Lemery-Chalfant K, Goldsmith HH. Genetic and environmental influences on individual differences in cortisol level and circadian rhythm in middle childhood. Hormones and Behavior. 2012;62(1):36–42. doi: 10.1016/j.yhbeh.2012.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeer HJ, van IJzendoorn MH. Children’s elevated cortisol levels at daycare: A review and meta-analysis. Early Childhood Research Quarterly. 2006;21(3):390–401. [Google Scholar]
- Westenberg PM, Gullone E, Bokhorst CL, Heyne DA, King NJ. Social evaluation fear in childhood and adolescence: Normative developmental course and continuity of individual differences. British Journal of Developmental Psychology. 2007;25(3):471–483. [Google Scholar]