Abstract
Objectives
The current study is the first to assess pregnant women’s perceptions of e-cigarettes and the prevalence of e-cigarette use during pregnancy, using a national sample of pregnant women (N = 445) recruited online.
Methods
An online survey was used to assess the prevalence and perceptions of e-cigarette use among pregnant women, including perceptions of e-cigarette safety.
Results
In our sample, 5.62% (n =25) of women solely used tobacco cigarettes, 6.52% (n =29) solely used e-cigarettes, 8.54% (n =38) used both tobacco cigarettes and e-cigarettes, and 79.33% (n = 353) used neither tobacco cigarettes nor e-cigarettes during their current pregnancy. Overall, 64.27% (n = 286) of participants viewed e-cigarettes as being safer than tobacco cigarettes. Having seen advertisements for e-cigarettes increased likelihood of viewing them as safer than tobacco cigarettes (OR [Odds Ratio] = 2.5, p < .01).
Conclusions for Practice
Taken together, findings from this study suggest that at least as many women use e-cigarettes during pregnancy as tobacco cigarettes, that pregnant women view e-cigarettes as being safer than tobacco cigarettes, and that these views may be influenced by exposure to e-cigarette advertisements.
Keywords: Electronic Cigarettes, Pregnancy, Nicotine, Smoking, Maternal Health
There has been substantial growth in the prevalence and popularity of electronic cigarettes (e-cigarettes; a battery operated device that vaporizes nicotine for inhalation) since they were developed in 2004, possibly motivated by advertisements that market them as a safer alternative to tobacco cigarettes (Grana, Benowitz, & Glantz, 2014). The rapid adoption of e-cigarettes into the market, despite unanswered questions about their overall public health impact, is a cause for concern among doctors, researchers, and policy makers. This is particularly true given studies that have shown e-cigarettes to deliver an equal, or possibly greater, amount of nicotine than tobacco cigarettes (Goniewicz, Kuma, Gawron, Knysak, & Kosmider, 2013; Grana et al., 2014; Vansickel & Eissenberg, 2013). In addition, although men are more likely to report awareness of e-cigarettes, women are more likely to try them (King, Alam, Promoff, Arrazola, & Dube, 2013). Taken together, it is possible that pregnant smokers, a subsample of women who may be particularly motivated to change their smoking habits and to improve their overall health, may be likely to initiate and engage in e-cigarette use during pregnancy. However, little research has specifically examined rates of e-cigarette use among pregnant women in the United States. Given the robust evidence demonstrating an association between prenatal exposure to nicotine and adverse health, behavioral, and cognitive outcomes in offspring (Mezzacappa, Buckner, & Earls, 2011; Wiebe et al., 2015), understanding the rates and motivations of e-cigarette use among this population is a key research question motivating the current study.
E-cigarettes are marketed as healthier alternatives to tobacco products which may increase their appeal to women who smoke when they become pregnant. Although research suggests that levels of toxicants in e-cigarette aerosols are 1 to 2 orders of magnitude lower than in combustible tobacco products, trace levels of toxicants, including formaldehyde, acetaldehyde, nickel, and lead, are still present (Goniewicz et al., 2014). While there is some variability in the reported amount of nicotine vaporized by e-cigarettes (i.e., 21% to 85% of nicotine present in cartridges), the majority of research suggest significant amounts of nicotine delivery (Etter, 2014; Goniewicz et al., 2013; Grana et al., 2014). One study which tested e-cigarettes of varying levels of nicotine found that e-cigarettes deliver between 0.5 ng/mL and 15.4 ng/mL (Goniewicz et al., 2013) and another reported a rise in participants’ serum cotinine of approximately 20 ng/mL immediately after use (Flouris et al., 2013). Despite evidence suggesting e-cigarettes can deliver less nicotine per puff than tobacco cigarettes (Bullen et al., 2010; Goniewicz et al., 2013), some research shows that nicotine absorption from e-cigarette use can equal or surpass that of conventional tobacco cigarettes as the user gains experience (Etter, 2014).
Efficient nicotine delivery from e-cigarettes is especially problematic during pregnancy. Previous research on tobacco cigarettes has found that nicotine readily crosses the placenta and fetal concentrations can exceed those in the mother, which has potential to interfere with delivery of oxygen to fetal tissues (Lambers & Clark, 1996). In turn, prenatal nicotine exposure has been linked to negative effects on the central nervous system (such as cell damage and disrupted development) that lead to problems with regulatory activities and reactivity to stress (Kinney, O’Donnell, Kriger, & White, 1993), cardiac functioning (Fried & Makin, 1987; Schuetze & Zeskind, 1997; Schuetze, Eiden, & Danielewicz, 2009), somatic motor control, and sleep-wake state organization (Stéphan-Blanchard et al., 2008). Additionally, prenatal exposure to nicotine is correlated with a number of severe health issues such as low birth weight, prematurity, asthma, congenital heart defects, higher risk of future addiction (Benowitz, 2008; Wakschlag, Pickett, Cook, Benowitz, & Leventhal, 2002; Windham, Hopkins, Fenster, & Swan, 2000), adverse behavioral outcomes including higher risk of aggression, attention deficit hyperactivity disorder, conduct disorder, and delinquency (Button, Thapar, & McGuffin, 2005; Day, Richardson, Goldschmidt, & Cornelius, 2000; Fergusson, 1999; Thapar et al., 2003; Wakschlag et al., 2002), as well as cognitive deficits in language, memory, and general intellectual ability (Cornelius, Ryan, Day, Goldschmidt, & Willford, 2001; Mezzacappa et al., 2011; Pa, Watkinson, Grant, & Knights, 1980). However, even with all of these known health risks from tobacco cigarettes, one recent study detected high-level nicotine exposure for 16.5 percent of women and low-level exposure for an additional 7.5 percent of their sample, despite only 8.6 percent of their sample reporting cigarette use (Hall, Wexelblatt, & Greenberg, 2016). Further, less than half (37% – 46%) of all women who smoke will quit before or during pregnancy (Colman & Joyce, 2003). Thus far, no prevalence estimates have been reported for e-cigarette use during pregnancy, though we hypothesize that it may be equal to or exceed rates of traditional cigarette use.
E-cigarettes were not tested and approved by regulatory agencies (e.g., U.S. Food and Drug Agency (FDA), U.K. Medicines and Healthcare Products Regulatory Agency) prior to their release in the global market (Trtchounian & Talbot, 2011), although in 2016, the FDA expanded their coverage to include electronic cigarettes. Thus, for several years, e-cigarette packaging and advertisements were not federally required to display warning messages about smoking-related pregnancy complications. This fact is especially concerning that changes in market share resulting from advertising are due mainly to young smokers and that the content of e-cigarette advertisements may particularly appeal to young people because they emphasize themes of independence and maturity (Duke et al., 2014; Pierce, Gilpin, & Burns, 1991). Given that our study was conducted prior to the regulation of e-cigarettes by the FDA, we hypothesize that exposure to e-cigarette advertisements will be high among pregnant women, and that viewing advertisements will be related to women’s perceptions of e-cigarette safety.
The current study is the first to examine not only the prevalence of e-cigarette use among pregnant women, but also exposure to advertisements and perceptions of safety of these devices. We specifically examine the extent to which pregnant women view e-cigarettes as a safe alternative to tobacco cigarettes. These aims address sizeable gaps in the nicotine literature and promise to inform future research and regulatory efforts.
METHODS
Participants and Procedures
Data were obtained from on online survey of pregnant women (N = 445) recruited using a national website survey service (Amazon Mechanical Turk or MTurk). MTurk is an online labor market where requesters post opportunities to complete tasks for compensation. The behavior of MTurk participants is comparable to that of other recruitment methods, and MTurk has been identified as a useful tool for conducting behavioral research (Mason & Suri, 2012). Participant IP addresses, randomly generated identification numbers, and location information were collected solely for the purposes of restricting duplicate submissions, and were not retained in the final dataset. Because the study was conducted online, we employed a number of steps to maximize the likelihood that participants were pregnant women. The survey was advertised as a set of questions focused on experiences of adults living in the United States. Participants were informed that they would complete a 5-question unpaid screener prior to completing the study but were not given any additional information regarding desired qualifications. Those who met the criteria for participation provided sociodemographic characteristics, including age, race/ethnicity, education, household income, and rurality. Compensation for participation was sent through protocols established by Amazon Mechanical Turk. Although the study protocol was reviewed and designated as exempt by the University of North Carolina at Chapel Hill Institutional Review Board (UNC-IRB) due to the lack of identifying information collected and the low risk associated with participation, the research was conducted in accord with prevailing ethical principles of the UNC-IRB. All data were collected in July and August 2015.
Measures
The online survey included a series of questions intended to assess the prevalence and perceptions of electronic cigarette use among pregnant women. All of the items included in the survey were reviewed by experts affiliated with the Center for Regulatory Research on Tobacco Communication at the University of North Carolina at Chapel Hill and were piloted by electronic cigarette users in the community.
Prevalence of Electronic Cigarette Use among Pregnant Women
Participants were asked a series of questions that assessed the extent to which they used electronic and tobacco cigarettes before and during their current pregnancy. Possible responses to describe participants’ frequency of use included ‘tried once’, ‘less than once a week’, ‘once a week’, more than once a week’, and ‘daily’. Participants were also asked if they switched to or began using electronic cigarettes when they learned that they were pregnant, if their use had increased, decreased, or stayed the same over the course of their pregnancy, and if they intended to alter their use from the time of survey completion until the end of their pregnancy. Participants who indicated that they used electronic cigarettes during pregnancy were offered an opportunity to provide a written response describing the reason they began using e-cigarettes. Questions regarding the use of electronic and tobacco cigarettes were only completed by participants who indicated that they were currently using either form of cigarette at the time of survey completion.
Exposure to Advertisements and Perceptions of Electronic Cigarettes among Pregnant Women
Participants were asked a number of questions regarding the extent to which they had seen advertisements (e.g. internet, print, television) for electronic cigarettes in the past. They were also asked to indicate their agreement with several statements relating to the safety of electronic cigarettes, both in general and for pregnant women. Finally, participants responded to a set of questions concerning the regulation and sale of electronic cigarettes. For example, participants were asked if they believed that electronic cigarettes should be regulated like tobacco cigarettes, if they should be available for purchase on the internet, and if they should be available for purchase by minors. All participants completed questions regarding advertisement exposure and perceptions of electronic cigarettes, regardless of current electronic or tobacco cigarette use.
Analytic Strategy
We created four groups based on participants’ responses to questions regarding their electronic and tobacco cigarette use during pregnancy: tobacco cigarette-only users, electronic cigarette-only users, dual users, and non-users. One-way analysis of variance (ANOVA) procedures were used to compare demographic differences and patterns of use across these four groups. We then performed logistic regression analyses using dummy-coded grouping variables to compare participants’ perceptions of electronic cigarettes, likelihood of having seen electronic cigarette advertisements, and views on e-cigarette safety and regulation across the four groups described above. Analyses controlled for demographic covariates, including age, race/ethnicity, education, household income, and rurality. All participants (n = 445) provided complete data. Analyses were conducted using SAS version 9.3 (SAS Institute Inc.). In order to aid interpretation, analyses were specified to model the likelihood of endorsing a given outcome.
RESULTS
Demographics
Participants who indicated that they were under the age of 18, male, or currently not pregnant were informed that they did not qualify for the study. Of 14,467 people who viewed the survey, 12,427 completed the screener questions. Of these, 4,918 (38%) were male and 7,644 (62%) were female. A total of 607 of the 7,644 (7.9%) women who completed the screener were pregnant. A final sample of 445 pregnant women consented to participate in the study and provided data (Figure 1). Participating women ranged in age from 18 to 45 (Mage = 27.63, SD = 5.34). Maternal race was 72.58% (n = 323) Caucasian, 15.06% (n = 67) African-American, and 12.36% (n = 55) other or mixed race with several mothers reporting more than one race. Reported income ranged from less than $10,000 to more than $150,000 with 75% of the sample reporting income between $20,000 and $75,000. At the time of the time of participation, about 8% of mothers had completed a GED or high school degree, 31% had completed some post-secondary courses, 13% had completed an associate’s degree, and 36% of women had received a degree from a four-year college. A slight majority of participants reported living in a ‘suburban’ area (52.13%, n = 232), while 33.71% (n = 150) reported living in an ‘urban’ area and 14.16% (n = 63) reported living in a ‘rural’ area. A majority of women (63.37%, n = 282) were primiparous (i.e. pregnant for the first time).
Figure 1.
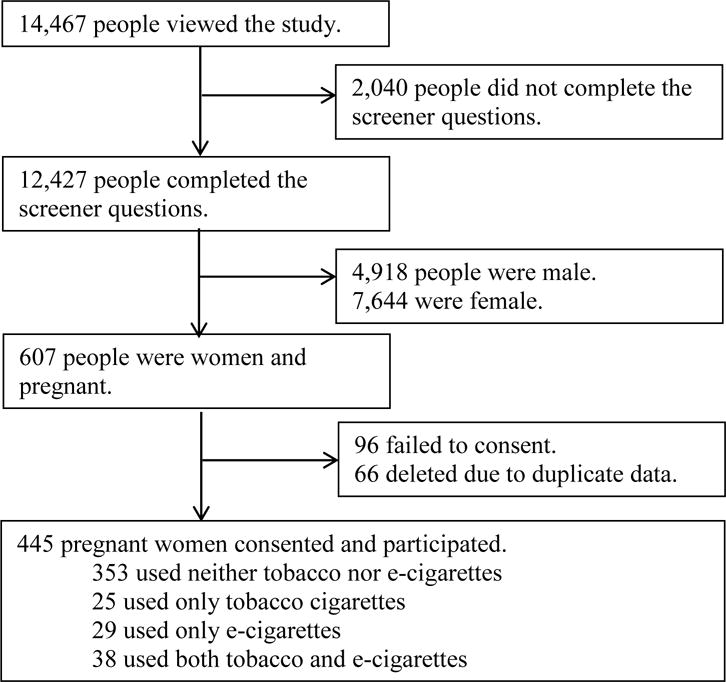
Flow of Pregnant Women Recruitment and Participation.
Prevalence of Electronic Cigarette Use among Pregnant Women
In our sample, 5.62% (n =25) of women were tobacco cigarette users, 6.52% (n =29) were e-cigarette users, 8.54% (n =38) used both tobacco cigarettes and e-cigarettes, and 79.33% (n = 353) used neither tobacco cigarettes nor e-cigarettes. Of the e-cigarette users, 74.6% (n=50) reported switching to e-cigarettes when they learned they were pregnant. E-cigarette users (Mage = 26.6 yrs.) and dual users (Mage = 27.1 yrs.) were significantly younger than cigarette-users (Mage = 30.6), f(3) = 3.24, p < .05. Type of use (i.e. e-cigarette, tobacco cigarette, or dual use) did not vary by race, income, or rurality (Table 1). There were no differences in the frequency of use of electronic cigarettes during pregnancy between e-cigarette users and dual users, f(1) = 0.50, p = .48. E-cigarette users were more likely to be satisfied with their experiences using electronic cigarettes during pregnancy than were dual users, although this difference only approached significance (odds ratio [OR] = 2.8, p = .06 [95% CI, 0.9 – 13.4]).
Table 1.
Sample Characteristics by Groups
| Total (n = 445) |
Non-Users (n = 353) |
Tobacco Cigarette Only (n = 25) |
E-Cigarette only (n = 29) |
Dual Users (n = 38) | P Value | |
|---|---|---|---|---|---|---|
| Age, mean (SD) | 27.6 (5.3) | 27.5 (5.2)a | 30.7 (5.9)a,b,c | 26.7 (4.6)c | 27.1 (5.7)b | .02d |
|
| ||||||
| Race/Ethnicity | ||||||
|
| ||||||
| American Indian | 5 (1.1%) | 4 (1.2%) | 0 (0.0%) | 0 (0.0%) | 1 (2.6%) | 0.85f |
| Asian | 36 (8.1%) | 31 (8.7%) | 0 (0.0%) | 2 (6.8%) | 3 (7.9%) | |
| Black | 52 (11.8%) | 40 (11.3%) | 3 (22.0%) | 4 (13.7%) | 5 (13.1%) | |
| Latino(a)/Hispanic | 13 (2.9%) | 12 (3.4%) | 0 (0.0%) | 0 (0.0%) | 1 (2.6%) | |
| White | 335 (75.2%) | 263 (74.5%) | 22 (88.0%) | 23 (79.5%) | 27 (71.2%) | |
| Other | 4 (0.9%) | 3 (0.9%) | 0 (0.0%) | 0 (0.0%) | 1 (2.6%) | |
|
| ||||||
| Education | ||||||
|
| ||||||
| < High School | 10 (2.3%) | 6 (1.7%) | 1 (4.0%) | 1 (3.4%) | 2 (5.3%) | 0.001f |
| Some High School | 18 (4.1%) | 9 (2.6%) | 3 (12.0%) | 3 (10.3%) | 3 (7.9%) | |
| High School | 18 (4.1%) | 13 (3.7%) | 0 (0.0%) | 4 (13.9%) | 1 (2.6%) | |
| Some College | 196 (44.1%) | 147 (41.6%) | 16 (64.0%) | 15 (51.7%) | 18 (47.4%) | |
| College Graduate | 151 (33.9%) | 134 (37.9%) | 2 (8.0%) | 6 (20.7%) | 9 (23.7%) | |
| Graduate Degree | 52 (11.5%) | 44 (12.5%) | 3 (12.0%) | 0 (0.0%) | 5 (13.1%) | |
|
| ||||||
| Incomee | ||||||
|
| ||||||
| <10,000 | 31 (7.5%) | 23 (7.0%) | 2 (8.0%) | 1 (3.7%) | 5 (14.3%) | 0.09f |
| 10,000 – 29,999 | 116 (27.9%) | 81 (24.7%) | 10 (40.0%) | 10 (37.1%) | 15 (40.0%) | |
| 30,000 – 49,999 | 118 (28.4%) | 91 (27.7%) | 6 (24.0%) | 11 (40.7%) | 10 (28.6%) | |
| 50,000 – 69,999 | 78 (18.8%) | 68 (20.7%) | 5 (20.0%) | 3 (11.1%) | 2 (5.7%) | |
| 70,000 – 99,999 | 43 (10.3%) | 40 (12.2%) | 0 (0.0%) | 1 (3.7%) | 2 (5.7%) | |
| >100,000 | 29 (7.1%) | 25 (7.7%) | 2 (8.0%) | 1 (3.7%) | 1 (5.7%) | |
|
| ||||||
| Rurality | ||||||
|
| ||||||
| Rural | 150 (33.7%) | 114 (32.3%) | 11 (44.0%) | 10 (34.5%) | 15 (39.5%) | 0.83f |
| Urban | 232 (52.1%) | 188 (53.3%) | 10 (40.0%) | 16 (55.2%) | 18 (47.4%) | |
| Suburban | 64 (14.2%) | 51 (14.4%) | 4 (16.0%) | 3 (10.3%) | 5 (13.1%) | |
|
| ||||||
| Weeks Pregnant, Mean (SD) | 17.3 (9.8) | 17.6 (9.9) | 21 (10.1)a,b | 13.8 (8.4)a | 13.8 (8.9)b | 0.005d |
Note
ANOVA Contrasts;
Analysis-of-Variance;
Thirty participants chose not to respond;
X2 analysis;
Exposure to Advertisements and Perceptions of Electronic Cigarettes among Pregnant Women
Overall, 64.27% (n = 286) of participants viewed electronic cigarettes as being safer than tobacco cigarettes in general. However, only 35.28% (n = 157) of participants viewed electronic cigarettes as being safer than tobacco cigarettes for pregnant women. E-cigarette users and participants who used both electronic and tobacco cigarettes during pregnancy were significantly more likely to view electronic cigarettes as being safer than tobacco cigarettes in general (OR = 9.7, p < .01 [95% CI, 2.3 – 42.2] and OR = 3.7, p < .01 [95% CI, 1.5 – 9.2], respectively) and during pregnancy (OR = 13.4, p < .01 [95% CI, 4.9 – 36.9] and OR = 10.9, p < .01 [95% CI, 4.7 – 25.1], respectively) compared to women who did not report smoking during pregnancy. Tobacco cigarettes users did not differ from those who did not smoke in their views regarding the safety of electronic cigarettes in general (OR = 0.7, p = .52) or during pregnancy (OR = 2.0, p = .11). A majority of the sample (83.15%, n = 370) reported that they have seen advertisements for electronic cigarettes, which was associated with an increased likelihood of viewing them as safer than tobacco cigarettes in general (OR = 2.5, p < .01 [95% CI, 1.5 – 4.1]) and for pregnant women (OR = 2.1, p < .05 [95% CI, 1.2 – 3.8]), controlling for demographics and tobacco use group. There were no differences between use groups in the likelihood of having ever seen an electronic cigarette advertisement. Of the 50 participants who indicated that they switched to or began using electronic cigarettes when they learned they were pregnant, 46% (n = 23) wrote that they did so because they are safer than tobacco cigarettes or would do less harm to their child, 18% (n = 9) indicated that they did so in order to quit using tobacco cigarettes, and two participants indicated that they began using electronic cigarettes at the direction of their health care provider. A majority of participants indicated that electronic cigarettes should be regulated like tobacco cigarettes (67.87%, n = 302), should not be sold to minors (89.89%, n = 400), and pose similar public health risks as tobacco cigarettes (55.28%, n = 246). A larger proportion of tobacco cigarette users than e-cigarette users indicated that electronic cigarettes should be regulated like tobacco cigarettes (72% vs. 44%, respectively; f(1) = 4.23, p < .05), and pose similar public health risks as tobacco cigarettes (56% vs. 21%, respectively; f(1) = 6.11, p < .05), controlling for demographic variables. However, tobacco cigarette users and e-cigarette users did not differ in their views regarding sales to minors (16% vs. 17%, respectively; f(1) = 0.01, p = .91).
DISCUSSION
There has been growth in the prevalence and popularity of e-cigarette use in recent years. Studies of U.S. adults found that awareness of e-cigarettes doubled between 2009 and 2010 (Regan, Promoff, Dube, & Arrazola, 2011), that the number of people who have ever used an electronic cigarette increased from 1.8% [2010] to 13% [2013] (McMillen, Gottlieb, Shaefer, Winickoff, & Klein, 2014), and that the number of people who currently use e-cigarettes increased from 0.3% [2010] to 6.8% [2013] (McMillen et al., 2014). Despite the increase in e-cigarette use and the significant policy and health implications of prenatal nicotine exposure, little is known about the extent to which women use electronic cigarettes during pregnancy and how e-cigarettes are perceived by expecting mothers. This line of research is particularly relevant given the ubiquity of advertisements suggesting that e-cigarettes are a safe alternative to tobacco cigarettes (Grana, Popova, & Ling, 2014). Findings from this study suggest that rates of e-cigarette use among pregnant women may exceed those of tobacco cigarette users, that e-cigarette use may be initiated when women learn they are pregnant, and that advertisements may contribute to e-cigarette use during pregnancy.
These data are the first to provide estimates for the prevalence of e-cigarette use during pregnancy, using data collected from a large, nationwide sample. This demographic is a particularly important one to study, given the consistent links between prenatal nicotine exposure and negative perinatal outcomes (Lambers & Clark, 1996). The current findings suggest that the rate of e-cigarette use during pregnancy, both alone or in combination with tobacco cigarettes, approaches 13% and may exceed the rate of sole tobacco cigarette use. Because e-cigarettes deliver significant and potentially variable amounts of nicotine (Czogala et al., 2014; Dawkins & Corcoran, 2014), the rates of e-cigarette use found in the current study remain a cause for concern. This study also offers preliminary evidence that many of the women who use e-cigarettes during pregnancy initiated use when they learned that they were pregnant. Further, our data are the first to suggest that exposure to advertisements for e-cigarettes may be one factor influencing women’s beliefs about the safety of these devices. The possibility remains that individuals who view e-cigarettes as safer than tobacco cigarettes may be more likely to remember and report seeing e-cigarette advertisements. Despite this possibility, this study offers preliminary insight on prevalence and perceptions of e-cigarettes among pregnant women which has implications for practitioners and policy makers regarding the regulation and use of these devices.
The findings of this study are strengthened by the use of a large, diverse sample, a comprehensive assessment of both prevalence and perceptions of e-cigarettes, and statistical control for important covariates. The nature of data collection limited the extent to which we could collect detailed information regarding patterns of use across pregnancy and future studies should assess the extent to which use patterns differ across trimesters. Relatedly, the current study did not include data on past cigarette use, an important next step for research focused on examining the extent to which pregnancy disrupts trajectories of smoking across time. Although the current study included a large sample, small subgroup samples can lead to unstable estimates and future studies may benefit from targeted recruitment of tobacco and e-cigarette users. Additionally, this study relied on maternal-self report, as is standard with the majority of work on cigarette use during pregnancy. An important next step is to incorporate biological measurement of prenatal toxicity associated with e-cigarette use during pregnancy and to link use with important birth outcomes including birth weight and prematurity.
Significance.
Electronic cigarettes deliver significant amounts of nicotine to users and there is robust evidence demonstrating an association between prenatal exposure to nicotine and adverse health, behavioral, and cognitive outcomes in offspring. Despite this, there has been no empirical investigation of the prevalence and perceptions of e-cigarette use during pregnancy. This study provides initial evidence that the prevalence of e-cigarette use during pregnancy is at least equivalent to that of tobacco cigarette use, that expecting mothers view e-cigarettes as a safer alternative to tobacco products, and that advertisements may influence opinions of e-cigarette safety.
Acknowledgments
This work was supported by the National Cancer Institute and FDA Center for Tobacco Products (CTP) grant number 5P50CA180907. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Contributor Information
Nicholas J. Wagner, Human Development and Quantitative Methodology, University of Maryland, 3942 Campus Drive, College Park, MD 20742, 252.290.7444.
Marie Camerota, Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill, Chapel Hill NC USA.
Cathi Propper, The Center for Developmental Science, Chapel Hill NC USA.
References
- Benowitz NL. Clinical pharmacology of nicotine: implications for understanding, preventing, and treating tobacco addiction. Clinical Pharmacology and Therapeutics. 2008;83(4):531–541. doi: 10.1038/clpt.2008.3. http://doi.org/10.1038/clpt.2008.3. [DOI] [PubMed] [Google Scholar]
- Bullen C, McRobbie H, Thornley S, Glover M, Lin R, Laugesen M. Effect of an electronic nicotine delivery device (e cigarette) on desire to smoke and withdrawal, user preferences and nicotine delivery: randomised cross-over trial. Tobacco Control. 2010;19(2):98–103. doi: 10.1136/tc.2009.031567. http://doi.org/10.1136/tc.2009.031567. [DOI] [PubMed] [Google Scholar]
- Button TMM, Thapar A, McGuffin P. Relationship between antisocial behaviour, attention-deficit hyperactivity disorder and maternal prenatal smoking. The British Journal of Psychiatry : The Journal of Mental Science. 2005;187:155–60. doi: 10.1192/bjp.187.2.155. http://doi.org/10.1192/bjp.187.2.155. [DOI] [PubMed] [Google Scholar]
- Colman GJ, Joyce T. Trends in smoking before, during, and after pregnancy in ten states. American Journal of Preventive Medicine. 2003;24(1):29–35. doi: 10.1016/s0749-3797(02)00574-3. http://doi.org/10.1016/S0749-3797(02)00574-3. [DOI] [PubMed] [Google Scholar]
- Cornelius MD, Ryan CM, Day NL, Goldschmidt L, Willford JA. Prenatal tobacco effects on neuropsychological outcomes among preadolescents. Journal of Developmental & Behavioral Pediatrics. 2001;22(4):217–225. doi: 10.1097/00004703-200108000-00002. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=med4&AN=11530894\nhttp://202.120.227.56:3210/sfxlcl3?sid=OVID:medline&id=pmid:11530894&id=doi:&issn=0196-206X6isbn=&volume=22&issue=4&spage=217&pages=217-25&date=2001&title=Journal+of+De. [DOI] [PubMed] [Google Scholar]
- Czogala J, Goniewicz ML, Fidelus B, Zielinska-Danch W, Travers MJ, Sobczak A. Secondhand exposure to vapors from electronic cigarettes. Nicotine & Tobacco Research : Official Journal of the Society for Research on Nicotine and Tobacco. 2014;16(6):655–62. doi: 10.1093/ntr/ntt203. http://doi.org/10.1093/ntr/ntt203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawkins L, Corcoran O. Acute electronic cigarette use: Nicotine delivery and subjective effects in regular users. Psychopharmacology. 2014;231(2014):401–407. doi: 10.1007/s00213-013-3249-8. http://doi.org/10.1007/s00213-013-3249-8. [DOI] [PubMed] [Google Scholar]
- Day NL, Richardson GA, Goldschmidt L, Cornelius MD. Effects of prenatal tobacco exposure on preschoolers’ behavior. Journal of Developmental and Behavioral Pediatrics : JDBP. 2000;21(3):180–188. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med4&NEWS=N&AN=10883878. [PubMed] [Google Scholar]
- Duke JC, Lee YO, Kim AE, Watson KA, Arnold KY, Nonnemaker JM, Porter L. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134(1):e29–e36. doi: 10.1542/peds.2014-0269. http://doi.org/10.1542/peds.2014-0269. [DOI] [PubMed] [Google Scholar]
- Etter JF. Levels of saliva cotinine in electronic cigarette users. Addiction. 2014;109(5):825–829. doi: 10.1111/add.12475. http://doi.org/10.1111/add.12475. [DOI] [PubMed] [Google Scholar]
- Fergusson DM. Prenatal smoking and antisocial behavior. Archives of General Psychiatry. 1999;56(3):223–224. doi: 10.1001/archpsyc.56.3.223. http://doi.org/10.1001/archpsyc.56.3.223. [DOI] [PubMed] [Google Scholar]
- Flouris AD, Chorti MS, Poulianiti KP, Jamurtas AZ, Kostikas K, Tzatzarakis MN, Koutedakis Y. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhalation Toxicology. 2013;25(2):91–101. doi: 10.3109/08958378.2012.758197. http://doi.org/10.3109/08958378.2012.758197. [DOI] [PubMed] [Google Scholar]
- Fried PA, Makin JE. Neonatal behavioural correlates of prenatal exposure to marihuana, cigarettes and alcohol in a low risk population. Neurotoxicology and Teratology. 1987;9(1):1–7. doi: 10.1016/0892-0362(87)90062-6. http://doi.org/10.1016/0892-0362(87)90062-6. [DOI] [PubMed] [Google Scholar]
- Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, Benowitz N. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tobacco Control. 2014;23(2):133–9. doi: 10.1136/tobaccocontrol-2012-050859. http://doi.org/10.1136/tobaccocontrol-2012-050859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goniewicz ML, Kuma T, Gawron M, Knysak J, Kosmider L. Nicotine levels in electronic cigarettes. Nicotine and Tobacco Research. 2013;15(1):158–166. doi: 10.1093/ntr/nts103. http://doi.org/10.1093/ntr/nts103. [DOI] [PubMed] [Google Scholar]
- Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Internal Medicine. 2014;174(5):812–813. doi: 10.1001/jamainternmed.2014.187. http://doi.org/10.1001/jamainternmed.2014.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972–86. doi: 10.1161/CIRCULATIONAHA.114.007667. http://doi.org/10.1161/CIRCULATIONAHA.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall ES, Wexelblatt SL, Greenberg JM. Self-reported and laboratory evaluation of late pregnancy nicotine exposure and drugs of abuse. Journal of Perinatology. 2016:1–5. doi: 10.1038/jp.2016.100. (August 2015) http://doi.org/10.1038/jp.2016.100. [DOI] [PubMed]
- King BA, Alam S, Promoff G, Arrazola R, Dube SR. Awareness and ever-use of electronic cigarettes among U.S. adults, 2010-2011. Nicotine and Tobacco Research. 2013;15(9):1623–1627. doi: 10.1093/ntr/ntt013. http://doi.org/10.1093/ntr/ntt013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney HC, O’Donnell TJ, Kriger P, White WF. Early developmental changes in [3H]nicotine binding in the human brainstem. Neuroscience. 1993;55(4):1127–38. doi: 10.1016/0306-4522(93)90326-b. http://doi.org/10.1016/0306-4522(93)90326-B. [DOI] [PubMed] [Google Scholar]
- Lambers DS, Clark KE. The maternal and fetal physiologic effects of nicotine. Seminars in Perinatology. 1996;20(2):115–126. doi: 10.1016/s0146-0005(96)80079-6. http://doi.org/10.1016/S0146-0005(96)80079-6. [DOI] [PubMed] [Google Scholar]
- Mason W, Suri S. Conducting behavioral research on Amazon’s Mechanical Turk. Behavior Research Methods. 2012;44(1):1–23. doi: 10.3758/s13428-011-0124-6. http://doi.org/10.3758/s13428-011-0124-6. [DOI] [PubMed] [Google Scholar]
- McMillen RC, Gottlieb MA, Shaefer RMW, Winickoff JP, Klein JD. Trends in Electronic Cigarette Use Among U.S. Adults: Use is Increasing in Both Smokers and Nonsmokers. Nicotine & Tobacco Research. 2014:1–8. doi: 10.1093/ntr/ntu213. http://doi.org/10.1093/ntr/ntu213. [DOI] [PubMed]
- Mezzacappa E, Buckner JC, Earls F. Prenatal cigarette exposure and infant learning stimulation as predictors of cognitive control in childhood. Developmental Science. 2011;14(4):881–91. doi: 10.1111/j.1467-7687.2011.01038.x. http://doi.org/10.1111/j.1467-7687.2011.01038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pa F, Watkinson B, Grant A, Knights R. Changing Patterns of Soft Drug Use Prior to and During Pregnancy. 1980;6:323–343. doi: 10.1016/0376-8716(80)90199-4. [DOI] [PubMed] [Google Scholar]
- Pierce J, Gilpin E, Burns D. Does tobacco advertising target young people to start smoking?: evidence from California. Jama. 1991;266(22):3154–3158. http://doi.org/10.1001/jama.266.22.3154. [PubMed] [Google Scholar]
- Regan AK, Promoff G, Dube SR, Arrazola R. Electronic nicotine delivery systems: adult use and awareness of the “e-cigarette” in the USA. Tobacco Control. 2011:19–23. doi: 10.1136/tobaccocontrol-2011-050044. http://doi.org/10.1136/tobaccocontrol-2011-050044. [DOI] [PubMed]
- Schuetze P, Eiden RD, Danielewicz S. The association between prenatal cocaine exposure and physiological regulation at 13 months of age. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2009;50(11):1401–1409. doi: 10.1111/j.1469-7610.2009.02165.x. http://doi.org/10.1111/j.1469-7610.2009.02165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuetze P, Zeskind PS. Relation between reported maternal caffeine consumption during pregnancy and neonatal state and heart rate. Infant Behavior and Development. 1997;20(4):559–562. Retrieved from http://www.scopus.com/inward/record.url?eid=2-s2.0-0031256609&partnerID=40&md5=f79f642d6f538dabc88d061c14dbdb87. [Google Scholar]
- Stéphan-Blanchard E, Telliez F, Léké A, Djeddi D, Bach V, Libert JP, Chardon K. The influence of in utero exposure to smoking on sleep patterns in preterm neonates. Sleep. 2008;31(12):1683–1689. doi: 10.1093/sleep/31.12.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A, Fowler T, Rice F, Scourfield J, van den Bree M, Thomas H, Hay D. Maternal smoking during pregnancy and attention deficit hyperactivity disorder symptoms in offspring. The American Journal of Psychiatry. 2003;160(11):1985–9. doi: 10.1176/appi.ajp.160.11.1985. http://doi.org/10.1176/appi.ajp.160.11.1985. [DOI] [PubMed] [Google Scholar]
- Trtchounian A, Talbot P. Electronic nicotine delivery systems: is there a need for regulation? Tobacco Control. 2011;20(1):47–52. doi: 10.1136/tc.2010.037259. http://doi.org/10.1136/tc.2010.037259. [DOI] [PubMed] [Google Scholar]
- Vansickel AR, Eissenberg T. Electronic cigarettes: Effective nicotine delivery after acute administration. Nicotine and Tobacco Research. 2013;15(1):267–270. doi: 10.1093/ntr/ntr316. http://doi.org/10.1093/ntr/ntr316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Pickett KE, Cook E, Benowitz NL, Leventhal BL. Maternal smoking during pregnancy and severe antisocial behavior in offspring: A review. American Journal of Public Health. 2002;92(6):966–974. doi: 10.2105/ajph.92.6.966. http://doi.org/10.2105/AJPH.92.6.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe SA, Clark CAC, De Jong DM, Chevalier N, Espy KA, Wakschlag L. Prenatal tobacco exposure and self-regulation in early childhood: Implications for developmental psychopathology. Development and Psychopathology. 2015;27(02):397–409. doi: 10.1017/S095457941500005X. http://doi.org/10.1017/S095457941500005X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windham GC, Hopkins B, Fenster L, Swan SH. Prenatal active or passive tobacco smoke exposure and the risk of preterm delivery or low birth weight. Epidemiology (Cambridge, Mass.) 2000;11(4):427–433. doi: 10.1097/00001648-200007000-00011. [DOI] [PubMed] [Google Scholar]


