Abstract
Postoperative pain is a common problem after inguinal herniotomy. We aimed to compare the intravenous anesthesia effects of propofol and isoflurane inhalation anesthesia on postoperative pain after inguinal herniotomy. In a randomized clinical trial, 102 eligible patients were selected based on inclusion and exclusion criteria and were randomly divided in two groups. In the first group, propofol was used for the maintenance of anesthesia, while isoflurane was used in the second group. The patient’s heart rate, systolic and diastolic blood pressure and oxygen saturation before, during and after surgery, recovery time and postoperative pain were measured immediately, 2, 4 and 6 hours after surgery and compared between two groups. T-test, and repeated measurement test were used for statistical analysis. No statistically significant differences were observed in heart rate, blood pressure and oxygen saturation levels between the two groups (P > 0.05). Propofol has higher effect in easing postoperative pain of patients than isoflurane, but no difference in postoperative complications, including chills, nausea and vomiting, occurs in both two groups. Propofol is effective in declining the postoperative pain of patients after anesthesia in comparison with isoflurane. Moreover, due to the antioxidant, anti-inflammatory and analgesic properties of propofol, it is preferred to isoflurane and the authors recommended it to be used.
Keywords: intravenous anesthesia, inhalation anesthesia, isoflurane, inguinal hernia, pain, propofol
INTRODUCTION
Inguinal hernia is one of the most human defects and almost affecting 1–5% of people.1 Consequently, the inguinal herniotomy is one of the most common surgical procedures that accompanied with postoperative pain.2 It is an important problem for delay in the return of gastric motility and discharge from hospital. In addition, chronic pain after hernia surgery can affect more than half of patients because of improper treatment prior to the operation.3 Various analgesics could not provide patient satisfaction with postoperative pain treatment. Moreover, opioid drugs may be inappropriate to relieve pain at any dose level without respiratory depression, unbearable nausea, itching, and constipation.4,5 In addition, inadequate pain treatment is related to prolonged hospitalization, more intense pain and increased health care costs.6 Anesthesia is a temporary and short-term situation that can result in consequences after recovery. For example, changes in pain perception are caused in many different ways by anesthetics such as thiopental, which can decrease the pain threshold caused by pressure stimulation and increase heat pain threshold.4,7 Despite it is the most widely used general anesthetic and exhibits analgesic properties, the clinical use of propofol has been debated.8,9,10 It can decrease pain transmission in the rat spinal cord in vitro and in vivo studies and the subliminal dose of propofol has been reported to increase sensitivity to pain in many cases. The mechanism underlying the difference is not clear.11,12 Various studies have also shown a wide range of effects of inhalation anesthetic agents on pain sensitivity; for example, isoflurane exhibits dual effects on pain sensitivity in animal models. This means that it causes an increased sensitivity to pain at low doses and a decreased pain at doses higher than (or close to) the anesthesia dose.13
However, the effects of different anesthetic agents in reduction of postoperative pain during general anesthesia are demonstrated.6,9,11,14 Furthermore, the authors wanted to understand the best anesthesia method that has less postoperative pain besides less opioids need. Moreover, the clinicians look for a method that the patient can return to normal life quickly, as well as determining an adequate anesthesia for general or local surgeries is helpful for patients and physicians. Some contradictory studies have been founded that comparing postoperative pain after anesthesia with isoflurane and propofol.11,12,15,16 This study aimed to compare the effects of intravenous anesthesia with propofol and isoflurane inhalation anesthesia on postoperative pain after inguinal herniotomy in a randomized clinical trial.
SUBJECTS AND METHODS
In this randomized clinical trial, the patients that referred for elective inguinal herniotomy were enrolled in the study that the surgery section of Valiaasr Hospital in Arak, Iran since April 2016 to September 2016. Sample size determination conducted by the statistical methods for sampling in Med Cal software (International Association of Statistical Computing (IASC), Seoul, Korea), regarding to power 0.8 and type one error 0.05. Furthermore, according to our precision 49 patients was needed for each groups. Therefore, 118 patients randomized in two groups and finally 102 ones were analyzed. This RCT was registered in Iranian Registry Clinical Trial with registration No. IRCT2015112925277N1 and was approved by the ethical committee of Arak University of Medical Sciences with approval No. IR.ARAKMU. Res.1394.110.
According to the inclusion and exclusion criteria, after the permission from the chief of surgery, the informed consent was obtained from the eligible participants prior to the initiation of the trial.
All patients were hospitalized in the ward 1 day before their surgery, who were instructed to fast for up to 8 hours prior to the operation. Vital signs including heart rate, systolic and diastolic pressure (mean arterial pressure) and arterial oxygen saturation were measured before induction of anesthesia. Midazolam (0.05 mg/kg) and fentanyl (1 μg/kg) were administered as premedication to all patients. Crystalloid fluids (5 mL/kg body weight) were used for infusion and 100% oxygen was administered by mask to the patient during the first three minutes. In both groups, anesthesia is induced with propofol (2.5 mg/kg) and intravenous atracurium (0.5 mg/kg) is used for endotracheal intubation. The patients undergo mechanical ventilation in order to remain the concentration of exhaled carbon dioxide at 30–35 mmHg and oxygen saturation at 95%. Bispectral index (BIS) monitoring is used in all of the patients, with BIS values kept at 55. Moreover, fentanyl (1 μg/kg) was used at the duration of surgery procedure every half hour. Since the patients were matched regarding to the weight and the surgical procedures were same for two groups, the used fentanyl for maintaining anesthesia was not different.
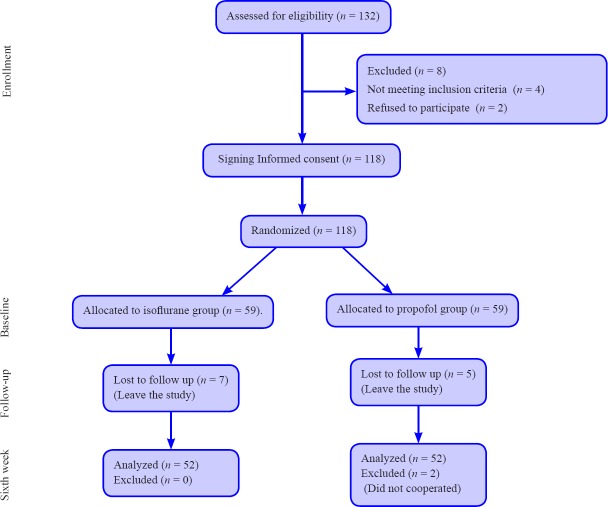
Random allocation for assignment of treatments was conducted by the block randomization method. The block size was considered as 4. The CONSORT diagram for random allocation and follow-up is depicted in Figure 1. Therefore, patients were divided randomly into two equal groups by the methodologist and research team. The agents used for general anesthesia included propofol (1% propofol (100 μg/kg/minute) manufactured by DONGKOOK PHARM. CO., LTD., Korea) in the first group, and isoflurane (Terrell™ Isoflurane, USP Manufactured by Pirimal Critical Care, Inc., Bethlem, PA, USA), 1 minimum alveolar concentration (MAC), was used in the second group. The rate of prescription was varied, depending on the patient needs, to maintain the BIS at 55. At 5 minutes before the end of surgery, the anesthetic gases and propofol infusion were stopped, and duration of intubation and recovery time were recorded. The visual analogue scale (VAS) was used to measure the degree of pain after the full return of consciousness in the recovery room (time zero) and after the patient transfer to the ward up to 6 hours (every 2 hours). The scale is a 10 cm ruler with zero indicating no pain and 10 indicating the unbearable pain. Patients were asked to mark their degree of pain, which is expressed as the distance from the zero point, on the ruler. Vital signs were measured and the incidences of nausea, vomiting, and chills were recorded during this period. In order to satisfy the requirements of a masking of anesthesiologist, an anesthesiology resident who was unaware of the group assignments was responsible for data collection. In cases where the VAS score was greater than 3, diclofenac suppository 100 mg was administered in the postoperative period up to 6 hours and the amount of diclofenac was recorded. The collected data were analyzed using the SPSS 18.0 software (SPSS Inc., Chicago, USA). Descriptive statistical methods and T-test, and analysis of variance for repeated measures were used. The statistical significance considered in 0.05 levels.
Figure 1.
CONSORT diagram showing the flow of participants through each stage of a randomized clinical trial.
RESULTS
Overall, 102 males with inguinal hernia underwent the surgery with two interventions methods for anesthesia including 52 males in propofol group and 52 males in isoflurane group. The baseline measurement for intergroup comparison before intervention was conducted by independent sample t-test and showed that two groups were same at baseline, indicating the random allocation was adequate. According to Table 1, the mean of age, heart rate, systolic and diastolic blood pressure, oxygen saturation, end tidal carbon dioxide (ETCO2) and BIS before surgery were not statistically significant between two groups (P > 0.05).
Table 1.
The baseline measurements for comparing the age, heart rate, systolic and diastolic blood pressure, oxygen saturation, ETCO2 and BIS before induction of anesthesia
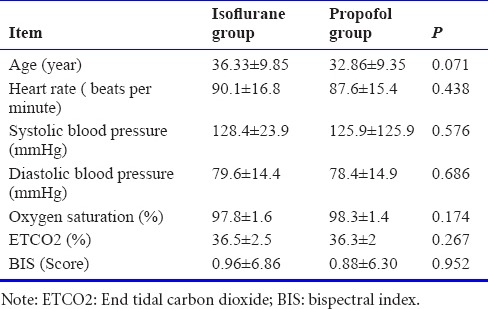
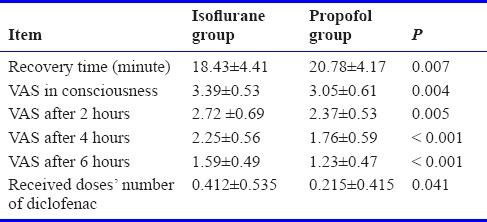
Table 2 shows the comparative results of heart rate, systolic and diastolic blood pressure, oxygen saturation, ETCO2 and BIS between the two groups after induction of anesthesia, during and after intubation and after extubation. Based on our results, there was a significant difference in the oxygen saturation (P = 0.34) and BIS (P = 0.001) between two groups after induction of anesthesia. Nevertheless, there was no significant difference between two groups regarding to the heart rate, systolic and diastolic blood pressure, and ETCO2 (P > 0.05). The independent sample t-test showed that only BIS was significantly different between propofol and isoflurane groups (P = 0.023) after intubation of anesthesia, but other vital signs were not significant at that time (P > 0.05). According to independent sample t-test, after intubation of anesthesia, the heart rate and BIS were statistically significant between propofol and isoflurane groups, but systolic and diastolic blood pressure, oxygen saturation and, ETCO2 were not significant statistically (P > 0.05). Our results showed that after extubation of anesthesia, there was no significant difference between propofol and isoflurane groups regarding to the heart rate, systolic and diastolic blood pressures, oxygen saturation, ETCO2 and BIS (P > 0.05). As seen in Table 3, the mean recovery time of patients in the propofol group was longer than that in the isoflurane group (20.78 ± 4.17 vs. 18.43 ± 4.41), showing a statistically significant difference between the two groups (P < 0.05). Moreover, the mean number of diclofenac suppository and the mean of pain at 2, 4 and 6 hours after the surgery in propofol group was statistically higher than isoflurane group (P < 0.05). Nevertheless, 7.8% of patients in isoflurane and propofol groups have nausea & vomiting (N/V) that were not significant (P = 0.99). Moreover, the rate of chills in propofol group was estimated 33.3% and in isoflurane group that this difference was not statistically significant (P = 0.334).
Table 2.
Comparing the heart rate, systolic and diastolic blood pressure, oxygen saturation, ETCO2 and BIS after induction of anesthesia, after and during intubation and extubation
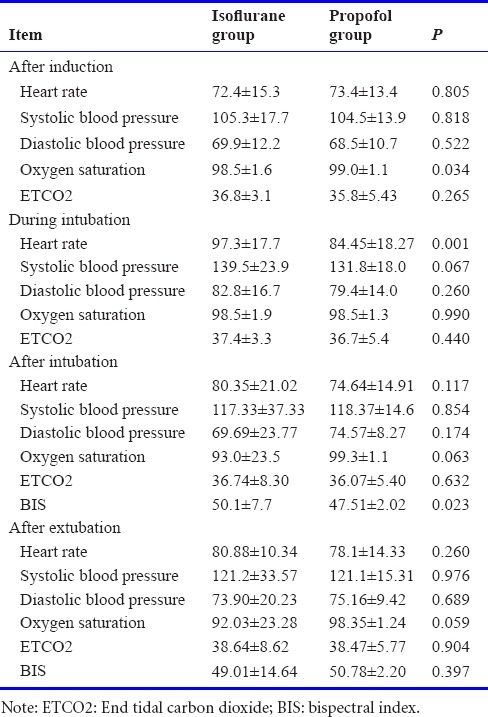
Table 3.
Comparing the recovery time, received doses’ number of diclofenac, and pain severity based on the visual analogue scale (VAS) scores at 2, 4 and 6 hours after the surgery
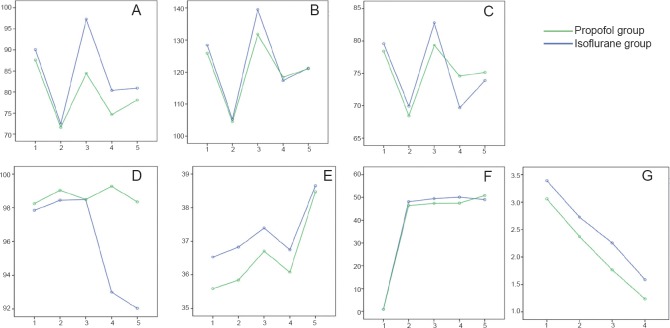
The generalized linear model (GLM) model for repeated measurement analysis showed thatthere was no significant difference in trend in heart rate, systolic and diastolic blood pressure, ETCO2 and BIS between propofol and isoflurane groups (P > 0.05; Figure 2A–C, E, F). Nevertheless the oxygen saturation and VAS score trend was statistically significant between two groups (P = 0.03, P < 0.001; Figure 2D, G).
Figure 2.
The generalized linear model (GLM) model for repeated measurement analysis of vital signs and pain between propofol and isoflurane groups.
Note: (A) Heart rate; (B) systolic blood pressure; (C) diastolic blood pressure; (D) oxygen saturation; (E) end tidal carbon dioxide (ETCO2); (F) bispectral index (BIS); (G) pain. (1) Baseline; (2) after induction of anesthesis; (3) after intubation; (4) during intubation; (5) after extubation.
DISCUSSION
A significant difference in average heart rate is found after intubation between two groups and the mean of heart rate was higher in propofol group than isoflurane group. A significant difference in oxygen saturation was observed after induction of anesthesia and the mean of oxygen saturation was estimately higher in the propofol group than isoflurane group. In addition, there was a significant difference in the mean BIS value at all stages between propofol group and isoflurane group, except after extubation of anesthesia. There was no significant difference in ETCO2, systolic and diastolic blood pressure at all stages of anesthesia. No significant difference in oxygen saturation was found before surgery, after anesthesia and after intubation. Moreover, the propofol group had a longer recovery time and a lower heart rate than the isoflurane group after intubation of anesthesia.
Inadequate treatment for acute postoperative pain can prolong the hospital stay and increase health care costs. Thus, the patient begins to move later and requires different analgesics and narcotics, due to prolonged hospitalization and hospital stay complications, which increase the rate of other perioperative complications.3 Despite the great advances in the surgery, the treatment of postoperative pains remains a major problem. Any factor that causes the patient to use less narcotic pain medication and to move sooner would be beneficial to patients and society.6 Some studies suggest that propofol-based anesthesia can lead to less postoperative pain than other anesthetics.3 Our results showed that the mean of pain scores at 2, 4 and 6 hours after the surgery in propofol group was statistically lower than isoflurane group. Another systematic review and meta-analysis study by Peng et al.11 is the most recent and comprehensive study ever done on the subject and covers 39 clinical studies evaluating 4,520 patients. That study showed that propofol-based anesthesia had the most efficacy in reducing postoperative pain compared to other drugs such as isoflurane, evoflurane and desflurane at 30 minutes, 1 hour and 12 hours after surgery and therefore decreasing the use of opioids11 that was in line with our results. Nevertheless, a report by Hasani et al.14 showed that children anesthetized with propofol had less postoperative pain than those receiving sevoflurane anesthesia which is opposite of our study.
In our study, propofol was compared with Isoflurane for the effects of maintaining anesthesia in adults of 20–50 years. Propofol is an anesthetic widely used in hospitals for anesthesia and sedation which was considered as a drug of choice in 2000 for 96.5% anesthesia and orthopedic surgical procedures in the UK. Propofol can slow down the activity of the central nervous system and perform different functions through action on pre- and postsynaptic cellular and molecular targets. The main mechanism of action of propofol is through γ-aminobutyric acid (GABA)-induced inhibitory postsynaptic activities, which inhibit the transmitter activity of N-methyl-D-aspartic acids (NMDAs) and slow calcium channels and also inhibit sodium channels.9 Moreover, the rate of consequences of surgery including chills and consumption of diclofenac was same between two groups and its differences was not statistically significant. Therefore, it seems that the intensity of pain was same between groups. The results of Peng et al.11 study, though consistent with our study in the incidence of pain, show no difference in the need for medication to control pain between the groups. In this study, which has a higher sample size of patients, other anesthetic agents such as sevoflurane have been used as compared to propofol to evaluate the amount of analgesia at 0.5, 1 and 12 hours after surgery, which includes a longer postoperative duration. In a study by Braz et al.17, isoflurane and propofol were shown to increase antioxidant status in patients undergoing elective surgery. The study points out that surgical procedures are always associated with oxidative stress that can increase reactive oxygen species (ROS), causing damage to human cells. During surgery, activated neutrophils can convert molecular oxygen into ROS such as superoxide radicals and other radicals that help to destroy cellular microorganisms. The neutrophil-produced ROS can be inhibited by some anesthetics, such as propofol and isoflurane. This study highlights the importance of oxidative stress induced by propofol and isoflurane; the former has higher antioxidant effects than the latter. The authors examined the role that the oxidative stress induced by propofol plays in surgery and suggested the general properties of propofol and isoflurane as an antioxidant. Since propofol, as an antioxidant, can increase the concentrations of gamma-tocopherol, it is better than isoflurane; but both drugs do not cause oxidative DNA damage in patients.17 In another study by Sayed et al.,18 the efficacy of propofol and isoflurane on hemodynamics and the inflammatory response was examined in forty patients undergoing coronary artery bypass graft (CABG) surgery, who were divided into two groups receiving propofol and isoflurane. In both groups, inflammatory markers such as CD11, hypoxia inducible factor 1α (HIF-1a), interleukin 8, interleukin 6, C-reaction protein and CD18 were checked before and after surgery and, as compared to the isoflurane group, were found to be significantly lower in the propofol group. In the end, they concluded that propofol has anti-inflammatory properties and can be suggested as the preferred induction agent relative to isoflurane; these results are consistent with the results presented here.18 However, in another study,10 the effects of propofol versus sevoflurane on postoperative pain assessed and the researchers were found to provide the same pain relief and the former was better than the latter. Contrary to our study in which propofol, as compared to isoflurane, has a clear effect on postoperative analgesia, this study found the same postoperative analgesic effects of propofol versus sevoflurane.10 It is considering that the study population was lower than the sample size in our study and consisted of 40 patients undergoing CABG surgery, which is a major and stressful operation.
In general, our study showed that propofol is superior to isoflurane for pain relief at induction of anesthesia and analgesia during surgery. Although, the recovery time for propofol was higher than isoflurane, but this difference is not significant clinically. However, the mean score of pain was lower in the propofol group than isoflurane group. Furthermore, transition to propofol after sevoflurane anesthesia to prevent emergence agitation is recomeneded by Costi et al.19 Moreover, co-administration of sevoflurane/propofol provides better recovery than sevoflurane in combined general/epidural anesthesia.20 Therefore, using isoflurane with propofol might be more effective for surgeries that need to anesthesia. Nevertheless, our study has some limitations worth noting. The variables in our study are simply limited to clinical criteria, and since the drugs used in the study exhibit anti-inflammatory and antioxidant effects, the relevant variables were not included in our study. In addition, it focused on a certain type of surgery.
CONCLUSION
Postoperative pain is a common form that occurs chronic in some situations and eventually leads to problems and interference with the patient’s functions. Propofol is better to reduce postoperative, pain of patients after anesthesia than isoflurane, but there is no difference in consequences such as chills, nausea and vomiting. Therefore, due to its antioxidant, anti-inflammatory and analgesic properties, propofol is preferred to isoflurane.
Acknowledgments
The authors would like to express their gratitude to the Deputy of Research of the University, the Clinical Research Development Center of Vali-Asr Hospital in Arak, Iran and all the colleagues who helped us during the study.
Footnotes
Funding: This work was supported by Arak University of Medical Sciences with fund No. 2262.
Conflicts of interest
There is no conflict of interest.
Research ethics
The study protocol was approved by the the ethical committee of Arak University of Medical Sciences (Approval number IR.ARAKMU.Res.1394.110). The study followed international and national regulations in accordance with the Declaration of Helsinki. The article complied with Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Registration
The trial was registered with Iranian Registry Clinical Trial on December 24, 2015 (identifier: IRCT2015112925277N1).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Contributor agreement
A statement of “Publishing Agreement” has been signed by an authorized author on behalf of all authors prior to publication.
Plagiarism check
This paper has been checked twice with duplication-checking software iThenticate.
Peer review
A double-blind and stringent peer review process has been performed to ensure the integrity, quality and significance of this paper.
Open peer reviewer
Xin-chun Jin, Institute of Neuroscience, Soochow University, China.
REFERENCES
- 1.Haratipour H, Zolfaghari P, Sohrabi MB, et al. External genital abnormalities and inguinal hernia among males of children nurseries, north west of Iran. Int J Pediatr. 2016;4:1407–1411. [Google Scholar]
- 2.Kamal MM, Hassan M. Intravenous esmolol versus ropivacaine abdominal wound infiltration for postoperative analgesia after inguinal herniotomy: a randomized controlled trial. Ain Shams J Anaesthesiol. 2015;8:360. [Google Scholar]
- 3.Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am. 2003;83:1045–1051. doi: 10.1016/S0039-6109(03)00132-4. v-vi. [DOI] [PubMed] [Google Scholar]
- 4.Esmail M, Nilufar D, Majid GE, Reza TN, Abolfazl M. Prophylactic effect of amiodarone in atrial fibrillation after coronary artery bypass surgery; a double-blind randomized controlled clinical trial. J Cardiovasc Dis Res. 2015;6:12–17. [Google Scholar]
- 5.Memari F, Jadidi R, Noroozi A, Mohammadbeigi A, Falahati J. Protecting effect of gabapentin for nausea and vomiting in the surgery of cesarean after spinal anesthesia. Anesth Essays Res. 2015;9:401–404. doi: 10.4103/0259-1162.157469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santos Gde C, Braga GM, Queiroz FL, Navarro TP, Gomez RS. Assessment of postoperative pain and hospital discharge after inguinal and iliohypogastric nerve block for inguinal hernia repair under spinal anesthesia: a prospective study. Rev Assoc Med Bras (1992) 2011;57:545–549. doi: 10.1590/s0104-42302011000500013. [DOI] [PubMed] [Google Scholar]
- 7.Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth. 2005;95:69–76. doi: 10.1093/bja/aei019. [DOI] [PubMed] [Google Scholar]
- 8.Wu Y, Jia N, Zhao C, et al. Synergistic antinociception of propofol-alfentanil combination in mice. Pharmacol Biochem Behav. 2014;116:25–29. doi: 10.1016/j.pbb.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Cheng SS, Yeh J, Flood P. Anesthesia matters: patients anesthetized with propofol have less postoperative pain than those anesthetized with isoflurane. Anesth Analg. 2008;106:264–269, table of contents. doi: 10.1213/01.ane.0000287653.77372.d9. [DOI] [PubMed] [Google Scholar]
- 10.Pokkinen SM, Yli-Hankala A, Kalliomäki ML. The effects of propofol vs. sevoflurane on post-operative pain and need of opioid. Acta Anaesthesiol Scand. 2014;58(8):980–985. doi: 10.1111/aas.12366. [DOI] [PubMed] [Google Scholar]
- 11.Peng K, Liu HY, Wu SR, Liu H, Zhang ZC, Ji FH. Does propofol anesthesia lead to less postoperative pain compared with inhalational anesthesia?: a systematic review and meta-analysis. Anesth Analg. 2016;123(4):846–858. doi: 10.1213/ANE.0000000000001504. [DOI] [PubMed] [Google Scholar]
- 12.Siampalioti A, Karavias D, Zotou A, Kalfarentzos F, Filos K. Anesthesia management for the super obese: is sevoflurane superior to propofol as a sole anesthetic agent? A double-blind randomized controlled trial. Eur Rev Med Pharmacol Sci. 2015;19:2493–2500. [PubMed] [Google Scholar]
- 13.Zhang Y, Eger EI, 2nd, Dutton RC, Sonner JM. Inhaled anesthetics have hyperalgesic effects at 0.1 minimum alveolar anesthetic concentration. Anesth Analg. 2000;91(2):462–466. doi: 10.1097/00000539-200008000-00044. [DOI] [PubMed] [Google Scholar]
- 14.Hasani A, Gecaj-Gashi A, Llullaku S, Jashari H. Postoperative analgesia in children after propofol versus sevoflurane anesthesia. Pain Med. 2013;14(3):442–446. doi: 10.1111/pme.12031. [DOI] [PubMed] [Google Scholar]
- 15.Kumar G, Stendall C, Mistry R, Gurusamy K, Walker D. A comparison of total intravenous anaesthesia using propofol with sevoflurane or desflurane in ambulatory surgery: systematic review and meta-analysis. Anaesthesia. 2014;69(10):1138–1150. doi: 10.1111/anae.12713. [DOI] [PubMed] [Google Scholar]
- 16.Qiu Q, Choi SW, Wong SS, Irwin MG, Cheung CW. Effects of intra-operative maintenance of general anaesthesia with propofol on postoperative pain outcomes - a systematic review and meta-analysis. Anaesthesia. 2016;71(10):1222–1233. doi: 10.1111/anae.13578. [DOI] [PubMed] [Google Scholar]
- 17.Braz MG, Braz LG, Freire CM, et al. Isoflurane and propofol contribute to increasing the antioxidant status of patients during minor elective surgery: a randomized clinical study. Medicine (Baltimore) 2015;94(31):e1266. doi: 10.1097/MD.0000000000001266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sayed S, Idriss NK, Sayyedf HG, et al. Effects of propofol and isoflurane on haemodynamics and the inflammatory response in cardiopulmonary bypass surgery. Br J Biomed Sci. 2015;72:93–101. doi: 10.1080/09674845.2015.11666803. [DOI] [PubMed] [Google Scholar]
- 19.Costi D, Ellwood J, Wallace A, Ahmed S, Waring L, Cyna A. Transition to propofol after sevoflurane anesthesia to prevent emergence agitation: a randomized controlled trial. Paediatr Anaesth. 2015;25:517–523. doi: 10.1111/pan.12617. [DOI] [PubMed] [Google Scholar]
- 20.Liang C, Ding M, Du F, Cang J, Xue Z. Sevoflurane/propofol coadministration provides better recovery than sevoflurane in combined general/epidural anesthesia: a randomized clinical trial. J Anesth. 2014;28:721–726. doi: 10.1007/s00540-014-1803-0. [DOI] [PubMed] [Google Scholar]