Abstract
Background
Delirium is associated with increased morbidity and mortality. The factors associated with post-lung transplant delirium and its impact on outcomes are under characterized.
Methods
The medical records of 163 consecutive adult lung transplant recipients were reviewed for delirium within 5 days (early-onset) and 30 hospital days (ever-onset) post-transplantation. A multivariable logistic regression model assessed factors associated with delirium. Multivariable negative binomial regression and Cox proportional hazards models assessed the association of delirium with ventilator duration, intensive care unit (ICU) length of stay (LOS), hospital LOS and one-year mortality.
Results
Thirty six % developed early-onset and 44% - ever-onset delirium. Obesity (OR 6.35, 95% CI 1.61–24.98) and bolused benzodiazepines within the first post-operative day (OR 2.28, 95% CI 1.07–4.89) were associated with early-onset delirium. Early-onset delirium was associated with longer adjusted mechanical ventilation duration (p=0.001), ICU LOS (p<0.001), and hospital LOS (p=0.005). Ever-onset delirium was associated with longer ICU (p<0.001) and hospital LOS (p<0.001). After adjusting for clinical variables, delirium was not significantly associated with one-year mortality (early-onset HR 1.65, 95% CI 0.67–4.03; ever-onset HR 1.70, 95% CI 0.63–4.55).
Conclusions
Delirium is common after lung transplant surgery and associated with increased hospital resources.
Keywords: lung transplantation, lung transplant, delirium, delirium outcomes, cognitive disorder
BACKGROUND
Delirium is the most common neuropsychiatric disorder, affecting 15–60% of hospitalized general medical and surgical patients and up to 87% of mechanically ventilated patients in the intensive care unit (ICU)1. In critically ill patients, the presence of delirium is associated with worse mortality, increased rates of self-extubation and prolonged duration of mechanical ventilation, increased ICU and hospital length of stay (LOS), and greater hospital costs2–5. Moreover, not only pre-morbid cognitive dysfunction is a risk factor for delirium, but delirium also has further lasting negative effects on cognitive function6,7.
As delirium has been associated with worse survival and outcomes in other critically ill3 and transplant populations8, it could be expected to have a similar effect in lung transplant recipients. The available data on delirium after lung transplantation is limited to a few small single center studies9–11. A retrospective study of 30 lung transplant recipients found that 73% of patients developed delirium in the first 2 weeks after transplantation9. In this sample, factors associated with an increased risk of delirium included use of cardiopulmonary bypass, higher cyclosporine levels, and relocation to await surgery9. A prospective study of 21 lung transplant recipients found a delirium incidence of 19% within 96 hours of surgery, which was associated with an increased time to extubation10. A recent prospective study of 63 lung transplant recipients found a delirium incidence of 37%, mostly in the immediate postoperative period, determined with the Confusion Assessment Method (CAM) screening tool11. Worse pre-operative cognitive functioning was associated with delirium occurrence, while the presence and duration of delirium were both associated with longer hospital stays11. In addition, lower cerebral perfusion pressure was found to be associated with doubling the risk of delirium in the same patient sample, as well as increasing the duration and severity of delirium12. Finally, delirium during the index hospitalization in lung transplant recipients without cystic fibrosis has been associated with worse post-transplant neurocognitive function13.
The purpose of our study was to determine the incidence of delirium in a large lung transplant population, identify predictors associated with the development of delirium, including post-operative sedative and pain medication use, and characterize delirium impact on hospital resource utilization and clinical outcomes, including mortality. Characterization of the recipient-level associations with delirium could help identify patients at high-risk and focus delirium screening and prevention interventions.
METHODS
A retrospective chart review was performed to identify delirium among all adult patients who underwent single or bilateral lung transplant at Stanford University Hospital, between July 18th, 2011 and March 18th, 2013. All patients who survived beyond 24 hours post-transplantation were included in these analyses. The data collection was limited to the index hospitalization associated with the actual transplantation surgery, except for the long-term mortality data. Baseline clinical characteristics, post-surgical medication use, cardiopulmonary bypass time, duration of mechanical ventilation, ICU and hospital LOS, and death were extracted. The presence of any primary graft dysfunction (PGD) at 48 or 72 hours post-transplant was determined by standard criteria14. Medications were divided into those administered as continuous drips as a part of the standard sedation and pain management protocol (i.e., dexmedetomidine, midazolam, hydromorphone or fentanyl infusions) or via intermittent administration, either scheduled or given on as needed basis (i.e., steroids, benzodiazepines, opiates). The exact dosages of bolused medications were extracted, while the administration of drip medications was documented in binary fashion (i.e., administered versus not administered). Post-transplant delirium was identified utilizing modifications to a previously-published chart-based instrument for delirium15,16, which required fulfilling standard Diagnostic and Statistical Manual of Mental Disorder 4th edition, Text Revision (DSM-IV TR) criteria17.
The entire electronic medical records including notes from critical care and lung transplant physicians, nurses, physical and occupational therapists, social workers, and psychiatry and neurology consultants when available, were examined by a psychosomatic medicine specialist (YS). Diagnosis of delirium required the following: 1) a noted change in patient’s mental status; 2) evidence of fluctuating attention, including either agitation, drowsiness, and/or inability to focus or follow commands; and 3) the presence of additional supportive features, such as confusion, new onset hallucinations or delusions, paranoia, delusions, severe sleep disturbances, restraints for behavioral management due to pulling on necessary lines or tubes, antipsychotic use for behavioral management, or documentation of delirium diagnosis. The presence of delirium was determined on a daily basis and characterized as early-onset if occurring within 5 days post-transplant, and as ever-onset if occurring within the first 30-days or until discharge (whichever was sooner) post-transplant during index admission. The study was approved by the Institutional Review Board at Stanford University, protocol # IRB-29667.
Statistical Analysis
Characteristics of recipients with and without delirium (early-onset and ever-onset) were compared using the chi-square test or Fisher’s exact test for categorical variables, and the Wilcoxon rank-sum test for continuous variables. A multivariable logistic regression was used to assess the recipient characteristics associated with the outcome of delirium. Recipient characteristics, including age, gender, underlying diagnosis, body mass index (BMI), transplant procedure type, lung allocation score (LAS) at the time of transplant, and presence of post-operative PGD along with pre-transplant benzodiazepine use and medications received within the first post-operative day were assessed. BMI was categorized as underweight (<18.5), normal weight (18.5–24.9), overweight (25.0–29.9), and obese (>30.0). Medications assessed included the use of opiates (separated into continuous infusion and intermittent doses), benzodiazepines (separated into continuous infusion and intermittent doses), corticosteroids, and dexmedetomidine within the first post-operative day. All bolused opiates were converted, as necessary, to a standardized dose of micrograms (mcg) of fentanyl equivalents and all bolused benzodiazepines to milligrams (mg) of lorazepam equivalents. Based upon prior literature, age, diagnosis, LAS, and PGD were a priori included in the final multivariable model along with variables identified as having a p<0.15 during univariate analysis.
A multivariable negative binomial regression model adjusting for the above recipient variables was fit to assess the association of early-onset delirium with ventilator duration and ICU or hospital LOS. One-year survival for those with and without delirium was calculated using Kaplan-Meier plots and compared using the log-rank test. A Cox proportional hazards model, adjusted for the recipient characteristics, was used to assess the impact of early-onset or ever-onset delirium on one-year post lung transplant survival. The proportional hazards assumption was assessed by visual inspection of the Kaplan-Meier and Schoenfeld residuals plots. All statistical analyses were performed with Stata software, version 14.1 (StataCorp).
The study was performed in a cardiothoracic ICU at Stanford Hospital. Patients were roomed either in double or single rooms. Non-pharmacological measures were used throughout the ICU and applied to all patients according to our hospital protocol to prevent emergence of delirium (e.g., frequent orientation, sleep-wake cycle regulation, early mobilization).
RESULTS
Delirium Demographics and Characteristics
Of 164 lung recipients transplanted within the study period, 163 patients met inclusion criteria. The average patient’s age was 50.8 years (SD 14.8) with 41.7% of the sample being female. Median LAS at the time of transplantation was 41.2 (range 30.2–94.6). Eighty five percent of the sample received double lung transplantation, while the remaining 15% underwent unilateral transplantation.
A total of 35.6% of all lung transplant recipients (58/163) developed early-onset delirium, while 44.2% (72/163) of recipients developed ever-onset delirium during their post-transplant hospitalization. The median time to onset of post-operative delirium was 2 days (mean 4.0 days, SD 4.2 days) with a median duration of 4.5 days (IQR 3, 7.5) (mean duration 6.9 days, SD 6.6 days).
The characteristics of recipients with and without early-onset or ever-onset delirium are shown in Table 1. Recipients with early-onset delirium were more likely to be obese (BMI>30) and less likely to be underweight (BMI<20) compared to those without delirium (p=0.008). There were no other significant differences in baseline characteristics between recipients with and without early-onset delirium. Recipients with ever-onset delirium were again more likely to be obese and less likely to be underweight (p=0.004), and had longer cardiopulmonary bypass time (p=0.011) than those who never developed hospital delirium.
Table 1.
Characteristics of Lung Transplant Recipients with and without Delirium
| Early-Onset Delirium | Ever-Onset Delirium | |||||
|---|---|---|---|---|---|---|
| No n = 105 |
Yes n = 58 |
P Value | No n = 91 |
Yes n = 72 |
P Value | |
|
| ||||||
| Age in years - median (IQR) | 53.65 (31.99, 61.03) | 55.81 (42.38, 62.34) | 0.3090 | 53.63 (25.65, 61.03) | 55.81 (IQR 42.31, 62.52) | 0.248 |
| Female Gender - n (%) | 48 (45.71%) | 20 (34.48%) | 0.1640 | 40 (43.96%) | 28 (38.89%) | 0.515 |
| Diagnosis Group - n (%) | 0.1960 | 0.060 | ||||
| Group A (Chronic Obstructive Pulmonary Disease) | 21 (20.19%) | 11 (18.97%) | 19 (21.11%) | 13 (18.06%) | ||
| Group B (Pulmonary Hypertension) | 2 (1.92%) | 2 (3.45%) | 2 (2.22%) | 2 (2.78%) | ||
| Group C (Cystic Fibrosis) | 30 (28.85%) | 9 (15.52%) | 28 (31.11%) | 11 (15.28%) | ||
| Group D (Pulmonary Fibrosis) | 51 (49.04%) | 36 (62.07%) | 41 (45.56%) | 46 (63.89%) | ||
| Body Mass Index Classification - n (%) | 0.0080 | 0.004 | ||||
| <20, Underweight | 29 (27.62%) | 6 (10.34%) | 26 (28.57%) | 9 (12.50%) | ||
| 20–25, Normal Weight | 28 (26.67%) | 14 (24.14%) | 26 (28.57%) | 16 (22.22%) | ||
| 25–30, Overweight | 37 (35.24%) | 22 (37.93%) | 31 (34.07%) | 28 (38.89%) | ||
| >30, Obese | 11 (10.48%) | 16 (27.59%) | 8 (8.79%) | 19 (26.39%) | ||
| Bilateral Transplant Procedure - n (%) | 89 (84.76%) | 50 (86.21%) | 0.8030 | 75 (82.42%) | 64 (88.89%) | 0.247 |
| Cardiopulmonary Bypass Time (minutes) - median (IQR) | 211 (180, 240) | 217 (189, 260) | 0.1646 | 204.5 (178.5, 228.5) | 225 (199, 262) | 0.011 |
| Lung Allocation Score - median (IQR) | 41.60 (36.02, 50.78) | 40.95 (35.23, 51.26) | 0.9641 | 41.60 (35.48, 49.47) | 40.95 (35.62, 52.11) | 0.818 |
Recipient Characteristics and Post-Transplant Medications Associated with Delirium
In univariate logistic regression analysis, age, gender, underlying diagnosis, LAS at transplant, and post-operative PGD were not associated with early-onset delirium. Similarly, pre-operative use of benzodiazepines or post-operative corticosteroid dose, use of continuous benzodiazepines, opiate, or dexmedetomidine infusions, or use of bolused opiates was not associated with early-onset delirium. After controlling for selected recipient characteristics and medications, obesity (adjusted OR 6.35, 95% CI: 1.61–24.98) and intermittent benzodiazepine use within the first post-operative day (adjusted OR 2.29, 95% CI: 1.07–4.89) were associated with early-onset delirium.
Delirium, Hospital Resource Use, and Mortality
The unadjusted outcomes between recipients with and without delirium are shown in Table 2.
Table 2.
Resource Use and Outcomes of Lung Transplant Recipients with and without Delirium
| Early-Onset Delirium | Ever-Onset Delirium | |||||
|---|---|---|---|---|---|---|
| No n = 105 |
Yes n = 58 |
P Value | No n = 91 |
Yes n = 72 |
P Value | |
|
| ||||||
| Mechanical Ventilation Duration - days | 1 (1, 2) | 2 (1, 7) | 0.001 | 1 (1, 1) | 3 (1, 9) | <0.001 |
| Intensive Care Unit Length of Stay - days | 3 (2, 6) | 5 (4, 12) | <0.001 | 3 (2, 4) | 6 (4, 14) | <0.001 |
| Hospital Length of Stay - days | 11 (9, 19) | 17 (11, 33) | <0.001 | 10 (8, 16) | 19 (12, 42) | <0.001 |
Results reported as median (IQR)
In unadjusted comparison, delirium was associated with longer duration of mechanical ventilation and length of stay. After adjusting for recipient and transplant characteristics, early-onset delirium was associated with a longer adjusted ventilator duration (p=0.001), ICU LOS (p<0.001), and hospital LOS (p=0.005) in those with early-onset delirium. The development of ever-onset delirium during post-transplant hospitalization was associated with both an increase in ICU (p<0.001) and total hospital LOS (p<0.001).
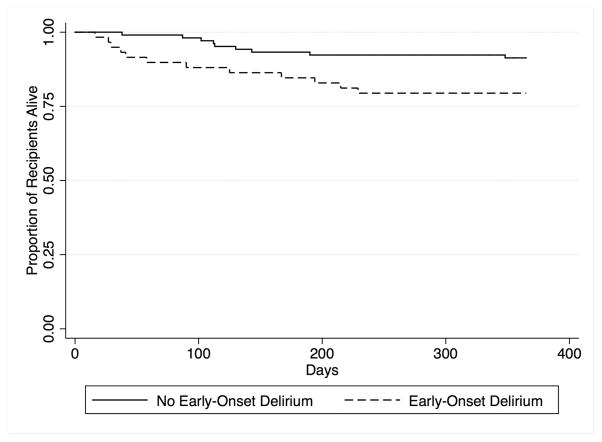
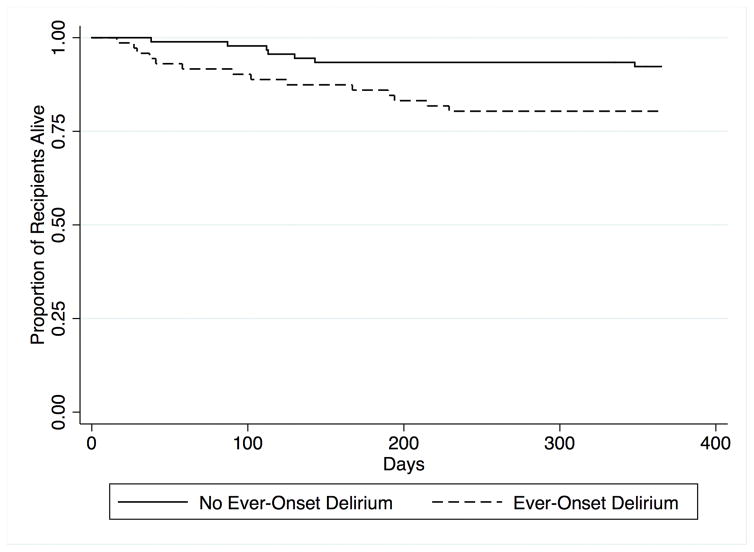
Unadjusted one-year survival was worse in those with early-onset delirium (p=0.026) and ever-onset delirium (p=0.027) than those without delirium (Figure 1 and 2). However, after adjusting for recipient variables, early-onset delirium (adjusted HR 1.65, 95% CI: 0.67–4.03) and ever-onset delirium (adjusted HR 1.70, 95% CI: 0.63–4.55 were not associated with one-year survival.
Figure 1. One-Year Lung Transplant Recipient Survival by Presence of Early-Onset Delirium.
Unadjusted one-year survival is shown for lung transplant recipients with early-onset of delirium (dashed line) and for those without early-onset delirium (solid line).
Figure 2. One-Year Lung Transplant Recipient Survival by Presence of Ever-Onset Delirium.
Unadjusted one-year survival is shown for lung transplant recipients with ever-onset of delirium (dashed line) and for those without ever-onset delirium (solid line).
DISCUSSION
The results of our study, analyzing delirium in the largest published recipient sample to date, support and expand upon previously published findings on the delirium incidence and predictors in lung transplant recipients. As in previous studies9–11, we found that delirium is common in this population, occurring in over 40% of lung transplant recipients, and is associated with worse medical outcomes. We confirmed the previously described association between post-lung transplant delirium and prolonged hospital stay, but also identified increased ventilation duration, and prolonged ICU stay post lung transplantation. Additionally, we found that recipient obesity, classified as BMI>30, and bolused benzodiazepines use within first post-operative day are associated with an increased risk for delirium.
Prolonged hospital stay has been previously demonstrated in ICU2 and in lung transplant recipients11 who experience delirium. We found that early-onset and ever-onset delirium are associated with longer ICU and hospital stays. ICU and hospital LOS are closely monitored metrics in organ transplantation, and shorter LOS is considered an important factor in reducing lung transplant cost and post-transplant morbidity18. Thus, delirium prevention measures and early and routine screening for delirium in lung transplant recipients directed at facilitating the prompt identification and treatment of this complication, may constitute an important intervention which may translate into decreased morbidity, shorter hospital stays, and decreased care costs.
Benzodiazepines are an established risk factor for development of delirium in ICU patients19 and our results similarly demonstrate a significant association between intermittent benzodiazepine use and early-onset delirium in lung transplant recipients. Notably, the use of benzodiazepine or dexmedetomidine infusions for post-operative sedation and comfort had no influence on the development of early-onset delirium in this study. We contribute this finding to standardization of our post lung transplant ICU order set that preferentially selects for dexmedetomidine infusion (total of 68.1% of patients received this on the first day) and discourages benzodiazepine infusions (only 7.36% of patients received this on the first day). Dexmedotomidine has been demonstrated to be protective against development of delirium in prior randomized controlled trials20, while benzodiazepines have been demonstrated to be deleterious for delirium development19. However, there was greater variability in the use of intermittent benzodiazepines with 28.77% of lung transplant recipients receiving a bolus within the first post-operative day. Our finding supports that overall avoidance of benzodiazepines should be encouraged and could potentially reduce the incidence of early-onset delirium in lung transplant recipients. Further prospective work is needed to test whether benzodiazepine avoidance and/or other behavioral or medication-related interventions can modify the incidence of delirium in lung transplant recipients.
The finding of higher BMI associated with early-onset delirium in lung transplant recipients is novel. Previous study of pre-transplant predictors in lung transplant recipients did not include BMI11. On the contrary, lower BMI has been shown to be associated with the development of delirium in other surgical populations, such as gastrointestinal surgery21, total knee arthroplasty22, and hip fracture repair23 patients. It has been postulated that low BMI might represent low nutritional status and inflammation facilitating development of delirium. However, in our study of lung transplant population, the opposite effect was seen with high BMI (>30) significantly associated with the development of delirium. Obesity is an established independent risk factor for the development of primary graft dysfunction (PGD) after lung transplantation24,25. However, we found that obesity remained independently associated with risk for delirium even after adjusting for the presence of PGD at 48 or 72 hours. Notably, obesity has been associated with increased incidence of sternal wound infections, prolonged ventilation, and increased rate of renal failure in cardiothoracic surgeries26,27. These complications can also lead to development of delirium in surgical populations. In any case, our findings suggest that obesity may need to be addressed prior to lung transplantation, and that these patients should be considered at higher risk for the development of delirium and thus require additional surveillance after transplantation.
Finally, we found an association between unadjusted mortality and development of delirium, which ceased to be statistically significant after adjustment for other clinical factors. Larger prospective studies are needed to further characterize this potential association. Studies on delirium in other populations have demonstrated that delirium is independently associated with increased mortality. As the median survival of lung transplant recipients is 5.7 years28, any interventions, such as delirium prophylaxis, aimed at potentially improving this outcome, could prove advantageous in improving graft outcomes.
This study has several limitations. First, the retrospective identification of delirium based upon chart analysis limits the accuracy of delirium incidence16. It is possible that cases of hypoactive delirium were under-recognized, as they are less likely to be identified and/or recorded by most ICU providers29,30. Similarly, it is also possible that hyperactive delirium was over-diagnosed as agitation due to physical discomfort can be mistaken for agitation in delirium. Yet, the rate of delirium in our sample is similar to that reported by Smith and colleagues in prospectively followed lung recipients11. In addition, the diagnosis of delirium based on the whole chart extraction has been previously reported to have good sensitivity (74%) and specificity (83%), when compared to reference standard interviewer ratings for delirium based on the widely used and validated Confusion Assessment Method (CAM)15.
Second, the abstraction of medication dosages had its limitations. While we were able to obtain the exact dosages of intermittent medications, we could only obtain binary (present/absent) data on the continuously infused medications. Thus, in our analyses we had to separate opiates and benzodiazepines based on whether they were administered via infusion (only binary data) or via intermittent boluses (exact dosages). Third, the absence of recipient’s pre-transplant cognitive status data prevented us from controlling for this variable. Finally, we were limited by the study design in establishing a causal relationship between recipient characteristics or medications used and delirium. Future prospective studies are needed to further characterize patients at risk for delirium, determine associations of administered medications and development of delirium and carefully evaluate and test the effect of interventions on delirium in lung transplant recipients.
Conclusions
Delirium is common among lung transplant recipients occurring in 44.2% of patients during the initial post-transplant hospitalization. Recipients who are obese (BMI>30) and who receive benzodiazepine boluses are at higher risk for early-onset delirium. The development of delirium is associated with an increase in the duration of mechanical ventilation, as well as increased ICU and hospital length of stay. While there was an association between delirium and unadjusted mortality, the association was not significant after controlling for other clinical factors. Future efforts are needed to further characterize delirium predictors in larger prospective trials and to study the effect of interventions that reduce post lung transplant delirium. Our findings highlight the need to closely monitor post-transplant lung recipients for the possible development of post-operative delirium and the need for early detection and treatment.
Acknowledgments
Grant Support: This work was conducted with partial support from a KL2 Mentored Career Development Award of the Stanford Clinical and Translational Science Award to Spectrum NIH KL2 TR 001083 (JJM).
We would like to extend our appreciation to the Advanced Lung Disease team at Stanford University for assistance in data collection and to all the lung transplant recipients at Stanford University involved in this study.
Footnotes
Disclosure: The authors disclosed no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Author Contributions: Yelizaveta Sher: concept/design, data analysis/interpretation, data collection, drafting article, critical revision of article, approval of article; Joshua Mooney: data analysis/interpretation, data collection, statistics, funding secured, drafting article, critical revision of article, approval of article, Gundeep Dhillon: design, data analysis/interpretation, critical revision of article, approval of article; Roy Lee: data collection, critical revision of article, approval of article; Jose Maldonado: design, drafting article, critical revision of article, approval of article.
References
- 1.Maldonado JR. Delirium: Neurobiology, Characteristics, and Management. In: Fogel B, Greenberg D, editors. Psychiatric Care of the Medically Ill. Oxford University Press; 2015. [Google Scholar]
- 2.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004 Apr 14;291(14):1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 3.Mehta S, Cook D, Devlin JW, et al. Prevalence, Risk Factors, and Outcomes of Delirium in Mechanically Ventilated Adults. Crit Care Med. 2014 Dec 9; doi: 10.1097/CCM.0000000000000727. [DOI] [PubMed] [Google Scholar]
- 4.Miller RR, 3rd, Ely EW. Delirium and cognitive dysfunction in the intensive care unit. Curr Psychiatry Rep. 2007 Feb;9(1):26–34. doi: 10.1007/s11920-007-0006-x. [DOI] [PubMed] [Google Scholar]
- 5.Dubois MJ, Bergeron N, Dumont M, Dial S, Skrobik Y. Delirium in an intensive care unit: a study of risk factors. Intensive Care Med. 2001 Aug;27(8):1297–1304. doi: 10.1007/s001340101017. [DOI] [PubMed] [Google Scholar]
- 6.Pandharipande P, Jackson J, Ely EW. Delirium: acute cognitive dysfunction in the critically ill. Curr Opin Crit Care. 2005 Aug;11(4):360–368. doi: 10.1097/01.ccx.0000170503.76528.4b. [DOI] [PubMed] [Google Scholar]
- 7.Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013 Oct 3;369(14):1306–1316. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lescot T, Karvellas CJ, Chaudhury P, et al. Postoperative delirium in the intensive care unit predicts worse outcomes in liver transplant recipients. Canadian journal of gastroenterology = Journal canadien de gastroenterologie. 2013 Apr;27(4):207–212. doi: 10.1155/2013/289185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Craven JL. Postoperative organic mental syndromes in lung transplant recipients. Toronto Lung Transplant Group. J Heart Transplant. 1990 Mar-Apr;9(2):129–132. [PubMed] [Google Scholar]
- 10.Santacruz J, EE, Guzman Zavala E, et al. Post-operative delirium in lung transplant recipients: incidence and associated risk factors and morbidity. Paper presented at: Chest; 2009; San Diego, CA. [Google Scholar]
- 11.Smith PJ, Rivelli SK, Waters AM, et al. Delirium affects length of hospital stay after lung transplantation. J Crit Care. 2015 Feb;30(1):126–129. doi: 10.1016/j.jcrc.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith PJ, Blumenthal JA, Hoffman BM, et al. Reduced Cerebral Perfusion Pressure during Lung Transplant Surgery Is Associated with Risk, Duration, and Severity of Postoperative Delirium. Annals of the American Thoracic Society. 2016 Feb;13(2):180–187. doi: 10.1513/AnnalsATS.201507-454OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith PJ, Rivelli S, Waters A, et al. Neurocognitive changes after lung transplantation. Ann Am Thorac Soc. 2014 Dec;11(10):1520–1527. doi: 10.1513/AnnalsATS.201406-232OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christie JD, Carby M, Bag R, Corris P, Hertz M, Weill D. Report of the ISHLT Working Group on Primary Lung Graft Dysfunction part II: definition. A consensus statement of the International Society for Heart and Lung Transplantation. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2005 Oct;24(10):1454–1459. doi: 10.1016/j.healun.2004.11.049. [DOI] [PubMed] [Google Scholar]
- 15.Inouye SK, Leo-Summers L, Zhang Y, Bogardus ST, Jr, Leslie DL, Agostini JV. A chart-based method for identification of delirium: validation compared with interviewer ratings using the confusion assessment method. J Am Geriatr Soc. 2005 Feb;53(2):312–318. doi: 10.1111/j.1532-5415.2005.53120.x. [DOI] [PubMed] [Google Scholar]
- 16.Saczynski JS, Kosar CM, Xu G, et al. A tale of two methods: chart and interview methods for identifying delirium. J Am Geriatr Soc. 2014 Mar;62(3):518–524. doi: 10.1111/jgs.12684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 18.Vogl M, Warnecke G, Haverich A, et al. Lung transplantation in the spotlight: Reasons for high-cost procedures. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2016 Oct;35(10):1227–1236. doi: 10.1016/j.healun.2016.05.024. [DOI] [PubMed] [Google Scholar]
- 19.Pandharipande P, Shintani A, Peterson J, et al. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology. 2006 Jan;104(1):21–26. doi: 10.1097/00000542-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Maldonado JR, Wysong A, van der Starre PJ, Block T, Miller C, Reitz BA. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics. 2009 May-Jun;50(3):206–217. doi: 10.1176/appi.psy.50.3.206. [DOI] [PubMed] [Google Scholar]
- 21.Scholz AF, Oldroyd C, McCarthy K, Quinn TJ, Hewitt J. Systematic review and meta-analysis of risk factors for postoperative delirium among older patients undergoing gastrointestinal surgery. The British journal of surgery. 2016 Jan;103(2):e21–28. doi: 10.1002/bjs.10062. [DOI] [PubMed] [Google Scholar]
- 22.Chung KS, Lee JK, Park JS, Choi CH. Risk factors of delirium in patients undergoing total knee arthroplasty. Archives of gerontology and geriatrics. 2015 May-Jun;60(3):443–447. doi: 10.1016/j.archger.2015.01.021. [DOI] [PubMed] [Google Scholar]
- 23.Oh ES, Li M, Fafowora TM, et al. Preoperative risk factors for postoperative delirium following hip fracture repair: a systematic review. International journal of geriatric psychiatry. 2015 Sep;30(9):900–910. doi: 10.1002/gps.4233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lederer DJ, Kawut SM, Wickersham N, et al. Obesity and primary graft dysfunction after lung transplantation: the Lung Transplant Outcomes Group Obesity Study. American journal of respiratory and critical care medicine. 2011 Nov 01;184(9):1055–1061. doi: 10.1164/rccm.201104-0728OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diamond JM, Lee JC, Kawut SM, et al. Clinical risk factors for primary graft dysfunction after lung transplantation. American journal of respiratory and critical care medicine. 2013 Mar 01;187(5):527–534. doi: 10.1164/rccm.201210-1865OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gao M, Sun J, Young N, et al. Impact of Body Mass Index on Outcomes in Cardiac Surgery. Journal of cardiothoracic and vascular anesthesia. 2016 Oct;30(5):1308–1316. doi: 10.1053/j.jvca.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Balachandran S, Lee A, Denehy L, et al. Risk Factors for Sternal Complications After Cardiac Operations: A Systematic Review. The Annals of thoracic surgery. 2016 Dec;102(6):2109–2117. doi: 10.1016/j.athoracsur.2016.05.047. [DOI] [PubMed] [Google Scholar]
- 28.Yusen RD, Edwards LB, Kucheryavaya AY, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-first adult lung and heart-lung transplant report--2014; focus theme: retransplantation. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2014 Oct;33(10):1009–1024. doi: 10.1016/j.healun.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 29.Swigart SE, Kishi Y, Thurber S, Kathol RG, Meller WH. Misdiagnosed delirium in patient referrals to a university-based hospital psychiatry department. Psychosomatics. 2008 Mar-Apr;49(2):104–108. doi: 10.1176/appi.psy.49.2.104. [DOI] [PubMed] [Google Scholar]
- 30.Panitchote A, Tangvoraphonkchai K, Suebsoh N, et al. Under-recognition of delirium in older adults by nurses in the intensive care unit setting. Aging clinical and experimental research. 2015 Oct;27(5):735–740. doi: 10.1007/s40520-015-0323-6. [DOI] [PubMed] [Google Scholar]