Abstract
[Purpose] The aim of this study was to determine the effects of central and unilateral posteroanterior (PA) mobilization on cervical lordosis, muscle stiffness and range of motion in a patient with ankylosing spondylitis (AS). [Subject and Methods] The subject of this case study was diagnosed with AS in 1997. At baseline, variance was measured without any intervention during the first 3 days (2016.6.13–2016.6.15). Cervical PA mobilization was applied to each segment from C2–C7 from the 4th to the 11th day for 8 days. Intervention was not performed from the 12th to the 15th days for 4 days. Variances were measured a final time without intervention on the 16th day (2016.6.28). [Results] Cervical lordosis was seen to have increased. Muscle stiffness was significantly decreased after intervention and the effect of treatment lasted for five days without any additional intervention. The cervical flexion and extension angles were increased. However these increases were not statistically significant. Both the lateral flexion and left rotation angle were significantly increased and the effects of treatment lasted for five days without any additional intervention. [Conclusion] These results suggest that central and unilateral PA mobilization is effective in increasing cervical lordosis and range of motion, and decreasing muscle stiffness in patients with AS.
Keywords: Ankylosing spondylitis, Posteroanterior mobilization, Cervical lordosis
INTRODUCTION
Ankylosing spondylitis (AS) is an inflammatory rheumatic disease that mainly affects the axial skeleton1). It is a chronic and systemic disease that is a type of sero negative spondyloarthopathy and is characterized by inflammation, especially in the spinal column2). AS may reduce spinal mobility and produce structural and functional impairments3). These restrictions can lead to a decreased daily activity level and diminished quality of life in patients with AS. Therefore, suppressing spinal inflammation and reducing pain and stiffness are major goals in the treatment and prevention of AS4). AS is prevalent in the men. Patient education, self-management techniques and orthopedic manual therapy are currently included as part of physical therapy for AS patients. Orthopedic manual therapy such as joint mobilization is particularly effective in improving the condition of patients with AS5).
Limitations of spinal mobility are produced by inflammation of the spinal joints in the early stage of AS2). Limitations of cervical movement are a characteristic feature of AS and cervical range of motion (ROM) is a fundamental component of the functional evaluation during physical therapy6, 7). Joint mobilization is known to increase cervical ROM8). Cervical joint mobilization contributes to reduction in pain and achieves vertebral palpation in patients with neck pain can increase joint mobility9,10,11). During AS treatment, appropriate application of force is necessary in the most inflammatory and painful phase of the disease, and grade III mobilization should be applied when inflammation subsided in order to prevent loss of joint mobility5). Maitland’s grade I & II mobilization can be performed primarily to decrease joint pain while grade III & IV mobilization can be used to increase joint ROM12). Maitland’s joint mobilization technique is normally used to treat neck pain, headaches and other neck problems. More specifically, pain localization and symptom reduction should be considered during the application of mobilization techniques. In addition, the vertebral level that is the most often subject to symptoms should be treated and the physiotherapists should perform passive joint mobilization of dysfunctional joints13, 14).
Recently, posteroanterior (PA) mobilization is being more widely used to assess and treat spinal segments. Physiotherapists usually use their thumbs or hands to apply pressure rhythmically to the vertebrae in a posterior-to-anterior direction15). PA mobilization that is applied manually is classified as central or unilateral PA, and stiffness is subjectively assessed16). PA mobilization enables physiotherapists evaluate a segment’s mobility, which is an indirect reflection of the integrity of periarticular structure (i.e., disc, capsule, or ligament)17).
Many studies have applied PA mobilization technique on the lumbar spine18,19,20). So far, however, there has been little discussion about PA mobilization of the cervical spine of AS patient. Therefore, this study investigated the effect of cervical central and unilateral PA mobilization such as its effects on cervical lordosis, muscle stiffness and ROM of the cervical vertebrae.
SUBJECT AND METHODS
This was a case study of a single patient with AS. The subject was a 57-year-old-man with a weight of 70 kg and a height of 160 cm. The subject was diagnosed with AS in 1997. The subject was determined to have grade V disability in 2003 and had a disease duration of at least ten years and limited spinal mobility. The subject agreed to participate in the study after receiving explanations regarding the purpose and procedures of the experiment. The subject signed an informed consent statement before participation. The protocol for this study was approved by the local ethics committee of Namseoul University in Cheonan, South Korea (1041479-201605-HR-032).
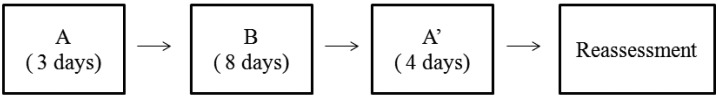
This was a single-case study with an ABA’ design (Fig. 1), where A and A’ were the baseline phases and B was the intervention phase. Times when intervention was not provided, were considered baseline phases in this study. The baseline phase occurred before or after an intervention phase. At baseline, variance was measured without any intervention during the first 3 days (2016.6.13–2016.6.15). The intervention was central and unilateral PA mobilization of the cervical vertebrae. Cervical PA mobilization was applied to each segment from C2–C7 from the 4th to the 11th day (2016.6.16–2016.6.23). It was administered once a day for 8 days. Intervention was not performed from the 12th to the 15th days for 4 days (2016.6.24–2016.6.27). Variances were measured a final time without intervention on the 16th day (2016.6.28).
Fig. 1.
Experimental flow chart
A=baseline 1 (no intervention, only assessment), B=intervention phase (intervention and assessment), A’=baseline 2 (no intervention and assessment)
Central and unilateral PA mobilization was applied to C2–C7, 20 times in each segment, with the patient in a prone position. Grade IV mobilization was applied by a physical therapist who had completed Maitland course 2b. Grade IV mobilization can be applied against tissue resistance at small amplitude to the restricted part of the joint.
Muscle stiffness and cervical ROM were measured once daily during the A and B phases as well as on the reassessment day. The A’ phase involved no intervention and occurred on the 12th to 15th days. After the A’ phase, muscle stiffness and cervical ROM were measured. The total period of this study was 16 days.
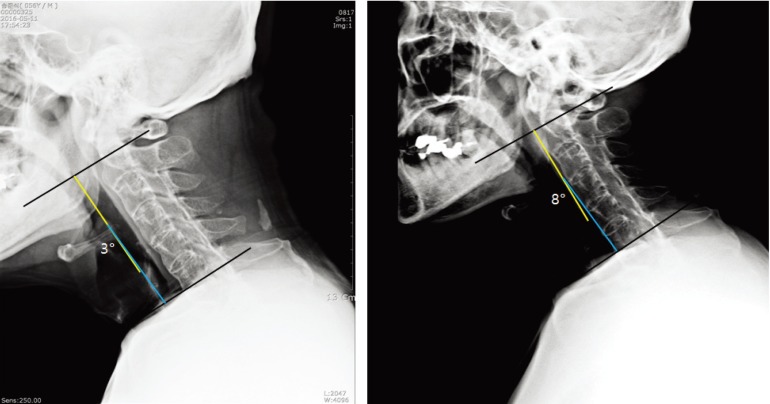
The patient’s cervical lordosis angle was measured with X-ray imaging before beginning treatment and after completing treatment. Cervical lordosis was measured identifying the horizontal surface of C1 and C7 and drawing a line perpendicular to each of those two horizontal lines. The angle formed by the two perpendicular lines was measured.
Muscle stiffness was measured with a Myoton®PRO (MyotonAS, Estonia) at 2 cm distance from the left side of the C4 spinous process. The device was positioned vertically on the skin marker with the patient in a relaxed condition in a prone position in order to measure stiffness. Stiffness was measured twice and the means values were analyzed. Cervical ROM measure, such as flexion, extension, lateral flexion and rotation were assessed with a Goniometer (EZ Read Jamar Goniometer, America). The measurement of ROM was conducted three times. The average value was used as the measured value. All data were encoded and analyzed using the SwingWin program. A χ2 test was used to compare differences before and after measurement. The statistical significance level was set at p<0.05.
RESULTS
Cervical lordosis, muscle stiffness and ROM were measured. The angle of cervical lordosis was increased from 3 to 8° after central and unilateral PA mobilization (Fig. 2). Muscle stiffness significantly decreased from 398.0 N/m to 321.5 N/m. The effect of treatment lasted for five days without any additional intervention. The cervical flexion increased from 12 to 16°, and the cervical extension increased from 8 to 10°. However, these increases were statistically non-significant. The left lateral flexion increased from 4 to t6°, and the right lateral flexion increased from 3.5 to 6°. Both the left and right lateral flexion angles significantly increased after the PA mobilization. This effect lasted for five days without any additional intervention. The left rotation increased from 25 to 32°, and the right lateral flexion increased from 26 to 32°. In terms of rotation angles, only the left rotation angles significantly increased after the PA mobilization and the effect of treatment lasted for five days without any additional intervention (Table 1).
Fig. 2.
Cervical lordosis on X-ray (left: baseline (1st day); right: 11th day)
Table 1. Change in cervical lordosis, muscle stiffness and ROM.
| Day | Baseline | Intervention | AI | χ 2 | df | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 16 | ||||
| CL (°) | 3.0 | 8.0 | |||||||||||||
| Stiffness (N/m) | 398.0 | 399.0 | 360.5 | 370.0 | 348.0 | 328.0 | 311.0 | 322.5 | 318.5 | 329.5 | 321.5 | 320.0 | 4.28 | 1 | 0.039* |
| Flex (°) | 12.0 | 12.0 | 13.0 | 14.0 | 15.0 | 14.0 | 15.0 | 16.0 | 16.0 | 17.0 | 16.0 | 16.0 | 1.64 | 1 | 0.201 |
| Ext (°) | 8.0 | 6.0 | 7.0 | 8.0 | 9.0 | 10.0 | 9.0 | 9.0 | 8.0 | 8.0 | 10.0 | 11.0 | 1.64 | 1 | 0.201 |
| Llf (°) | 4.0 | 3.0 | 5.0 | 4.0 | 5.0 | 5.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 6.0 | 4.28 | 1 | 0.039* |
| Rlf (°) | 3.5 | 3.0 | 4.0 | 4.0 | 5.0 | 5.0 | 5.0 | 6.0 | 6.0 | 6.0 | 6.0 | 5.0 | 4.28 | 1 | 0.039* |
| Lrot (°) | 25.0 | 22.0 | 19.0 | 19.0 | 21.0 | 26.0 | 28.0 | 29.0 | 32.0 | 32.0 | 32.0 | 32.0 | 4.28 | 1 | 0.039* |
| Rrot (°) | 26.0 | 26.0 | 22.0 | 27.0 | 28.0 | 29.0 | 30.0 | 30.0 | 32.0 | 32.0 | 32.0 | 35.0 | 1.93 | 1 | 0.165 |
ROM: range of motion; CL: cervical lordosis; AI: after intervention; Flex: flexion; Ext: extension; Llf: left lateral flexion; Rlf: right lateral flexion; Lrot: left rotation; Rrot: right rotation. *Significant difference between baseline and intervention
DISCUSSION
This study was a case study of a single patient with AS, and the aim of the study was to investigate the effect of central and unilateral PA mobilization of the cervical vertebrae. The study subject experienced a loss of function during the first 10 years of his disease. The loss of function was correlated with the occurrence of peripheral arthritis, spinal X-ray changes and development of a bamboo spine. After suffering from the disease for more than 20 years, more than 80% of AS patients experience daily pain and stiffness21).
In the present study, the cervical lordosis angle was increased from 3 to 8° following cervical central and unilateral PA. Cervical posture must be considered during a postural assessment. Specifically postural compensations are expected in adjant segments, considering that muscle chains are interconnected22). Power et al studied the effects of PA mobilization on lumbar segments and reported that PA spinal mobilization consistently produced lumbar extension18, 19). Application of PA force can cause motion of the target and neighboring vertebrae, and this motion is propagated cranially and caudally17). Application of PA force on the mid-lumbar vertebrae could produce extension at all lumbar segments, which can increase the degree of lumbar lordosis19). In the current results, cervical lordosis might have increased by a similar mechanism. Application of PA mobilization on one spinous process produced movements at the target vertebra and also caused movements of the entire cervical spine, resulting in increased cervical lordosis23).
In the present study, muscle stiffness decreased after intervention and the effect of the intervention was maintained for five days without any further treatment. Stiffness and loss of spinal mobility are characteristic symptoms of AS. These symptomes can be explained by spinal inflammation, structural damage, or both1). Stiffness has been related to pain, reduced voluntary movement, and abnormal spinal joint stiffness, which are major symptoms of AS4). Intervertebral mobilization has been recommended as a method for treating spinal stiffness17). Shum et al. has suggested that PA mobilization caused immediate desirable effects and reduced spinal stiffness24). These results suggest that PA mobilization is an effective rehabilitation method for reducing stiffness in AS patients.
AS is regarded as a chronic progressive disease leading to a variable degree of restricted mobility of the spine with loss of activity of daily living (ADL)21). The assessment of spinal mobility in AS patients is important as it indicates the structural damage. For this reason, mobility evaluation is include in all the recommendation of disease assessment and follow-up25). In this study, cervical mobility was assessed with a Goniometer. The patient’s cervical flexion and extension angles increased, however, the increases were statistically non-significant. The left and right lateral flexion and the left rotation angles significantly increased. Therefore, central and unilateral PA mobilization is considered to have a positive effect on lateral flexion and rotation. AS patients have limitations in all movements, particularly movement related to the lateral flexion6). Cervical flexion and extension principally occur at the atlanto-occipital joints. Rotation occurs at the atlanto-axial joint while cervical lateral movements occur from C2–C7. Application of PA force produced an extension movement leading to backwards bending of the cervical spine. The extension movement is generally observed at the upper cervical segments23), lending further support to the findings of this study. In this study, the cervical extension increase was not statistically significant. However, the value of the cervical extension was increased.
In conclusion, central and unilateral PA mobilization positively affected cervical lordosis, muscle stiffness and cervical ROM in an AS patient. Therefore, this study suggest that PA mobilization can be used to improve the musculoskeletal condition of patients with AS although only one subject participated in this study.
Acknowledgments
This article was funded by the International University of Korea.
REFERENCES
- 1.Braun J, Sieper J: Ankylosing spondylitis. Lancet, 2007, 369: 1379–1390. [DOI] [PubMed] [Google Scholar]
- 2.Ince G, Sarpel T, Durgun B, et al. : Effects of a multimodal exercise program for people with ankylosing spondylitis. Phys Ther, 2006, 86: 924–935. [PubMed] [Google Scholar]
- 3.Halvorsen S, Vøllestad NK, Fongen C, et al. : Physical fitness in patients with ankylosing spondylitis: comparison with population controls. Phys Ther, 2012, 92: 298–309. [DOI] [PubMed] [Google Scholar]
- 4.Braun J, Brandt J, Listing J, et al. : Treatment of active ankylosing spondylitis with infliximab: a randomised controlled multicentre trial. Lancet, 2002, 359: 1187–1193. [DOI] [PubMed] [Google Scholar]
- 5.Tricás-Moreno JM, Lucha-López MO, Lucha-López AC, et al. : Optimizing physical therapy for ankylosing spondylitis: a case study in a young football player. J Phys Ther Sci, 2016, 28: 1392–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Driscoll SL, Jayson MI, Baddeley H: Neck movements in ankylosing spondylitis and their responses to physiotherapy. Ann Rheum Dis, 1978, 37: 64–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Florêncio LL, Pereira PA, Silva ER, et al. : Agreement and reliability of two non-invasive methods for assessing cervical range of motion among young adults. Rev Bras Fisioter, 2010, 14: 175–181. [PubMed] [Google Scholar]
- 8.Gong W, Bo GH, Lee Y: Treatment of active ankylosing spondylitis with infliximab: a randomised controlled multicentre trial. J Phys Ther Sci, 2011, 23: 531–534. [Google Scholar]
- 9.Aquino RL, Caires PM, Furtado FC, et al. : Applying joint mobilization at different cervical vertebral levels does not influence immediate pain reduction in patients with chronic neck pain: a randomized clinical trial. J Manual Manip Ther, 2009, 17: 95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.López CC, Barra ME, Villar E: Effectiveness of the posteroanterior mobilization in the lumbar raquis with the Kaltenborn wedge in chronic low back pain patients. Fisioterapia, 2007, 29: 261–269. [Google Scholar]
- 11.McNair PJ, Portero P, Chiquet C, et al. : Acute neck pain: cervical spine range of motion and position sense prior to and after joint mobilization. Man Ther, 2007, 12: 390–394. [DOI] [PubMed] [Google Scholar]
- 12.Landrum EL, Kelln CB, Parente WR, et al. : Immediate effects of anterior-to-posterior talocrural joint mobilization after prolonged ankle immobilization: a preliminary study. J Manual Manip Ther, 2008, 16: 100–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maitland G, Hengeveld E, Banks K: Maitalnd’s Vertebral Manipulation, 6th ed. Woburn: Butterworth Heinemann, 2001. [Google Scholar]
- 14.Maitland G, Banks K, English K, et al. (ed.): Maitland’’s Vertebral Manipulation, 7th ed. Oxford: Butterworth Heineman, 2005. [Google Scholar]
- 15.Reid SA, Rivett DA, Katekar MG, et al. : Efficacy of manual therapy treatments for people with cervicogenic dizziness and pain: protocol of a randomised controlled trial. BMC Musculoskelet Disord, 2012, 13: 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Björnsdóttir SV, Guðmundsson G, Auðunsson GA, et al. : Posterior-anterior (PA) pressure Puffin for measuring and treating spinal stiffness: Mechanism and repeatability. Man Ther, 2016, 22: 72–79. [DOI] [PubMed] [Google Scholar]
- 17.Kulig K, Landel R, Powers CM: Assessment of lumbar spine kinematics using dynamic MRI: a proposed mechanism of sagittal plane motion induced by manual posterior-to-anterior mobilization. J Orthop Sports Phys Ther, 2004, 34: 57–64. [DOI] [PubMed] [Google Scholar]
- 18.Powers CM, Beneck GJ, Kulig K, et al. : Effects of a single session of posterior-to-anterior spinal mobilization and press-up exercise on pain response and lumbar spine extension in people with nonspecific low back pain. Phys Ther, 2008, 88: 485–493. [DOI] [PubMed] [Google Scholar]
- 19.Powers CM, Kulig K, Harrison J, et al. : Segmental mobility of the lumbar spine during a posterior to anterior mobilization: assessment using dynamic MRI. Clin Biomech (Bristol, Avon), 2003, 18: 80–83. [DOI] [PubMed] [Google Scholar]
- 20.Maher C, Adams R: Reliability of pain and stiffness assessments in clinical manual lumbar spine examination. Phys Ther, 1994, 74: 801–809, discussion 809–811. [DOI] [PubMed] [Google Scholar]
- 21.Gran JT, Skomsvoll JF: The outcome of ankylosing spondylitis: a study of 100 patients. Br J Rheumatol, 1997, 36: 766–771. [DOI] [PubMed] [Google Scholar]
- 22.Chaves TC, Turci AM, Pinheiro CF, et al. : Static body postural misalignment in individuals with temporomandibular disorders: a systematic review. Braz J Phys Ther, 2014, 18: 481–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee RY, McGregor AH, Bull AM, et al. : Dynamic response of the cervical spine to posteroanterior mobilisation. Clin Biomech (Bristol, Avon), 2005, 20: 228–231. [DOI] [PubMed] [Google Scholar]
- 24.Shum GL, Tsung BY, Lee RY: The immediate effect of posteroanterior mobilization on reducing back pain and the stiffness of the lumbar spine. Arch Phys Med Rehabil, 2013, 94: 673–679. [DOI] [PubMed] [Google Scholar]
- 25.Garrido-Castro JL, Medina-Carnicer R, Schiottis R, et al. : Assessment of spinal mobility in ankylosing spondylitis using a video-based motion capture system. Man Ther, 2012, 17: 422–426. [DOI] [PubMed] [Google Scholar]