Abstract
The bony pelvis is constituted by the ilium, ischium, pubis, and sacrum. The pelvic radiograph is an important component of the skeletal survey performed in suspected skeletal dysplasia. Most of the common skeletal dysplasias have either minor or major radiological abnormalities; hence, knowledge of the normal radiological appearance of bony pelvis is vital for recognizing the early signs of various skeletal dysplasias. This article discusses many common and some uncommon radiological findings on pelvic radiographs along with the specific dysplasia in which they are seen; common differential diagnostic considerations are also discussed.
Keywords: Achondroplasia, pelvic radiograph, skeletal dysplasia
Introduction
The bony pelvis is constituted by ilium, ischium, pubis, and sacrum. The pelvic radiograph is commonly included in routine radiographic examinations, and consequently often serves as the first evidence of skeletal dysplasia. Knowledge of the normal pelvic embryological development is vital for recognizing the early signs of various skeletal dysplasias manifesting in pelvis. The pelvic radiograph often reveals characteristic abnormalities in pelvic shape, size, number of bones, density, timing of ossification, etc., which may provide vital clues in the recognition of various dysplasias. Caffey was the first to recognize the importance of the pelvis in the diagnosis of bone dysplasias when he conducted a detailed analysis of the skeletal anomalies encountered in achondroplasia.[1] Further down the line, Kaufmann[2] described many other patterns of malformation, which shed more light on the significance of pelvis in diagnosing constitutional diseases of bone. This article discusses many common and some uncommon radiological findings on pelvic radiographs along with the specific dysplasia in which they are seen; common differential diagnostic considerations are also discussed.
Ossification
For interpretation of radiographic abnormalities in bony pelvis, thorough knowledge about the ossification centres in and around the pelvis is essential. The time of appearance of the ossification centres is listed in Table 1.
Table 1.
Appearance of ossification centres in bony pelvis
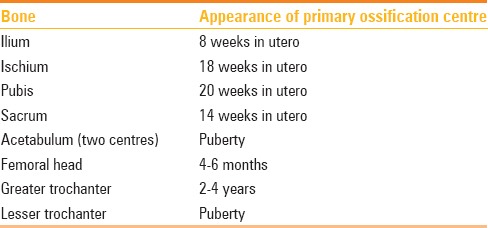
In the full-term neonatal pelvic radiograph, ilium, superior pubic, and ischial rami, 1st to 5th sacral vertebrae, 1st to 4th neural arches, 1st and 2nd lateral centres, and the first coccygeal vertebra are usually seen to be ossified [Figure 1].[3]
Figure 1.
Normal pelvic radiograph in a full term newborn
Abnormalities in different skeletal dysplasias
Iliac bone and acetabulum
Flared iliac wing and flat acetabular roof – Characteristic radiological signs seen in both achondroplasia and lethal dysplasias. The typical appearance in achondroplasia has been given numerous descriptions – “tombstone shape;” “mickey mouse ear pelvis;” “champagne glass pelvis.”
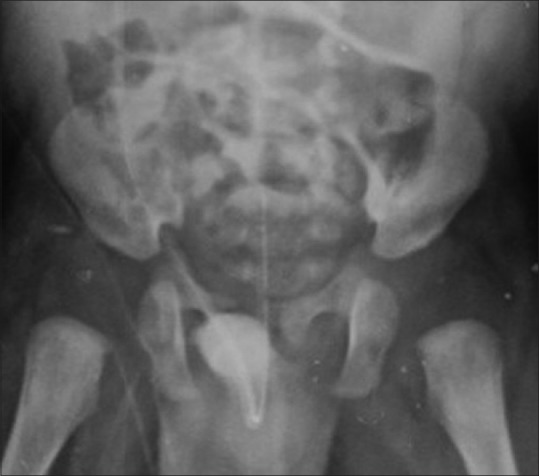
Square iliac wing (vide supra) – Refers to small square-shaped iliac wings akin to a tombstone. This sign is seen in the most common skeletal dysplasia, i.e., achondroplasia. Incidentally, it is also seen in the second most common lethal skeletal dysplasia viz., thanatophoric dysplasia. Rhizomelic dwarfism is a common feature of both dysplasias; however, telephone handle shaped femur, short horizontal ribs, and cloverleaf skull are distinctive features of thantophoric dysplasia.[4] Similarly, champagne glass shaped pelvic inlet, trident hand and pelvis (described below), metaphyseal flaring and horizontal acetabular roof are some of the unique features of achondroplasia that enable easy differentiation between the two entities [Figure 2]
Hypoplastic iliac wing – Seen in several spondyloepiphyseal dysplasias, namely spondyloepiphyseal dysplasia tarda with mental retardation, spondylomegaepihyseal dysplasia, and Dyggve–Melchior Claussen (DMC) syndrome. It should be differentiated from foreshortening of iliac bones in campomelic dysplasia (see below).
Champagne glass pelvis/mickey mouse ear pelvis (also see above) – Refers to the flattening of iliac blades with increased acetabular angles and small sacrosciatic notch giving rise to a champagne glass shaped pelvic inlet. This sign is seen in achondroplasia [Figure 2].
Sloping acetabular roof – Refers to shallow acetabular fossae and steep slope of acetabular roof, which is a common feature in mucopolysacchridosis. Similar finding may also be seen in acetabular dysplasia which may occur as a genetically determined condition or secondary to incomplete reduction of a congenital dislocation, damage to the lateral acetabular epiphysis, or femoral head maldevelopment [Figure 3].[5]
”Trident sign” – Spurs at the medial and lateral acetabular margin and in the center of the acetabulum gives rise to shape resembling a three-pronged spear known as trident [Figure 2]. This sign is seen in achondroplasia, Jeune's asphyxiating thoracic dystrophy (JATD), Ellis-van Creveld syndrome, and thanatophoric dysplasia.[6] Mesomelic pattern of dwarfism and bell shape of the chest are distinctive features of Ellis-van Creveld syndrome.
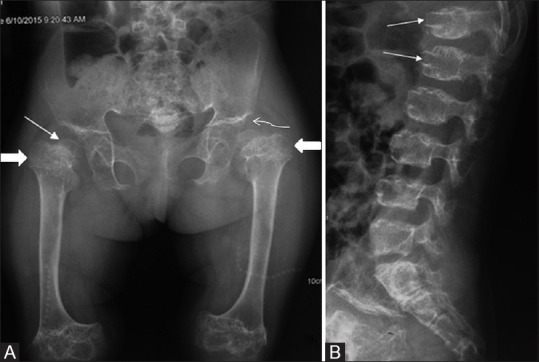
Figure 2.

Pelvis radiograph in achondroplasia shows square shape of the iliac bone, horizontal acetabular roof (squiggly arrow), and rhizomelic shortening of the femur. Also note the trident sign in achondroplasia. The three-pronged pear shape of the sciatic notch is well visualized in this radiograph (straight arrow)
Figure 3(A and B).
(A and B) Pelvis radiograph in mucopolysaccharidosis type I (A) reveals steep sloping of bilateral acetabular roofs (marked), which are irregular. Lumbosacral spine radiograph lateral view (B) of the same patient reveals localized angular kyphosis at the dorsolumbar junction and beak-like projection (arrows) from the inferior aspect of visualized thoracolumbar vertebral bodies (inferior beaking)
The imaging findings in achondroplasia include
Trident pelvis/tombstone shape of the iliac bone
Rhizomelic shortening of long bones with metaphyseal flaring
Gradual narrowing of interpedicular distance in the lumbar spine
Short pedicles of lumbar vertebrae
Large calvarium and a relatively small base
Trident hand (increased gap between third and fourth fingers)
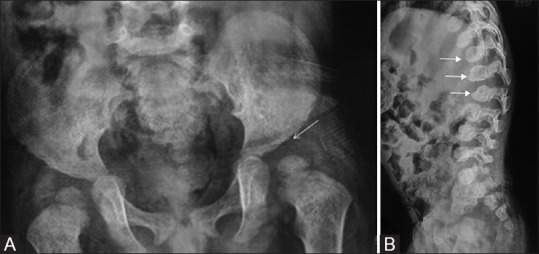
JATD shows short ribs and a narrow thorax [Figure 4].
Figure 4(A and B).
Trident pelvis in Jeune's asphyxiating thoracic dystrophy. Pelvis radiograph (A) shows a flared iliac bone having a trident shape (marked) at sciatic notch. The chest radiograph (B) reveals that the ribs are small and thoracic cavity narrow
Thanatophoric dysplasia is a lethal dysplasia with FGFR3 mutation (allelic but much severe than achondroplasia and hypochondroplasia) with characteristic “cloverleaf skull,” extreme long bone shortening, bowed appearance of long bones (telephone handle shape of femora), more severe rib shortening, and increased platyspondyly with characteristic U and H-shaped vertebrae.[7]
Imaging clues towards Ellis-van Crevald syndrome (clinical setting of post-axial polydactyly, midline cleft lip and cardiac anomalies) include
Trident pelvis
Acro-mesomelic limb shortening
Outward bowing of humeri
Bell-shaped thorax improving with age
Laterally deficient upper tibial epiphyses
Cone shaped epiphyses in hands, capito-hamate coalition
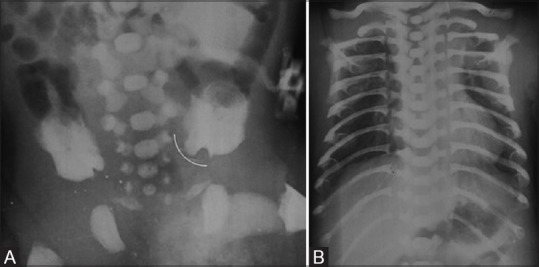
Foreshortened iliac bone – In campomelic dysplasia, the iliac bone is small, oriented in the anterior-posterior direction, and hence appears foreshortened Figure 5. Campomelic dysplasia is a lethal dysplasia associated with XY sex reversal.
Figure 5(A and B).
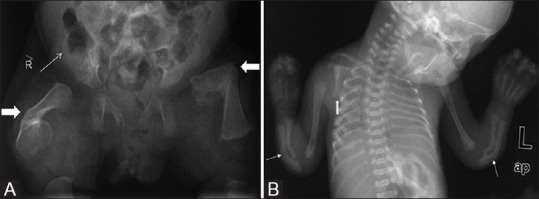
(A, B) Campomelic dysplasia. Radiograph of pelvis (A) of the stillborn fetus shows apparent shortening of the iliac bone (thin arrow); and curved long bone of the lower limb (block arrow). Chest radiograph (B) revealed hypoplastic scapula (thick arrow) and bent radii and ulnae (thin arrows)
This appearance is also seen in chondroectodermal dysplasia and cleidocranial dysostosis. Bowed long bones, hypoplastic scapulae, and narrow chest seen in campomelic dysplasia allow differentiation from these entities.
The imaging pointers towards campomelic dysplasia include
Bowing of long bones of extremities
Angulated bowing of femur at the junction of upper third and middle third
Angulated bowing of tibia at the middle and lower third junction
Small/foreshortened iliac wing
Hypoplastic angle of scapula
Lateral acetabular notch – Refers to a notch at the superolateral margin of the acetabulum seen in acromesomelic dysplasia and in some cases of neonatal hip dysplasia
Lacy iliac wing – This sign is ascribed to the iliac crest irregularity due to dystrophic ossification of the osteochondral junction giving an appearance of a lace border around the iliac crest. This radiological sign is a pathognomonic feature of Dyggve- Melchior Claussen (DMC) syndrome [Figure 6].[8] Other pelvic findings in this syndrome include short iliac wings, wide sacroiliac joints, narrow sciatic notches, wide pubic and ischial rami, dysplastic acetabular fossae, and laterally displaced femoral heads [Figure 6]. Similar findings are seen in enchondromatosis (Ollier's disease) [Figure 7] as well as in Smith-McCort syndrome, a condition clinically and radiologically identical to DMC syndrome except for absence of mental retardation.[9]
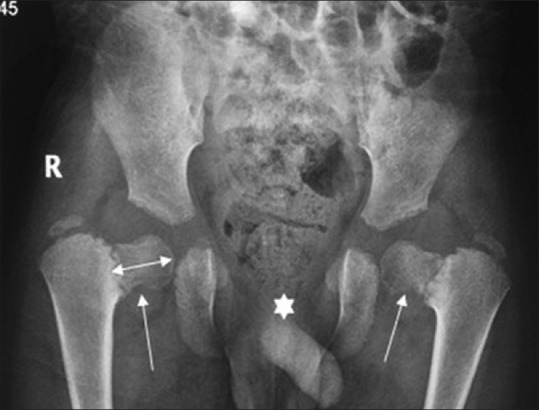
Figure 6.

Dyggve-Melchior Claussen syndrome: Pelvic X-ray demonstrates bilateral iliac crest irregularity (squiggly arrows), wide sacroiliac joints (straight arrow), wide pubic, and ischial rami. Note dysplastic acetabular fossae with abnormally shaped and laterally displaced femoral heads (block arrows)
Figure 7.

Ollier's disease. Pelvic radiograph shows the characteristic lace-like irregular lace-like configuration of the iliac crest margins on both sides (marked). Also of note are the multiple enchondromas in bilateral proximal femoral shafts (marked on left side) and right iliac wing, which point towards the right diagnosis
The imaging pointers towards DMC and Smith-McCort syndrome include
Lacy iliac crest
Dysplastic acetabulum with “laterally placed” femoral heads
Wide sacroiliac joints
Wide pubic and ischial rami
Central notching in the vertebrae
Lace-like appearance of scapular angle
Lacy appearance of iliac wings may also be seen in parastremmatic dwarfism (Greek word parastremmatic = twisted). Symmetrical bowing of the long bones, severe genu valgum, short neck, kyphoscoliosis, etc., permit easy differentiation of this entity from others.
”Paraglider” or “crescent” shape of iliac wing – Deficient mineralization of the iliac wings in achondrogenesis gives rise to the characteristic “paraglider” shape of the iliac wings [Figure 8]. Achondrogenesis is a lethal skeletal dysplasia, with poor mineralization of the skeleton. Three types have been described, type IA, IB, and II. The imaging findings and the disease severity vary in these types. All the three types show a crescent/paraglider shape iliac bone. Type IA is a severe form of the disease, where the skull vault appears completely unmineralized. There is severe shortening of the long bones and the ribs are short and beaded. The vertebral bodies show poor mineralization (c.f: pedicles of thoracic vertebrae unmineralized in Campomelic dysplasia). In type IB, there is a typical expansion of the bony vertebral column at the lumbar level, giving rise to the “cobra head” appearance.
Halberd pelvis – Metatropic dysplasia is a spondyloepimetaphyseal dysplasia with diagnostic radiographic findings comprising of marked platyspondyly, short tubular bones with broad metaphyses, and small epiphyses.[10] The unique shape of the iliac wing – a notch between the shortened iliac body and prominent crescent-shaped iliac wing resembles a two-handed pole weapon known as halberd. This pathognomonic radiological sign distinguishes this entity from other common forms of spondylometaphyseal and spondyloepimetaphyseal dysplasias.
Snail-like appearance of iliac wing – Refers to hypoplastic iliac bones with a snail like configuration [Figure 9]. Seen in Schneckenbecken dysplasia (German for snail pelvis), a rare lethal neonatal chondrodysplasia with autosomal recessive inheritance.[6] Other distinctive features seen in this disorder include flattened and hypoplastic vertebral bodies, short ribs, dumb bell-like appearance of long bones, and precocious ossification of the tarsal bones.[6]
Sunburst appearance of iliac wings – Dense bands of bone radiating from the acetabulum to iliac crest [Figure 10] in a fan-like pattern give rise to “sunburst” appearance which is a characteristic feature of osteopathia striata.[11] Similar bands extending from metaphysis to diaphysis of long bones are the other important radiological feature of this dysplasia.
Posterior iliac horn – Bilateral symmetrical posterior iliac horns [Figure 11] are a unique feature of Nail Patella syndrome (also known as Fong's disease). The horns are formed as a result of exostoses from posterior aspect of iliac bones and are consider as a pathognomonic feature seen in as many as 80% of the patients with this syndrome.[12]
Bone within bone appearance – Increased density of pelvic bones with pelvic endobones (bone within bone) appearance is a classical feature of type II autosomal dominant osteopetrosis [Figure 12].[13]
Multiple scattered sclerotic foci in pelvic bones: Seen in osteopoikilosis, a sclerosing bony dysplasia characterised by multiple bone islands. The pelvis is a common site of involvement with clustering of sclerotic foci around hip and sacroiliac joints [Figure 13].
Figure 8.

Representative illustration depicting relatively well ossified iliac bone with long crescent-shaped medial and inferior margins (arrows) typical of Paraglider shaped pelvis – classical finding seen in achondrogenesis
Figure 9.

Representative illustration depicting extremely small, snail-shaped ilium (left) with a superomedial extension (arrow) resembling a snail's head – seen in Schneckenbecken dysplasia
Figure 10.

Osteopathia striata. Radiograph of the pelvis showing alternating sclerotic bands in the iliac wings (marked)
Figure 11.

Representative illustration depicting typical triangle-shaped excrescence arising from the posterior aspect of the ilium (posterior iliac horn)– classical finding seen in Nail–patella syndrome
Figure 12.

Osteopetrosis. Radiograph of the pelvis reveals generalized sclerosis of the pelvic bones with loss of corticomedullary differentiation
Figure 13.

Osteopoikilosis. Radiograph of the pelvis reveals multiple well defined sclerotic lesions around the pelvis arrows, especially centred around the joints
Sacrum and lower lumbar vertebrae
Calcific Stippling of sacrum and lumbar vertebrae – Seen in chondrodysplasia punctata, especially Sheffield type. This disorder is characterized by calcific stippling of cartilage, particularly epiphyses of long bones.[14] Stippling with rhizomelic shortening can suggest rhizomelic chondrodysplasia punctata [Figure 14].
Figure 14.

Chondrodysplasia punctata in another newborn. Pelvic radiograph shows extensive calcific stippling of sacrum and lower lumbar vertebrae (marked)
The imaging findings include
Stippling of sacral and lumbar vertebrae
Rhizomelic shortening of long bones
Tarsal bone stippling
Coronal cleft vertebrae
Scoliosis
Decreasing interpedicular distance in lumbar vertebrae – seen in achondroplasia (see above)
Medially placed, more rounded pedicles of lumbar vertebrae – Seen in spondylometaphyseal dyaplasia Kozlowski type.
Absent sacral vertebrae – Aplasia/dyslasia of the lumbosacral vertebral bodies is a common feature of caudal regression syndrome, sometimes associated with complete sacral agenesis [Figure 15].
Figure 15(A and B).

Caudal regression syndrome. Lumbosacral spine AP radiograph (A) in a neonate shows absence of lower sacral vertebrae and coccyx. Lateral projection of lumbosacral spine in same patient shows presence of L1 vertebra (marked) with absence of remaining lower vertebrae
Pubic bone and triradiate cartilage
Absent ossification of the pubic bone – Among the pathognomonic features of cleidocranial dysostosis is retarded/absent ossification of the pubic bones which gives rise to an apparent increase in interpubic distance (pseudo diastasis) [Figure 16]. This feature is also seen in achondrogenesis, hypochondrogenesis (short long bones), Sjogren Larssen syndrome, Wolf syndrome, and spondyloepiphyseal dysplasia congenital.[15]
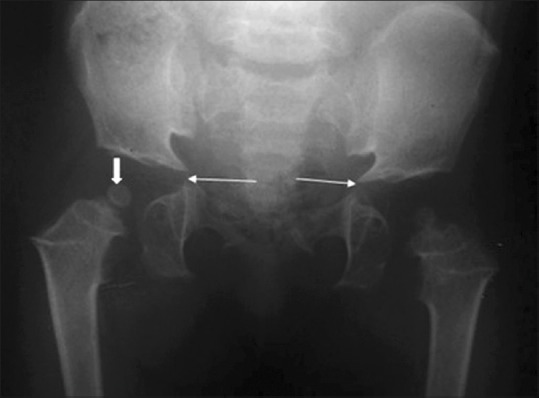
Figure 16.
Cleidocranial dysostosis. Pelvic radiograph revealing retarded ossification of pubic bones resulting in widening of symphysis pubis (pseudo diastasis, asterisk). Also note the elongated shape of capital femoral epiphyses giving a “chef's hat” sign, along with coxa vara (arrows)
Imaging features of cleidocranial dysostosis include
Widely spaced pubic bones, pubic diastasis like appearance
Elongated femoral head (chef's hat sign)
Accessory epiphyses at the second metacarpal base
Wide open cranial sutures
Multiple wormian bones
Multiple unerupted teeth
Distal phalangeal tapering
Hypoplastic/absent clavicles
True dislocation of hip – Superolateral displacement of femoral head and shallow acetabulum is seen in the developmental dysplasia of hip. Other important pelvic radiographic findings include small capital femoral epiphysis, delayed femoral head ossification, and acetabular sclerosis. Delayed femoral head ossification renders plain film radiography unreliable in children less than 12 months of age with ultrasonography being the optimum imaging modality.
Apparent dislocation of hip – Delayed ossification of capital femoral epiphyses and horizontal acetabular roofs result in this radiographic appearance seen in spondyloepiphyseal dysplasia congenita (SEDC). This disease is a type II collagenopathy, having autosomal dominant transmission, and clinical presentations include hearing loss and retinal detachment. Other important pelvic findings in this disorder include metaphyseal flaring, triangular fragment on the inferior aspect of the broad femoral neck, and coxa vara [Figure 17]. Similar findings can also be seen in spondyloepimetaphyseal dysplasia (Strudwick type) [Figure 18], but with more prominent metaphyseal irregularity.
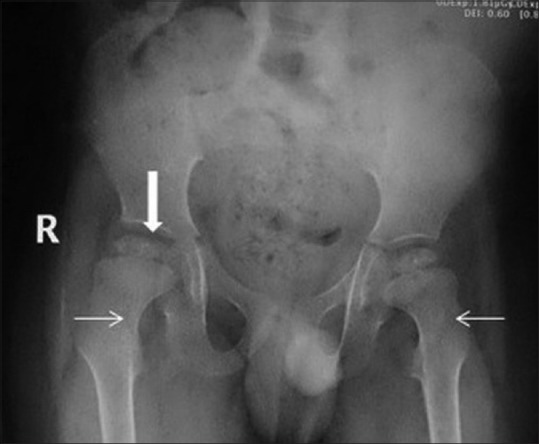
Figure 17(A and B).
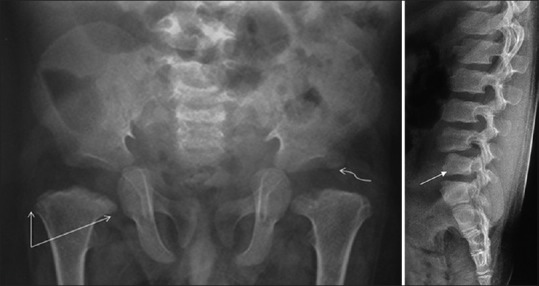
SEDC with pelvic radiograph (A) demonstrating delayed ossification of bilateral femoral heads and horizontal configuration of acetabular roofs (squiggly arrow). Also note bilateral femoral metaphyseal flaring (straight arrows) and coxa vara. Radiograph of lumbosacral spine (B) in the same patient depicts anisospondyly (L4 vertebral body larger than L5 vertebral body) (arrow)
Figure 18.

SEMD: Pelvic radiograph reveals imaging findings similar to SEDC, with metaphyseal flaring and coxa vara – note the prominent metaphyseal irregularity (arrow)
SEDC has the imaging features as follows
Absent ossification of pubic bones
Apparent dislocation of hip joints
Coxa vara
Poorly developed femoral head epiphyses
Platyspondyly
Anisospondyly (variable size of lumbar vertebrae; e.g., L1 bigger than L5)
Spondyloepiphyseal dyaplasia tarda (SEDT), in comparison, has a typical morphology of the vertebral bodies; a “hump” at the posterior two-thirds of the vertebral bodies.
Pubic diastasis – Refers to abnormally wide gap between the pubic bones of >10 mm. This radiological sign is seen in Bladder exostrophy, Prune Belly syndrome, and osteogenesis imperfecta.
Wide triradiate cartilage – Widening and delayed fusion of triradiate cartilage is seen in pseudoachondroplasia [Figure 19].
Figure 19.
Pelvic radiograph in pseudoachondroplasia in a 10-year-old reveals wide triradiate cartilage (arrows) and small femoral head for age (block arrow)
The imaging findings in pseudoachondroplasia are
Square iliac bones (similar to achondroplasia)
Wide triradiate cartilage
Delayed ossification of femoral head
Metaphyseal flaring
Irregular epiphyses
Tongue like projection from anterior aspect of vertebrae
Widened costo-chondral and costo-transverse junction.
Proximal femur and hip joints
Coxa vara – Refers to characteristic hip deformity due to angle between femoral neck and shaft being <120 degrees. This sign is nonspecific and can be seen in many skeletal dysplasias such as spondyloepiphyseal dysplasia congenita, spondyloepimetaphyseal dysplasia Strudwick type, congenital coxa vara with Fairbank's triangle, and pseudoachondroplasia.
Coxa valga – Refers to abnormally increased femoral neck shaft angle which may range normally up to 160 degrees in newborns and 145 degrees in children. This sign is seen in mucoplysacchridosis [Figure 3], Turner syndrome, and developmental dysplasia of hip.
Small capital femoral epiphyses/irregularity and fragmentation/snow cap epiphysis – Seen in Perthes' disease/avascular necrosis of head of femur. If bilateral, search should be made for any history of steroid intake, hypothyroidism, sickle cell disease, and other hemoglobinopathy. ARMED [Figure 20] is an autosomal recessive form of multiple epiphyseal dysplasia which can mimic the appearance of bilateral Perthes' disease.
Figure 20.

Small capital femoral epiphyses in multiple epiphyseal dysplasia. Radiograph of the pelvis shows small and irregular bilateral femoral head (marked); akin to bilateral Perthe's disease. Radiograph of the knee (not shown here) showed irregular epiphyses around the knee joint, and a tibiotalar slant was apparent in ankle radiograph
The imaging findings in multiple epiphyseal dysplasia include
Flattened irregular capital femoral epiphyses
Subluxation of femoral head/protrusio acetabulae
Cone-shaped epiphyses
Irregular carpal bones
Delayed bone age
Double-layered patella, a characteristic finding seen in the lateral knee radiograph, is found in ARMED.
Chef's hat sign – Attributed to deformed capital femoral ossification centre with a rounded appearance and tapered edge directed towards femoral neck which gives the overall impression of a “Chef's Hat.”[16] This sign is a characteristic feature of cleidocranial dysplasia with absent ossification of the pubic symphysis being the other important pelvic sign of this dysplasia [Figure 16].
Prominent medial beak at medial femoral neck – Characteristic feature of pseudoachondroplasia, a rare rhizomelic short limbed skeletal dysplasia which shows radiographic similarity with achondroplasia in many aspects.[17] However, unlike achondroplasia, the skull is normal with normal interpedicular distance and marked platyspondyly [Figure 21].[17]
“Monkey-wrench femora” – Seen in two rare osteochondrodysplasias, i.e., diastrophic dysplasia/desboqouis dysplasia and Larsen's syndrome of Reunion Island. In diastrophic dysplasia, the typical appearance of the femoral heads resembling a Swedish Key or monkey wrench [Figure 22], is a pathognomonic radiological sign with other important radiological features including advanced carpal ossification and radial deviation of the second phalanx with a supernumerary ossicle at base of second phalanx.[18] Larsen's syndrome of Reunion Island shows similar clinical and radiological appearances including monkey wrench femora (inconstant feature), however, extra ossification centre is not seen in these patients enabling differentiation between the two.[18]
Irregular metaphyses of femur – Seen in nutritional rickets, vitamin D dependent rickets, metaphyseal dysplasias, and spondylometaphyseal dysplasias. The different types of metaphyseal dysplasia are Schmidt type, McKusick type [Figure 23], and Jansen type (although several other rarer types exist). Spondylometaphyseal dysplasia group of diseases have additional changes in the spine.
“Corner fracture” at upper femoral metaphysis – Unique radiological feature seen in spondylometaphyseal dysplasia Sutcliffe type.[19] Spondylometaphyseal dysplasia Sutcliffe type (corner fracture type) is a rare disorder involving the spine and the long bone metaphyses. The clinical presentation is with waddling gait and coxa vara with imaging revealing distinctive “corner fractures” at the ends of long bone metaphyses [Figure 24]. Bilateral coxa vara is another important pelvic finding in this disorder. Additional imaging features include irregularity at vertebral endplates, odontoid hypoplasia, and ovoid shape of vertebral bodies. The differential diagnosis of “corner fractures” includes nonaccidental injury of childhood, which needs to be carefully ruled out. Points favoring spondylometaphyseal dysplasia will include the presence of vertebral changes, generalized metaphyseal irregularity, and lack of any other fractures in the body.[19]
Delayed ossification and fusion of femoral head – Feature of Meyer's dysplasia and Perthes' disease. Other differential diagnoses include SEDC, pseudoachondroplasia, multiple epiphyseal dysplasia, hypothyroidism [Figure 25], dyschondroplasia, arthritis, and infection.
Figure 21(A and B).
Pseudoachondroplasia – Pelvic radiograph (A) demonstrating metaphyseal flaring (block arrows), squared iliac wings, and horizontal acetabular roofs (squiggly arrow) akin to achondroplasia. Note that the femoral head are small (straight thin arrow). Also, in lateral spine radiograph (B), the tongue-shaped projection from the lumbar vertebrae (arrows) are a specific imaging finding in pseudoachondroplasia
Figure 22.
Case of Desboqouis dysplasia – Anteroposterior radiograph of the pelvis showing “monkey wrench” appearance of both femora, elevated greater trochanters (thin arrows), coxa vara and dysplastic femoral epiphyses (thick arrow)
Figure 23.

Irregular upper femoral metaphyses in McKusick type metaphyseal chondrodysplasia
Figure 24(A and B).
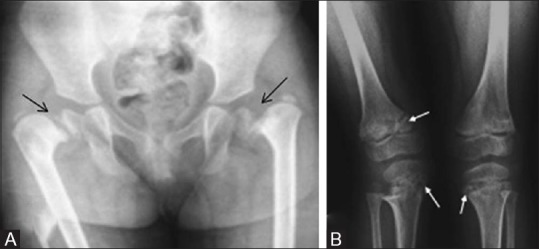
Spondylometaphyseal dysplasia Sutcliffe type – (A) Pelvis with hip joint anteroposterior radiograph reveals bilateral coxa vara and slipped capital femoral epiphyses (B) bilateral knee anteroposterior radiograph reveals metaphyseal fraying with corner fractures (arrows)
Figure 25.

Juvenile hypothyroidism – Pelvic radiograph revealing unfused femoral head epiphysis and apophysis (small arrow) with perisistent triradiate cartilage (arrows) and irregular epiphyses (block arrows)
The imaging clues which can support a diagnosis of juvenile or congenital hypothyroidism are
Delayed bone age
Small irregular epiphyses
Irregular sclerosis of metaphyses
Wide triradiate cartilage
Dorsolumbar kyphosis, bullet-shaped L1 vertebra
Enlarged sella
Delayed ossification of femoral head – Seen in Mucopolysacchridosis, pseudoachondroplasia, spondyloepiphyseal dysplasia, and developmental dysplasia of the hip. Irregular ossification of the femoral head in mucopolysacchridosis along with presence of bilateral coxa vara and bulbous femoral metaphyses in pseudoachondroplasia[20] helps in differentiating between these entities based on pelvic radiographic findings.
Abnormal soft tissue ossification
Seen in fibrodysplasia ossificans progressiva [Figure 26], a rare hereditary mesodermal disorder with pelvic radiographs revealing ectopic soft tissue ossification which may ultimately result in bony bridging between thorax and pelvis.[21]
Figure 26.

Pelvic radiograph in a case of fibrodysplasia ossificans progresiva reveals soft tissue ossification in bilateral thighs adjacent to femur (straight arrows) as well as in righ hemipelvis adjacent to right iliac wing (squiggly arrow)
The imaging findings in this rare condition include
Multiple sheet-like ossification in soft tissues
Bridging ossifications in soft tissues of neck and back
Hallux valgus
Microdactyly of the great toe
Conclusion
Radiograph of the pelvis is an important component of the skeletal survey in suspected skeletal dysplasia. Even in isolation, it can provide a host of information to guide the radiologist towards a possible group of disorders; thus, helping to perform a more specific/targeted search for additional findings to finally reach a diagnosis.
Essentials
Knowledge of the ossification centres in the bony pelvis is very important [Table 1]
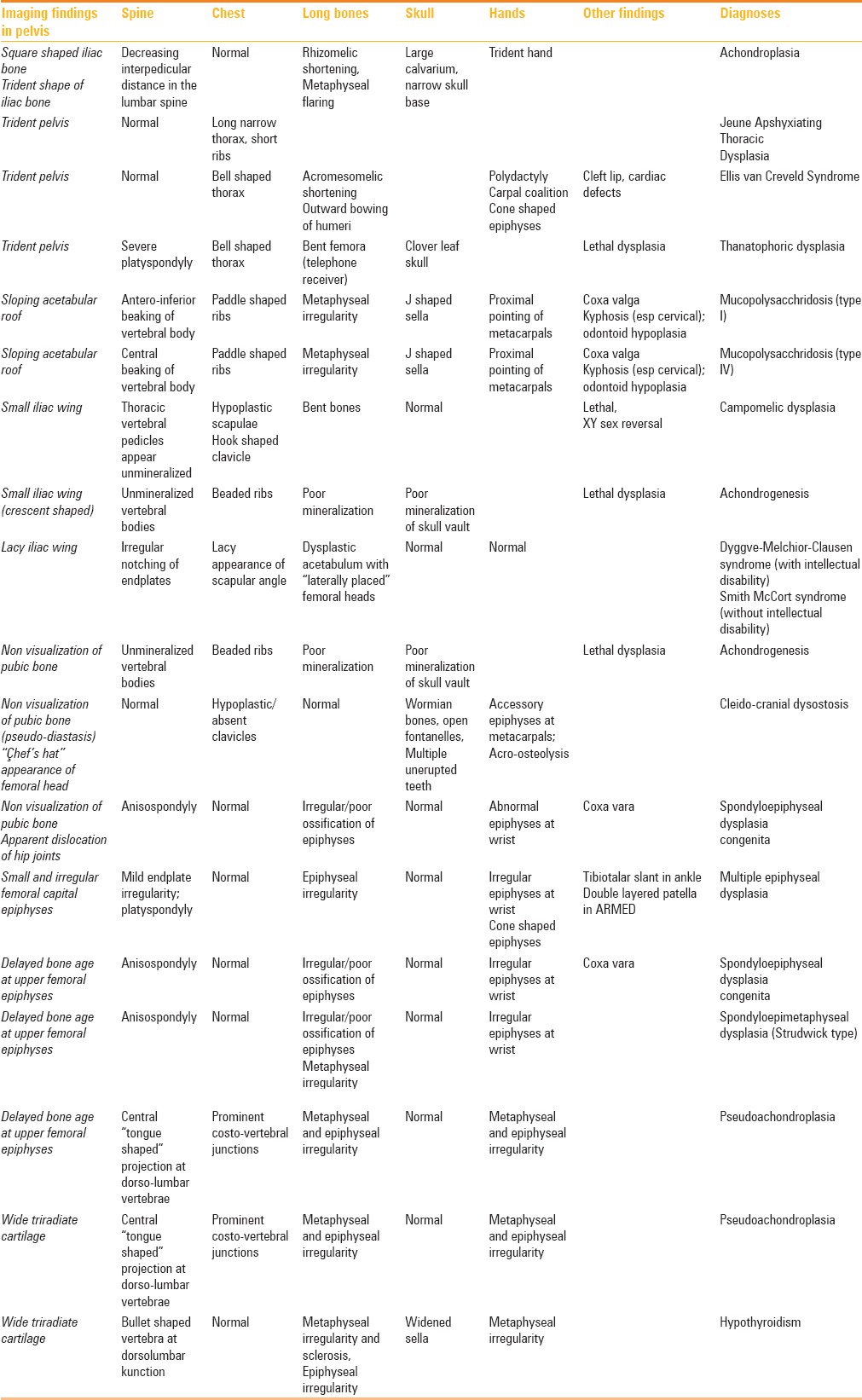
Few named signs and specific morphology can help make a definitive diagnosis in some dysplasias [Table 2]
A combined interpretation of the entire skeletal survey is essential to reach a diagnosis [Table 3].
Table 2.
Differential diagnoses of various imaging findings in pelvis radiograph
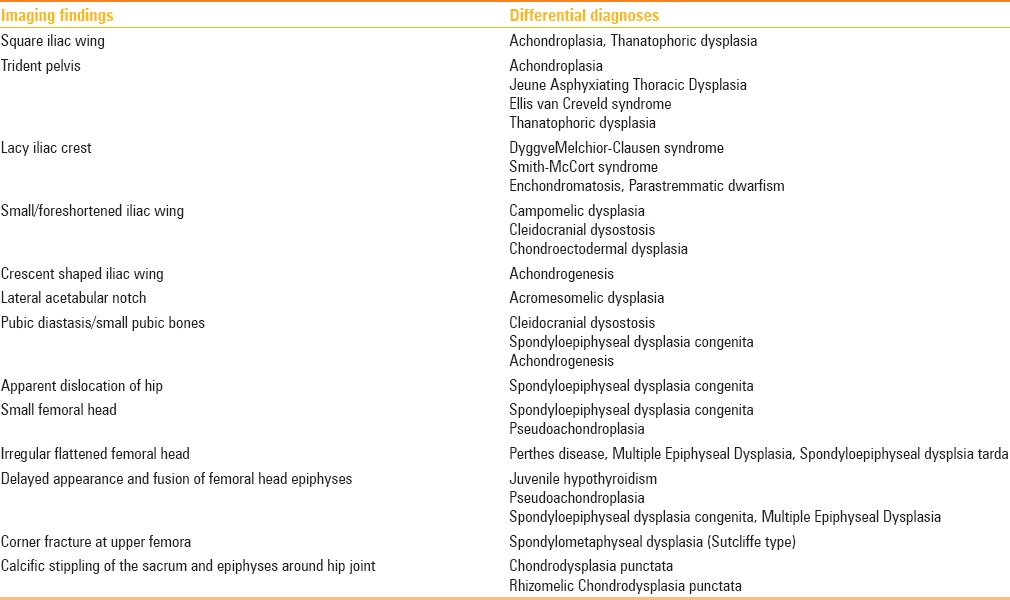
Table 3.
Concise approach of combining findings on pelvic radiograph; along with other pointers towards a definitive diagnoses
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Caffey J. Achondroplasia of pelvis and lumbo-sacral spine: Some roentgenographic features. AJR. 1958;80:449–57. [PubMed] [Google Scholar]
- 2.Kaufmann HJ. Rontgenbefunde am kindlichen becken bei angeborenen skelettaffektionen und chromosomalen aberrationen. Stuttgart, Germany: Thieme; 1964. [PubMed] [Google Scholar]
- 3.Kohler A, Zimmer EA. Borderlands of the normal and early pathologic in skeletal roentgenology. Case JT. 10th ed. New York: Grune and Stratton; 1956. [Google Scholar]
- 4.Sharma M, Jyoti, Jain R, Devendra Thanatophoric Dysplasia: A Case Report. J Clin Diagn Res. 2015;9:QD01–3. doi: 10.7860/JCDR/2015/13201.6702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solomon L, Warwick DJ, Nayagam S. Apley's Concise System of Orthopaedics and Fractures. Third Edition. Boca Raton: CRC Press; 2005. p. 209. ePDF. [Google Scholar]
- 6.Eich GF, Babyn P, Giedion A. Pediatric Pelvis: Radiographic Appearance in Various Congenital Disorders. Radiographics. 1992;12:467–84. doi: 10.1148/radiographics.12.3.1609139. [DOI] [PubMed] [Google Scholar]
- 7.Reid J, Davros W, Paladin A, Lee E, Carrico C. Pediatric Radiology. Oxford: Oxford University Press; 2013. p. 305. [Google Scholar]
- 8.Aglan MS, Temtamy SA, Fateen E, Ashour AM, Eldeeb K, Hosny GA. Dyggve–Melchior–Clausen syndrome: Clinical, genetic, and radiological study of 15 Egyptian patients from nine unrelated families. J Child Orthop. 2009;3:451–8. doi: 10.1007/s11832-009-0211-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta V, Kohli A, Dewan V. Dyggve–Melchior–Clausen syndrome. Indian Pediatr. 2010;47:973–5. doi: 10.1007/s13312-010-0151-x. [DOI] [PubMed] [Google Scholar]
- 10.Sulko J, Marik I, Wisniewska M, Zemkowa D, Kozlowski K. Metatropic dysplasia – case reports. Pol J Radiol. 2008;73:81–4. [Google Scholar]
- 11.Roche CJ, O'Keeffe DP, Lee WK, Duddalwar VA, Torreggiani WC, Curtis JM. Selections from the Buffet of Food Signs in Radiology. Radiographics. 2002;22:1369–84. doi: 10.1148/rg.226025521. [DOI] [PubMed] [Google Scholar]
- 12.West JA, Louis TH. Radiographic findings in the nail-patella syndrome. Proceedings (Baylor University Medical Center) 2015;28:334–6. doi: 10.1080/08998280.2015.11929265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sit C, Agrawal K, Fogelman I, Gnanasegaran G. Osteopetrosis: Radiological & Radionuclide Imaging. Indian J Nucl Med. 2015;30:55–8. doi: 10.4103/0972-3919.147544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanfilippo A, Bartoletti S. Brachytelephalangic chondrodysplasia punctata: A difficult diagnosis. Radiol Case Rep. 2010;51:Article 308. doi: 10.2484/rcr.v5i1.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cortina H, Vallcanera A, Andres V, Gracia A, Aparici R, Mari A. The non-ossified pubis. Paediatr Radiol. 1979;8:87–92. doi: 10.1007/BF00973997. [DOI] [PubMed] [Google Scholar]
- 16.Aktas S, Wheeler D, Sussman MD. The 'chef's hat' appearance of the femoral head in cleidocranial dysplasia. J Bone Joint Surg Br. 2000;82:404–8. doi: 10.1302/0301-620x.82b3.9919. [DOI] [PubMed] [Google Scholar]
- 17.Tandon A, Bhargava SK, Goel S, Bhatt S. Pseudoachondroplasia: A rare cause of rhizomelic dwarfism. Indian J Orthop. 2008;42:477–9. doi: 10.4103/0019-5413.43400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al Kaissi A, Radler C, Klaushofer K, Grill F. Advanced ossification of the carpal bones, and monkey wrench appearance of the femora, features suggestive of a propable mild form of desbeqious dysplasia: A case report and review of the literature. Cases J. 2009;2:45. doi: 10.1186/1757-1626-2-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nair N, Satapathy, Gupta N, Kabra M, AK Gupta, Jana M. Spondylometaphyseal Dysplasia Corner Fracture (Sutcliffe) Type. Indian J Pediatr. 2016;83:1191–4. doi: 10.1007/s12098-016-2121-3. [DOI] [PubMed] [Google Scholar]
- 20.Hefti F. Pediatric Orthopedics in Practice. 2nd edition. Hiedelberg: Springer-Verlag; 2015. p. 767. ebook. [Google Scholar]
- 21.Al-Salmi I, Raniga S, Hadidi AA. Fibrodysplasia Ossificans Progressiva-Radiological Findings: A Case Report. Oman Med J. 2014;29:368–70. doi: 10.5001/omj.2014.97. [DOI] [PMC free article] [PubMed] [Google Scholar]


