Abstract
The L-type calcium channels (LTCCs) Cav1.2 and Cav1.3, encoded by the CACNA1C and CACNA1D genes, respectively, are important regulators of calcium influx into cells and are critical for normal brain development and plasticity. In humans, CACNA1C has emerged as one of the most widely reproduced and prominent candidate risk genes for a range of neuropsychiatric disorders, including bipolar disorder (BD), schizophrenia (SCZ), major depressive disorder, autism spectrum disorder, and attention deficit hyperactivity disorder. Separately, CACNA1D has been found to be associated with BD and autism spectrum disorder, as well as cocaine dependence, a comorbid feature associated with psychiatric disorders. Despite growing evidence of a significant link between CACNA1C and CACNA1D and psychiatric disorders, our understanding of the biological mechanisms by which these LTCCs mediate neuropsychiatric-associated endophenotypes, many of which are shared across the different disorders, remains rudimentary. Clinical studies with LTCC blockers testing their efficacy to alleviate symptoms associated with BD, SCZ, and drug dependence have provided mixed results, underscoring the importance of further exploring the neurobiological consequences of dysregulated Cav1.2 and Cav1.3. Here, we provide a review of clinical studies that have evaluated LTCC blockers for BD, SCZ, and drug dependence-associated symptoms, as well as rodent studies that have identified Cav1.2- and Cav1.3-specific molecular and cellular cascades that underlie mood (anxiety, depression), social behavior, cognition, and addiction.
Electronic supplementary material
The online version of this article (doi:10.1007/s13311-017-0532-0) contains supplementary material, which is available to authorized users.
Keywords: Cav1.2, Cav1.3, CACNA1C, CACNA1D, Mood, Social, Addiction
Introduction
Over the last 2 decades, work from multiple laboratories has established that Cav1.2 and Cav1.3 L-type calcium channels (LTCCs) are critical mediators of experience-dependent plasticity in the brain. More recently these channels have been identified to be key for various neuronal processes that are essential for normal brain development, connectivity, and function [1–3]. This is further underscored by the discovery of neuropsychiatric risk genetic variants in CACNA1C, which codes for the Cav1.2 α1 subunit of LTCCs [4, 5], and CACNA1D, which codes for the Cav1.3 α1 subunit [6, 7]. These variants can alter levels and function of the channels with consequences on neural processing and connectivity as revealed by human imaging studies [1, 8, 9].
The LTCCs belong to the family of voltage-gated Ca2+ channels, with Cav1.2 and Cav1.3 being the primary LTCC subunits expressed in the brain [10]. Although there is considerable overlap in their expression pattern, as revealed by in situ hybridization (Table 1), Fos expression, a measure of neuronal activity [21], and studies with genetic mutant mice ([1, 2] and as discussed below) have revealed differential contributions of these isoforms to neuronal function and behavior. These LTCC isoforms are present as heteromeric complexes with Cav1 encoding the α1 pore-forming subunit that determines the physiological and pharmacological properties of these channels [2, 22]. The Cav1.2 and Cav1.3 subunits share a high degree of sequence and structural similarity resulting in lack of selectivity of LTCC pharmacological activators and blockers [2]. However, as we now know, Cav1.2 and Cav1.3 have different physiological characteristics [23–25] and associate with different proteins to form unique subunit-specific signaling complexes at the neuronal membrane [26–28], resulting in differential contributions to neuronal function and neuropathology underlying disease.
Table 1.
Cav1.2 and Cav1.3 mRNA expression within mesocorticolimbic brain regions in rodents
| Brain region | Cav1.2 mRNA | Cav1.3 mRNA | Reference |
|---|---|---|---|
| Hippocampus | [11] | ||
| CA1 | * | ** | |
| CA2 | *** | ** | |
| CA3 | *** | ** | |
| Dentate gyrus | *** | *** | |
| Hippocampus | [12] | ||
| Dentate gyrus | ** | ** | |
| Amygdala | * | * | |
| Hippocampus | [13] | ||
| CA1 | NR | ** | |
| CA3 | NR | ** | |
| Dentate gyrus | NR | *** | |
| Hippocampus | [14] | ||
| Dentate gyrus | *** | NR | |
| Amygdala | ** | NR | |
| VTA | * | *** | [15] |
| NAc | |||
| Core | * | ** | |
| Shell | ** | *** | |
| Hippocampus | [16] | ||
| CA | *** | *** | |
| Dentate gyrus | *** | *** | |
| VTA | * | * | |
| PFC | ** | ** | |
| Hippocampus | [17] | ||
| CA1 | ** | * | |
| CA3 | *** | * | |
| Dentate gyrus | *** | * | |
| Amygdala | |||
| BLA | ** | * | |
| Hippocampus | [18] | ||
| CA1 | * | ** | |
| CA3 | *** | ** | |
| Dentate gyrus | *** | *** | |
| Hippocampus | [19] | ||
| Hippocampal formation | *** | NR | |
| Hippocampus | [20] | ||
| CA1 | ** | ** | |
| CA3 | ** | ** | |
| Dentate gyrus | ** | *** | |
| Amygdala | |||
| CeA | * | ** | |
| MeA | * | ** | |
| BLA | * | ** | |
| NAc | |||
| Core | * | * | |
| Shell | ** | ** | |
| PFC | |||
| Cing | * | ** | |
| PreL | * | ** | |
| IL | * | ** | |
| OFC | * | ** | |
Comparison of Cav1.2 and Cav1.3 mRNA levels are made within and across brain regions for each study and not across different studies
NR = not reported; VTA = ventral tegmental area; NAc = nucleus accumbens; CA = hippocampal comus ammon regions CA1, CA2, and CA3; PFC = prefrontal cortex; BLA = basolateral amygdala; CeA = central amygdala; MeA = medial amygdala; Cing = cingulate cortex; PreL = prelimbic cortex; IL = infralimbic cortex; OFC = orbitofrontal cortex
*Low expression, **moderate, or ***strong expression
In this review we will first provide an overview of CACNA1C and CACNA1D genetic risk variants linked to neuropsychiatric disorders. As recent genetic findings have raised great interest in targeting LTCCs as a potential strategy for the treatment of neuropsychiatric disorders and drug dependence, as well as repurposing current clinically used LTCC medications [2, 6, 29, 30], we will next review clinical studies performed to date with LTCC blockers. We will then provide an overview of our current knowledge of the brain-region-specific contribution of Cav1.2 and Cav1.3 channels to neural and molecular mechanisms underlying the pathophysiology of neuropsychiatric and neurodevelopmental-associated behavioral endophenotypes, obtained using preclinical animal models (Fig. 1). Given the complex nature of neuropsychiatric disorders, we believe that understanding biological phenotypes in the context of behavioral endophenotypes, will greatly help both in better understanding neuropathology, as well as provide a framework for exploring new therapeutic targets for CACNA1C- and CACNA1D-associated disorders.
Fig. 1.
Cav1.2- and Cav1.3-mediated anatomical and molecular pathways underlying the endophenotypes associated with neuropsychiatric disorders. Solid lines indicate pathways that have been identified for the respective behavioral endophenotypes and dotted lines indicate potential pathways that may be recruited AMPAR = α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors; PFC = prefrontal cortex; HPC = hippocampus; NAc = nucleus accumbens; VTA = ventral tegmental area; REDD1 = regulated in development and DNA damage response 1; CP-AMPAR = Ca2+-permeable AMPAR; ERK2 = extracellular regulated kinase 2; CaMKII = CaM-dependent protein kinase II
Functional Impact of CACNA1C and CACNA1D Genetic Risk Variants
As recently reviewed in detail in Heyes et al. [5], genome-wide association studies have identified multiple single nucleotide polymorphisms (SNPs) in CACNA1C to be significantly associated with bipolar disorder (BD) [31] and schizophrenia (SCZ) [32]. Additionally, risk SNPs within CACNA1C have also been linked to major depressive disorder (MDD) [33], autism spectrum disorder (ASD) [34], and attention deficit hyperactivity disorder (ADHD) [35]. Furthermore, a meta-analysis study has linked disease-associated CACNA1C SNPs to all the abovementioned 5 disorders [35]. The majority of these SNPs are present in the intronic, 5' or 3' untranslated regions of CACNA1C [4, 5], in accordance with the growing body of literature establishing that large numbers of SNPs associated with complex diseases such as neuropsychiatric disorders, are present within noncoding regions [36]. Most of the CACNA1C risk SNPs associated with SCZ and BP, particularly SNP rs1006737 and those in linkage disequilibrium, are present in a large intron between exons 3 and 4 [5]. Functional studies to evaluate the impact of risk SNPs on gene expression are beginning to establish that these SNPs lie within regions that are under tight transcriptional control, with risk SNPs being able to alter gene expression by differentially binding nuclear proteins and also altering long-range intronic enhancer and promoter interactions within CACNA1C [37, 38]. Biological studies to measure levels of CACNA1C have found both increased [38–40] and decreased [37, 38, 40, 41] expression of CACNA1C, depending on the brain region and cellular system examined. This suggests that transcriptional control of CACNA1C is highly complex and most likely, differentially controlled at the level of brain region and cell type. Nevertheless, these studies demonstrate that intronic CACNA1C risk SNPs can alter levels of CACNA1C and that loss or gain of Cav1.2 can contribute to disease symptoms.
In addition to the noncoding variants, 2 truncating mutations in CACNA1C have been identified in a whole-exome sequencing study of SCZ that are predicted to cause loss of function [42], though this remains to be confirmed. As discussed in Heyes et al. [5], these truncation mutations in CACNA1C could exert a dominant negative effect through the interaction of truncated mutant proteins with the Cav1.2 channel, as has been reported for other voltage-gated subunits [43–45].
A coding CACNA1C variant has also been linked to ASD. A gain-of-function mutation in Cav1.2 causes Timothy syndrome (TS), an autosomal dominant developmental disorder [46]. This syndrome is a multiorgan disorder associated with malformations, cardiac symptoms (long QT), and neurological developmental defects [46–48], including manifestation of neuropsychiatric phenotypes [48]. The mutation in Cav1.2 that causes TS is a sporadic, dominant glycine-to-arginine mutation that is located at position 406 (G406R) in a mutually exclusive, alternatively spliced exon 8 or 8A of CACNA1C [46]. G406R in exon 8a causes TS1 and G406R or G402S in exon 8 causes a rare variant of TS, namely TS2 [46, 48]. TS1 has been associated with ASD [46, 48], whereas patients with TS2 additionally manifest with neuropsychiatric conditions [41, 48]. One patient with TS2 was reported to exhibit obsessive compulsive disorder and depression [48], while another patient with TS2 who carried the G402S mutation developed BD in adulthood [41].
Similar to CACNA1C, genetic variants in CACNA1D have also been identified in neuropsychiatric disorders. A SNP in CACNA1D (rs893363), which codes for Cav1.3, has been associated in the 5-disorder gene analysis, including BD, SCZ, ADHD, MDD, and ASD [35]. Separately noncoding variants [31] and 2 coding variants (A1751P and R1771W) have been linked to BD [49]. However, a study in the Han Chinese population found no significant SNPs in CACNA1D associated with SCZ [50]. SNPs in CACNA1D have also been associated with cocaine dependence [51]. Furthermore, whole-exome sequencing studies have identified 2 de novo mutations (p.A749G and p.G407R) in CACNA1D in patients with sporadic autism and intellectual disability [52, 53]. Functional studies have identified these mutations as gain-of-function of Cav1.3 LTCCs [7, 54].
Thus, based on the above findings on the impact of CACNA1C and CACNA1D disease-associated genetic variants on gene expression and channel function, the available data suggest that higher or lower levels of Ca2+ influx in neurons can be detrimental. In addition, LTCCs can also regulate neuronal firing. For example, LTCCs can directly provide a depolarizing stimulus; this can stabilize upstates/plateau potentials (e.g. [55]), thus affecting neuronal firing. LTCCs can also couple to Ca2+-activated K channels [56, 57], thus moderating neuronal firing. Therefore, decreased LTCC activity could actually increase firing in some neurons, which may trigger Ca2+ influx through other sources (other voltage-gated Ca2+ channels subtypes or glutamate N-methyl-D-aspartate receptors). Similarly, increase in LTCC activity as a result of gain of LTCC function could silence neurons. Thus, altered Cav1.2 and Cav1.3 LTCC levels or activity, in a cell-type-specific manner, can affect neuronal function in multiple ways that could negatively affect brain function and contribute to neuropsychiatric symptoms in disorders associated with CACNA1C and CACNA1D.
Targeting L-Type Calcium Channels in the Treatment of Neuropsychiatric Disorders and Drug Dependence
LTCC blockers have been used clinically for several decades in the treatment of cardiac conditions such as hypertension, arrhythmias, and cardiac ischemia [2]. Recently, with growing evidence of the association between LTCC genes and neuropsychiatric disorders [5], there has been increased interest in repurposing these drugs for the treatment of neuropsychiatric conditions and drug dependence [6, 29]. Since the 1980s several clinical studies have examined the efficacy of LTCC blockers using the 3 classes of LTCC pharmacological blockers—dihydropyridines (DHPs; nifedipine, amlodipine, felodipine, isradipine, nicardipine, nisoldipine, and nimodipine); phenylalkylamines (verapamil); and benzothiazepines (diltiazem)—to alleviate symptoms in patients presenting with neuropsychiatric conditions and drug dependence. Below, we review the findings of these studies (see Table 2). Of note, many of these clinical studies have utilized high systemic doses of LTCC blockers, particularly the DHPs and thus could have significant confounding effects on behavior, as demonstrated by rodent studies [105, 106]. Additionally, several of these studies have used the phenylalkylamine blocker, verapamil (Table 2). In addition to verapamil’s nonspecific effects such as blocking other Ca2+ channels [107], potassium channels [108–110], and α-adrenergic receptors [111], studies examining how well verapamil enters the brain in humans have been sparse. Verapamil is a substrate for P-glycoprotein (P-gp) substrate, an efflux transporter found in several organs, including the blood–brain barrier, where it plays an important role for the entry of drugs, including verapamil, into the brain [112]. Verapamil can function as a stimulator of the P-gp activity at low concentrations, preventing brain entry, whereas at high concentrations it acts as an inhibitor of P-gp, allowing brain entry [113, 114]. However, verapamil at high concentrations, although capable of penetrating the blood–brain barrier, can have toxics effects [115].
Table 2.
Type of clinical study using L-type calcium channel blockers in neuropsychiatric disease
| Neuropsychiatric disease treated | L-type calcium channel blocker used | Type of clinical study performed | Reference(s) |
|---|---|---|---|
| Bipolar disorder | Verapamil | Nonrandomized | [58–61] |
| Randomized; patients received either verapamil or lithium and efficacy compared | [62] | ||
| Randomized: crossover study; patients received either verapamil or lithium and then treatment switched | [63] | ||
| Case report | [64–67] | ||
| Randomized placebo-controlled within subject | [68] | ||
| Nonrandomized placebo within subjects | [69] | ||
| Randomized: phase I—lithium, phase II—nonresponders (verapamil or lithium); phase III—nonresponders (combined verapamil/lithium) |
[70] | ||
| Randomized placebo | [71, 72] | ||
| Randomized; patients received verapamil or the antihypertensive drug atenolol and efficacy compared | [73] | ||
| Nimodipine | Randomized placebo-controlled within-subjects | [74] | |
| Nonrandomized placebo within-subject | [75] | ||
| Nonrandomized | [76] | ||
| Case report | [77, 78] | ||
| Diltiazem | Nonrandomized | [79, 80] | |
| Nifedipine | Case report | [81] | |
| Schizophrenia | Verapamil | Case report | [82] |
| Randomized placebo | [83, 84] | ||
| Randomized placebo-controlled within subject | [85] | ||
| Nonrandomized | [86] | ||
| Nonrandomized placebo within subject | [87, 88] | ||
| Nifedipine | Nonrandomized | [89] | |
| Randomized placebo | [90] | ||
| Cocaine dependence | Nimodipine | Randomized placebo-controlled within subject | [91] |
| Isradipine | Randomized placebo-controlled within subject | [92, 93] | |
| Nimodipine | Randomized placebo | [94] | |
| Nifedipine | Randomized placebo-controlled within subject | [95] | |
| Amlodipine | Nonrandomized | [96] | |
| Isradipine | Randomized placebo-controlled within subject | [97] | |
| Morphine dependence | Verapamil | Randomized placebo | [98] |
| Diltiazem, verapamil, nimodipine | Randomized placebo-controlled within subject | [99] | |
| Nifedipine | Randomized; patients received nifedipine or the α-adrenoceptor blocker, clonidine; only nifedipine effects reported | [100] | |
| Alcohol dependence | Verapamil, nimodipine | Randomized placebo | [101] |
| Isradipine | Quasirandom placebo within subject; patients received 9 different combinations of ethanol or isradipine at different doses; only the first and second treatment was not randomly given | [102] | |
| Verapamil, nifedipine | Randomized placebo-controlled within subject | [103] | |
| Nimodipine | Nonrandomized | [104] |
BD
The efficacy of the LTCC blocker verapamil in alleviating acute mania observed in BD has been explored in several studies [116]. While some studies report a significant decrease in the severity of mania in patients with BD or manic patients [58, 59, 62–66, 68, 69], several others report no antimanic effects when verapamil was administered as a monotherapy [60, 61, 70–72]. However, when verapamil was administered in combination with the mood stabilizer lithium to patients with BD who were unresponsive to lithium [70] or in conjunction with the antipsychotic medication chlorpromazine [60] there was significant improvement in manic symptoms. This suggests that verapamil could have some potential for maintenance therapy of mania but only when administered in combination with other drugs. In addition to these findings, verapamil was found to improve significantly major psychotic depressive symptoms in 1 patient [67] and improve depressive symptom scores in patients prescribed verapamil for hypertension [73].
Although there are only a handful of studies with nimodipine and diltiazem, the findings are more consistent, though not as thoroughly investigated as verapamil. Bipolar manic patients treated with nimodipine either as a monotherapy [74–76] or in combination with lithium [77] or the antiseizure medication carbamazepine [74] showed significant improvements. Similar improvements in mood were reported when an adolescent with refractory, ultradian rapid cycling BD was treated with nimodipine [78]. Likewise, both bipolar manic patients [79] and treatment-resistant bipolar patients [80] treated with diltiazem had significantly decreased manic symptoms. However, in patients with no prior psychiatric history, the use of nifedipine to treat angina was associated with the onset of depression [81].
SCZ
Verapamil has also been tested in patients with SCZ. In patients with acute SCZ, verapamil treatment when administered as a monotherapy resulted in a significant decrease in psychotic symptoms [82]. These findings were confirmed in a separate study that reported a similar small, but significant, attenuation of psychotic symptoms with verapamil [83]. Similarly, patients with chronic SCZ treated with verapamil for 28 days displayed significant improvements in positive and negative symptoms, as well as in anxiety and depression [86]. In contrast to these findings, other studies have reported an increase in paranoia in verapamil-treated patients with chronic schizophrenia who were recently withdrawn from neuroleptics [87], or no effect on the psychological state [88] and negative symptoms [84]. Similar to the results with verapamil, the effects of nifedipine on alleviating the psychotic symptoms are conflicting. While some studies showed that patients with chronic schizophrenia receiving nifedipine showed an improvement on the Dementia Scale [85] and the Brief Psychiatric Rating Scale [89], another showed no improvements based on the Psychiatric Symptom Assessment Scale ratings [90].
Cocaine Dependence
Evidence from rodent studies has identified an important role of LTCCs in multiple aspects of cocaine addiction, making these channels a potential target for the treatment of addiction. Over the last few decades, clinical studies have tested the efficacy of LTCC blockers on the subjective effects of cocaine, though the results have been mixed. While some studies report no effect with isradipine and nimodipine [91, 92], others have reported a reduction in the subjective response to cocaine with nifedipine [95]. In contrast, a recent study reported enhanced subjective effects with isradipine [93]. The effects of LTCCs have also been tested on cocaine craving, the primary cause of relapse to cocaine use, with nimodipine [94], amlodipine [96], and isradipine [97] reducing cocaine craving.
Morphine Dependence
The impact of LTCC blockers on the subjective effects of morphine are mixed. While 1 study reported a reduction in the subjective effect of morphine with verapamil [98], another study showed no influence of nimodipine, verapamil, and diltiazem on counteracting morphine’s subjective effects in healthy humans [99]. Separately, it has been reported that nifedipine treatment caused confusion in individuals that were in morphine withdrawal [100]. These studies suggest that LTCC blockers may show selective effects in morphine-dependent individuals, having beneficial effects in some but detrimental effects in others.
Alcohol Dependence
With ethanol, LTCC blockers nimodipine and verapamil have been reported to have no effect on the subjective and psychomotor effects of the drug [101]. Similarly, isradipine had no effect on ethanol’s acute effects on poor psychomotor performance [102], and failed to antagonize ethanol intoxication [103]. However, nimodipine has been found to be effective for the treatment of ethanol’s withdrawal symptoms [104].
The discrepancies in the effects of LTCC blockers in the treatment of psychiatric disorder-associated symptoms and on the symptoms associated with drug dependence, as reviewed above, may be a consequence of a myriad of factors, including the high doses used; however, it highlights the complexity of neuropsychiatric disorders, as well as how dysregulated LTCCs may influence different psychiatric symptoms. Given our current knowledge of the varying impact of disease-risk variants to CACNA1C and CACNA1D levels (increase or decrease) and Cav1.2 and Cav1.3 function (gain or loss), it is not surprising that LTCC blockers may be efficacious in some individuals but not all and for some symptoms and not all those seen in CACNA1C and CACNA1D-linked neuropsychiatric conditions. Thus, understanding how Cav1.2 and Cav1.3 channel mechanisms contribute to neuropsychiatric-related symptoms can be greatly helpful. As progress on the development of new therapeutics for psychiatric disorders has been slow, understanding biological pathways in the context of disease symtoms (e.g., anxiety, social, depression, cognition) are key in identifying new targets for developing medications. We believe that this is particularly important given the complex nature of neuropsychiatric disorders versus the idea that they are sole entities as previously considered.
L-Type Calcium Channel Signaling in Neurons and Relevance to Neuropsychiatric Disorders
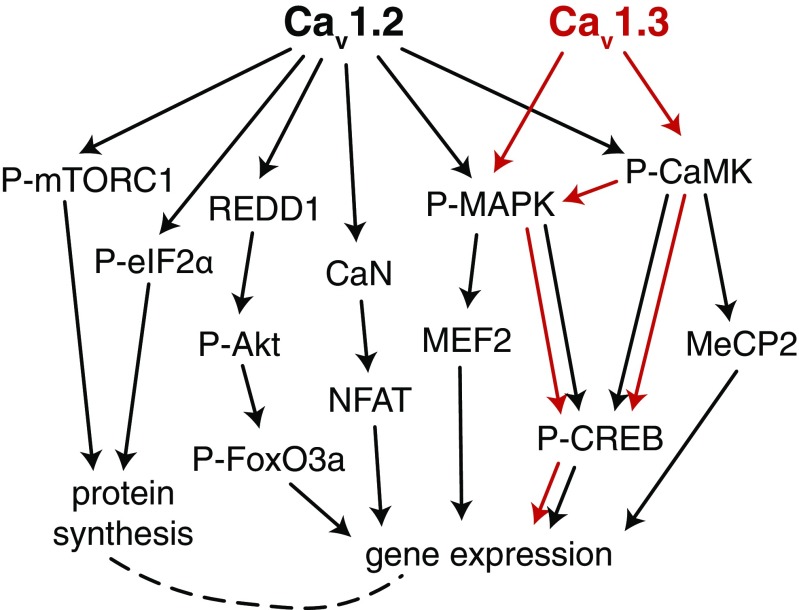
Several lines of evidence from both human and animal studies have unequivocally established a critical contribution of Ca2+ signaling pathways to the pathophysiology of both neuropsychiatric and neurodevelopmental disorder [1, 6, 117]. Cav1.2 and Cav1.3 channels are key mediators of Ca2+ signaling in neurons [26]. In vitro studies have established that depolarization-induced increase in local Ca2+ activates the calcium sensor calmodulin (CaM) at the synapse that subsequently activates a series of Ca2+/CaM-dependent protein kinases (CaMKs) [118–122] and also the Ras/mitogen-activated protein kinase (MAPK) pathway [123–125], both of which transduce molecular cascades to the nucleus, activating gene expression via the extensively studied transcriptional factor cAMP response element-binding protein (CREB) (Fig. 2). CREB-activated genes are critically involved in synaptic, neuronal, and behavioral plasticity [126–130]. LTCC-induced kinase pathways are also recruited for phosphorylation of signaling molecules that activate other transcription regulators, including myocyte enhancer factor-2 [131–134] and MeCP2 (Fig. 2), key factors involved in neuronal development, behavioral alterations, and neurodevelopmental disorders. In addition to activation of the kinase pathways, LTCCs can also activate the phosphatase pathway that likewise modulates transcription factor function. This includes the nuclear factor of activated T cells (NFAT) family of transcription factors that is regulated by the LTCC-activated Ca2+–calmodulin-dependent phosphatase calcineurin that dephosphorylates NFAT cytoplasmic 3 [135] and NFAT cytoplasmic 4 [136], inducing its translocation from the cytoplasm to the nucleus to regulate gene expression. Alteration of myocyte enhancer factor-2 and NFAT, as well as CREB signaling networks, has been linked to dendritic retraction as a consequence of elevated Ca2+ in induced pluripotent cells from patients with TS [132].
Fig. 2.
Cav1.2 and Cav1.3 signaling mechanisms. Solid lines indicate pathways that have been directly linked to Cav1.2 or Cav1.3 channels and dotted line indicates potential pathway that may be recruited. Black arrows indicate Cav1.2-specific pathways; red arrows indicate Cav1.3-specific pathways. mTORC1 = mammalian target of rapamycin complex 1; REDD1 = regulated in development and DNA damage response 1; P-MAPK = phosphorylated mitogen-activated protein kinase; P-CaMK = phosphorylated CAM-dependent protein kinase; P-eIF2α = phosphorylated eukaryotic initiation factor 2 alpha; CaN = calcineurin; P-Akt = phosphorylated protein kinase B; MEF2 = myocyte enhancer factor 2; NFAT = nuclear factor of activated T cells; P-CREB = phosphorylated cAMP response element-binding protein
The significance of these LTCC-activated pathways to neuropsychiatric disease pathology is underscored by several pathway network analyses that have repeatedly identified significant association of the calcium signaling pathway to BD [137, 138], SCZ [138, 139], MDD [138], and ASD [140], highlighting the calcium pathway as a common dysregulated mechanism underlying the etiology of these disorders. This has also been observed using proteomic approaches with postsynaptic density fractions from the cortex of patients with SCZ [141] and BD [142] that have identified altered levels of proteins that are mediators of calcium signaling. Additionally, pathway analyses have identified significant enrichment of the MAPK/extracellular regulated kinase (ERK) pathway in ASD [140, 143], SCZ [141], and depression [144], and whole-exome sequencing has found rare and likely protein-damaging mutations in members of the MAPK/ ERK and CREB-regulated intracellular signaling pathways in patients with BD [145]. Another pathway enriched in the proteomics-based pathway analysis from the postsynaptic density of patients with BD was the eukaryotic initiation factor 2α (eIF2α) signaling pathway [142], which is involved in mRNA translation [146] and a pathway we review below as a new candidate pathway linked to behavioral deficits in Cav1.2-deficient mice. In light of these findings, it is evident that dysregulation in LTCC and Ca2+ signaling can result in neuronal alterations that contribute to the pathogenesis of neuropsychiatric-related cellular [51, 147–150], physiological, synaptic [150, 151], and behavioral phenotypes [51, 150, 152, 153], all of which we discuss below.
L-Type Ca2+ Channels and Neuropsychiatric-Related Phenotypes: Preclinical Animal Studies
Rodents have proved to be a useful tool to study human disease-related behavioral symptoms. Given the predominance of noncoding variants in CACNA1C that are predicted to affect transcriptional control and result in lower or higher levels of CACNA1C, studying gene knockout and overexpressing mice can be highly useful. Similarly, mice harboring coding mutations that cause either loss or gain of function can be informative. The Cav1.2 and Cav1.3 LTCC isoforms have structural similarities making them both equally sensitive to LTCC pharmacological agents [154], posing a challenge to study isoform-specific brain and behavioral alterations. To overcome this, several different laboratories have developed genetic mutant mouse models that have altered expression or function of either Cav1.2 or Cav1.3. The most common models used to study Cav1.2-specific mechanisms have been the heterozygous constitutive knockout mouse model (homozygous is embryonic lethal [155]), and temporal, spatial, and cell-type-specific conditional mouse models with restricted knockdown of cacna1c (encoding Cav1.2) in the brain using Cre-recombinase specific drivers (mouse lines and viral vectors). Constitutive Cav1.2 heterozygous knockout mice develop a cardiac phenotype, particularly following stress [156]; however, it is unlikely that this cardiac phenotype affects brain phenotypes at baseline [153, 157] or following stress [158]. For Cav1.3 studies, there exists the Cav1.3 knockout mouse, though because of the high expression of Cav1.3 in the hair cells of the ear are deaf and limit their use for behavioral studies. To overcome this and the lack of subunit-specific pharmacological agents, the Striessnig laboratory developed a Cav1.2 DHP-insensitive (Cav1.2DHP–/–) mouse that harbors a single point mutation in the Cav1.2α1 subunit at the DHP binding site, rendering Cav1.2 channels insensitive to DHPs [159], allowing the specific pharmacological manipulation of Cav1.3 channels [21, 51, 159–161]. Below we review studies that have utilized these preclinical mouse models to examine behavioral and molecular phenotypes related to neuropsychiatric disorders.
Cav1.2 Channel Mechanisms and Neuropsychiatric-Related Endophenotypes
Anxiety
Symptoms of anxiety are one of the most prevalent endophenotypes of psychiatric disorders [162]. In mice with a 50% reduction of cacna1c (Cav1.2; Cav1.2 heterozygous mice), both females [153, 157] and males [153] display anxiety-like behavior. Similarly, restricted elimination of cacna1c (Cav1.2) in excitatory glutamatergic neurons of the forebrain (forebrain Cav1.2 conditional knockout mice), a cell type with high expression of Cav1.2, as well as selective elimination of Cav1.2 in the adult prefrontal cortex (PFC) has been found to result in anxiety-like behavior [150, 153].
These preclinical findings are supported by clinical studies that have identified generalized anxiety [163, 164] and trait anxiety [165] in CACNA1C risk allele (rs1006737) carriers together with structural [166] and functional alterations in the PFC of these individuals [167]. In contrast, male mice harboring the TS gain-of-function Cav1.2 mutation display no anxiety-like phenotype [168], suggesting that a loss, rather than a gain, of Cav1.2 function may mediate anxiety-like behavior.
Social Behavior
Impairments in social behavior are observed in a range of neuropsychiatric disorders [169] and represent a core domain in ASD [170]. Using rodents studies, it has become evident that dysregulated Ca2+ as a consequence of altered Cav1.2 channel function can influence social behavior [168]. The TS Cav1.2 gain-of-function mouse model displays a significant social deficit [168], demonstrating that excess Ca2+ can adversely affect social behavior. Similarly, mice with restricted deletion of Cav1.2 in glutamatergic neurons of the forebrain display a similar deficit in social behavior [150]. Focal knockdown of Cav1.2 in the adult PFC is sufficient to induce the social behavioral deficits [150], identifying the PFC as the common anatomical structure of Cav1.2’s effects on social function and anxiety-like behavior (Fig. 1). This is not surprising given that anxiety has been shown to negatively impact social function [171–173].
As loss of Cav1.2 results in both anxiety and social behavioral deficits, work from our laboratory has begun to dissect the mechanistic interaction between anxiety and social function by examining the biological pathways underlying these impairments. One mechanism that has received tremendous attention in recent years is dysregulation of dendritic mRNA translation and protein synthesis, being attributed to behavioral impairments. The role of LTCCs in regulating dendritic mRNA translation versus nuclear transcription remains largely unknown. One in vitro study has linked LTCCs to the mammalian target of rapamycin (mTOR) pathway [174], one of the most highly studied pathways regulating mRNA translation and protein synthesis [175]. In support of this, loss of Cav1.2 in glutamatergic neurons of the forebrain results in a significant decrease in levels of general protein synthesis in the PFC [150] (Figs. 1 and 2). Molecular studies have identified lower phosphorylated (at serine S2448) mTOR, indicating lower activity of mTOR complex 1 (mTORC1). In parallel, Cav1.2 deficiency also results in heightened levels of phosphorylated (at S51) eIF2α [150], a translational repressor. Both of these molecular findings support lower protein synthesis in Cav1.2-deficient mice. Altered protein synthesis, particularly heightened levels via the mTORC1 pathway has been implicated in both neurodevelopmental disorders, including ASD and neuropsychiatric disorders [176]. Preclinical mouse models with genetic manipulations of substrates of the mTORC1 pathway have been reported to display altered protein synthesis concurrent with neuropsychiatric-associated behavioral phenotypes, particularly social deficits [177–179]. Pharmacological manipulation of the mTOR pathway has been explored for treatment of neuropsychiatric disorders. For example, normalizing elevated protein synthesis with the mTOR inhibitor rapamycin [179] or inhibiting the mRNA translation factor, eIF4 [177, 178], has been shown to reverse social deficits. Supporting these preclinical findings a recent case study in a patient with the neurodevelopmental disorder, tuberous sclerosis complex (TSC), benefitted from the mTOR inhibitor everolimus. TSC in this patient resulted from a genetic deletion in TSC2, which increased mTOR activity, as seen in vitro experiments. Everolimus improved behavioral deficits (cognition, attention, social interaction, language development, and repetitive motor movements), seizures, and improved autism behavioral scores [180].
In contrast to the increase in general protein synthesis observed in several of the above mentioned models, Cav1.2-deficient mice, as also seen in MeCP2-deficient mice [181], display lower general protein synthesis, suggesting that any disruption in translational regulation may induce overlapping behavioral endophenotypes. In support of this, inhibiting the effects of elevated phosphorylated eIF2α S51 and lowering protein synthesis with ISRIB, a small molecule that potently inhibits the effects of eIF2α [182], is sufficient to not only normalize the social deficits, but also to reverse the elevated anxiety-like behavior in forebrain Cav1.2 conditional knockout mice [150]. Because of the lack of pharmacological agents that can elevate general protein synthesis via the mTORC1 pathway, ISRIB provides an alternative strategy to normalize the lower protein synthesis in mouse models such as forebrain Cav1.2 conditional knockout mice. It is interesting that despite lower active mTOR, targeting eIF2α is sufficient to normalize behavioral deficits, suggesting cross-talk between the mTOR and eIF2α pathways [183].
These findings provide a unique role of Cav1.2 in protein synthesis via the eIF2α pathway and potentially the mTOR pathway (Fig. 2), and also identify a common Cav1.2-mediated molecular mechanism underlying social and anxiety-like behaviors (Fig. 1). Furthermore, it identifies a novel target in a Cav1.2-deficient mouse model that can be manipulated in the adult brain to rescue behavioral deficits. The contribution of eIF2α and its pathway to psychiatric and neurodevelopmental disease-associated symptoms remains unexplored but warrants further investigation. Increases in phosphorylation of eIF2α at S51 can not only decrease translation of most mRNAs [184], but can also induce translation of a subset of mRNAs containing short upstream open reading frames in an activating transcription factor 4-dependent manner [146], a member of the CREB family of transcription factors [185]. Thus, further studies to explore the specific proteins targeted by elevated phosphorylated eIF2α in the PFC of Cav1.2-deficient mice that are modulating both anxiety and social function will be informative.
Depressive-Like Behavior
In addition to the above mentioned endophenotypes, depression-related symptoms are also commonly observed in BD, MDD, and SCZ [162]. In the late 1980s, a role for LTCCs in regulating depression-related behavior was first realized using LTCC pharmacological agents demonstrating that the DHP LTCC blocker nifedipine has an antidepressant-like effect in rats [186]. This was further expanded in a later study that showed that, in addition to nifedipine, other DHP blockers, including nicardipine, nitrendipine, isradipine, felodipine, and nimodipine but not amlodipine, had a similar antidepressant-like effect [187]. More recently, in support of the pharmacological antidepressant-like effect, the use of genetic mutant mice has revealed that Cav1.2 heterozygous mice exhibit antidepressant-like behavior [152, 157]. Furthermore, focal knockdown of cacna1c (Cav1.2) in the adult PFC was sufficient to induce a similar antidepressant-like effect [152], consistent with antidepressants exerting their effects through cellular changes in the PFC [188].
In the context of CACNA1C SNPs the above findings suggest that gain of Cav1.2 function mutations would contribute to depression-related symptoms. In support of this, it has been shown that pharmacological activation of LTCCs with the DHP activator BayK8644 induces a depressive-like phenotype [189]. Although depression-related behavior has not been tested in the Cav1.2 gain-of-function TS mouse, there are case reports identifying 1 patient with TS with depression [48] and another patient with TS who developed BD in adulthood [41]. Together, these findings support the theory that gain of Cav1.2 function results in depression-related symptoms.
It is intriguing that loss of Cav1.2 in the PFC results in anxiety-like behavior but has an antidepressant-like effect. A deeper understanding of this differential effect of Cav1.2 deficiency has come from molecular studies that have identified separate mechanisms influencing anxiety and depression-related behaviors. In contrast to dysregulation of the mRNA translation pathway underlying anxiety in Cav1.2-deficient mice (described above), the regulated in development and DNA damage response 1 (REDD1; also known at DDIT4 or RTP801) pathway modulates depression-related behaviors (Fig. 1; [152]). Cav1.2 heterozygous mice that exhibit an antidepressant-like phenotype have lower levels of the depression-related protein REDD1 in the PFC, and increasing levels of REDD1 in this anatomical region of adult Cav1.2 heterozygous mice is sufficient to reverse the antidepressant-like phenotype [152]. This is consistent with present findings of higher REDD1 levels in the PFC of depressed patients [190].
Downstream of REDD1, the protein FoxO3a has been identified to play a role in modulating the antidepressant-like effect observed in Cav1.2 heterozygous mice (Fig. 2; [152]). FoxO3a belongs to the FoxO family of transcription factors with SNPs within the FoxO3a gene linked to BD [191]. In rodents FoxO3a has been identified as a modulator of depression-related behavior [192]. FoxO3a knockout mice exhibit an antidepressant-like phenotype, and the antidepressant imipramine [193] and the mood stabilizer lithium [194] have been found to decrease levels of nuclear FoxO3a, suggesting that higher levels of nuclear FoxO3a may be associated with depressive behavior. In support of this, elevated levels of nuclear FoxO3a in the PFC of Cav1.2 heterozygous mice, following REDD1 overexpression, has been associated with dampening the antidepressant-like phenotype seen in these mice [152]. These findings provide the first evidence of a role of the REDD1/FoxO3a signaling pathway in the PFC in regulating depression-related behavior in Cav1.2 heterozygous mice (Figs. 1 and 2), and a new framework to study Cav1.2-associated depressive behavior.
Cognitive Function
Although not as broadly recognized as a symptom in neuropsychiatric disorders as changes in mood and emotion, cognitive impairments are a prominent feature of the CACNA1C-associated psychiatric disorders, as well as ASD [195]. In particular, deficits within different aspects of learning and memory have been observed in BD, SCZ, MDD, ASD, and, to a lesser extent, ADHD [195]. Using rodent models, there is evidence that loss of Cav1.2 influences discrete forms of learning and memory. In the hippocampal-dependent Morris water maze (MWM) spatial memory task, Cav1.2 conditional knockout mice display normal acquisition and consolidation of the platform location with similar performance to the controls during the short- and long-term (24 hour) probe tests [150, 196], whereas during the remote 30-day probe trial Cav1.2 knockout mice display a significant deficit [196]. Recently, it has been demonstrated that by increasing the difficulty of the MWM task by decreasing the number of available spatial cues, Cav1.2 conditional knockout mice exhibit a delay in the acquisition of the platform location and a significant deficit in the long-term memory probe test [197]. A similar hippocampal-dependent deficit has been observed in the fear-associated context discrimination task [197]. This supports previous data by Moosmang et al. [198] demonstrating that Cav1.2 channels in the hippocampus (using hippocampus-specific conditional knockout mice) are necessary for a hippocampal-dependent discriminatory water-maze task. This is supported by a role of Cav1.2 in hippocampal long-term potentiation [198], a cellular model of learning and memory [199], as well as a role in adult hippocampal neurogenesis [149, 197], a cellular mechanism linked to learning/memory processes ([200, 201]; discussed below).
Similar to Cav1.2-deficient mice, the Cav1.2 gain-of-function TS mice display no deficit in learning and memory in the MWM spatial memory task or the Y-maze task [168]. However, when the hidden escape platform is moved to a different location to test reversal learning in both tasks, mice display a significant delay in determining the new platform location [168]. Because of this mild persistence in continuing to seek the original location of the platform in the MWM and repeatedly attempting to enter the arm of the Y-maze with the original platform, despite the presence of a physical obstruction, the authors interpret these observations as evidence of repetitive, restrictive, and perseverative behavior [168], and possibly a sign of lack of cognitive flexibility, seen in disorders such as SCZ [202]. In contrast to these findings, loss of Cav1.2 in the glutamatergic neurons of the forebrain appears to negatively impact learning and memory in the Y-maze hidden-platform task [150], an observation that begs further exploration on the anatomical and cell-type specificity of loss of Cav1.2 signaling.
Separately from studies in rodents, it is clear that the LTCCs also play an important role in fear-associated memories, the most common behavioral paradigm utilized to study the biological basis of emotion [203–205]. This is not surprising given that altered emotional processing has been reported in patients with SCZ, BD, and ADHD [206]. In rodents, it has been observed that systemic inhibition of LTCCs with nifedipine had no impact on the acquisition or long-term expression of cue-associated fear memories [207]. However, focal delivery of verapamil in the basolateral amygdala, a brain region involved in fear, of adult rats immediately prior to fear conditioning blocked cue-associated long-term fear memory but not the short-term memory [208]. Similarly, focal delivery of the LTCC blockers verapamil or nifedipine into the basolateral amygdala of adult rats immediately before cue extinction training impaired the long-term memory of fear extinction [209]. This is consistent with a previous study that showed impaired cue extinction with systemic administration of the LTCC blockers nifedipine and nimodipine [207]. These studies suggest that differential LTCC-mediated mechanisms are being recruited for acquisition versus extinction of cue-associated fear memories.
Using genetic mutant mice, recent studies have focused on dissociating the differential contribution of the Cav1.2 and Cav1.3 isoforms in fear processes. In agreement with pharmacological studies, brain-specific Cav1.2 knockout mice have no deficit in the consolidation and recall of a cue-associated fear memory [210]. However, selective conditional knockout of Cav1.2 in glutamatergic neurons of the forebrain display enhanced freezing during the long-term cue-associated fear memory test [150]. This discrepancy is most likely a result of compensatory upregulation of Ca2+-permeable glutamate α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors (AMPARs) in the amygdala [210]. Interestingly in the Cav1.2 gain-of-function TS mouse, an increase in freezing during the long-term cue-associated fear memory test has been reported [168], suggesting that too much or too little Cav1.2 signaling can have similar behavioral phenotypes in certain tasks. Interestingly, in contextual fear conditioning, loss of Cav1.2 in genetic mutant mice [197, 211] did not impact freezing during the context-associated fear memory test. In contrast, the Cav1.2 gain-of-function TS mice exhibited enhanced freezing during the context-associated fear memory test [168], identifying that loss and gain of function can have differential effects of certain brain region-specific tasks. In addition to the conventional fear-conditioning paradigms, LTCC inhibitors have been shown to block latent inhibition of conditioned fear [212] and fear-potentiated startle [213], suggesting a role of these channels in other forms of emotional learning and plasticity.
The mechanism underlying altered fear memories described above are not known. Late-phase long-term potentiation (LTP) at thalamic inputs to the lateral amygdala, a mechanism that requires LTCCs [198, 208, 214, 215], has been associated with cue fear conditioning [216]. One molecule that mediates LTP in the thalamoamygdala pathway is brain-derived neurotrophic factor (BDNF) [217], a downstream target of LTCCs [149, 218]. Induction of BDNF in the amygdala is required for consolidation of fear memories [219]. Supporting these findings, administration of the LTCC inhibitor verapamil blocks the induction of BDNF after cue-associated fear conditioning [220]. The findings from this study suggest that this occurs as a result of lack of activation of CaMKIV [220], a CREB kinase and a downstream target of LTCCs [221], resulting in decreased binding of phosphorylated CREB at the promoter regions of BDNF [220]. This is consistent with previous studies that have identified LTCCs as critical regulators of BDNF expression both in vitro [222] and in vivo [149]. Currently, the specific LTCC isoform mediating this fear conditioning-induced LTP in the thalamoamygdalar pathway is unknown.
Cav1.2 Channels, Adult Hippocampal Neurogenesis, and Neuropsychiatric-Related Phenotypes
Adult hippocampal neurogenesis that involves addition of newborn neurons (granule cells) to the dentate gyrus of the hippocampus throughout life has been implicated in the pathology underlying SCZ, based on rodent models of the disorder [223–230], BD based on genes associated with the disorder [137, 231], and depression [232, 233], autism [234–237], and ADHD, based on rodent disease models [229, 235, 238]. Rodent behavioral studies suggest a role of adult hippocampal neurogenesis in many of the phenotypes related to these disorders that are also observed in Cav1.2-deficient mice described above, including memory formation [200, 201], context discrimination [239], modulation of anxiety and depressive-like behavior [240], as well as mediating the effects of antidepressants. In support of this, 2 independent studies have identified a deficit in adult hippocampal neurogenesis in mice with loss of Cav1.2 restricted to glutamatergic neurons of the forebrain [149] and in neurons of the entire brain [197]. This is consistent with a previous in vitro study identifying a role of LTCCs in activity-dependent regulation of adult-derived neural precursor cells [241].
The deficit in adult hippocampal neurogenesis in Cav1.2 conditional knockout mice is specific to survival and not proliferation of neural precursor cells (NPCs) [149]. This finding is supported by an in vitro study that has identified a role of LTCCs during the later neurogenic stages of survival and maturation of NPCs derived from adult rat hippocampus [242]. As adult hippocampal neurogenesis is a highly regulated process and results from a balance of proliferation of NPCs and the survival of young newborn neurons into which NPCs differentiate [243], the discovery of Cav1.2 channels in supporting the survival of newborn neurons suggests that this stage of adult neurogenesis may be important for certain aspects of neuropsychiatric disease.
The precise mechanism of the deficit in survival of newborn neurons remains unknown. Given that Cav1.2 expression is restricted to mature young hippocampal neurons in adult mice [244], one potential mechanism is via the neurotrophic factor, BDNF. LTCCs mediate BDNF production in glutamatergic neurons of the hippocampus [149], release of which acts on both the secreting neuron and neighboring neurons [245]. LTCCs serve as a primary Ca2+ source for Bdnf transcriptional regulation, particularly at the promoter of Bdnf exon IV, a splice variant critically involved in experience-dependent neuronal plasticity [246–249]. Multiple LTCC-activated transcription regulators, including CREB, Ca2+ response factor, and MeCP2, which are also involved in regulating adult hippocampal neurogenesis [127, 237, 250, 251], control Bdnf expression by binding to Bdnf exon IV promoter in hippocampal neurons [222, 252–255]. Thus, it is plausible that lack of activation of these factors in the hippocampus results in lower BDNF and thus lowers survival of newborn neurons. This mechanism may also contribute to the LTP deficit observed in hippocampal-specific Cav1.2 knockout mice [198] as BDNF signaling and adult newborn neurons are required for hippocampal-dependent learning and memory processes [256]. Additionally, BDNF is a key player in regulating mood-related phenotypes [257]. Thus, collectively, it is plausible that the lower survival of adult born neurons as a result of Cav1.2/BDNF deficiency could contribute to the neuropsychiatric-related phenotypes observed in Cav1.2-deficient mice, a mechanism to be confirmed in future studies.
Another key question is whether restoring reduced survival of newborn neurons is sufficient to rescue phenotypes observed in Cav1.2-deficient mice. Using the neuroprotective aminopropyl carbazole P7C3-A20, a small molecule that blocks neuronal cell death [258–264] and thus increases cell survival of hippocampal newborn neurons [243, 265, 266], it has been found that this compound is capable of restoring hippocampal neurogenesis to normal levels in forebrain Cav1.2 conditional knockout mice [149]. This therapeutic effect occurred despite a lack in the normalization of BDNF levels. Given that BDNF-enhancing agents have not proved to be effective therapeutically to date, P7C3-A20 offers an alternative therapeutic mechanistic route to restore impaired adult neurogenesis in Cav1.2-deficient mice that circumvents lower BDNF signaling. If P7C3-A20 is able to rescue behavioral deficits, this work may provide new treatment opportunities for patients suffering from CACNA1C-associated neuropsychiatric symptoms. Additionally the identification of a previously unidentified role for Cav1.2 channels in neuronal cell survival may provide novel insight and approaches to treating neuropsychiatric disease, particularly in situations of decreased Cav1.2 or loss of Cav1.2 function.
Cav1.2, Excitatory/Inhibitory Imbalance and Neuropsychiatric Phenotypes
One emerging hypothesis for the pathophysiological mechanisms underlying the behavioral impairments in neuropsychiatric disorders is altered synaptic excitation (E) to inhibition (I) balance [151, 267], a cellular perturbation reported in multiple mouse models exhibiting anxiety-like behavior, altered social behavior, and impaired cognitive function [150, 177, 178, 267–269]. However, the impact of loss or gain of LTCC function on synaptic E/I balance and its impact on behavior remains largely unknown. In vitro pharmacological studies have provided evidence that LTCC-mediated mechanisms modulate synaptic plasticity in a homeostatic fashion [270]. Cortical neurons treated for 24 hours with the LTCC blocker nifedipine have been shown to increase both frequency and amplitude of miniature excitatory postsynaptic currents [271]. Furthermore, in hippocampal neurons, 24-hour blockade of LTCCs with nifedipine has been found to decrease the expression of synaptic γ-aminobutryic acid A receptors [272], which mediate inhibitory neurotransmission, suggesting that LTCCs can modulate E/I balance. This is supported by an in vivo study, which found that loss of Cav1.2 in glutamatergic neurons of the forebrain results in higher frequency and amplitude of miniature excitatory postsynaptic currents in layer-5 neurons of the PFC, suggesting an increase in the overall E/I balance in this region [150], supporting other mouse models of neuropsychiatric disorders with higher E/I associated with neuropsychiatric-related behaviors.
These in vivo and in vitro studies suggest that chronic loss of LTCC signaling can have long-term consequences on synaptic scaling and, subsequently, function. The precise mechanism underlying this synaptic plasticity is not known. There are, however, 2 possible mechanisms that may be involved. First, impaired LTCC signaling may impact on nuclear transcriptional processes that can subsequently affect dendritic synaptic protein changes. This possibility is supported by an in vitro study that found that 24-hour inhibition of LTCCs results in increased (as opposed to the expected decrease) CREB-dependent transcription of the GluA1 subunit of the excitatory AMPARs [271]. Second, loss of LTCC signaling can negatively affect the mRNA translation machinery within spines and alter the composition of synaptic proteins [150]. These findings add to the growing literature that neuropsychiatric disorders are disorders of the synapse and that altered Cav1.2 signaling, even though shown not to impact spine and dendritic architecture [198, 210] as opposed to Cav1.3 channels [28, 273], can impact synaptic function via secondary homeostatic effects.
Cav1.3 Channels and Neuropsychiatric-Related Phenotypes
Anxiety-Like, Depressive-Like, and Social Behavior
Using rodent preclinical models, Cav1.3 channels, although less studied than Cav1.2 channels, also modulate neuropsychiatric-related endophenotypes. Cav1.3-deficient mice demonstrate an anxiolytic-like phenotype [274], although this effect may be attributed to the congenital deafness observed in these mice [275]. This is supported by recent findings in Cav1.2DHP–/– mice wherein treatment with the LTCC activator BayK8644, which selectively activates Cav1.3 channels, does not induce anxiety-like behavior [51]. In contrast to this, Cav1.3 regulates depressive-like behavior with Cav1.3 deficiency resulting in an antidepressant-like phenotype [274], whereas systemic activation of the Cav1.3 channels induces a depressive-like phenotype [159]. Cav1.3 channel activation with BayK8644 has also been found to induce a deficit in social behavior [51], in support of Cav1.3 gain-of-function mutations associated with ASD [7, 54]. The systemic effect of Cav1.3 channel activation on depression-related and social behaviors has been attributed to its role in the ventral tegmental area (VTA) [51], supporting the role of dopaminergic neurotransmission in both depressive and social behavior (discussed below).
Cognitive Function
Rodent studies have identified a role of Cav1.3 in certain forms of learning and memory. Although Cav1.3-deficient mice displayed no deficit in the MWM spatial memory task [276], these mice have significantly impaired object location memory in a discrimination test [244], suggesting that Cav1.3 channels may be recruited in specific spatial memory tasks. However, given the findings of Temme et al. [197] that Cav1.2 is recruited when the difficulty of the MWM is increased, it would be interesting to test Cav1.3-deficient mice in a similar task, particularly given the deficit in adult hippocampal neurogenesis observed in these mice ([244]; reviewed below). In the contextual fear-conditioning test, Cav1.3 channels are not required during acquisition or extinction of the conditioned memory [106, 276], but play an important role in the consolidation of the context-associated fear memory [276]. This has been attributed to reduced LTP in the basolateral amygdala [277].
Adult Hippocampal Neurogenesis
In contrast to the high expression of Cav1.2 LTCCs in the hippocampus, Cav1.3 channels are expressed at much lower levels [278]. Despite this, loss of Cav1.3 channels has a profound effect on adult hippocampal neurogenesis [244]. Cav1.3 knockout mice display a deficit in both proliferation of neural progenitor cells and survival of newborn hippocampal neurons [244], an effect not observed following deletion of Cav1.2 channels that only impacts survival [149]. These differential roles of Cav1.2 and Cav1.3 may be a consequence of the differential expression of Cav1.2 and Cav1.3 channels in the adult neurogenic regions [244]. While Cav1.2 is expressed exclusively in mature young hippocampal neurons, Cav1.3 is expressed in both newly formed immature NPCs, as well as mature young hippocampal neurons [244]. The contribution of reduced adult hippocampal neurogenesis to mood and learning/memory behaviors as a result of deficient Cav1.3 remains currently unknown, but it is plausible that it could contribute to the mood and memory deficits associated with dysregulated Cav1.3 Ca2+ signaling.
L-Type Ca2+ Channels and Drug Dependence
LTCCs have been demonstrated to play a role in mediating the effects of multiple drugs of abuse, including psychostimulants (cocaine, amphetamine), opioids (morphine), alcohol, and nicotine. To date, no genetic studies have been reported linking CACNA1C to drug dependence; however, CACNA1C-risk SNP carriers have altered reward processing [279], and a recent study has weakly linked CACNA1C to food addiction [280]. In contrast, recent work has identified a significant association between CACNA1D and cocaine dependence [51]. Below we review both LTCC pharmacological studies (summarized in Table 3) and LTCC isoform-specific contribution to drug dependence-specific phenotypes in rodent models.
Table 3.
L-Type calcium-channel pharmacological studies and its contribution to drug dependence-specific phenotypes in rodent models
| Drug | Behavioral paradigm | LTCC blocker | Behavioral outcome | Reference |
|---|---|---|---|---|
| Cocaine | Behavioral sensitization | Nimodipine | Suppressed development [157, 281] and expression [157, 282] of sensitization | [283] |
| Nifedipine | [160] | |||
| Diltiazem | [284] | |||
| Conditioned place preference | Isradipine | Decreased conditioned place preference | [282, 285] | |
| Nifedipine and verapamil | [286] | |||
| Nifedipine | [51, 287] | |||
| Self-administration | Isradipine and nimodipine | Decreased self administration | [288] | |
| Self-administration: cocaine-primed reinstatement | Diltiazem | Decreased reinstatement of cocaine seeking following extinction | [289] | |
| Morphine | Behavioral sensitization | Nimodipine, nifedipine, and verapamil | Suppressed development of sensitization | [290] |
| Conditioned place preference | Nifedipine, verapamil | Decreased conditioned place preference | [286] | |
| Nifedipine | [287] | |||
| Isradipine | [291] | |||
| Self-administration | Isradipine and nimodipine | Decreased self-administration | [288] | |
| Naloxone-induced withdrawal |
Nifedipine, nimodipine and verapamil (prior to morphine) | Attenuated the withdrawal effects | [292] | |
| Diltiazem (along with morphine) | Attenuated the withdrawal effects | [293, 294] | ||
| Verapamil (after morphine but before naloxone) | [295] | |||
| Verapamil, nimodipine (after morphine but before naloxone) | [296] | |||
| Verapamil, nicardipine and diltiazem (after morphine but before naloxone) | [297] | |||
| Withdrawal after chronic morphine | Nimodipine (along with morphine) | Attenuated some of the withdrawal effects | [298, 299] | |
| Nifedipine (along with morphine) | [300] | |||
| Ethanol | Consumption | Nifedipine | Decreased ethanol intake | [301] |
| Verapamil | [302] | |||
| Nifedipine, verapamil and isradipine | [303] | |||
| Nifedipine, felodipine, nimodipine, isradipine, nicardipine, nitredipine and diltiazem | [304] | |||
| Isradipine and nifedipine | No effect | [305] | ||
| Nimodipine | [306] | |||
| Locomotor activity | Nifedipine | Decreased locomotor activity induced by low dose of ethanol (2.5 g/kg) exposure | [301, 307, 308] | |
| Verapamil and diltiazem | ||||
| Nifedipine and verapamil | No effect after chronic treatment of the blockers | [309] | ||
| Self-administration | Verapamil | Prevented cue-primed reinstatement following 21 days of abstinence | [20] | |
| Withdrawal following chronic ethanol consumption | Nitrendipine | Reduced withdrawal symptoms | [310, 311] | |
| Withdrawal following chronic ethanol inhalation | Nitrendipine | Reduced withdrawal symptoms | [310, 311] | |
| Nimodipine, nitrendipine and isradipine | Reduced convulsive behavior during withdrawal | [310] | ||
| Withdrawal following binge drinking | Nimodipine | Reduced withdrawal symptoms following binge drinking | [312] | |
| Chronic alcohol-induced seizures | Nifedipine | Reduced chronic alcohol-induced seizures | [313] | |
| Nifedipine and nimodipine | [314] | |||
| Nicotine | Locomotor activity | Nimodipine | Reduced acute nicotine induced locomotor activity | [315] |
| Behavioral sensitization; Locomotor activity | Nimodipine, verapamil and diltiazem | Suppressed development and expression of behavioral sensitization | [316] | |
| Nifedipine | Suppressed expression of behavioral sensitization | [16] | ||
| Mecamylamine-induced withdrawal | Nimodipine, verapamil and diltiazem | Reduced withdrawal symptoms | [317] | |
| Withdrawal from acute nicotine | Nimodipine, verapamil and diltiazem | Attenuated withdrawal- induced anxiety | [315, 318] | |
| Withdrawal from chronic nicotine treatment | Nimodipine and verapamil | No effect on withdrawal-induced anxiety | [319] |
Cocaine
In rodents, pharmacological studies have established an important role of LTCCs in various aspects of cocaine’s effects. LTCC blockers, nimodipine, nifedipine, and diltiazem have been shown to attenuate the development and expression of cocaine behavioral sensitization [160, 283, 284], a model of drug-induced plasticity [320–322]. Using cocaine-conditioned place preference (CPP), a model used to study the rewarding effects of drugs [281], isradipine [282, 285] and nifedipine [51, 286, 287] diminish the rewarding effects of cocaine. Additionally, using cocaine self-administration, a model of the reinforcing effects of drugs [323], isradipine and nimodipine attenuate the reinforcing effects of cocaine [288].
LTCC blockers have also demonstrated efficacy in rodent models of relapse to cocaine-seeking behavior, one of the central clinical problems in treating cocaine addiction. In a self-administration model of relapse following extinction of cocaine-seeking behavior, diltiazem treatment in the nucleus accumbens (NAc) has been shown to block the effects of cocaine-primed seeking behavior [289]. Similarly, blocking LTCCs with isradipine in the VTA has also shown efficacy in attenuating cocaine-seeking behavior following exposure to drug-associated cues in drug-abstinent rats [324], another model of relapse. Of clinical significance, this study found that isradipine had no effect on sucrose-seeking behavior, suggesting that isradipine could be directly targeted in cocaine-dependent individuals without affecting their natural reward processing.
Studies addressing the specific role of the individual LTCC isoforms have identified a critical role of the Cav1.3 LTCCs in dopaminergic neurons of the VTA in the development of cocaine behavioral sensitization [325] and the acquisition of cocaine CPP [51]. Given that Cav1.3 channels are the primary L-type subunit in VTA dopamine neurons [15], the effects of isradipine in the VTA on attenuation of cocaine CPP [282] and cocaine-seeking behavior [324] are most likely due to its effects on Cav1.3 channels. However, VTA Cav1.2 channels may also play a role as they mediate acute responses [326] and VTA physiology [327]. In contrast, Cav1.2 channels play a role in mediating the long-term effects of cocaine via its effects in the NAc [160, 161].
Molecular studies find that Cav1.3 channels activate the CamKII/ERK pathway in the VTA and Cav1.2 channels in the NAc activate CamKII (Fig. 2), which increases GluA1 phosphorylation and elevates surface expression of GluA1 [161]. Recently, these findings have been extended to demonstrate that Ca2+-permeable AMPARs (CP-AMPARs) in the NAc mediate the long-term effects of cocaine (Fig. 1) [51], and add to the growing body of evidence that long-lasting addiction-related behaviors are mediated by an increase in NAc CP-AMPAR neurotransmission [328].
Morphine
LTCCs have also been shown to play a role in the rewarding effects of morphine. The LTCC blockers nimodipine, nifedipine, and verapamil attenuate the development of morphine sensitization [290]. Similarly, isradipine and nifedipine attenuate the rewarding effects of morphine using CPP [286, 287, 291], and isradipine and nimodipine suppress the reinforcing effects of morphine using self-administration [288].
A major aspect of morphine and opioids, in general, is the manifestation of physical withdrawal symptoms [329]. This can be modeled in rodents by precipitating withdrawal symptoms with the use of the compound naloxone [330, 331]. Multiple studies have also shown that LTCC blockers when administered prior to (nifedipine, nimodipine, verapamil [292]), along with (diltiazem, nimodipine, nifedipine [293, 294, 298–300]) or after morphine treatment (verapamil, nimodipine, diltiazem, nicardipine [295–297]) can alleviate physical withdrawal symptoms, suggesting that LTCC blockers may be helpful in easing withdrawal symptoms following onset.
The molecular mechanisms by which LTCCs mediate the effects of morphine remain unknown. However, there is evidence of increased Cav1.2 and Cav1.3 protein levels in the frontal cortex and limbic forebrain regions of mice exposed to morphine [287, 332]. Separately, it has also been reported that chronic morphine treatment results in a decrease in Cav1.3 but not Cav1.2 protein levels in midbrain regions (pons, midbrain, and medulla [333]). Together, these findings suggest that morphine may regulate Cav1.2 and Cav1.3 in a brain region-specific manner.
Ethanol
Pharmacological studies provide evidence that LTCCs are important mediators of the effects of ethanol. Verapamil, isradipine, nifedipine, felodipine, nimodipine, nicardipine, nitrendipine, diltiazem, and verapamil reduce ethanol consumption [301–304], and nifedipine, verapamil, and diltiazem decrease the heightened locomotor activity induced by low doses of ethanol [301, 307, 308]. In contrast, a study reported that nifedipine and verapamil had no impact on the ethanol-induced increase in locomotor activity [309], nor did isradipine, nifedipine or nimodipine on ethanol consumption [305, 306]. This discrepancy in findings may rely mainly on the different doses of LTCC blockers used. Verapamil has also been shown to block alcohol-seeking behavior in response to alcohol-associated cues following abstinence using self-administration [20], and mice deficient in Cav1.2 in forebrain glutamatergic neurons show a deficit in alcohol-seeking behavior [20]. These behavioral findings are consistent with the previous report showing that protracted abstinence from alcohol increases Cav1.2 but not Cav1.3 in the amygdala and hippocampus [20], 2 brain regions involved in mediating the effects of alcohol [334–336].
Separately, nitrendipine has been shown to reduce withdrawal symptoms when administered during chronic ethanol exposure [310, 311]. Excessive ethanol consumption in a short period of time (also referred to as “binge drinking”) can be mimicked in rodents, with nimodipine reducing the withdrawal effects resulting from binge drinking [312]. Furthermore, nifedipine and nimodipine have been found to reduce seizures that occur during withdrawal from chronic alcohol [313, 314], a symptom suggested to be driven, in part, by increased LTCC currents [337]. Similarly, nimodipine, nitrendipine, and isradipine can also decrease the convulsive behavior associated with chronic ethanol withdrawal [338].
Nicotine
As with other drugs of abuse, the continuous use of nicotine results in dependency and adverse withdrawal symptoms while in abstinence [339]. Acute nicotine treatment in mice increases forebrain Cav1.3 mRNA levels 24 hours after exposure, while chronic nicotine treatment alters Cav1.2 mRNA levels [16]. Additionally, cortical neurons exposed to long-term nicotine, enhances Cav1.2 and Cav1.3 protein levels [340]. This was later confirmed by chronic nicotine treatment for 7 days in mice that led to an increase in Cav1.2 and Cav1.3 protein levels in the cortex [341]. Behaviorally, LTCC blockers have been shown to attenuate acute nicotine-induced locomotor activity (nimodipine [315]), as well as decrease the development (nimodipine, verapamil, diltiazem [316]) and expression (nimodipine, verapamil, diltiazem, nifedipine [16, 316]) of nicotine behavioral sensitization. Similarly, treatment with nimodipine, diltiazem, and verapamil reduced the rewarding effects of nicotine using CPP [316]. Moreover, nimodipine was capable of attenuating nicotine-induced drug seeking using the self-administration paradigm [318].
Nicotine dependent individuals undergo physical withdrawal that can be modeled in rodents using the compound mecamylamine [342]. Nimodipine, verapamil, and diltiazem have been shown to attenuate the mecamylamine-induced withdrawal symptoms [317]. Anxiety is one of the most common features observed in nicotine-dependent individuals when they abstain from smoking [343]. Nimodipine, verapamil, and diltiazem reduced the anxiogenic effects during withdrawal resulting from acute nicotine treatment [318]. However, one study found that nimodipine and verapamil administered during withdrawal from nicotine had no impact on the anxiogenic effect of chronic nicotine treatment [319]. These studies suggest that LTCCs can modulate nicotine-induced anxiety only if the blocker is administered before nicotine dependency.
Model of Comorbid Mood and Substance Use Disorders
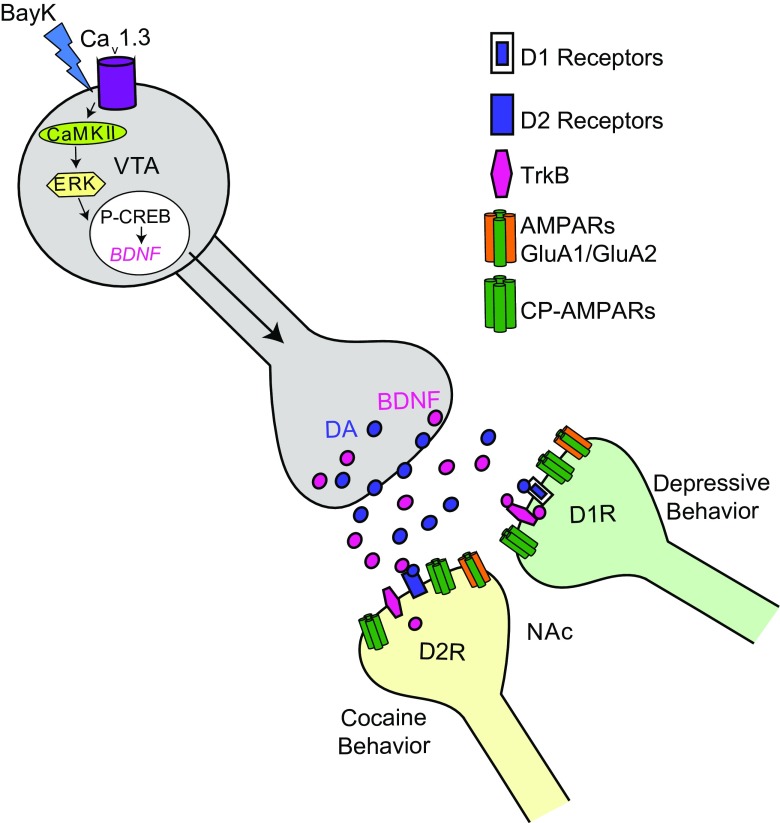
Genetic factors significantly influence susceptibility to mood disorders and substance abuse that are often comorbid, particularly as seen for BD and cocaine dependence [344], conditions linked to CACNA1D [31, 49, 51]. Overlapping neural circuitry and convergent cellular and molecular mechanisms have been suggested to underlie such comorbidity [345–347]. As reviewed above, emerging data on the impact of CACNA1D mutations on Cav1.3 physiology [7, 54], together with animal studies, suggest that enhanced Cav1.3 activity (resulting from gain-of-function mutations or increased gene expression from noncoding variants) may contribute to co-occurring mood and drug-dependence phenotypes. Recent rodent studies have found that common molecular mechanisms can regulate depressive-like behavior, deficits in social behavior, and cocaine-related behaviors [348–352]. In support of the human genetic findings, work from our laboratory has identified that repeated activation of Cav1.3 channels in the VTA in Cav1.2DHP–/– mice, with high Cav1.3 expression [15], is sufficient to induce depressive-like behavior, social deficits, and cocaine-related behaviors [51]. A potential mechanism could be via Cav1.3 channels increasing burst firing of VTA dopamine neurons [327], a neuronal property known to mediate depressive-like behavior [353–355], social behavior [356], and reward-related behavior [357].
The NAc is another key brain reward region that mediates the effects of all 3 behaviors, and molecular adaptations within this region drive long-term behavioral changes [347, 358, 359], a crucial problem in substance abuse disorders and possibly depressive behavior and social impairments, particularly following stressful insults. In fact, it has been shown that the NAc mediates the effects of Cav1.3 channel activation in the VTA [51]. This is not surprising as the VTA–NAc mesolimbic pathway has a central role in mediating the effects of depressive-like behavior [353, 354], social behavior [356], and cocaine [360], with glutamatergic signaling in the NAc driving many of these behaviors [328]. In support of this, depressive-like and cocaine behaviors resulting from VTA Cav1.3 activation are mediated by increased CP-AMPARs in the NAc shell, whereas social deficits are mediated by increased GluA1/GluA2 AMPARs in the NAc core [51], 2 subregions demonstrated to play distinct roles within the brain’s reward pathway [361]. This is consistent with studies that have identified CP-AMPARs as a key synaptic mechanism underlying cocaine-behaviors [328] and heightened AMPAR activity in the NAc as a mediator of depressive [362–364] and social behaviors [365]. Together, these findings provide evidence of a useful, disease relevant model to study mechanisms of co-occurring mood- and cocaine-dependence-related behavioral phenotypes.
How VTA Cav1.3 channel activation can simultaneously promote depression- and cocaine-related behaviors remains an unanswered question. Given that Cav1.3 activation is expected to increase VTA dopamine burst firing [327] and thus increase dopamine release in the NAc that is expected to increase cocaine behaviors but decrease depressive symptoms, opposite of what is seen in patients and animal models, dopamine alone is not sufficient to explain the emergence of both behaviors. A potential candidate that could be mediating both these behaviors is BDNF. It has been found that BDNF via its receptor, tropomyosin receptor kinase B (TrkB) in the NAc mediates both depressive behavior [366] and cocaine behaviors [367]; however, it exerts its effects on the 2 behaviors in a cell-type-specific manner. The NAc is composed of 2 primary populations: the dopamine D1 receptor-containing and dopamine D2 receptor-containing cells [368, 369]. BDNF/TrkB in D1 receptor cells have been shown to mediate depressive behavior [366], whereas BDNF/TrkB in D2 receptor cells mediate cocaine behaviors [367]. As BDNF is a downstream target of LTCCs it is plausible that BDNF is generated following Cav1.3 activation in the VTA, most likely via activation of the CaMKII/ERK/CREB pathway [325] that is transported to the NAc (Fig. 3).
Fig. 3.
Proposed mechanistic model for ventral tegmental area (VTA) Cav1.3 activation, which leads to depressive-like and cocaine-related behaviors. VTA Cav1.3 channel activation by BayK 8644 promotes CAM-dependent protein kinase (CaMK)II/extracellular regulated kinase (ERK)/ cAMP response element-binding protein (CREB) signaling, which results in the production of the neurotrophic factor, brain-derived neurotrophic factor (BDNF). Subsequently, BDNF gets transported from the VTA to the nucleus accumbens (NAc), which may mediate both depressive-like and cocaine behaviors, via increase in Ca2+-permeable α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors (CP-AMPARs). We propose that depressive like-behavior is mediated by a BDNF/tropomyosin receptor kinase B (TrkB) mechanism in NAc dopamine (DA) D1 receptor-expressing cells [350] and cocaine-related behaviors in NAc DA D2 receptor-expressing cells [351]
Conclusions
From these studies, it is clear that dysregulation of both brain-specific LTCC isoforms Cav1.2 and Cav1.3 can contribute to neuropsychiatric-associated endophenotypes and that LTCC blockers have the potential for alleviating some, if not all, psychiatric symptoms resulting from CACNA1C and CACNA1D dysfunction. Targeted anatomical approaches and molecular studies in preclinical animal models provide evidence that dysfunction of Cav1.2 and Cav1.3 channels alter distinct signaling cascades in separate anatomical structures that influence behavioral outcomes. This underscores the complexity of neuropsychiatric disorders and the cell-type- and brain-region-specific influence of CACNA1C and possibly CACNA1D risk SNPs on disease symptoms. Another factor to consider as studies continue to examine potential mechanisms of CACNA1C- and CACNA1D-associated disorders, as well as treatment options, is the impact of secondary effects as a result of persistent dysregulated Ca2+ in neurons on neuropsychiatric symptoms. We now know that dysregulated Ca2+-mediated molecular and transcriptional gene networks [370], as well as the inability to maintain neuronal homeostasis [371], can disrupt normal development of neuronal circuits and lead to brain disease. Thus, by identifying biological pathways underlying specific symptoms and discovering novel substrates that are altered as a consequence of dysregulated Cav1.2 and Cav1.3 may provide better targets for therapeutics.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
Acknowledgments
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Z.D. Kabir and A. Martínez-Rivera contributed equally to this paper.
Electronic supplementary material
The online version of this article (doi:10.1007/s13311-017-0532-0) contains supplementary material, which is available to authorized users.
References
- 1.Kabir ZD, Lee AS, Rajadhyaksha AM. L-type Ca2+ channels in mood, cognition and addiction: integrating human and rodent studies with a focus on behavioural endophenotypes. J Physiol. 2016;594(20):5823–5837. doi: 10.1113/JP270673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zamponi GW, Striessnig J, Koschak A, Dolphin AC. The physiology, pathology, and pharmacology of voltage-gated calcium channels and their future therapeutic potential. Pharmacol Rev. 2015;67(4):821–870. doi: 10.1124/pr.114.009654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ebert DH, Greenberg ME. Activity-dependent neuronal signalling and autism spectrum disorder. Nature. 2013;493(7432):327–337. doi: 10.1038/nature11860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhat S, Dao DT, Terrillion CE, et al. CACNA1C (Cav1.2) in the pathophysiology of psychiatric disease. Prog Neurobiol. 2012;99(1):1–14. doi: 10.1016/j.pneurobio.2012.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heyes S, Pratt WS, Rees E, et al. Genetic disruption of voltage-gated calcium channels in psychiatric and neurological disorders. Prog Neurobiol. 2015;134:35–54. doi: 10.1016/j.pneurobio.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ortner NJ, Striessnig J. L-type calcium channels as drug targets in CNS disorders. Channels (Austin) 2016;10(1):7–13. doi: 10.1080/19336950.2015.1048936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinggera A, Lieb A, Benedetti B, et al. CACNA1D de novo mutations in autism spectrum disorders activate Cav1.3 L-type calcium channels. Biol Psychiatry. 2015;77(9):816–822. doi: 10.1016/j.biopsych.2014.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romme IA, de Reus MA, Ophoff RA, Kahn RS, van den Heuvel MP. Connectome disconnectivity and cortical gene expression in patients with schizophrenia. Biol Psychiatry. 2017;81(6):495–502. doi: 10.1016/j.biopsych.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 9.Gurung R, Prata DP. What is the impact of genome-wide supported risk variants for schizophrenia and bipolar disorder on brain structure and function? A systematic review. Psychol Med. 2015;45(12):2461–2480. doi: 10.1017/S0033291715000537. [DOI] [PubMed] [Google Scholar]
- 10.Striessnig J, Pinggera A, Kaur G, Bock G, Tuluc P. L-type Ca(2+) channels in heart and brain. Wiley Interdiscip Rev Membr Transp Signal. 2014;3(2):15–38. doi: 10.1002/wmts.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tanaka O, Sakagami H, Kondo H. Localization of mRNAs of voltage-dependent Ca(2+)-channels: four subtypes of alpha 1- and beta-subunits in developing and mature rat brain. Brain Res Mol Brain Res. 1995;30(1):1–16. doi: 10.1016/0169-328X(94)00265-G. [DOI] [PubMed] [Google Scholar]
- 12.Ludwig A, Flockerzi V, Hofmann F. Regional expression and cellular localization of the alpha1 and beta subunit of high voltage-activated calcium channels in rat brain. J Neurosci. 1997;17(4):1339–1349. doi: 10.1523/JNEUROSCI.17-04-01339.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herman JP, Chen KC, Booze R, Landfield PW. Up-regulation of alpha1D Ca2+ channel subunit mRNA expression in the hippocampus of aged F344 rats. Neurobiol Aging. 1998;19(6):581–587. doi: 10.1016/S0197-4580(98)00099-2. [DOI] [PubMed] [Google Scholar]
- 14.Clark NC, Nagano N, Kuenzi FM, et al. Neurological phenotype and synaptic function in mice lacking the CaV1.3 alpha subunit of neuronal L-type voltage-dependent Ca2+ channels. Neuroscience. 2003;120(2):435–442. doi: 10.1016/S0306-4522(03)00329-4. [DOI] [PubMed] [Google Scholar]
- 15.Rajadhyaksha A, Husson I, Satpute SS, et al. L-type Ca2+ channels mediate adaptation of extracellular signal-regulated kinase 1/2 phosphorylation in the ventral tegmental area after chronic amphetamine treatment. J Neurosci. 2004;24(34):7464–7476. doi: 10.1523/JNEUROSCI.0612-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bernardi RE, Uhrig S, Spanagel R, Hansson AC. Transcriptional regulation of L-type calcium channel subtypes Cav1.2 and Cav1.3 by nicotine and their potential role in nicotine sensitization. Nicotine Tob Res. 2014;16(6):774–785. doi: 10.1093/ntr/ntt274. [DOI] [PubMed] [Google Scholar]
- 17.Liebmann L, Karst H, Sidiropoulou K, et al. Differential effects of corticosterone on the slow afterhyperpolarization in the basolateral amygdala and CA1 region: possible role of calcium channel subunits. J Neurophysiol. 2008;99(2):958–968. doi: 10.1152/jn.01137.2007. [DOI] [PubMed] [Google Scholar]
- 18.Brewer LD, Dowling AL, Curran-Rauhut MA, Landfield PW, Porter NM, Blalock EM. Estradiol reverses a calcium-related biomarker of brain aging in female rats. J Neurosci. 2009;29(19):6058–6067. doi: 10.1523/JNEUROSCI.5253-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daschil N, Kniewallner KM, Obermair GJ, et al. L-type calcium channel blockers and substance P induce angiogenesis of cortical vessels associated with beta-amyloid plaques in an Alzheimer mouse model. Neurobiol Aging. 2015;36(3):1333–1341. doi: 10.1016/j.neurobiolaging.2014.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Uhrig S, Vandael D, Marcantoni A, et al. Differential roles for L-type calcium channel subtypes in alcohol dependence. Neuropsychopharmacology. 2017;42:1058–1069. doi: 10.1038/npp.2016.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hetzenauer A, Sinnegger-Brauns MJ, Striessnig J, Singewald N. Brain activation pattern induced by stimulation of L-type Ca2+-channels: contribution of Ca(V)1.3 and Ca(V)1.2 isoforms. Neuroscience 139(3), 1005-1015 (2006). [DOI] [PubMed]
- 22.Catterall WA. Structure and regulation of voltage-gated Ca2+ channels. Annu Rev Cell Dev Biol. 2000;16:521–555. doi: 10.1146/annurev.cellbio.16.1.521. [DOI] [PubMed] [Google Scholar]
- 23.Xu W, Lipscombe D. Neuronal Ca(V)1.3alpha(1) L-type channels activate at relatively hyperpolarized membrane potentials and are incompletely inhibited by dihydropyridines. J Neurosci 21(16), 5944-5951 (2001). [DOI] [PMC free article] [PubMed]
- 24.Lipscombe D. L-type calcium channels: highs and new lows. Circ Res. 2002;90(9):933–935. doi: 10.1161/01.RES.0000019740.52306.92. [DOI] [PubMed] [Google Scholar]
- 25.Koschak A, Reimer D, Huber I, et al. alpha 1D (Cav1.3) subunits can form l-type Ca2+ channels activating at negative voltages. J Biol Chem. 2001;276(25):22100–22106. doi: 10.1074/jbc.M101469200. [DOI] [PubMed] [Google Scholar]
- 26.Simms BA, Zamponi GW. Neuronal voltage-gated calcium channels: structure, function, and dysfunction. Neuron. 2014;82(1):24–45. doi: 10.1016/j.neuron.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 27.Calin-Jageman I, Lee A. Ca(v)1 L-type Ca2+ channel signaling complexes in neurons. J Neurochem. 2008;105(3):573–583. doi: 10.1111/j.1471-4159.2008.05286.x. [DOI] [PubMed] [Google Scholar]
- 28.Stanika R, Campiglio M, Pinggera A, et al. Splice variants of the CaV1.3 L-type calcium channel regulate dendritic spine morphology. Sci Rep 6, 34528 (2016). [DOI] [PMC free article] [PubMed]
- 29.Zamponi GW. Targeting voltage-gated calcium channels in neurological and psychiatric diseases. Nat Rev Drug Discov. 2016;15(1):19–34. doi: 10.1038/nrd.2015.5. [DOI] [PubMed] [Google Scholar]
- 30.Striessnig J, Ortner NJ, Pinggera A. Pharmacology of L-type calcium channels: novel drugs for old targets? Curr Mol Pharmacol. 2015;8(2):110–122. doi: 10.2174/1874467208666150507105845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ament SA, Szelinger S, Glusman G, et al. Rare variants in neuronal excitability genes influence risk for bipolar disorder. Proc Natl Acad Sci U S A. 2015;112(11):3576–3581. doi: 10.1073/pnas.1424958112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nyegaard M, Demontis D, Foldager L, et al. CACNA1C (rs1006737) is associated with schizophrenia. Mol Psychiatry. 2010;15(2):119–121. doi: 10.1038/mp.2009.69. [DOI] [PubMed] [Google Scholar]
- 33.Rao S, Yao Y, Zheng C, et al. Common variants in CACNA1C and MDD susceptibility: a comprehensive meta-analysis. Am J Med Genet B Neuropsychiatr Genet. 2016;171(6):896–903. doi: 10.1002/ajmg.b.32466. [DOI] [PubMed] [Google Scholar]
- 34.Li J, Zhao L, You Y, et al. Schizophrenia related variants in CACNA1C also confer risk of autism. PLOS ONE. 2015;10(7):e0133247. doi: 10.1371/journal.pone.0133247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cross-Disorder Group of the Psychiatric Genomics Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet 381(9875), 1371-1379 (2013). [DOI] [PMC free article] [PubMed]
- 36.Zhang F, Lupski JR. Non-coding genetic variants in human disease. Hum Mol Genet. 2015;24(R1):R102–110. doi: 10.1093/hmg/ddv259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roussos P, Mitchell AC, Voloudakis G, et al. A role for noncoding variation in schizophrenia. Cell Rep. 2014;9(4):1417–1429. doi: 10.1016/j.celrep.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eckart N, Song Q, Yang R, et al. Functional characterization of schizophrenia-associated variation in CACNA1C. PLOS ONE. 2016;11(6):e0157086. doi: 10.1371/journal.pone.0157086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bigos KL, Mattay VS, Callicott JH, et al. Genetic variation in CACNA1C affects brain circuitries related to mental illness. Arch Gen Psychiatry. 2010;67(9):939–945. doi: 10.1001/archgenpsychiatry.2010.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yoshimizu T, Pan JQ, Mungenast AE, et al. Functional implications of a psychiatric risk variant within CACNA1C in induced human neurons. Mol Psychiatry. 2015;20(2):162–169. doi: 10.1038/mp.2014.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gershon ES, Grennan K, Busnello J, et al. A rare mutation of CACNA1C in a patient with bipolar disorder, and decreased gene expression associated with a bipolar-associated common SNP of CACNA1C in brain. Mol Psychiatry. 2014;19(8):890–894. doi: 10.1038/mp.2013.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.International Schizophrenia C, Purcell SM, Wray NR, et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature. 2009;460(7256):748–752. doi: 10.1038/nature08185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Page KM, Heblich F, Margas W, et al. N terminus is key to the dominant negative suppression of Ca(V)2 calcium channels: implications for episodic ataxia type 2. J Biol Chem. 2010;285(2):835–844. doi: 10.1074/jbc.M109.065045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Page KM, Heblich F, Davies A, et al. Dominant-negative calcium channel suppression by truncated constructs involves a kinase implicated in the unfolded protein response. J Neurosci. 2004;24(23):5400–5409. doi: 10.1523/JNEUROSCI.0553-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mezghrani A, Monteil A, Watschinger K, et al. A destructive interaction mechanism accounts for dominant-negative effects of misfolded mutants of voltage-gated calcium channels. J Neurosci. 2008;28(17):4501–4511. doi: 10.1523/JNEUROSCI.2844-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Splawski I, Timothy KW, Sharpe LM, et al. Ca(V)1.2 calcium channel dysfunction causes a multisystem disorder including arrhythmia and autism. Cell. 2004;119(1):19–31. doi: 10.1016/j.cell.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 47.Gillis J, Burashnikov E, Antzelevitch C, et al. Long QT, syndactyly, joint contractures, stroke and novel CACNA1C mutation: expanding the spectrum of Timothy syndrome. Am J Med Genet A. 2012;158A(1):182–187. doi: 10.1002/ajmg.a.34355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Splawski I, Timothy KW, Decher N, et al. Severe arrhythmia disorder caused by cardiac L-type calcium channel mutations. Proc Natl Acad Sci U S A. 2005;102(23):8089–8096. doi: 10.1073/pnas.0502506102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ross J, Gedvilaite E, Badner JA, et al. A rare variant in CACNA1D segregates with 7 bipolar I disorder cases in a large pedigree. Mol Neuropsychiatry. 2016;2(3):145–150. doi: 10.1159/000448041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guan F, Li L, Qiao C, et al. Evaluation of genetic susceptibility of common variants in CACNA1D with schizophrenia in Han Chinese. Sci Rep. 2015;5:12935. doi: 10.1038/srep12935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martinez-Rivera A, Hao J, Tropea TF, et al. Enhancing VTA Cav1.3 L-type Ca2+ channel activity promotes cocaine and mood-related behaviors via overlapping AMPA receptor mechanisms in the nucleus accumbens. Mol Psychiatry 2017 Feb 14 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 52.Iossifov I, O'Roak BJ, Sanders SJ, et al. The contribution of de novo coding mutations to autism spectrum disorder. Nature. 2014;515(7526):216–221. doi: 10.1038/nature13908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.O'Roak BJ, Vives L, Girirajan S, et al. Sporadic autism exomes reveal a highly interconnected protein network of de novo mutations. Nature. 2012;485(7397):246–250. doi: 10.1038/nature10989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Limpitikul WB, Dick IE, Ben-Johny M, Yue DT. An autism-associated mutation in CaV1.3 channels has opposing effects on voltage- and Ca(2+)-dependent regulation. Sci Rep 6, 27235 (2016). [DOI] [PMC free article] [PubMed]
- 55.Olson PA, Tkatch T, Hernandez-Lopez S, et al. G-protein-coupled receptor modulation of striatal CaV1.3 L-type Ca2+ channels is dependent on a Shank-binding domain. J Neurosci 25(5), 1050-1062 (2005). [DOI] [PMC free article] [PubMed]
- 56.Berkefeld H, Fakler B. Repolarizing responses of BKCa-Cav complexes are distinctly shaped by their Cav subunits. J Neurosci. 2008;28(33):8238–8245. doi: 10.1523/JNEUROSCI.2274-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Berkefeld H, Sailer CA, Bildl W, et al. BKCa-Cav channel complexes mediate rapid and localized Ca2+-activated K+ signaling. Science. 2006;314(5799):615–620. doi: 10.1126/science.1132915. [DOI] [PubMed] [Google Scholar]
- 58.Goodnick PJ. Treatment of mania: relationship between response to verapamil and changes in plasma calcium and magnesium levels. South Med J. 1996;89(2):225–226. doi: 10.1097/00007611-199602000-00014. [DOI] [PubMed] [Google Scholar]
- 59.Wisner KL, Peindl KS, Perel JM, Hanusa BH, Piontek CM, Baab S. Verapamil treatment for women with bipolar disorder. Biol Psychiatry. 2002;51(9):745–752. doi: 10.1016/S0006-3223(01)01338-5. [DOI] [PubMed] [Google Scholar]
- 60.Lenzi A, Marazziti D, Raffaelli S, Cassano GB. Effectiveness of the combination verapamil and chlorpromazine in the treatment of severe manic or mixed patients. Prog Neuropsychopharmacol Biol Psychiatry. 1995;19(3):519–528. doi: 10.1016/0278-5846(95)00033-R. [DOI] [PubMed] [Google Scholar]
- 61.Barton BM, Gitlin MJ. Verapamil in treatment-resistant mania: an open trial. J Clin Psychopharmacol. 1987;7(2):101–103. doi: 10.1097/00004714-198704000-00011. [DOI] [PubMed] [Google Scholar]
- 62.Garza-Trevino ES, Overall JE, Hollister LE. Verapamil versus lithium in acute mania. Am J Psychiatry. 1992;149(1):121–122. doi: 10.1176/ajp.149.1.121. [DOI] [PubMed] [Google Scholar]
- 63.Giannini AJ, Taraszewski R, Loiselle RH. Verapamil and lithium in maintenance therapy of manic patients. J Clin Pharmacol. 1987;27(12):980–982. doi: 10.1002/j.1552-4604.1987.tb05600.x. [DOI] [PubMed] [Google Scholar]
- 64.Dubovsky SL, Franks RD, Allen S. Verapamil: a new antimanic drug with potential interactions with lithium. J Clin Psychiatry. 1987;48(9):371–372. [PubMed] [Google Scholar]
- 65.Solomon L, Williamson P. Verapamil in bipolar illness. Can J Psychiatry. 1986;31(5):442–444. doi: 10.1177/070674378603100512. [DOI] [PubMed] [Google Scholar]
- 66.Gitlin MJ, Weiss J. Verapamil as maintenance treatment in bipolar illness: a case report. J Clin Psychopharmacol. 1984;4(6):341–343. doi: 10.1097/00004714-198412000-00009. [DOI] [PubMed] [Google Scholar]
- 67.Jacques RM, Cox SJ. Verapamil in major (psychotic) depression. Br J Psychiatry. 1991;158:124–125. doi: 10.1192/bjp.158.1.124. [DOI] [PubMed] [Google Scholar]
- 68.Dubovsky SL, Franks RD, Allen S, Murphy J. Calcium antagonists in mania: a double-blind study of verapamil. Psychiatry Res. 1986;18(4):309–320. doi: 10.1016/0165-1781(86)90016-8. [DOI] [PubMed] [Google Scholar]
- 69.Giannini AJ, Houser WL, Jr, Loiselle RH, Giannini MC, Price WA. Antimanic effects of verapamil. Am J Psychiatry. 1984;141(12):1602–1603. doi: 10.1176/ajp.141.12.1602. [DOI] [PubMed] [Google Scholar]
- 70.Mallinger AG, Thase ME, Haskett R, et al. Verapamil augmentation of lithium treatment improves outcome in mania unresponsive to lithium alone: preliminary findings and a discussion of therapeutic mechanisms. Bipolar Disord. 2008;10(8):856–866. doi: 10.1111/j.1399-5618.2008.00636.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Janicak PG, Sharma RP, Pandey G, Davis JM. Verapamil for the treatment of acute mania: a double-blind, placebo-controlled trial. Am J Psychiatry. 1998;155(7):972–973. doi: 10.1176/ajp.155.7.972. [DOI] [PubMed] [Google Scholar]
- 72.Hoschl C, Kozeny J. Verapamil in affective disorders: a controlled, double-blind study. Biol Psychiatry. 1989;25(2):128–140. doi: 10.1016/0006-3223(89)90157-1. [DOI] [PubMed] [Google Scholar]
- 73.Ried LD, Tueth MJ, Handberg E, Kupfer S, Pepine CJ, Invest Study Group A Study of Antihypertensive Drugs and Depressive Symptoms (SADD-Sx) in patients treated with a calcium antagonist versus an atenolol hypertension Treatment Strategy in the International Verapamil SR-Trandolapril Study (INVEST) Psychosom Med. 2005;67(3):398–406. doi: 10.1097/01.psy.0000160468.69451.7f. [DOI] [PubMed] [Google Scholar]
- 74.Pazzaglia PJ, Post RM, Ketter TA, et al. Nimodipine monotherapy and carbamazepine augmentation in patients with refractory recurrent affective illness. J Clin Psychopharmacol. 1998;18(5):404–413. doi: 10.1097/00004714-199810000-00009. [DOI] [PubMed] [Google Scholar]
- 75.Pazzaglia PJ, Post RM, Ketter TA, George MS, Marangell LB. Preliminary controlled trial of nimodipine in ultra-rapid cycling affective dysregulation. Psychiatry Res. 1993;49(3):257–272. doi: 10.1016/0165-1781(93)90066-P. [DOI] [PubMed] [Google Scholar]
- 76.Brunet G, Cerlich B, Robert P, Dumas S, Souetre E, Darcourt G. Open trial of a calcium antagonist, nimodipine, in acute mania. Clin Neuropharmacol. 1990;13(3):224–228. doi: 10.1097/00002826-199006000-00004. [DOI] [PubMed] [Google Scholar]
- 77.Grunze H, Walden J, Wolf R, Berger M. Combined treatment with lithium and nimodipine in a bipolar I manic syndrome. Prog Neuropsychopharmacol Biol Psychiatry. 1996;20(3):419–426. doi: 10.1016/0278-5846(96)00006-1. [DOI] [PubMed] [Google Scholar]
- 78.Davanzo PA, Krah N, Kleiner J, McCracken J. Nimodipine treatment of an adolescent with ultradian cycling bipolar affective illness. J Child Adolesc Psychopharmacol. 1999;9(1):51–61. doi: 10.1089/cap.1999.9.51. [DOI] [PubMed] [Google Scholar]
- 79.Caillard V. Treatment of mania using a calcium antagonist—preliminary trial. Neuropsychobiology. 1985;14(1):23–26. doi: 10.1159/000118196. [DOI] [PubMed] [Google Scholar]
- 80.Silverstone PH, Birkett L. Diltiazem as augmentation therapy in patients with treatment-resistant bipolar disorder: a retrospective study. J Psychiatry Neurosci. 2000;25(3):276–280. [PMC free article] [PubMed] [Google Scholar]
- 81.Hullett FJ, Potkin SG, Levy AB, Ciasca R. Depression associated with nifedipine-induced calcium channel blockade. Am J Psychiatry. 1988;145(10):1277–1279. doi: 10.1176/ajp.145.10.1277. [DOI] [PubMed] [Google Scholar]
- 82.Price WA, Heil D. Treatment of the negative symptoms of schizophrenia with verapamil. Jefferson Journal of Psychiatry 5(1) (1987).
- 83.Price WA. Antipsychotic effects of verapamil in schizophrenia. Hillside J Clin Psychiatry. 1987;9(2):225–230. [PubMed] [Google Scholar]
- 84.Uhr SB, Jackson K, Berger PA, Csernansky JG. Effects of verapamil administration on negative symptoms of chronic schizophrenia. Psychiatry Res. 1988;23(3):351–352. doi: 10.1016/0165-1781(88)90027-3. [DOI] [PubMed] [Google Scholar]
- 85.Schwartz BL, Fay-McCarthy M, Kendrick K, Rosse RB, Deutsch SI. Effects of nifedipine, a calcium channel antagonist, on cognitive function in schizophrenic patients with tardive dyskinesia. Clin Neuropharmacol. 1997;20(4):364–370. doi: 10.1097/00002826-199708000-00009. [DOI] [PubMed] [Google Scholar]
- 86.Bartko G, Horvath S, Zador G, Frecska E. Effects of adjunctive verapamil administration in chronic schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry. 1991;15(3):343–349. doi: 10.1016/0278-5846(91)90065-9. [DOI] [PubMed] [Google Scholar]
- 87.Pickar D, Wolkowitz OM, Doran AR, et al. Clinical and biochemical effects of verapamil administration to schizophrenic patients. Arch Gen Psychiatry. 1987;44(2):113–118. doi: 10.1001/archpsyc.1987.01800140015002. [DOI] [PubMed] [Google Scholar]
- 88.Grebb JA, Shelton RC, Taylor EH, Bigelow LB. A negative, double-blind, placebo-controlled, clinical trial of verapamil in chronic schizophrenia. Biol Psychiatry. 1986;21(7):691–694. doi: 10.1016/0006-3223(86)90132-0. [DOI] [PubMed] [Google Scholar]
- 89.Stedman TJ, Whiteford HA, Eyles D, Welham JL, Pond SM. Effects of nifedipine on psychosis and tardive dyskinesia in schizophrenic patients. J Clin Psychopharmacol. 1991;11(1):43–47. doi: 10.1097/00004714-199102000-00006. [DOI] [PubMed] [Google Scholar]
- 90.Suddath RL, Straw GM, Freed WJ, Bigelow LB, Kirch DG, Wyatt RJ. A clinical trial of nifedipine in schizophrenia and tardive dyskinesia. Pharmacol Biochem Behav. 1991;39(3):743–745. doi: 10.1016/0091-3057(91)90157-W. [DOI] [PubMed] [Google Scholar]
- 91.Kosten TR, Woods SW, Rosen MI, Pearsall HR. Interactions of cocaine with nimodipine: a brief report. Am J Addict. 1999;8(1):77–81. doi: 10.1080/105504999306117. [DOI] [PubMed] [Google Scholar]
- 92.Sofuoglu M, Singha A, Kosten TR, McCance-Katz FE, Petrakis I, Oliveto A. Effects of naltrexone and isradipine, alone or in combination, on cocaine responses in humans. Pharmacol Biochem Behav. 2003;75(4):801–808. doi: 10.1016/S0091-3057(03)00157-6. [DOI] [PubMed] [Google Scholar]
- 93.Roache JD, Johnson BA, Ait-Daoud N, et al. Effects of repeated-dose isradipine on the abuse liability of cocaine. Exp Clin Psychopharmacol. 2005;13(4):319–326. doi: 10.1037/1064-1297.13.4.319. [DOI] [PubMed] [Google Scholar]
- 94.Rosse RB, Alim TN, Fay-McCarthy M, et al. Nimodipine pharmacotherapeutic adjuvant therapy for inpatient treatment of cocaine dependence. Clin Neuropharmacol. 1994;17(4):348–358. doi: 10.1097/00002826-199408000-00007. [DOI] [PubMed] [Google Scholar]
- 95.Muntaner C, Kumor KM, Nagoshi C, Jaffe JH. Effects of nifedipine pretreatment on subjective and cardiovascular responses to intravenous cocaine in humans. Psychopharmacology (Berl) 1991;105(1):37–41. doi: 10.1007/BF02316861. [DOI] [PubMed] [Google Scholar]
- 96.Malcolm R, Brady KT, Moore J, Kajdasz D. Amlodipine treatment of cocaine dependence. J Psychoactive Drugs. 1999;31(2):117–120. doi: 10.1080/02791072.1999.10471733. [DOI] [PubMed] [Google Scholar]
- 97.Johnson BA, Roache JD, Ait-Daoud N, Wells LT, Mauldin JB. Effects of isradipine on cocaine-induced subjective mood. J Clin Psychopharmacol. 2004;24(2):180–191. doi: 10.1097/01.jcp.0000115662.45074.c3. [DOI] [PubMed] [Google Scholar]
- 98.Vaupel DB, Lange WR, London ED. Effects of verapamil on morphine-induced euphoria, analgesia and respiratory depression in humans. J Pharmacol Exp Ther. 1993;267(3):1386–1394. [PubMed] [Google Scholar]
- 99.Hasegawa AE, Zacny JP. The influence of three L-type calcium channel blockers on morphine effects in healthy volunteers. Anesth Analg. 1997;85(3):633–638. doi: 10.1213/00000539-199709000-00026. [DOI] [PubMed] [Google Scholar]
- 100.Silverstone PH, Attenburrow MJ, Robson P. The calcium channel antagonist nifedipine causes confusion when used to treat opiate withdrawal in morphine-dependent patients. Int Clin Psychopharmacol. 1992;7(2):87–90. [PubMed] [Google Scholar]
- 101.Zacny JP, Yajnik S. Effects of calcium channel inhibitors on ethanol effects and pharmacokinetics in healthy volunteers. Alcohol. 1993;10(6):505–509. doi: 10.1016/0741-8329(93)90074-X. [DOI] [PubMed] [Google Scholar]
- 102.Rush CR, Pazzaglia PJ. Pretreatment with isradipine, a calcium-channel blocker, does not attenuate the acute behavioral effects of ethanol in humans. Alcohol Clin Exp Res. 1998;22(2):539–547. doi: 10.1111/j.1530-0277.1998.tb03686.x. [DOI] [PubMed] [Google Scholar]
- 103.Perez-Reyes M, White WR, Hicks RE. Interaction between ethanol and calcium channel blockers in humans. Alcohol Clin Exp Res. 1992;16(4):769–775. doi: 10.1111/j.1530-0277.1992.tb00676.x. [DOI] [PubMed] [Google Scholar]
- 104.Altamura AC, Regazzetti MG, Porta M. Nimodipine in human alcohol withdrawal syndrome--an open study. Eur Neuropsychopharmacol. 1990;1(1):37–40. doi: 10.1016/0924-977X(90)90008-X. [DOI] [PubMed] [Google Scholar]
- 105.Waltereit R, Mannhardt S, Nescholta S, Maser-Gluth C, Bartsch D. Selective and protracted effect of nifedipine on fear memory extinction correlates with induced stress response. Learn Mem. 2008;15(5):348–356. doi: 10.1101/lm.808608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Busquet P, Hetzenauer A, Sinnegger-Brauns MJ, Striessnig J, Singewald N. Role of L-type Ca2+ channel isoforms in the extinction of conditioned fear. Learn Mem. 2008;15(5):378–386. doi: 10.1101/lm.886208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bergson P, Lipkind G, Lee SP, Duban ME, Hanck DA. Verapamil block of T-type calcium channels. Mol Pharmacol. 2011;79(3):411–419. doi: 10.1124/mol.110.069492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhang S, Zhou Z, Gong Q, Makielski JC, January CT. Mechanism of block and identification of the verapamil binding domain to HERG potassium channels. Circ Res. 1999;84(9):989–998. doi: 10.1161/01.RES.84.9.989. [DOI] [PubMed] [Google Scholar]
- 109.Catacuzzeno L, Trequattrini C, Petris A, Franciolini F. Mechanism of verapamil block of a neuronal delayed rectifier K channel: active form of the blocker and location of its binding domain. Br J Pharmacol. 1999;126(8):1699–1706. doi: 10.1038/sj.bjp.0702477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Harper AA, Catacuzzeno L, Trequattrini C, Petris A, Franciolini F. Verapamil block of large-conductance Ca-activated K channels in rat aortic myocytes. J Membr Biol. 2001;179(2):103–111. doi: 10.1007/s002320010041. [DOI] [PubMed] [Google Scholar]
- 111.Motulsky HJ, Snavely MD, Hughes RJ, Insel PA. Interaction of verapamil and other calcium channel blockers with alpha 1- and alpha 2-adrenergic receptors. Circ Res. 1983;52(2):226–231. doi: 10.1161/01.RES.52.2.226. [DOI] [PubMed] [Google Scholar]
- 112.Marzolini C, Paus E, Buclin T, Kim RB. Polymorphisms in human MDR1 (P-glycoprotein): recent advances and clinical relevance. Clin Pharmacol Ther. 2004;75(1):13–33. doi: 10.1016/j.clpt.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 113.Pauli-Magnus C, von Richter O, Burk O, et al. Characterization of the major metabolites of verapamil as substrates and inhibitors of P-glycoprotein. J Pharmacol Exp Ther. 2000;293(2):376–382. [PubMed] [Google Scholar]
- 114.Loscher W, Luna-Tortos C, Romermann K, Fedrowitz M. Do ATP-binding cassette transporters cause pharmacoresistance in epilepsy? Problems and approaches in determining which antiepileptic drugs are affected. Curr Pharm Des. 2011;17(26):2808–2828. doi: 10.2174/138161211797440212. [DOI] [PubMed] [Google Scholar]
- 115.Raderer M, Scheithauer W. Clinical trials of agents that reverse multidrug resistance. A literature review. Cancer. 1993;72(12):3553–3563. doi: 10.1002/1097-0142(19931215)72:12<3553::AID-CNCR2820721203>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 116.Cipriani A, Saunders K, Attenburrow MJ, et al. A systematic review of calcium channel antagonists in bipolar disorder and some considerations for their future development. Mol Psychiatry. 2016;21(10):1324–1332. doi: 10.1038/mp.2016.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Casamassima F, Hay AC, Benedetti A, Lattanzi L, Cassano GB, Perlis RH. L-type calcium channels and psychiatric disorders: a brief review. Am J Med Genet B Neuropsychiatr Genet. 2010;153B(8):1373–1390. doi: 10.1002/ajmg.b.31122. [DOI] [PubMed] [Google Scholar]
- 118.Deisseroth K, Heist EK, Tsien RW. Translocation of calmodulin to the nucleus supports CREB phosphorylation in hippocampal neurons. Nature. 1998;392(6672):198–202. doi: 10.1038/32448. [DOI] [PubMed] [Google Scholar]
- 119.Ma H, Groth RD, Cohen SM, et al. gammaCaMKII shuttles Ca(2)(+)/CaM to the nucleus to trigger CREB phosphorylation and gene expression. Cell 159(2), 281-294 (2014). [DOI] [PMC free article] [PubMed]
- 120.Wheeler DG, Barrett CF, Groth RD, Safa P, Tsien RW. CaMKII locally encodes L-type channel activity to signal to nuclear CREB in excitation-transcription coupling. J Cell Biol. 2008;183(5):849–863. doi: 10.1083/jcb.200805048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cohen SM, Li B, Tsien RW, Ma H. Evolutionary and functional perspectives on signaling from neuronal surface to nucleus. Biochem Biophys Res Commun. 2015;460(1):88–99. doi: 10.1016/j.bbrc.2015.02.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ma H, Li B, Tsien RW. Distinct roles of multiple isoforms of CaMKII in signaling to the nucleus. Biochim Biophys Acta. 2015;1853(9):1953–1957. doi: 10.1016/j.bbamcr.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wu GY, Deisseroth K, Tsien RW. Activity-dependent CREB phosphorylation: convergence of a fast, sensitive calmodulin kinase pathway and a slow, less sensitive mitogen-activated protein kinase pathway. Proc Natl Acad Sci U S A. 2001;98(5):2808–2813. doi: 10.1073/pnas.051634198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wu GY, Deisseroth K, Tsien RW. Spaced stimuli stabilize MAPK pathway activation and its effects on dendritic morphology. Nat Neurosci. 2001;4(2):151–158. doi: 10.1038/83976. [DOI] [PubMed] [Google Scholar]
- 125.Dolmetsch RE, Pajvani U, Fife K, Spotts JM, Greenberg ME. Signaling to the nucleus by an L-type calcium channel-calmodulin complex through the MAP kinase pathway. Science. 2001;294(5541):333–339. doi: 10.1126/science.1063395. [DOI] [PubMed] [Google Scholar]
- 126.Hofmann HA. Functional genomics of neural and behavioral plasticity. J Neurobiol. 2003;54(1):272–282. doi: 10.1002/neu.10172. [DOI] [PubMed] [Google Scholar]
- 127.Ortega-Martinez S. A new perspective on the role of the CREB family of transcription factors in memory consolidation via adult hippocampal neurogenesis. Front Mol Neurosci. 2015;8:46. doi: 10.3389/fnmol.2015.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Nestler EJ. Cellular basis of memory for addiction. Dialogues Clin Neurosci. 2013;15(4):431–443. doi: 10.31887/DCNS.2013.15.4/enestler. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Harrington AJ, Raissi A, Rajkovich K, et al. MEF2C regulates cortical inhibitory and excitatory synapses and behaviors relevant to neurodevelopmental disorders. Elife. 2016;5:e20059. doi: 10.7554/eLife.20059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lombardi LM, Baker SA, Zoghbi HY. MECP2 disorders: from the clinic to mice and back. J Clin Invest. 2015;125(8):2914–2923. doi: 10.1172/JCI78167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Mao Z, Bonni A, Xia F, Nadal-Vicens M, Greenberg ME. Neuronal activity-dependent cell survival mediated by transcription factor MEF2. Science. 1999;286(5440):785–790. doi: 10.1126/science.286.5440.785. [DOI] [PubMed] [Google Scholar]
- 132.Tian Y, Voineagu I, Pasca SP, et al. Alteration in basal and depolarization induced transcriptional network in iPSC derived neurons from Timothy syndrome. Genome Med. 2014;6(10):75. doi: 10.1186/s13073-014-0075-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Chen WG, Chang Q, Lin Y, et al. Derepression of BDNF transcription involves calcium-dependent phosphorylation of MeCP2. Science. 2003;302(5646):885–889. doi: 10.1126/science.1086446. [DOI] [PubMed] [Google Scholar]
- 134.Pfeiffer BE, Zang T, Wilkerson JR, et al. Fragile X mental retardation protein is required for synapse elimination by the activity-dependent transcription factor MEF2. Neuron. 2010;66(2):191–197. doi: 10.1016/j.neuron.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Murphy JG, Sanderson JL, Gorski JA, et al. AKAP-anchored PKA maintains neuronal L-type calcium channel activity and NFAT transcriptional signaling. Cell Rep. 2014;7(5):1577–1588. doi: 10.1016/j.celrep.2014.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Graef IA, Mermelstein PG, Stankunas K, et al. L-type calcium channels and GSK-3 regulate the activity of NF-ATc4 in hippocampal neurons. Nature. 1999;401(6754):703–708. doi: 10.1038/44378. [DOI] [PubMed] [Google Scholar]
- 137.Nurnberger JI, Jr, Koller DL, Jung J, et al. Identification of pathways for bipolar disorder: a meta-analysis. JAMA Psychiatry. 2014;71(6):657–664. doi: 10.1001/jamapsychiatry.2014.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Darby MM, Yolken RH, Sabunciyan S. Consistently altered expression of gene sets in postmortem brains of individuals with major psychiatric disorders. Transl Psychiatry. 2016;6(9):e890. doi: 10.1038/tp.2016.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Hertzberg L, Katsel P, Roussos P, Haroutunian V, Domany E. Integration of gene expression and GWAS results supports involvement of calcium signaling in Schizophrenia. Schizophr Res. 2015;164(1-3):92–99. doi: 10.1016/j.schres.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 140.Wen Y, Alshikho MJ, Herbert MR. Pathway network analyses for autism reveal multisystem involvement, major overlaps with other diseases and convergence upon MAPK and calcium signaling. PLOS ONE. 2016;11(4):e0153329. doi: 10.1371/journal.pone.0153329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Focking M, Lopez LM, English JA, et al. Proteomic and genomic evidence implicates the postsynaptic density in schizophrenia. Mol Psychiatry. 2015;20(4):424–432. doi: 10.1038/mp.2014.63. [DOI] [PubMed] [Google Scholar]
- 142.Focking M, Dicker P, Lopez LM, et al. Proteomic analysis of the postsynaptic density implicates synaptic function and energy pathways in bipolar disorder. Transl Psychiatry. 2016;6(11):e959. doi: 10.1038/tp.2016.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Pinto D, Delaby E, Merico D, et al. Convergence of genes and cellular pathways dysregulated in autism spectrum disorders. Am J Hum Genet. 2014;94(5):677–694. doi: 10.1016/j.ajhg.2014.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Nho K, Ramanan VK, Horgusluoglu E, et al. Comprehensive gene- and pathway-based analysis of depressive symptoms in older adults. J Alzheimers Dis. 2015;45(4):1197–1206. doi: 10.3233/JAD-148009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Kerner B, Rao AR, Christensen B, Dandekar S, Yourshaw M, Nelson SF. Rare genomic variants link bipolar disorder with anxiety disorders to CREB-regulated intracellular signaling pathways. Front Psychiatry. 2013;4:154. doi: 10.3389/fpsyt.2013.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Wek RC, Cavener DR. Translational control and the unfolded protein response. Antioxid Redox Signal. 2007;9(12):2357–2371. doi: 10.1089/ars.2007.1764. [DOI] [PubMed] [Google Scholar]
- 147.Krey JF, Paşca SP, Shcheglovitov A, et al. Timothy syndrome is associated with activity-dependent dendritic retraction in rodent and human neurons. Nat Neurosci. 2013;16(2):201–209. doi: 10.1038/nn.3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Pasca SP, Portmann T, Voineagu I, et al. Using iPSC-derived neurons to uncover cellular phenotypes associated with Timothy syndrome. Nat Med. 2011;17(12):1657–1662. doi: 10.1038/nm.2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lee AS, De Jesus-Cortes H, Kabir ZD, et al. The neuropsychiatric disease-associated gene cacna1c mediates survival of young hippocampal neurons. eNeuro 3(2) (2016). [DOI] [PMC free article] [PubMed]
- 150.Kabir ZD, Che A, D F et al. Rescue of impaired sociability and anxietylike behavior in adult cacna1cdeficient mice by pharmacologically targeting eIF2α. Molecular Psychiatry (2017, in press). [DOI] [PMC free article] [PubMed]
- 151.Mullins C, Fishell G, Tsien RW. Unifying views of autism spectrum disorders: a consideration of autoregulatory feedback loops. Neuron. 2016;89(6):1131–1156. doi: 10.1016/j.neuron.2016.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kabir ZD, Lee AS, Burgdorf CE, et al. Cacna1c in the prefrontal cortex regulates depression-related behaviors via REDD1. Neuropsychopharmacology 2017 Jan 4 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 153.Lee AS, Ra S, Rajadhyaksha AM, et al. Forebrain elimination of cacna1c mediates anxiety-like behavior in mice. Mol Psychiatry. 2012;17(11):1054–1055. doi: 10.1038/mp.2012.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hess P, Lansman JB, Tsien RW. Different modes of Ca channel gating behaviour favoured by dihydropyridine Ca agonists and antagonists. Nature. 1984;311(5986):538–544. doi: 10.1038/311538a0. [DOI] [PubMed] [Google Scholar]
- 155.Seisenberger C, Specht V, Welling A, et al. Functional embryonic cardiomyocytes after disruption of the L-type alpha1C (Cav1.2) calcium channel gene in the mouse. J Biol Chem. 2000;275(50):39193–39199. doi: 10.1074/jbc.M006467200. [DOI] [PubMed] [Google Scholar]
- 156.Goonasekera SA, Hammer K, Auger-Messier M, et al. Decreased cardiac L-type Ca(2)(+) channel activity induces hypertrophy and heart failure in mice. J Clin Invest. 2012;122(1):280–290. doi: 10.1172/JCI58227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Dao DT, Mahon PB, Cai X, et al. Mood disorder susceptibility gene CACNA1C modifies mood-related behaviors in mice and interacts with sex to influence behavior in mice and diagnosis in humans. Biol Psychiatry. 2010;68(9):801–810. doi: 10.1016/j.biopsych.2010.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Bavley CC, Fischer DK, Rizzo BK, Rajadhyaksha AM. Cav1.2 channels mediate persistent chronic stress-induced behavioral deficits that are associated with prefrontal cortex activation of the p25/Cdk5-glucocorticoid receptor pathway. Neurobiol Stress. 2017;7:27–37. doi: 10.1016/j.ynstr.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sinnegger-Brauns MJ, Hetzenauer A, Huber IG, et al. Isoform-specific regulation of mood behavior and pancreatic beta cell and cardiovascular function by L-type Ca 2+ channels. J Clin Invest. 2004;113(10):1430–1439. doi: 10.1172/JCI20208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Giordano TP, Tropea TF, Satpute SS, et al. Molecular switch from L-type Ca v 1.3 to Ca v 1.2 Ca2+ channel signaling underlies long-term psychostimulant-induced behavioral and molecular plasticity. J Neurosci 30(50), 17051-17062 (2010). [DOI] [PMC free article] [PubMed]
- 161.Schierberl K, Hao J, Tropea TF, et al. Cav1.2 L-type Ca(2)(+) channels mediate cocaine-induced GluA1 trafficking in the nucleus accumbens, a long-term adaptation dependent on ventral tegmental area Ca(v)1.3 channels. J Neurosci 31(38), 13562-13575 (2011). [DOI] [PMC free article] [PubMed]
- 162.Kessler RC, Aguilar-Gaxiola S, Alonso J, et al. The global burden of mental disorders: an update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18(1):23–33. doi: 10.1017/S1121189X00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Erk S, Meyer-Lindenberg A, Linden DE, et al. Replication of brain function effects of a genome-wide supported psychiatric risk variant in the CACNA1C gene and new multi-locus effects. Neuroimage. 2014;94:147–154. doi: 10.1016/j.neuroimage.2014.03.007. [DOI] [PubMed] [Google Scholar]
- 164.Erk S, Meyer-Lindenberg A, Schnell K, et al. Brain function in carriers of a genome-wide supported bipolar disorder variant. Arch Gen Psychiatry. 2010;67(8):803–811. doi: 10.1001/archgenpsychiatry.2010.94. [DOI] [PubMed] [Google Scholar]
- 165.Roussos P, Giakoumaki SG, Georgakopoulos A, Robakis NK, Bitsios P. The CACNA1C and ANK3 risk alleles impact on affective personality traits and startle reactivity but not on cognition or gating in healthy males. Bipolar Disord. 2011;13(3):250–259. doi: 10.1111/j.1399-5618.2011.00924.x. [DOI] [PubMed] [Google Scholar]
- 166.Wang F, McIntosh AM, He Y, Gelernter J, Blumberg HP. The association of genetic variation in CACNA1C with structure and function of a frontotemporal system. Bipolar Disord. 2011;13(7-8):696–700. doi: 10.1111/j.1399-5618.2011.00963.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Dima D, Jogia J, Collier D, Vassos E, Burdick KE, Frangou S. Independent modulation of engagement and connectivity of the facial network during affect processing by CACNA1C and ANK3 risk genes for bipolar disorder. JAMA Psychiatry. 2013;70(12):1303–1311. doi: 10.1001/jamapsychiatry.2013.2099. [DOI] [PubMed] [Google Scholar]
- 168.Bader PL, Faizi M, Kim LH, et al. Mouse model of Timothy syndrome recapitulates triad of autistic traits. Proc Natl Acad Sci U S A. 2011;108(37):15432–15437. doi: 10.1073/pnas.1112667108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Kennedy DP, Adolphs R. The social brain in psychiatric and neurological disorders. Trends Cogn Sci. 2012;16(11):559–572. doi: 10.1016/j.tics.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.), (2013). Arlington, VA: American Psychiatric Association.
- 171.Grant BF, Hasin DS, Blanco C, et al. The epidemiology of social anxiety disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66(11):1351–1361. doi: 10.4088/JCP.v66n1102. [DOI] [PubMed] [Google Scholar]
- 172.Hidalgo RB, Barnett SD, Davidson JR. Social anxiety disorder in review: two decades of progress. Int J Neuropsychopharmacol. 2001;4(3):279–298. doi: 10.1017/S1461145701002504. [DOI] [PubMed] [Google Scholar]
- 173.Allsop SA, Vander Weele CM, Wichmann R, Tye KM. Optogenetic insights on the relationship between anxiety-related behaviors and social deficits. Front Behav Neurosci. 2014;8:241. doi: 10.3389/fnbeh.2014.00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Workman ER, Niere F, Raab-Graham KF. mTORC1-dependent protein synthesis underlying rapid antidepressant effect requires GABABR signaling. Neuropharmacology. 2013;73:192–203. doi: 10.1016/j.neuropharm.2013.05.037. [DOI] [PubMed] [Google Scholar]
- 175.Nandagopal N, Roux PP. Regulation of global and specific mRNA translation by the mTOR signaling pathway. Translation. 2015;3(1):e983402. doi: 10.4161/21690731.2014.983402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Costa-Mattioli M, Monteggia LM. mTOR complexes in neurodevelopmental and neuropsychiatric disorders. Nat Neurosci. 2013;16(11):1537–1543. doi: 10.1038/nn.3546. [DOI] [PubMed] [Google Scholar]
- 177.Gkogkas CG, Khoutorsky A, Ran I, et al. Autism-related deficits via dysregulated eIF4E-dependent translational control. Nature. 2013;493(7432):371–377. doi: 10.1038/nature11628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Santini E, Huynh TN, MacAskill AF, et al. Exaggerated translation causes synaptic and behavioural aberrations associated with autism. Nature. 2013;493(7432):411–415. doi: 10.1038/nature11782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Sato A, Kasai S, Kobayashi T, et al. Rapamycin reverses impaired social interaction in mouse models of tuberous sclerosis complex. Nat Commun. 2012;3:1292. doi: 10.1038/ncomms2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hwang SK, Lee JH, Yang JE, et al. Everolimus improves neuropsychiatric symptoms in a patient with tuberous sclerosis carrying a novel TSC2 mutation. Mol Brain. 2016;9(1):56. doi: 10.1186/s13041-016-0222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ricciardi S, Boggio EM, Grosso S, et al. Reduced AKT/mTOR signaling and protein synthesis dysregulation in a Rett syndrome animal model. Hum Mol Genet. 2011;20(6):1182–1196. doi: 10.1093/hmg/ddq563. [DOI] [PubMed] [Google Scholar]
- 182.Sidrauski C, McGeachy AM, Ingolia NT, Walter P. The small molecule ISRIB reverses the effects of eIF2alpha phosphorylation on translation and stress granule assembly. Elife 4 (2015). [DOI] [PMC free article] [PubMed]
- 183.Zimmerman HR, Beckelman B, Yang W, Ma T. Interactions between the eIF2a and mTORC1 signaling pathways. Program No. 126.02. 2016 Neuroscience Meeting Planner, San Diego, Society for Neuroscience, Online (2016).
- 184.Sidrauski C, Acosta-Alvear D, Khoutorsky A, et al. Pharmacological brake-release of mRNA translation enhances cognitive memory. Elife 2, e00498 (2013). [DOI] [PMC free article] [PubMed]
- 185.Hai T, Hartman MG. The molecular biology and nomenclature of the activating transcription factor/cAMP responsive element binding family of transcription factors: activating transcription factor proteins and homeostasis. Gene. 2001;273(1):1–11. doi: 10.1016/S0378-1119(01)00551-0. [DOI] [PubMed] [Google Scholar]
- 186.Mogilnicka E, Czyrak A, Maj J. Dihydropyridine calcium channel antagonists reduce immobility in the mouse behavioral despair test; antidepressants facilitate nifedipine action. Eur J Pharmacol. 1987;138(3):413–416. doi: 10.1016/0014-2999(87)90480-8. [DOI] [PubMed] [Google Scholar]
- 187.Cohen C, Perrault G, Sanger DJ. Assessment of the antidepressant-like effects of L-type voltage-dependent channel modulators. Behav Pharmacol. 1997;8(6-7):629–638. doi: 10.1097/00008877-199711000-00019. [DOI] [PubMed] [Google Scholar]
- 188.Li N, Lee B, Liu RJ, et al. mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science. 2010;329(5994):959–964. doi: 10.1126/science.1190287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Mogilnicka E, Czyrak A, Maj J. BAY K 8644 enhances immobility in the mouse behavioral despair test, an effect blocked by nifedipine. Eur J Pharmacol. 1988;151(2):307–311. doi: 10.1016/0014-2999(88)90813-8. [DOI] [PubMed] [Google Scholar]
- 190.Ota KT, Liu RJ, Voleti B, et al. REDD1 is essential for stress-induced synaptic loss and depressive behavior. Nat Med. 2014;20(5):531–535. doi: 10.1038/nm.3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Magno LA, Santana CV, Sacramento EK, et al. Genetic variations in FOXO3A are associated with Bipolar Disorder without confering vulnerability for suicidal behavior. J Affect Disord. 2011;133(3):633–637. doi: 10.1016/j.jad.2011.04.031. [DOI] [PubMed] [Google Scholar]
- 192.Wang H, Quirion R, Little PJ, et al. Forkhead box O transcription factors as possible mediators in the development of major depression. Neuropharmacology. 2015;99:527–537. doi: 10.1016/j.neuropharm.2015.08.020. [DOI] [PubMed] [Google Scholar]
- 193.Polter A, Yang S, Zmijewska AA, et al. Forkhead box, class O transcription factors in brain: regulation and behavioral manifestation. Biol Psychiatry. 2009;65(2):150–159. doi: 10.1016/j.biopsych.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Mao Z, Liu L, Zhang R, Li X. Lithium reduces FoxO3a transcriptional activity by decreasing its intracellular content. Biol Psychiatry. 2007;62(12):1423–1430. doi: 10.1016/j.biopsych.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 195.Millan MJ, Agid Y, Brune M, et al. Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov. 2012;11(2):141–168. doi: 10.1038/nrd3628. [DOI] [PubMed] [Google Scholar]
- 196.White JA, McKinney BC, John MC, Powers PA, Kamp TJ, Murphy GG. Conditional forebrain deletion of the L-type calcium channel Ca V 1.2 disrupts remote spatial memories in mice. Learn Mem. 2008;15(1):1–5. doi: 10.1101/lm.773208. [DOI] [PubMed] [Google Scholar]
- 197.Temme SJ, Bell RZ, Fisher GL, Murphy GG. Deletion of the mouse homolog of CACNA1C disrupts discrete forms of hippocampal-dependent memory and neurogenesis within the dentate gyrus. eNeuro, 3(6) (2016). [DOI] [PMC free article] [PubMed]
- 198.Moosmang S, Haider N, Klugbauer N, et al. Role of hippocampal Cav1.2 Ca2+ channels in NMDA receptor-independent synaptic plasticity and spatial memory. J Neurosci. 2005;25(43):9883–9892. doi: 10.1523/JNEUROSCI.1531-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Nicoll RA. A brief history of long-term potentiation. Neuron. 2017;93(2):281–290. doi: 10.1016/j.neuron.2016.12.015. [DOI] [PubMed] [Google Scholar]
- 200.Yau SY, Li A, So KF. Involvement of adult hippocampal neurogenesis in learning and forgetting. Neural Plast. 2015;2015:717958. doi: 10.1155/2015/717958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Deng W, Aimone JB, Gage FH. New neurons and new memories: how does adult hippocampal neurogenesis affect learning and memory? Nat Rev Neurosci. 2010;11(5):339–350. doi: 10.1038/nrn2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Waltz JA. The neural underpinnings of cognitive flexibility and their disruption in psychotic illness. Neuroscience. 2017;345:203–217. doi: 10.1016/j.neuroscience.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.LeDoux JE. Emotion circuits in the brain. Annu Rev Neurosci. 2000;23:155–184. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- 204.Pezze MA, Feldon J. Mesolimbic dopaminergic pathways in fear conditioning. Prog Neurobiol. 2004;74(5):301–320. doi: 10.1016/j.pneurobio.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 205.Singewald N, Schmuckermair C, Whittle N, Holmes A, Ressler KJ. Pharmacology of cognitive enhancers for exposure-based therapy of fear, anxiety and trauma-related disorders. Pharmacol Ther. 2015;149:150–190. doi: 10.1016/j.pharmthera.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Phillips ML, Drevets WC, Rauch SL, Lane R. Neurobiology of emotion perception I: The neural basis of normal emotion perception. Biol Psychiatry. 2003;54(5):504–514. doi: 10.1016/S0006-3223(03)00168-9. [DOI] [PubMed] [Google Scholar]
- 207.Cain CK, Blouin AM, Barad M. L-type voltage-gated calcium channels are required for extinction, but not for acquisition or expression, of conditional fear in mice. J Neurosci. 2002;22(20):9113–9121. doi: 10.1523/JNEUROSCI.22-20-09113.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Bauer EP, Schafe GE, LeDoux JE. NMDA receptors and L-type voltage-gated calcium channels contribute to long-term potentiation and different components of fear memory formation in the lateral amygdala. J Neurosci. 2002;22(12):5239–5249. doi: 10.1523/JNEUROSCI.22-12-05239.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Davis SE, Bauer EP. L-type voltage-gated calcium channels in the basolateral amygdala are necessary for fear extinction. J Neurosci. 2012;32(39):13582–13586. doi: 10.1523/JNEUROSCI.0809-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Langwieser N, Christel CJ, Kleppisch T, Hofmann F, Wotjak CT, Moosmang S. Homeostatic switch in hebbian plasticity and fear learning after sustained loss of Cav1.2 calcium channels. J Neurosci 30(25), 8367-8375 (2010). [DOI] [PMC free article] [PubMed]
- 211.McKinney BC, Sze W, White JA, Murphy GG. L-type voltage-gated calcium channels in conditioned fear: a genetic and pharmacological analysis. Learn Mem. 2008;15(5):326–334. doi: 10.1101/lm.893808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Barad M, Blouin AM, Cain CK. Like extinction, latent inhibition of conditioned fear in mice is blocked by systemic inhibition of L-type voltage-gated calcium channels. Learn Mem. 2004;11(5):536–539. doi: 10.1101/lm.78304. [DOI] [PubMed] [Google Scholar]
- 213.Shinnick-Gallagher P, McKernan MG, Xie J, Zinebi F. L-type voltage-gated calcium channels are involved in the in vivo and in vitro expression of fear conditioning. Ann N Y Acad Sci. 2003;985:135–149. doi: 10.1111/j.1749-6632.2003.tb07078.x. [DOI] [PubMed] [Google Scholar]
- 214.Weisskopf MG, Bauer EP, LeDoux JE. L-type voltage-gated calcium channels mediate NMDA-independent associative long-term potentiation at thalamic input synapses to the amygdala. J Neurosci. 1999;19(23):10512–10519. doi: 10.1523/JNEUROSCI.19-23-10512.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Lee O, Lee CJ, Choi S. Induction mechanisms for L-LTP at thalamic input synapses to the lateral amygdala: requirement of mGluR5 activation. Neuroreport. 2002;13(5):685–691. doi: 10.1097/00001756-200204160-00030. [DOI] [PubMed] [Google Scholar]
- 216.Pape HC, Pare D. Plastic synaptic networks of the amygdala for the acquisition, expression, and extinction of conditioned fear. Physiol Rev. 2010;90(2):419–463. doi: 10.1152/physrev.00037.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Meis S, Endres T, Lessmann V. Postsynaptic BDNF signalling regulates long-term potentiation at thalamo-amygdala afferents. J Physiol. 2012;590(1):193–208. doi: 10.1113/jphysiol.2011.220434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Ghosh A, Carnahan J, Greenberg ME. Requirement for BDNF in activity-dependent survival of cortical neurons. Science. 1994;263(5153):1618–1623. doi: 10.1126/science.7907431. [DOI] [PubMed] [Google Scholar]
- 219.Rattiner LM, Davis M, French CT, Ressler KJ. Brain-derived neurotrophic factor and tyrosine kinase receptor B involvement in amygdala-dependent fear conditioning. J Neurosci. 2004;24(20):4796–4806. doi: 10.1523/JNEUROSCI.5654-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Ou LC, Gean PW. Transcriptional regulation of brain-derived neurotrophic factor in the amygdala during consolidation of fear memory. Mol Pharmacol. 2007;72(2):350–358. doi: 10.1124/mol.107.034934. [DOI] [PubMed] [Google Scholar]
- 221.See V, Boutillier AL, Bito H, Loeffler JP. Calcium/calmodulin-dependent protein kinase type IV (CaMKIV) inhibits apoptosis induced by potassium deprivation in cerebellar granule neurons. FASEB J. 2001;15(1):134–144. doi: 10.1096/fj.00-0106com. [DOI] [PubMed] [Google Scholar]
- 222.Tao X, Finkbeiner S, Arnold DB, Shaywitz AJ, Greenberg ME. Ca2+ influx regulates BDNF transcription by a CREB family transcription factor-dependent mechanism. Neuron. 1998;20(4):709–726. doi: 10.1016/S0896-6273(00)81010-7. [DOI] [PubMed] [Google Scholar]
- 223.Pieper AA, Wu X, Han TW, et al. The neuronal PAS domain protein 3 transcription factor controls FGF-mediated adult hippocampal neurogenesis in mice. Proc Natl Acad Sci U S A. 2005;102(39):14052–14057. doi: 10.1073/pnas.0506713102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Pickard BS, Pieper AA, Porteous DJ, Blackwood DH, Muir WJ. The NPAS3 gene—emerging evidence for a role in psychiatric illness. Ann Med. 2006;38(6):439–448. doi: 10.1080/07853890600946500. [DOI] [PubMed] [Google Scholar]
- 225.Reif A, Schmitt A, Fritzen S, Lesch KP. Neurogenesis and schizophrenia: dividing neurons in a divided mind? Eur Arch Psychiatry Clin Neurosci. 2007;257(5):290–299. doi: 10.1007/s00406-007-0733-3. [DOI] [PubMed] [Google Scholar]
- 226.Pickard B. Progress in defining the biological causes of schizophrenia. Exp Rev Mol Med. 2011;13:e25. doi: 10.1017/S1462399411001955. [DOI] [PubMed] [Google Scholar]
- 227.Wu Q, Li Y, Xiao B. DISC1-related signaling pathways in adult neurogenesis of the hippocampus. Gene. 2013;518(2):223–230. doi: 10.1016/j.gene.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 228.Schreiber R, Newman-Tancredi A. Improving cognition in schizophrenia with antipsychotics that elicit neurogenesis through 5-HT(1A) receptor activation. Neurobiol Learn Mem. 2014;110:72–80. doi: 10.1016/j.nlm.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 229.Ohira K, Kobayashi K, Toyama K, et al. Synaptosomal-associated protein 25 mutation induces immaturity of the dentate granule cells of adult mice. Mol Brain. 2013;6:12. doi: 10.1186/1756-6606-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Le Strat Y, Ramoz N, Gorwood P. The role of genes involved in neuroplasticity and neurogenesis in the observation of a gene-environment interaction (GxE) in schizophrenia. Curr Mol Med. 2009;9(4):506–518. doi: 10.2174/156652409788167104. [DOI] [PubMed] [Google Scholar]
- 231.Knight HM, Walker R, James R, et al. GRIK4/KA1 protein expression in human brain and correlation with bipolar disorder risk variant status. Am J Med Genet B Neuropsychiatr Genet. 2012;159B(1):21–29. doi: 10.1002/ajmg.b.31248. [DOI] [PubMed] [Google Scholar]
- 232.Serafini G, Hayley S, Pompili M, et al. Hippocampal neurogenesis, neurotrophic factors and depression: possible therapeutic targets? CNS Neurol Disord Drug Targets. 2014;13(10):1708–1721. doi: 10.2174/1871527313666141130223723. [DOI] [PubMed] [Google Scholar]
- 233.Walker AK, Rivera PD, Wang Q, et al. The P7C3 class of neuroprotective compounds exerts antidepressant efficacy in mice by increasing hippocampal neurogenesis. Mol Psychiatry. 2015;20(4):500–508. doi: 10.1038/mp.2014.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Amiri A, Cho W, Zhou J, et al. Pten deletion in adult hippocampal neural stem/progenitor cells causes cellular abnormalities and alters neurogenesis. J Neurosci. 2012;32(17):5880–5890. doi: 10.1523/JNEUROSCI.5462-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Jolly LA, Homan CC, Jacob R, Barry S, Gecz J. The UPF3B gene, implicated in intellectual disability, autism, ADHD and childhood onset schizophrenia regulates neural progenitor cell behaviour and neuronal outgrowth. Hum Mol Genet. 2013;22(23):4673–4687. doi: 10.1093/hmg/ddt315. [DOI] [PubMed] [Google Scholar]
- 236.Cope EC, Briones BA, Brockett AT, et al. Immature neurons and radial glia, but not astrocytes or microglia, are altered in adult Cntnap2 and Shank3 mice, models of autism. eNeuro, 3(5) (2016). [DOI] [PMC free article] [PubMed]
- 237.Chen Z, Li X, Zhou J, et al. Accumulated quiescent neural stem cells in adult hippocampus of the mouse model for the MECP2 duplication syndrome. Sci Rep. 2017;7:41701. doi: 10.1038/srep41701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Dabe EC, Majdak P, Bhattacharya TK, Miller DS, Rhodes JS. Chronic D-amphetamine administered from childhood to adulthood dose-dependently increases the survival of new neurons in the hippocampus of male C57BL/6J mice. Neuroscience. 2013;231:125–135. doi: 10.1016/j.neuroscience.2012.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Sahay A, Scobie KN, Hill AS, et al. Increasing adult hippocampal neurogenesis is sufficient to improve pattern separation. Nature. 2011;472(7344):466–470. doi: 10.1038/nature09817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Hill AS, Sahay A, Hen R. Increasing adult hippocampal neurogenesis is sufficient to reduce anxiety and depression-like behaviors. Neuropsychopharmacology. 2015;40(10):2368–2378. doi: 10.1038/npp.2015.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Deisseroth K, Singla S, Toda H, Monje M, Palmer TD, Malenka RC. Excitation-neurogenesis coupling in adult neural stem/progenitor cells. Neuron. 2004;42(4):535–552. doi: 10.1016/S0896-6273(04)00266-1. [DOI] [PubMed] [Google Scholar]
- 242.Teh DB, Ishizuka T, Yawo H. Regulation of later neurogenic stages of adult-derived neural stem/progenitor cells by L-type Ca2+ channels. Dev Growth Differ. 2014;56(8):583–594. doi: 10.1111/dgd.12158. [DOI] [PubMed] [Google Scholar]
- 243.Pieper AA, Xie S, Capota E, et al. Discovery of a proneurogenic, neuroprotective chemical. Cell. 2010;142(1):39–51. doi: 10.1016/j.cell.2010.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Marschallinger J, Sah A, Schmuckermair C, et al. The L-type calcium channel Cav1.3 is required for proper hippocampal neurogenesis and cognitive functions. Cell Calcium 58(6), 606-616 (2015). [DOI] [PubMed]
- 245.Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006;59(12):1116–1127. doi: 10.1016/j.biopsych.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 246.Hill JL, Martinowich K. Activity-dependent signaling: influence on plasticity in circuits controlling fear-related behavior. Curr Opin Neurobiol. 2016;36:59–65. doi: 10.1016/j.conb.2015.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Martinowich K, Manji H, Lu B. New insights into BDNF function in depression and anxiety. Nat Neurosci. 2007;10(9):1089–1093. doi: 10.1038/nn1971. [DOI] [PubMed] [Google Scholar]
- 248.Lu B, Martinowich K. Cell biology of BDNF and its relevance to schizophrenia. Novartis Foundation symposium, 289, 119-129; discussion 129-135, 193-115 (2008). [DOI] [PMC free article] [PubMed]
- 249.Zheng F, Zhou X, Luo Y, Xiao H, Wayman G, Wang H. Regulation of brain-derived neurotrophic factor exon IV transcription through calcium responsive elements in cortical neurons. PLOS ONE. 2011;6(12):e28441. doi: 10.1371/journal.pone.0028441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Smrt RD, Eaves-Egenes J, Barkho BZ, et al. Mecp2 deficiency leads to delayed maturation and altered gene expression in hippocampal neurons. Neurobiol Dis. 2007;27(1):77–89. doi: 10.1016/j.nbd.2007.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Li H, Zhong X, Chau KF, et al. Cell cycle-linked MeCP2 phosphorylation modulates adult neurogenesis involving the Notch signalling pathway. Nat Commun. 2014;5:5601. doi: 10.1038/ncomms6601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Chen WG, West AE, Tao X, et al. Upstream stimulatory factors are mediators of Ca2+-responsive transcription in neurons. J Neurosci. 2003;23(7):2572–2581. doi: 10.1523/JNEUROSCI.23-07-02572.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Tao J, Hu K, Chang Q, et al. Phosphorylation of MeCP2 at Serine 80 regulates its chromatin association and neurological function. Proc Natl Acad Sci U S A. 2009;106(12):4882–4887. doi: 10.1073/pnas.0811648106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Tao X, West AE, Chen WG, Corfas G, Greenberg ME. A calcium-responsive transcription factor, CaRF, that regulates neuronal activity-dependent expression of BDNF. Neuron. 2002;33(3):383–395. doi: 10.1016/S0896-6273(01)00561-X. [DOI] [PubMed] [Google Scholar]
- 255.Chao HT, Zoghbi HY. The yin and yang of MeCP2 phosphorylation. Proc Natl Acad Sci U S A. 2009;106(12):4577–4578. doi: 10.1073/pnas.0901518106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Cunha C, Brambilla R, Thomas KL. A simple role for BDNF in learning and memory? Front Mol Neurosci. 2010;3:1. doi: 10.3389/neuro.02.001.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Castren E, Kojima M. Brain-derived neurotrophic factor in mood disorders and antidepressant treatments. Neurobiol Dis 97(Pt B), 119-126 (2017). [DOI] [PubMed]
- 258.Kemp SW, Szynkaruk M, Stanoulis KN, et al. Pharmacologic rescue of motor and sensory function by the neuroprotective compound P7C3 following neonatal nerve injury. Neuroscience. 2015;284:202–216. doi: 10.1016/j.neuroscience.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 259.Tesla R, Wolf HP, Xu P, et al. Neuroprotective efficacy of aminopropyl carbazoles in a mouse model of amyotrophic lateral sclerosis. Proc Natl Acad Sci U S A. 2012;109(42):17016–17021. doi: 10.1073/pnas.1213960109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.De Jesus-Cortes H, Xu P, Drawbridge J, et al. Neuroprotective efficacy of aminopropyl carbazoles in a mouse model of Parkinson disease. Proc Natl Acad Sci U S A. 2012;109(42):17010–17015. doi: 10.1073/pnas.1213956109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Blaya MO, Bramlett HM, Naidoo J, Pieper AA, Dietrich WD. Neuroprotective efficacy of a proneurogenic compound after traumatic brain injury. J Neurotrauma. 2014;31(5):476–486. doi: 10.1089/neu.2013.3135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Yin TC, Britt JK, De Jesus-Cortes H, et al. P7C3 neuroprotective chemicals block axonal degeneration and preserve function after traumatic brain injury. Cell Rep. 2014;8(6):1731–1740. doi: 10.1016/j.celrep.2014.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Dutca LM, Stasheff SF, Hedberg-Buenz A, et al. Early detection of subclinical visual damage after blast-mediated TBI enables prevention of chronic visual deficit by treatment with P7C3-S243. Invest Ophthalmol Vis Sci. 2014;55(12):8330–8341. doi: 10.1167/iovs.14-15468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.De Jesus-Cortes H, Miller AD, Britt JK, et al. Protective efficacy of P7C3-S243 in the 6-hydroxydopamine model of Parkinson's disease. NPJ Parkinsons Dis 1 (2015). [DOI] [PMC free article] [PubMed]
- 265.Naidoo J, De Jesus-Cortes H, Huntington P, et al. Discovery of a neuroprotective chemical, (S)-N-(3-(3,6-dibromo-9H-carbazol-9-yl)-2-fluoropropyl)-6-methoxypyridin-2-amine [(-)-P7C3-S243], with improved druglike properties. J Med Chem. 2014;57(9):3746–3754. doi: 10.1021/jm401919s. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Pieper AA, McKnight SL, Ready JM. P7C3 and an unbiased approach to drug discovery for neurodegenerative diseases. Chem Soc Rev. 2014;43(19):6716–6726. doi: 10.1039/C3CS60448A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Gao R, Penzes P. Common mechanisms of excitatory and inhibitory imbalance in schizophrenia and autism spectrum disorders. Curr Mol Med. 2015;15(2):146–167. doi: 10.2174/1566524015666150303003028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Bicks LK, Koike H, Akbarian S, Morishita H. Prefrontal cortex and social cognition in mouse and man. Front Psychol. 2015;6:1805. doi: 10.3389/fpsyg.2015.01805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Nelson SB, Valakh V. Excitatory/inhibitory balance and circuit homeostasis in autism spectrum disorders. Neuron. 2015;87(4):684–698. doi: 10.1016/j.neuron.2015.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Frank CA. How voltage-gated calcium channels gate forms of homeostatic synaptic plasticity. Front Cell Neurosci. 2014;8:40. doi: 10.3389/fncel.2014.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Gong B, Wang H, Gu S, Heximer SP, Zhuo M. Genetic evidence for the requirement of adenylyl cyclase 1 in synaptic scaling of forebrain cortical neurons. Eur J Neurosci. 2007;26(2):275–288. doi: 10.1111/j.1460-9568.2007.05669.x. [DOI] [PubMed] [Google Scholar]
- 272.Saliba RS, Gu Z, Yan Z, Moss SJ. Blocking L-type voltage-gated Ca2+ channels with dihydropyridines reduces gamma-aminobutyric acid type A receptor expression and synaptic inhibition. J Biol Chem. 2009;284(47):32544–32550. doi: 10.1074/jbc.M109.040071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Hirtz JJ, Braun N, Griesemer D, et al. Synaptic refinement of an inhibitory topographic map in the auditory brainstem requires functional Cav1.3 calcium channels. J Neurosci. 2012;32(42):14602–14616. doi: 10.1523/JNEUROSCI.0765-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Busquet P, Nguyen NK, Schmid E, et al. CaV1.3 L-type Ca2+ channels modulate depression-like behaviour in mice independent of deaf phenotype. Int J Neuropsychopharmacol. 2010;13(4):499–513. doi: 10.1017/S1461145709990368. [DOI] [PubMed] [Google Scholar]
- 275.Platzer J, Engel J, Schrott-Fischer A, et al. Congenital deafness and sinoatrial node dysfunction in mice lacking class D L-type Ca2+ channels. Cell. 2000;102(1):89–97. doi: 10.1016/S0092-8674(00)00013-1. [DOI] [PubMed] [Google Scholar]
- 276.McKinney BC, Murphy GG. The L-Type voltage-gated calcium channel Cav1.3 mediates consolidation, but not extinction, of contextually conditioned fear in mice. Learn Mem 13(5), 584-589 (2006). [DOI] [PMC free article] [PubMed]
- 277.McKinney BC, Sze W, Lee B, Murphy GG. Impaired long-term potentiation and enhanced neuronal excitability in the amygdala of Ca(V)1.3 knockout mice. Neurobiol Learn Mem 92(4), 519-528 (2009). [DOI] [PMC free article] [PubMed]
- 278.Hell JW, Westenbroek RE, Warner C, et al. Identification and differential subcellular localization of the neuronal class C and class D L-type calcium channel alpha 1 subunits. J Cell Biol. 1993;123(4):949–962. doi: 10.1083/jcb.123.4.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Lancaster TM, Heerey EA, Mantripragada K, Linden DE. CACNA1C risk variant affects reward responsiveness in healthy individuals. Transl Psychiatry. 2014;4:e461. doi: 10.1038/tp.2014.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Pedram P, Zhai G, Gulliver W, Zhang H, Sun G. Two novel candidate genes identified in adults from the Newfoundland population with addictive tendencies towards food. Appetite 2017 Jan 20 [Epub ahead of print]. [DOI] [PubMed]
- 281.Bardo MT, Bevins RA. Conditioned place preference: what does it add to our preclinical understanding of drug reward? Psychopharmacology (Berl) 2000;153(1):31–43. doi: 10.1007/s002130000569. [DOI] [PubMed] [Google Scholar]
- 282.Degoulet M, Stelly CE, Ahn KC, Morikawa H. L-type Ca(2)(+) channel blockade with antihypertensive medication disrupts VTA synaptic plasticity and drug-associated contextual memory. Mol Psychiatry. 2016;21(3):394–402. doi: 10.1038/mp.2015.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Reimer AR, Martin-Iverson MT. Nimodipine and haloperidol attenuate behavioural sensitization to cocaine but only nimodipine blocks the establishment of conditioned locomotion induced by cocaine. Psychopharmacology (Berl) 1994;113(3-4):404–410. doi: 10.1007/BF02245216. [DOI] [PubMed] [Google Scholar]
- 284.Pierce RC, Quick EA, Reeder DC, Morgan ZR, Kalivas PW. Calcium-mediated second messengers modulate the expression of behavioral sensitization to cocaine. J Pharmacol Exp Ther. 1998;286(3):1171–1176. [PubMed] [Google Scholar]
- 285.Pani L, Kuzmin A, Martellotta MC, Gessa GL, Fratta W. The calcium antagonist PN 200-110 inhibits the reinforcing properties of cocaine. Brain Res Bull. 1991;26(3):445–447. doi: 10.1016/0361-9230(91)90022-C. [DOI] [PubMed] [Google Scholar]
- 286.Biala G, Langwinski R. Effects of calcium channel antagonists on the reinforcing properties of morphine, ethanol and cocaine as measured by place conditioning. J Physiol Pharmacol. 1996;47(3):497–502. [PubMed] [Google Scholar]
- 287.Shibasaki M, Kurokawa K, Ohkuma S. Upregulation of L-type Ca(v)1 channels in the development of psychological dependence. Synapse. 2010;64(6):440–444. doi: 10.1002/syn.20745. [DOI] [PubMed] [Google Scholar]
- 288.Kuzmin A, Zvartau E, Gessa GL, Martellotta MC, Fratta W. Calcium antagonists isradipine and nimodipine suppress cocaine and morphine intravenous self-administration in drug-naive mice. Pharmacol Biochem Behav. 1992;41(3):497–500. doi: 10.1016/0091-3057(92)90363-K. [DOI] [PubMed] [Google Scholar]
- 289.Anderson SM, Famous KR, Sadri-Vakili G, et al. CaMKII: a biochemical bridge linking accumbens dopamine and glutamate systems in cocaine seeking. Nat Neurosci. 2008;11(3):344–353. doi: 10.1038/nn2054. [DOI] [PubMed] [Google Scholar]
- 290.Zhang Q, Li J-X, Zheng J-W, Liu R-K, Liang J-H. L-type Ca2+ channel blockers inhibit the development but not the expression of sensitization to morphine in mice. Eur J Pharmacol. 2003;467(1-3):145–150. doi: 10.1016/S0014-2999(03)01567-X. [DOI] [PubMed] [Google Scholar]
- 291.Kuzmin A, Patkina N, Pchelintsev M, Zvartau E. Isradipine is able to separate morphine-induced analgesia and place conditioning. Brain Res. 1992;593(2):221–225. doi: 10.1016/0006-8993(92)91311-2. [DOI] [PubMed] [Google Scholar]
- 292.Michaluk J, Karolewicz B, Antkiewicz-Michaluk L, Vetulani J. Effects of various Ca2+ channel antagonists on morphine analgesia, tolerance and dependence, and on blood pressure in the rat. Eur J Pharmacol. 1998;352(2-3):189–197. doi: 10.1016/S0014-2999(98)00373-2. [DOI] [PubMed] [Google Scholar]
- 293.Tokuyama S, Feng Y, Wakabayashi H, Ho IK. Ca2+ channel blocker, diltiazem, prevents physical dependence and the enhancement of protein kinase C activity by opioid infusion in rats. Eur J Pharmacol. 1995;279(1):93–98. doi: 10.1016/0014-2999(95)00140-G. [DOI] [PubMed] [Google Scholar]
- 294.Tokuyama S, Ho IK. Inhibitory effects of diltiazem, an L-type Ca2+ channel blocker, on naloxone-increased glutamate levels in the locus coeruleus of opioid-dependent rats. Brain Res. 1996;722(1-2):212–216. doi: 10.1016/0006-8993(96)00187-4. [DOI] [PubMed] [Google Scholar]
- 295.Baeyens JM, Esposito E, Ossowska G, Samanin R. Effects of peripheral and central administration of calcium channel blockers in the naloxone-precipitated abstinence syndrome in morphine-dependent rats. Eur J Pharmacol. 1987;137(1):9–13. doi: 10.1016/0014-2999(87)90176-2. [DOI] [PubMed] [Google Scholar]
- 296.Bongianni F, Carla V, Moroni F, Pellegrini-Giampietro DE. Calcium channel inhibitors suppress the morphine-withdrawal syndrome in rats. Br J Pharmacol. 1986;88(3):561–567. doi: 10.1111/j.1476-5381.1986.tb10236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Barrios M, Baeyens JM. Differential effects of L-type calcium channel blockers and stimulants on naloxone-precipitated withdrawal in mice acutely dependent on morphine. Psychopharmacology (Berl) 1991;104(3):397–403. doi: 10.1007/BF02246042. [DOI] [PubMed] [Google Scholar]
- 298.Zharkovsky A, Totterman AM, Moisio J, Ahtee L. Concurrent nimodipine attenuates the withdrawal signs and the increase of cerebral dihydropyridine binding after chronic morphine treatment in rats. Naunyn Schmiedebergs Arch Pharmacol. 1993;347(5):483–486. doi: 10.1007/BF00166739. [DOI] [PubMed] [Google Scholar]
- 299.Vaseghi G, Rabbani M, Hajhashemi V. The effect of nimodipine on memory impairment during spontaneous morphine withdrawal in mice: Corticosterone interaction. Eur J Pharmacol. 2012;695(1-3):83–87. doi: 10.1016/j.ejphar.2012.08.022. [DOI] [PubMed] [Google Scholar]
- 300.Vitcheva V, Mitcheva M. Effects of nifedipine on behavioral and biochemical parameters in rats after multiple morphine administration. Methods Find Exp Clin Pharmacol. 2004;26(8):631–634. doi: 10.1358/mf.2004.26.8.863729. [DOI] [PubMed] [Google Scholar]
- 301.Engel JA, Fahlke C, Hulthe P, et al. Biochemical and behavioral evidence for an interaction between ethanol and calcium channel antagonists. J Neural Transm. 1988;74(3):181–193. doi: 10.1007/BF01244784. [DOI] [PubMed] [Google Scholar]
- 302.Rezvani AH, Janowsky DS. Decreased alcohol consumption by verapamil in alcohol preferring rats. Prog Neuropsychopharmacol Biol Psychiatry. 1990;14(4):623–631. doi: 10.1016/0278-5846(90)90013-7. [DOI] [PubMed] [Google Scholar]
- 303.Fadda F, Garau B, Colombo G, Gessa GL. Isradipine and other calcium channel antagonists attenuate ethanol consumption in ethanol-preferring rats. Alcohol Clin Exp Res. 1992;16(3):449–452. doi: 10.1111/j.1530-0277.1992.tb01398.x. [DOI] [PubMed] [Google Scholar]
- 304.De Beun R, Schneider R, Klein A, Lohmann A, De Vry J. Effects of nimodipine and other calcium channel antagonists in alcohol-preferring AA rats. Alcohol. 1996;13(3):263–271. doi: 10.1016/0741-8329(95)02054-3. [DOI] [PubMed] [Google Scholar]
- 305.Green-Jordan K, Grant KA. Modulation of the ethanol-like discriminative stimulus effects of diazepam and phencyclidine by L-type voltage-gated calcium-channel ligands in rats. Psychopharmacology (Berl) 2000;149(1):84–92. doi: 10.1007/s002139900344. [DOI] [PubMed] [Google Scholar]
- 306.Holt JD, Watson WP, Little HJ. Studies on a model of long term alcohol drinking. Behav Brain Res. 2001;123(2):193–200. doi: 10.1016/S0166-4328(01)00206-6. [DOI] [PubMed] [Google Scholar]
- 307.Balino P, Pastor R, Aragon CM. Participation of L-type calcium channels in ethanol-induced behavioral stimulation and motor incoordination: effects of diltiazem and verapamil. Behav Brain Res. 2010;209(2):196–204. doi: 10.1016/j.bbr.2010.01.036. [DOI] [PubMed] [Google Scholar]
- 308.White JM, Smith AM. Modification of the behavioural effects of ethanol by nifedipine. Alcohol Alcohol. 1992;27(2):137–141. [PubMed] [Google Scholar]
- 309.Czarnecka E, Kubik-Bogucka E. Effects of calcium antagonists on central actions of ethanol: comparative studies with nifedipine, verapamil and cinnarizine. Alcohol Alcohol. 1993;28(6):649–655. [PubMed] [Google Scholar]
- 310.Whittington MA, Dolin SJ, Patch TL, Siarey RJ, Butterworth AR, Little HJ. Chronic dihydropyridine treatment can reverse the behavioural consequences of and prevent adaptations to, chronic ethanol treatment. Br J Pharmacol. 1991;103(3):1669–1676. doi: 10.1111/j.1476-5381.1991.tb09845.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Gatch MB. Nitrendipine blocks the nociceptive effects of chronically administered ethanol. Alcohol Clin Exp Res. 2002;26(8):1181–1187. doi: 10.1111/j.1530-0277.2002.tb02654.x. [DOI] [PubMed] [Google Scholar]
- 312.Rossetti ZL, Isola D, De Vry J, Fadda F. Effects of nimodipine on extracellular dopamine levels in the rat nucleus accumbens in ethanol withdrawal. Neuropharmacology. 1999;38(9):1361–1369. doi: 10.1016/S0028-3908(99)00039-8. [DOI] [PubMed] [Google Scholar]
- 313.Veatch LM, Gonzalez LP. Nifedipine alleviates alterations in hippocampal kindling after repeated ethanol withdrawal. Alcohol Clin Exp Res. 2000;24(4):484–491. doi: 10.1111/j.1530-0277.2000.tb02015.x. [DOI] [PubMed] [Google Scholar]
- 314.N'Gouemo P. Altered voltage-gated calcium channels in rat inferior colliculus neurons contribute to alcohol withdrawal seizures. Eur Neuropsychopharmacol. 2015;25(8):1342–1352. doi: 10.1016/j.euroneuro.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Hart C, Kisro NA, Robinson SL, Ksir C. Effects of the calcium channel blocker nimodipine on nicotine-induced locomotion in rats. Psychopharmacology (Berl) 1996;128(4):359–361. doi: 10.1007/s002130050145. [DOI] [PubMed] [Google Scholar]
- 316.Biala G. Calcium channel antagonists suppress nicotine-induced place preference and locomotor sensitization in rodents. Pol J Pharmacol. 2003;55(3):327–335. [PubMed] [Google Scholar]
- 317.Biala G, Weglinska B. Blockade of the expression of mecamylamine-precipitated nicotine withdrawal by calcium channel antagonists. Pharmacol Res. 2005;51(5):483–488. doi: 10.1016/j.phrs.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 318.Biala G, Budzynska B. Reinstatement of nicotine-conditioned place preference by drug priming: effects of calcium channel antagonists. Eur J Pharmacol. 2006;537(1-3):85–93. doi: 10.1016/j.ejphar.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 319.Jackson KJ, Damaj MI. L-type calcium channels and calcium/calmodulin-dependent kinase II differentially mediate behaviors associated with nicotine withdrawal in mice. J Pharmacol Exp Ther. 2009;330(1):152–161. doi: 10.1124/jpet.109.151530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Brain Res Rev. 1993;18(3):247–291. doi: 10.1016/0165-0173(93)90013-P. [DOI] [PubMed] [Google Scholar]
- 321.Pierce RC, Kalivas PW. A circuitry model of the expression of behavioral sensitization to amphetamine-like psychostimulants. Brain Res Brain Res Rev. 1997;25(2):192–216. doi: 10.1016/S0165-0173(97)00021-0. [DOI] [PubMed] [Google Scholar]
- 322.Vanderschuren LJ, Pierce RC. Sensitization processes in drug addiction. Curr Top Behav Neurosci. 2010;3:179–195. doi: 10.1007/7854_2009_21. [DOI] [PubMed] [Google Scholar]
- 323.Stewart J. Review. Psychological and neural mechanisms of relapse. Philos Trans R Soc Lond B Biol Sci. 2008;363(1507):3147–3158. doi: 10.1098/rstb.2008.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Nunes EJ, Hughley SM, Small KM, Rajadhyaksha AM, Addy NA. Ventral tegmental area L-type calcium channels mediate cue-induced cocaine seeking and dopamine release during early withdrawal. Program No. 351.05/FFF18, San Diego, CA(Society for Neuroscience), Online (2016).
- 325.Schierberl K, Hao J, Tropea TF, et al. Cav1.2 L-type Ca2+ channels mediate cocaine-induced GluA1 trafficking in the nucleus accumbens, a long-term adaptation dependent on ventral tegmental area Ca(v)1.3 channels. J Neurosci 31(38), 13562-13575 (2011). [DOI] [PMC free article] [PubMed]
- 326.Terrillion CE, Dao DT, Cachope R, et al. Reduced levels of Cacna1c attenuate mesolimbic dopamine system function. Genes Brain Behav 2017 Feb 10 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 327.Liu Y, Harding M, Pittman A, et al. Cav1.2 and Cav1.3 L-type calcium channels regulate dopaminergic firing activity in the mouse ventral tegmental area. J Neurophysiol. 2014;112(5):1119–1130. doi: 10.1152/jn.00757.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Wolf ME. Synaptic mechanisms underlying persistent cocaine craving. Nat Rev Neurosci. 2016;17(6):351–365. doi: 10.1038/nrn.2016.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Enck RE. Understanding tolerance, physical dependence and addiction in the use of opioid analgesics. Am J Hosp Palliat Care. 1991;8(1):9–11. doi: 10.1177/104990919100800102. [DOI] [PubMed] [Google Scholar]
- 330.Blasig J, Herz A, Reinhold K, Zieglgansberger S. Development of physical dependence on morphine in respect to time and dosage and quantification of the precipitated withdrawal syndrome in rats. Psychopharmacologia. 1973;33(1):19–38. doi: 10.1007/BF00428791. [DOI] [PubMed] [Google Scholar]
- 331.Wei E, Loh HH, Way EL. Quantitative aspects of precipitated abstinence in morphine-dependent rats. J Pharmacol Exp Ther. 1973;184(2):398–403. [PubMed] [Google Scholar]
- 332.Shibasaki M, Kurokawa K, Mizuno K, Ohkuma S. Up-regulation of Ca(v)1.2 subunit via facilitating trafficking induced by Vps34 on morphine-induced place preference in mice. Eur J Pharmacol 651(1-3), 137-145 (2011). [DOI] [PubMed]
- 333.Haller VL, Bernstein MA, Welch SP. Chronic morphine treatment decreases the Cav1.3 subunit of the L-type calcium channel. Eur J Pharmacol. 2008;578(2-3):101–107. doi: 10.1016/j.ejphar.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 334.Roberto M, Gilpin NW, Siggins GR. The central amygdala and alcohol: role of gamma-aminobutyric acid, glutamate, and neuropeptides. Cold Spring Harb Perspect Med. 2012;2(12):a012195. doi: 10.1101/cshperspect.a012195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Silberman Y, Winder DG. Ethanol and corticotropin releasing factor receptor modulation of central amygdala neurocircuitry: an update and future directions. Alcohol. 2015;49(3):179–184. doi: 10.1016/j.alcohol.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Zorumski CF, Mennerick S, Izumi Y. Acute and chronic effects of ethanol on learning-related synaptic plasticity. Alcohol. 2014;48(1):1–17. doi: 10.1016/j.alcohol.2013.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.N'Gouemo P, Morad M. Ethanol withdrawal seizure susceptibility is associated with upregulation of L- and P-type Ca2+ channel currents in rat inferior colliculus neurons. Neuropharmacology. 2003;45(3):429–437. doi: 10.1016/S0028-3908(03)00191-6. [DOI] [PubMed] [Google Scholar]
- 338.Littleton JM, Little HJ, Whittington MA. Effects of dihydropyridine calcium channel antagonists in ethanol withdrawal; doses required, stereospecificity and actions of Bay K 8644. Psychopharmacology (Berl) 1990;100(3):387–392. doi: 10.1007/BF02244612. [DOI] [PubMed] [Google Scholar]
- 339.De Biasi M, Dani JA. Reward, addiction, withdrawal to nicotine. Annu Rev Neurosci. 2011;34:105–130. doi: 10.1146/annurev-neuro-061010-113734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Katsura M, Mohri Y, Shuto K, et al. Up-regulation of L-type voltage-dependent calcium channels after long term exposure to nicotine in cerebral cortical neurons. J Biol Chem. 2002;277(10):7979–7988. doi: 10.1074/jbc.M109466200. [DOI] [PubMed] [Google Scholar]
- 341.Hayashida S, Katsura M, Torigoe F, Tsujimura A, Ohkuma S. Increased expression of L-type high voltage-gated calcium channel alpha1 and alpha2/delta subunits in mouse brain after chronic nicotine administration. Brain Res Mol Brain Res. 2005;135(1-2):280–284. doi: 10.1016/j.molbrainres.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 342.Malin DH, Lake JR, Carter VA, et al. The nicotinic antagonist mecamylamine precipitates nicotine abstinence syndrome in the rat. Psychopharmacology (Berl) 1994;115(1-2):180–184. doi: 10.1007/BF02244770. [DOI] [PubMed] [Google Scholar]
- 343.Malin DH. Nicotine dependence: studies with a laboratory model. Pharmacol Biochem Behav. 2001;70(4):551–559. doi: 10.1016/S0091-3057(01)00699-2. [DOI] [PubMed] [Google Scholar]
- 344.Post RM, Kalivas P. Bipolar disorder and substance misuse: pathological and therapeutic implications of their comorbidity and cross-sensitisation. Br J Psychiatry. 2013;202(3):172–176. doi: 10.1192/bjp.bp.112.116855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Lüthi A, Lüscher C. Pathological circuit function underlying addiction and anxiety disorders. Nat Neurosci. 2014;17(12):1635–1643. doi: 10.1038/nn.3849. [DOI] [PubMed] [Google Scholar]
- 346.Nestler EJ, Carlezon WA., Jr The mesolimbic dopamine reward circuit in depression. Biol Psychiatry. 2006;59(12):1151–1159. doi: 10.1016/j.biopsych.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 347.Russo SJ, Nestler EJ. The brain reward circuitry in mood disorders. Nat Rev Neurosci. 2013;14(9):609–625. doi: 10.1038/nrn3381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Sun H, Martin JA, Werner CT, et al. BAZ1B in nucleus accumbens regulates reward-related behaviors in response to distinct emotional stimuli. J Neurosci. 2016;36(14):3954–3961. doi: 10.1523/JNEUROSCI.3254-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Khibnik LA, Beaumont M, Doyle M, et al. Stress and cocaine trigger divergent and cell type-specific regulation of synaptic transmission at single spines in nucleus accumbens. Biol Psychiatry. 2016;79(11):898–905. doi: 10.1016/j.biopsych.2015.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Lobo MK, Zaman S, Damez-Werno DM, et al. DeltaFosB induction in striatal medium spiny neuron subtypes in response to chronic pharmacological, emotional, and optogenetic stimuli. J Neurosci. 2013;33(47):18381–18395. doi: 10.1523/JNEUROSCI.1875-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Covington HE, 3rd, Maze I, Sun H, et al. A role for repressive histone methylation in cocaine-induced vulnerability to stress. Neuron. 2011;71(4):656–670. doi: 10.1016/j.neuron.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.LaPlant Q, Vialou V, Covington HE, 3rd, et al. Dnmt3a regulates emotional behavior and spine plasticity in the nucleus accumbens. Nat Neurosci. 2010;13(9):1137–1143. doi: 10.1038/nn.2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Chaudhury D, Walsh JJ, Friedman AK, et al. Rapid regulation of depression-related behaviours by control of midbrain dopamine neurons. Nature. 2013;493(7433):532–536. doi: 10.1038/nature11713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Tye KM, Mirzabekov JJ, Warden MR, et al. Dopamine neurons modulate neural encoding and expression of depression-related behaviour. Nature. 2013;493(7433):537–541. doi: 10.1038/nature11740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Walsh JJ, Han MH. The heterogeneity of ventral tegmental area neurons: Projection functions in a mood-related context. Neuroscience. 2014;282:101–108. doi: 10.1016/j.neuroscience.2014.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Gunaydin LA, Grosenick L, Finkelstein JC, et al. Natural neural projection dynamics underlying social behavior. Cell. 2014;157(7):1535–1551. doi: 10.1016/j.cell.2014.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Covey DP, Roitman MF, Garris PA. Illicit dopamine transients: reconciling actions of abused drugs. Trends Neurosci. 2014;37(4):200–210. doi: 10.1016/j.tins.2014.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Nestler EJ. Role of the brain's reward circuitry in depression: transcriptional mechanisms. Int Rev Neurobiol. 2015;124:151–170. doi: 10.1016/bs.irn.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Russo SJ, Dietz DM, Dumitriu D, Morrison JH, Malenka RC, Nestler EJ. The addicted synapse: mechanisms of synaptic and structural plasticity in nucleus accumbens. Trends Neurosci. 2010;33(6):267–276. doi: 10.1016/j.tins.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Pascoli V, Terrier J, Hiver A, Luscher C. Sufficiency of mesolimbic dopamine neuron stimulation for the progression to addiction. Neuron. 2015;88(5):1054–1066. doi: 10.1016/j.neuron.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 361.Saddoris MP, Sugam JA, Cacciapaglia F, Carelli RM. Rapid dopamine dynamics in the accumbens core and shell: learning and action. Front Biosci. 2013;5:273–288. doi: 10.2741/E615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Goffer Y, Xu D, Eberle SE, et al. Calcium-permeable AMPA receptors in the nucleus accumbens regulate depression-like behaviors in the chronic neuropathic pain state. J Neurosci. 2013;33(48):19034–19044. doi: 10.1523/JNEUROSCI.2454-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Lim BK, Huang KW, Grueter BA, Rothwell PE, Malenka RC. Anhedonia requires MC4R-mediated synaptic adaptations in nucleus accumbens. Nature. 2012;487(7406):183–189. doi: 10.1038/nature11160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Vialou V, Robison AJ, Laplant QC, et al. DeltaFosB in brain reward circuits mediates resilience to stress and antidepressant responses. Nat Neurosci. 2010;13(6):745–752. doi: 10.1038/nn.2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Araki R, Ago Y, Hasebe S, et al. Involvement of prefrontal AMPA receptors in encounter stimulation-induced hyperactivity in isolation-reared mice. Int J Neuropsychopharmacol. 2014;17(6):883–893. doi: 10.1017/S1461145713001582. [DOI] [PubMed] [Google Scholar]
- 366.Wook Koo J, Labonte B, Engmann O, et al. Essential role of mesolimbic brain-derived neurotrophic factor in chronic social stress-induced depressive behaviors. Biol Psychiatry. 2016;80(6):469–478. doi: 10.1016/j.biopsych.2015.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Lobo MK, Covington HE, 3rd, Chaudhury D, et al. Cell type-specific loss of BDNF signaling mimics optogenetic control of cocaine reward. Science. 2010;330(6002):385–390. doi: 10.1126/science.1188472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Le Moine C, Normand E, Bloch B. Phenotypical characterization of the rat striatal neurons expressing the D1 dopamine receptor gene. Proc Natl Acad Sci U S A. 1991;88(10):4205–4209. doi: 10.1073/pnas.88.10.4205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Lu XY, Ghasemzadeh MB, Kalivas PW. Expression of D1 receptor, D2 receptor, substance P and enkephalin messenger RNAs in the neurons projecting from the nucleus accumbens. Neuroscience. 1998;82(3):767–780. doi: 10.1016/S0306-4522(97)00327-8. [DOI] [PubMed] [Google Scholar]
- 370.Lohmann C. Calcium signaling and the development of specific neuronal connections. Prog Brain Res. 2009;175:443–452. doi: 10.1016/S0079-6123(09)17529-5. [DOI] [PubMed] [Google Scholar]
- 371.Ramocki MB, Zoghbi HY. Failure of neuronal homeostasis results in common neuropsychiatric phenotypes. Nature. 2008;455(7215):912–918. doi: 10.1038/nature07457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)