Key Teaching Points.
-
•
To treat atrial tachycardia triggering foci that were located in the coronary sinus (CS) with ostial atresia, we performed puncture with a novel method; transseptal puncture from the right atrium septum to the inside of the coronary sinus.
-
•
To perform transseptal puncture of the CS, a crease that is more than 90 degrees and 5 cm from the tip of the Brockenbrough needle must be created. To retain the crease, we used a steerable long sheath (long-curve Agilis) for transseptal puncture.
-
•
This procedure has a high risk of complications such as cardiac tamponade and His bundle/slow pathway injury; therefore, careful judgment is necessary before performing this procedure.
-
•
To treat atrial fibrillation for which the site of earliest activation was found in the left atrium around the ligament of Marshall, we performed endocardial and epicardial ablation with percutaneous pericardial puncture.
Introduction
The coronary sinus (CS) and ligament of Marshall (LOM) have been reported to have arrhythmogenic properties and can initiate atrial fibrillation (AF) triggers as well as participate in left atrial reentrant circuits.1, 2, 3, 4 In a recent study, epicardial and endocardial ablation of the CS in patients with AF after pulmonary vein isolation prolonged the AF cycle length and terminated AF and atrial tachycardia (AT).5 However, a few cases of CS ostial atresia (CSA) involving rare congenital cardiac anatomy exist.6, 7 In these cases, ablation of the CS and LOM is difficult. We present a case of a 44-year-old man with CSA who underwent catheter ablation for AF and AT with a Brockenbrough needle puncture from the right atrium (RA) to the inside of the CS. Percutaneous pericardial puncture was used for the epicardial site.
Case report
A 44-year-old man diagnosed with hypertrophic cardiomyopathy, paroxysmal AF, and sick sinus syndrome was admitted to our hospital because of palpitations and syncope. Pulmonary vein isolation had already been performed at another hospital. We performed linear ablation of the top and bottom of the left atrium (LA), cavotricuspid isthmus linear ablation, and superior vena cava isolation; however, the AF did not terminate. Instead, the AF converted to AT during the ablation procedure targeting complex fractionated atrial electrograms of the LA. Three-dimensional mapping of the AT showed that the bottom of the LA and the lower septal region of the RA were the sites of earliest activation according to LA and RA activation mapping, respectively. The AT did not terminate even though ablation was performed at the sites that were activated the earliest in the LA and RA. Therefore, the foci of the AT were suspected to be in the CS; however, we could not introduce an ablation catheter into the CS from the RA. Multidetector computed tomography revealed CSA, which communicated between the LA and CS via the intraseptal vein (Figure 1). We could not approach the CS from the LA because of the meandering intraseptal vessel; therefore, we approached the CS from the RA by using the Brockenbrough method. Using this method during the second procedure, we were able to insert a steerable long sheath (long-curve Agilis, St. Jude Medical, Minneapolis, MN) into the CS. Angiography of the CS revealed ectasia and demonstrated the vein of Marshall (VOM) (Figure 1). AT was successfully terminated by ablation of the site of earliest activation in the CS (Figure 2). However, a short episode of AF recurred the day after the procedure, and we tried to target the AF trigger during a third procedure. AF-triggering foci were found around the LOM, but not around the CS. The AF was temporarily terminated by ablation of the endocardial side of the LOM; however, it recurred after a short time. Therefore, we performed a percutaneous posterior pericardial puncture in the epigastric fossa and introduced the ablation catheter into the epicardial side. The AF was terminated by ablation in the area of the LOM on the contralateral side of the endocardial site where the AF had been temporarily terminated (Figure 3). The patient has been free of AF for 2 years, without any antiarrhythmic drugs.
Figure 1.
Transseptal approach to coronary sinus ostial atresia (CSA). Multidetector computed tomography revealed CSA. CSA had communication between the left atrium (LA) and the coronary sinus (CS) via the intraseptal vein. Transseptal puncture was performed by Brockenbrough needle and a steerable long sheath. CS angiography revealed ectasia and demonstrated the Marshall vein. AP = anterior posterior; LAO = left anterior oblique; LV = left ventricle; RA = right atrium; RAO = right anterior oblique; RV = right ventricle.
Figure 2.
Atrial tachycardia (AT) in the coronary sinus (CS) roof. Three-dimensional mapping of AT. The bottom of the left atrium (LA) and the low septal region of the right atrium (RA) were the earliest sites of activation according to LA and RA activation mapping, respectively. AT did not terminate even though ablation was performed at the earliest site of activation in the LA and RA. After the Brockenbrough puncture, AT was successfully eliminated by ablation at the earliest site of activation in the CS. ABL = ablation catheter; AP = anterior posterior; HRA = high right atrium.
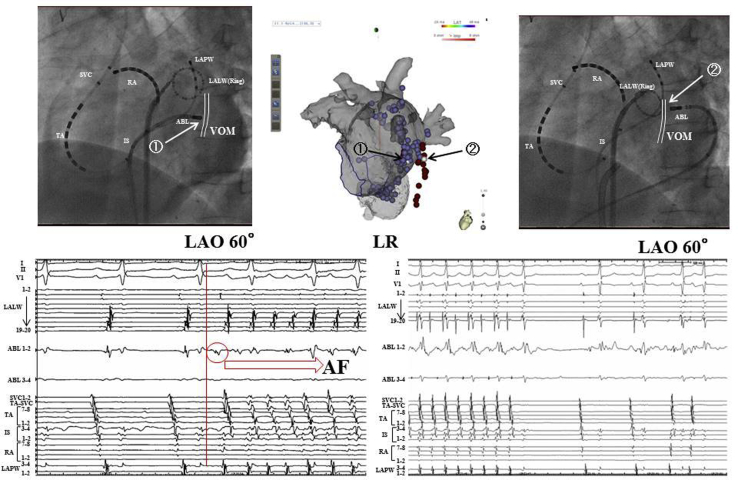
Figure 3.
Hybrid endocardial and epicardial ablation at the vein of Marshall (VOM) site. Atrial fibrillation (AF) was temporarily terminated by ablation at the endocardial side of the VOM (arrow 1), but recurred after short time. AF was terminated by ablation in the VOM area (arrow 2), which was on the contralateral side of the endocardial site where partial success was achieved. AF foci were eliminated by hybrid endocardial and epicardial ablation. ABL = ablation catheter; IS = intraatrial septum; LALW = left atrium lateral wall; LAO = left anterior oblique; LAPW = left atrium posterior wall; LR = left-right; RA = right atrium; SVC = superior vena cava; TA = tricuspid annulus.
Discussion
To our knowledge, this is the first report of the use of transseptal puncture from the RA septum to the interior of the CS for CSA. This procedure has a high risk of complications such as cardiac tamponade; therefore, careful judgment is necessary before performing the procedure. In this case, the patient wanted catheter ablation even though we recommended pacemaker implantation. An anticoagulant drug (apixaban; 10 mg per day) was continued until the day before the catheter ablation. To perform transseptal puncture of the RA of the CS, the location of the CS, whether the CS is close to the RA, and the exit site of the CS orifice should be investigated using computed tomography. In this case, the CS orifice was located at the LA through the ascending septal vein. An intracardiac echocardiography catheter revealed that the CS was close to the RA.
To perform transseptal puncture of the CS, a crease that is more than 90 degrees and 5 cm from the tip of a Brockenbrough needle (St. Jude Medical, Minneapolis, MN) must be created (Figure 1). To retain the crease, we used a steerable long sheath (long-curve Agilis) for transseptal puncture. We illustrated the His bundle on the 3D map in advance. We inserted the sheath into the right ventricle and pulled it toward the RA, with clockwise rotation, to turn the tip of the sheath posteriorly and toward the RA posteroseptal wall where the CS orifice is usually found. We slowly moved the needle tip to the CS and penetrated the septal wall. We did not pull the sheath back from the superior vena cava to the RA because this method may turn the needle tip toward the superior direction and increase the risk of His bundle and slow pathway injuries. We slowly moved the needle tip to the CS and penetrated the septal wall. To avoid the complication of cardiac tamponade and His bundle injury, we aimed toward the posterior CS roof in the 60-degree left anterior oblique projection under fluoroscopic guidance. Constant injection of contrast medium from the needle tip was performed to confirm the location of the needle to avoid the complication of cardiac tamponade. If the CS was visualized by contrast medium infusion, we pushed the needle and sheath slowly into the CS. Great care was taken while pushing because the septal wall is thicker and stiffer than the foramen ovale. When the steerable long sheath was inserted into the CS, we were able to insert an ablation catheter into the CS. It is difficult to transfer the ablation catheter to the CS because of control issues, especially near the entry position of the sheath. Cardiac tamponade is assessed during the ablation period using an intracardiac echocardiography catheter.
Although AT was successfully eliminated by ablation of the earliest activation site in the CS, a short episode of AF sometimes recurred. The site of earliest activation at AF onset was found to be in the lateral LA near the LOM. Hwang et al4 reported that the Marshall bundle can serve as the origin of focal AF. AF was temporarily terminated by ablation of the endocardial side of the LOM, but it recurred after a short time and continued incessantly. Thus, endocardial VOM ablation is not sufficient to target arrhythmogenic cardiomyopathy because of the epicardial structures. Valderrabáno et al8, 9 and Báez-Escudero et al10 reported that retrograde ethanol infusion in the VOM improved the feasibility and ablative effects in the LA tissue. In this case, angiography of the CS clearly demonstrated the VOM; thus, if CSA did not exist, ethanol infusion might be effective for the AF. Báez-Escudero et al10 reported that there was no complication in 80 patients who received ethanol infusion in the VOM. On the other hand, ablation from the epicardial side had a high risk of complications, such as injury to the left bronchus, phrenic nerve, and other adjacent structures. However, we performed epicardial puncture for this patient because we had to perform high-risk transseptal puncture one more time to perform ethanol ablation using a balloon catheter with an inner lumen. We performed percutaneous pericardial puncture and inserted a guidewire toward the cardiac posterior in the 60-degree left anterior oblique projection under fluoroscopic guidance and a steerable long sheath (short-curve Agilis, St. Jude Medical, Minneapolis, MN) was inserted into the epicardial space. It was easier to insert an ablation catheter into the LA using the posterior approach than the anterior approach.11
To avoid complications, we filled the epicardial space with saline, using an irrigation catheter, to gain sufficient capacity before ablation, and performed high-output pacing to avoid phrenic nerve injury.
AF occurred incessantly; thus, we mapped the earliest activating trigger of AF onset. Previous studies described the LOM site as having ganglionated plexuses and continuous fractionated atrial electrograms12; however, in this case, the electrograms were less fractionated and we thought that the fractionation potential decreased because we performed ablation from the endocardial site.
Pak et al5 first used hybrid epicardial and endocardial ablation for AF in 2007. They performed epicardial ablation during 4 redo ablation procedures for persistent AF with a risk of pulmonary vein stenosis and 1 de novo ablation procedure for permanent AF. Three of the 5 cases involved epicardial ablation of the LOM.5 In our case, the AF was terminated during epicardial ablation at the site of the LOM, which was on the contralateral side of the endocardial site where the AF was temporarily terminated. Focal AF originating in the VOM might be a good indication for epicardial ablation.
Conclusion
CSA sometimes involves rare congenital cardiac anatomy. To treat AT-triggering foci located in the CS with ostial atresia, we performed a puncture using a novel method: transseptal puncture from the RA septum to the interior of the CS. As a result of performing epicardial ablation in addition to pericardial puncture for the AF for which the site of earliest activation was found in the LA around the LOM, the patient has been free from atrial fibrillation/tachycardia for 2 years, without any antiarrhythmic drugs.
References
- 1.Chauvin M., Shah D.C., Haïssaguerre M., Marcellin L., Brechenmacher C. The anatomic basis of connections between the coronary sinus musculature and the left atrium in humans. Circulation. 2000;101:647–652. doi: 10.1161/01.cir.101.6.647. [DOI] [PubMed] [Google Scholar]
- 2.Olgin J.E., Jayachandran J.V., Engesstein E., Groh W., Zipes D.P. Atrial macrorentry involving the myocardium of the coronary sinus: a unique mechanism for atypical flutter. J Cardiovasc Electrophysiol. 1998;9:1094–1099. doi: 10.1111/j.1540-8167.1998.tb00886.x. [DOI] [PubMed] [Google Scholar]
- 3.Lin W.S., Tai C.T., Hsieh M.H., Tsai C.F., Lin Y.K., Tsao H.M., Huang J.L., Yu W.C., Yang S.P., Ding Y.A., Chang M.S., Chen S.A. Catheter ablation of paroxysmal atrial fibrillation indicated by non-pulmonary vein ectopy. Circulation. 2003;107:3176–3183. doi: 10.1161/01.CIR.0000074206.52056.2D. [DOI] [PubMed] [Google Scholar]
- 4.Hwang C., Wu T.J., Doshi R.N., Peter C.T., Chen P.S. Vein of Marshall cannulation for the analysis of electrical activity in patients with focal atrial fibrillation. Circulation. 2010;101:1503–1508. doi: 10.1161/01.cir.101.13.1503. [DOI] [PubMed] [Google Scholar]
- 5.Pak H.N., Hwang C., Lim H.E., Kim J.S., Kim Y.H. Hybrid epicardial and endocardial ablation of persistent or permanent atrial fibrillation: a new approach for difficult cases. J Cardiovasc Electrophysiol. 2007;18:917–923. doi: 10.1111/j.1540-8167.2007.00882.x. [DOI] [PubMed] [Google Scholar]
- 6.Noheria A., DeSimone C.V., Lachman N., Edwards W.D., Gami A.S., Maleszewski J.J., Friedman P.A., Munger T.M., Hammill S.C., Hayes D.L., Packer D.L., Asirvatham S.J. Anatomy of the coronary sinus and epicardial coronary venous system in 620 hearts: an electrophysiology perspective. J Cardiovasc Electrophysiol. 2013;24:1–6. doi: 10.1111/j.1540-8167.2012.02443.x. [DOI] [PubMed] [Google Scholar]
- 7.Yan X.L., Dong J.Z., Tang R.B., Ma C.S. Congenital anomalous coronary sinus ostium. Acta Cardiol. 2014;69:319–321. doi: 10.1080/ac.69.3.3027839. [DOI] [PubMed] [Google Scholar]
- 8.Valderrábano M., Liu X., Sasaridis C., Sidhu J., Little S., Khoury D.S. Ethanol infusion in the vein of Marshall: adjunctive effects during ablation of atrial fibrillation. Heart Rhythm. 2009;6:1552–1558. doi: 10.1016/j.hrthm.2009.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valderrábano M., Chen H.R., Sidhu J., Rao L., Ling Y., Khoury D.S. Retrograde ethanol infusion in the vein of Marshall: regional left atrial ablation, vagal denervation and feasibility in humans. Circ Arrhythm Electrophysiol. 2009;2:50–56. doi: 10.1161/CIRCEP.108.818427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Báez-Escudero J.L., Keida T., Dave A.S., Okishige K., Valderrábano M. Ethanol infusion in the vein of Marshall leads to parasympathetic denervation of the human left atrium: implications for atrial fibrillation. J Am Coll Cardiol. 2014;68:1892–1901. doi: 10.1016/j.jacc.2014.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D’Avila A., Koruth J.S., Dukkipati S., Reddy V.Y. Epicardial access for the treatment of cardiac arrhythmias. Europace. 2012;14(Suppl 2):ii13–ii18. doi: 10.1093/europace/eus214. [DOI] [PubMed] [Google Scholar]
- 12.Nakagawa H., Ssherlag B.J., Patterson E., Ikeda A., Lockwood D., Jackman W.M. Pathophysiologic basis of autonomic ganglionated plexus ablation in patients with atrial fibrillation. Heart Rhythm. 2009;6:26–34. doi: 10.1016/j.hrthm.2009.07.029. [DOI] [PubMed] [Google Scholar]