Abstract
Introduction
Chronic diseases such as cancer have a strong influence on both physical health and quality of life, which together comprise the concept of health-related quality of life (HRQoL) – in other words, the complete state of physical, social, and psychological functioning. Herein, we review the literature on the theory of HRQoL in relation to oncological diseases.
Material and methods
A literature search of English-language publications that included an analysis of the conceptual models of HRQoL was performed using PubMed. The data were screened and synthesized by all authors and relevant papers were selected.
Results
We outline the theoretical models most often used to conceptualize HRQoL, including the Centre for Health Promotion model from the University of Toronto, the conceptual model of Wilson and Cleary and the contextual model of Ashing-Giwa formulated specifically for cancer patients.
Conclusions
Understanding the theoretical basis of HRQoL is indispensable for valid research in this area.
Keywords: quality of life, health-related quality of life, theoretical model
INTRODUCTION
In determining the effectiveness of therapeutic procedures, modern oncology must not only consider the parameters related to life expectancy, such as the survival rate specific to cancer (cancer specific survival) and overall survival, but also increasingly the patient’s own subjective evaluations of his or her well-being and condition following treatment [1]. In particular, a patient’s quality of life is an important measure of treatment effectiveness, particularly for oncological diseases, where recovery is not necessarily indicative of satisfactory treatment and the patient’s own well-being is not necessarily aligned with the possibility of a permanent cure.
Understanding the mechanism and the theory of quality of life is becoming an important issue among physicians. Indeed, having a good background on this topic allows doctors to conduct better evaluations of patients and more astutely detect the influence of medical treatment on patients ’lives. Thus, the goal of this review is to clarify the theoretical approaches to health-related quality of life and to outline the current specific tools used to assess the quality of life in uro-oncologcial patients.
MATERIAL AND METHODS
A literature search using the MEDLINE/Pubmed and Embase database was performed in order to identify original articles, review articles, and editorials that focused on an analysis of conceptual or theoretical models of health-related quality of life (HRQoL). We limited the search to studies published in the English language. Relevant papers (294 articles) were preselected by two authors, and the list of 12 papers that would be included was edited by all of the authors.
Health-Related Quality of Life
In the past, quality of life referred to ‘having a good life’ and deriving ‘satisfaction from life’. Today, by contrast, quality of life is defined as a statistical index based on multiple parameters – economic, health- related, and environmental related to an individual’s or group’s life conditions. In 1991, Levine proposed a model of socio-psychological quality of life, which is an’ area of human life by which a given person is directly affected and which is important for him or her and as an ’individual perception of position in life within the cultural context and the system of values in which a person lives, in relation to the tasks, expectations and standards set by environmental conditions [2]. Drawing on this definition, Saxen and Orley, in 1997, isolated those factors that make up an individual’s quality of life, including physical health, psychological state, level of independence, relationships with other people and the environment in which the person lives [3]. As research on the quality of life progressed, it was found to play an exceedingly important role in medicine. In the 1990s, assessment of quality of life began to focus on the individual and his or her emotions and inner life. At this point, researchers became interested in not only the objective, quantitative parameters concerning quality of life, but also in its more subjective quality-namely, an individual’s sense of satisfaction.
Also in the 1990s, Schipper and colleagues introduced the concept of quality of life in relation to health namely, HRQoL [4, 5], which they defined as the ‘functional effect of disease and its treatment, as perceived (experienced) by the patient’. Specifically, they noted that a human’s state of health can significantly influence their life and functioning, and might ultimately have some bearing on any assessment of their quality of life. Accordingly, when assessing quality of life in a medical context, healthcare providers should analyze the impact of the disease and therapy on a patient’s life, as subjectively perceived by the patient. In other words, HRQoL can be defined as an index of a patient’s perception of their own position in life made over the course of a particular disease and its treatment.
HRQoL was also defined by the World Health Organization (1997) as ‘individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns" [6].
HRQoL comprises four dimensions: physical and motor skills, mental state, social and economic conditions, and somatic perception (e.g., symptoms, especially pain). Importantly, the concept draws attention to the need to distinguish between an objective state of health (as determined by observed symptoms) and the subjective experience of the patient (i.e., HRQoL) concerning that state using objective and subjective methods of assessment. An objective assessment refers to a method of determining a person’s actual situation, or the facts independent of the person’s subjective opinions or feelings about their particular situation. In contrast, a subjective assessment refers to a method of determining the situation as described by the patient, with sufficient consideration of the emotional dimension of their experience. This assessment should take into account the full range of psychological states – that is, it is important to not only diagnose negative emotional states such as depression and anxiety, but also the positive components of one’s experience, such as satisfaction, hope, and ease of adaptability [7]. Overall, both types of assessments must be used to ensure a full evaluation of a patient’s quality of life.
Theoretical models of the quality of life
A number of theoretical models have been conceived to explain the variety of bio-psycho-social factors that determine quality of life, particularly in the context of a chronic disease such as cancer. Three theoretical models are most frequently cited: the Centre for Health Promotion model, created by Dennis Raphael, Rebecca Renwick, Ivan Brown, and Ted Myerscough in 2002 at the University of Toronto, which relates to quality of life as related to disease in general [8, 9]; the contextual model of HRQoL (CM-HRQoL), developed by Kimlin Tam Ashing-Giwa in 2005,which applies specifically to explaining the health status of cancer patients [10] and a conceptual model of patient outcomes created by Ira Wilson and Paul Clery [11].
The Centre for Health Promotion model is based on the definition of the quality of life by the World Health Organisation [6] and the multidimensional conceptualization of health in other words, it considers quality of life to comprise the dimensions of mental and physical health, social functioning, performance of roles in life and general well-being [2]. Essentially, quality of life according to this model is defined as the extent to which an individual makes use of the opportunities that life brings, particularly in relation to the three most important areas of human life: belonging, being, and becoming. ‘Being’ comprises three main domains, each of which can be further delineated into more precise categories. The first domain of being is physical being, which includes physical health, personal hygiene, nutrition, exercise, grooming and clothing, and general physical appearance. The second domain is psychological being, which includes psychological health and adjustment, cognition (e.g. perception, attention, memory), feelings, self-esteem, self-concept, and self-control. The third main domain is spiritual being, including personal values, personal standards of conduct, and spiritual beliefs. ‘Belonging’ similarly comprises three domains: physical belonging (one’s perception of the home, workplace/school, neighbourhood, and community); social belonging (one’s perception of intimate others, family, friends, co-workers, neighbours, and community members);and community belonging (one’s perception of having an adequate income, health and social services, employment, educational programs, recreational programs, community events, and activities). Finally, ‘becoming’ contains the domains of practical becoming (one’s evaluation of domestic activities, paid work, school or volunteer activities, focusing on achieving one’s health or social needs), leisure becoming (one’s evaluation of activities that promote relaxation and stress reduction), and growth becoming (activities that promote the maintenance or improvement of knowledge and skills, and adapting to change). The specific individual components of quality of life according to this theoretical model are shown in Figure 1.
Figure 1.
Components of the concept of quality of life according to health.
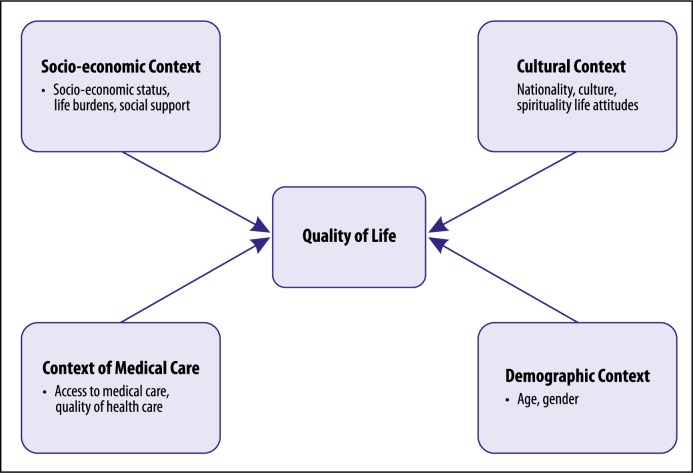
The second model – Ashing-Giwa’s CM-HRQoL – was created specifically to explain the quality of life of
cancer patients [10]. The model comprises two levels: macro and micro. The macro level, also called the systemic level, includes factors outside of the individual that influence his or her functioning and the process of his or her recovery. Among the macro factors, the most prominent are socioeconomic, such as socioeconomic status, life burden, and social support; cultural, such as nationality, culture, spirituality, and life attitudes; demographic, such as age and gender; and related to medical care, such as medical care quality and access. The micro level, also referred to as the individual level, includes those characteristics of an individual that affect his or her functioning and the process of his or her recovery.
They fall into the categories of factors specific to the disease, such as type of illness, the nature of the symptoms and the degree to which they are debilitated; the individual’s general health condition and comorbidities, health beliefs and knowledge, their motivation to engage in health-related behaviour, and the actual patterns of such behaviour; and psychological factors such as the presence of anxiety, depression, anger, hope, optimism, and self-esteem. The micro and macro components of quality of life according to the CM-HRQoL are shown in Figure 2 and Figure 3, respectively.
Figure 2.
Components of the concept of quality of life conditioned by health at the micro level.
Figure 3.
Components of the concept of the quality of life conditioned by health at the macro level.
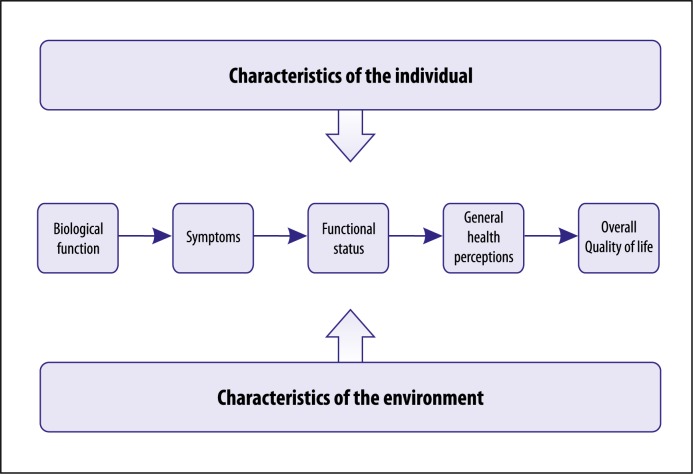
Another prominent model of HRQoL is that developed by Wilson and Cleary [11]. They proposed that general quality of life is perceived as a subjective feeling of happiness and satisfaction with life that is determined by individual factors such as sex, marital status, emotional reactivity to difficult situations, cognitive functions and the degree of motivation to employ corrective measures; social-environmental factors, such as the one’s family, friends, neighbors, place of work, and overall support system; biological factors, such as the functioning of cells, organs, and biological systems; symptoms, or how the patient perceives his/her own physical, emotional, and cognitive status as deviating from the norm; bio- psycho-social functioning, or an individual’s ability to perform tasks in various spheres of life relating to their physical, social, and psychological functioning and role playing; and the general perception of health, or an individual’s subjective assessment of their own health status. As can be seen in Figure 4, the model is organized such that the personal and environmental characteristics influence the biological processes, which in turn jointly influence the remaining elements of the model.
Figure 4.
Elements of quality of life conditioned by health status.
HRQoL among uro-oncological patients
The field of psycho-oncology has several additional definitions of quality of life, most of which are used as supplements of the more general definitions of HRQoL, thereby extending them to suit an oncological context. One such definition is the ‘functional effect of illness and its treatment which can lead to a subjective evaluation of life as a whole’ [12]. This definition includes four aspects of human functioning – physical, emotional, cognitive, and social. Another definition is ‘the general evaluation of the quality of life is a picture of a patient’s life situation assessed by the person at a given period of time’ [13]. This definition covers two dimensions: cognitive and emotional. The cognitive dimension refers to a patient’s assessment of quality of life according to information obtained on his/her disease and life situation, thus enabling the patient to evaluate his/her disease and its influence on quality of life. The emotional dimension refers to the various emotional states arising from the individual’s experience of his/her illness, as well as the strategies for coping with the illness.
It is important to note that all models of quality of life emphasize the subjective nature of its assessment. In general, an evaluation of HRQoL aims to describe the patient’s perceived degree of satisfaction with their general health status in comparison with their ideal health status. When evaluations of quality of life are carried out by a physician, they draw on the physician’s opinion, which are based on the more objective indicators of the patient’s health, status in addition to considering the patient’s own subjective evaluation according to his/her subjective experience of the disease.
When assessing uro-oncological patients’ HRQoL, three types of questionnaires are used [14]. First, there are generic questionnaires that universally evaluate patients, regardless of their diagnosis. Examples include the Short Form 36 [15] or the WHO Quality of Life-BREF [16]. Second, there are cancer-specific questionnaires, such as the European Organisation for the Research and Treatment of Cancer QLQ-C30 [17] or Functional Assessment of Cancer Therapy-General [18]. Third, there are cancer-specific (urological-cancer-specific) questionnaires available to use. Uro-oncological specific tools have been studied in many systemic reviews in the past; a number of recent publications [14, 19–28] are shown in Table 1. Since every disease or disorder has specific symptoms, it is often more effective to use a tool specific to that disease for monitoring patients’ state. While a generic tool might, for example, contain a question on patients’ pain level, a disease-specific questionnaire might contain a question about feeling pain in specific areas, thus giving physicians a better understanding of a patients’ well-being at that particular point.
Table 1.
Recent publications on the quality of life assessment tools in uro-oncology
| Author | Year of publication | Journal | Type of review | Topic |
|---|---|---|---|---|
| Mohamed N, et al. [19] | 2016 | Bladder Cancer | Review | Bladder |
| Bergman J, et al. [20] | 2014 | Nat Rev Urol | Review | Prostate |
| Wright J, et al. [21] | 2007 | Nat Clin Pract Urol | Review | Bladder |
| Liu J, et al. [22] | 2010 | Cancer Invest | Review | Kidney |
| Maddineni S, et al. [23] | 2009 | BMC Urol | Systemic review | Penile |
| Hamoen E, et al. [24] | 2015 | Urol Oncol | Systemic review | Prostate |
| Schmidt S, et al. [25] | 2014 | Qual Life Res | Systemic review | Prostate |
| Broering J, et al. [26] | 2014 | Qual Life Res | Review | Prostate |
| Sosnowski R, et al. [14] | 2016 | Minerva Urol Nefrol | Systemic review | Prostate, bladder, kidney |
| Bergman J, et al. [27] | 2010 | J Urol | Systemic review | Prostate, bladder, kidney |
| Heldwein F, et al. [28] | 2009 | Arch Esp Urol | Systemic review | Prostate, bladder, kidney |
Instruments that assess patients’ mental adaptation to their disease are often used when analyzing the quality of life of cancer patients; this allows for the expansion and refinement of the assessment of the quality of life and functioning to cover the emotional and social dimensions. The patient’s psychological adaptation to cancer is inextricably linked with their quality of life. In the oncological literature, a two-way relationship of the mental adaptation to cancer vis-à-vis HRQoL is often found and this relationship appears to be synergic in nature. The overall level of quality of life and physical functioning, as well as the emotional and social development of the patient, often determine, maintain, or induce changes in attitudes towards disease and one’s strategies for dealing with it. Indeed, greater quality of life together with decreased dysfunctionality and fewer distressing symptoms in all of the various dimensions of quality of life are associated with stronger engagement in treatment and a more positive attitude towards the disease, as well as fewer severely negative emotions. Furthermore, attitudes towards the disease and one’s disease-related coping strategies bring about specific behavioural and emotional reactions, which in turn have a significant impact on the overall quality of life and physical functioning at various levels.
In 1999, Siegfried Juczyński classified the various attitudes associated with mental adaptation to cancer into four groups: stoic acceptance and positive re-evaluation; a fighting spirit; denial and preoccupation with anxiety; and helplessness-hopelessness [29]. This classification is based on the results of the Mini-MAC [30]. The active, constructive engagement in coping with cancer, manifested as a ‘a desire to fight the disease’ and a positive re-evaluation of one’s situation (i.e., the first two groups) are often associated with a better overall quality of life and with better physical, emotional, and social functioning overall. In contrast, less active, more destructive involvement in coping, manifested as anxiety, self-absorption, and feelings of helplessness and hopelessness (i.e., the second two groups), is associated with a much poorer quality of life and with far worse functioning in all domains. Together, these attitudes make up two types of mental adaptation strategies to disease: the constructive (manifesting as active, optimistic and highly self-sufficient struggle with the illness) and the destructive (dominated by feelings of helplessness and hopelessness, anxiety, a fatalistic attitude, a low sense of self-sufficiency, and, upon becoming totally inactive, a complete withdrawal into the self).
Since patient’s evaluation of their quality of life is strongly connected with a number of psychological outcomes, it should be taken into account and monitored carefully during the disease and healing processes. It can help understanding in which areas one’s functioning can be improved and by modifying them, patient’s mental adaptation can be improved.
CONCLUSIONS
The above theoretical models of HRQoL are important for understanding the mechanisms that determine patients’ HRQoL. More specifically, understanding what factors determine HRQoL enables proper evaluation of these factors for a better understanding of a patient’s state during chronic illness.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118:622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- 2.Levine NM. In: Incorporation of quality of life assessment into clinical trials in: effect of cancer on quality of life. Osoba D, editor. CRC Press; 1991. [Google Scholar]
- 3.Saxena S, Orley J. Quality of life assessment: The world health organization perspective. Eur Psychiatry. 1997;12(Suppl 3):263–266. doi: 10.1016/S0924-9338(97)89095-5. [DOI] [PubMed] [Google Scholar]
- 4.Schipper H. Quality of life: principles of the clinical paradigm. J Psychosocial Oncology. 1990;8:171–185. [Google Scholar]
- 5.Schipper H, Clinch JJ, Olweny CLM. Quality of life studies: definitions and conceptual issues. In: Spilker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia: Lippincott- Raven Publishers; 1997. pp. 11–23. [Google Scholar]
- 6.WHOQOL Measuring Quality of Life. World Health Organization. 1997. [2016 Oct 1] Available from: http://www.who.int/mental_health/media/68.pdf.
- 7.de Walden-Gałuszko K. In: Ocena jakości życia uwarunkowana stanem zdrowia. Meyza J, editor. Warszawa: Centrum Onkologii; 1997. [Google Scholar]
- 8.Renwick R, Raphael D, Brown I, Myerscough T. The Quality of Life Model, The Centre for Health Promotion. 2002. [2016 Oct 1] Available from: http://www.utoronto.ca/qol/qol_model.htm.
- 9.Raphael D, Brown I, Renwick R, Rootman I. Assessing the quality of life of persons with developmental disabilities: Description of a new model, measuring instruments, and initial findings. International Journal of Disability, Development and Education. 1996;43:25–42. [Google Scholar]
- 10.Ashing-Giwa KT. The contextual model of HRQoL: a paradigm for expanding the HRQoL framework. Qual Life Res. 2005;14:297–307. doi: 10.1007/s11136-004-0729-7. [DOI] [PubMed] [Google Scholar]
- 11.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273:59–65. [PubMed] [Google Scholar]
- 12.Aaronson N, Cull A, Kaasa S, Sprangers M. The EORTC modular approach to quality of life assessment in oncology. Int J Ment Health. 1994;23:75–96. [Google Scholar]
- 13.de Walden-Gałuszko K. Jakość życia - rozważania ogólne. In: Wydawnictwo UG, editor. Jakość życia w chorobie nowotworowej. Gdańsk; 1994. pp. 13–19. [Google Scholar]
- 14.Sosnowski R, Kulpa M, Kosowicz M, et al. Basic methods for the assessment of the health related quality of life in uro- oncological patients. Minerva Urol Nefrol. 2016 doi: 10.23736/S0393-2249.16.02726-0. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 16.Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 17.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 18.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 19.Mohamed NE, Gilbert F, Lee CT, et al. Pursuing Quality in the Application of Bladder Cancer Quality of Life Research. Bladder Cancer (Amsterdam, Netherlands) 2016;2:139–149. doi: 10.3233/BLC-160051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bergman J, Laviana A. Quality-of-life assessment tools for men with prostate cancer. Nat Rev Urol. 2014;11:352–359. doi: 10.1038/nrurol.2014.101. [DOI] [PubMed] [Google Scholar]
- 21.Wright JL, Porter MP. Quality-of-life assessment in patients with bladder cancer. Nat Clin Pract Urol. 2007;4:147–154. doi: 10.1038/ncpuro0750. [DOI] [PubMed] [Google Scholar]
- 22.Liu J, Mittendorf T, von der Schulenburg JM. A structured review and guide through studies on health-related quality of life in kidney cancer, hepatocellular carcinoma, and leukemia. Cancer Invest. 2010;28:312–322. doi: 10.3109/07357900903287022. [DOI] [PubMed] [Google Scholar]
- 23.Maddineni SB, Lau MM, Sangar VK. Identifying the needs of penile cancer sufferers: a systematic review of the quality of life, psychosexual and psychosocial literature in penile cancer. BMC Urol. 2009;9:8. doi: 10.1186/1471-2490-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamoen EH, De Rooij M, Witjes JA, Barentsz JO, Rovers MM. Measuring health-related quality of life in men with prostate cancer: A systematic review of the most used questionnaires and their validity. Urol Oncol. 2015;33:19–28. doi: 10.1016/j.urolonc.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Schmidt S, Garin O, Pardo Y, et al. Assessing quality of life in patients with prostate cancer: a systematic and standardized comparison of available instruments. Qual Life Res. 2014;23:2169–2181. doi: 10.1007/s11136-014-0678-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Broering JM, Paciorek A, Carroll PR, Wilson LS, Litwin MS, Miaskowski C. Measurement equivalence using a mixed-mode approach to administer health-related quality of life instruments. Qual Life Res. 2014;23:495–508. doi: 10.1007/s11136-013-0493-7. [DOI] [PubMed] [Google Scholar]
- 27.Bergman J, Gore JL, Singer JS, Anger JT, Litwin MS. Readability of health related quality of life instruments in urology. J Urol. 2010;183:1977–1981. doi: 10.1016/j.juro.2009.12.107. [DOI] [PubMed] [Google Scholar]
- 28.Heldwein FL, Sanchez-Salas RE, Sanchez-Salas R, et al. Health and quality of life in urology: issues in general urology and urological oncology. Arch Esp Urol. 2009;62:519–530. [PubMed] [Google Scholar]
- 29.Juczyński Z, Chrystowska-Jabłońska B. Strategie radzenia sobie z chorobą nowotworową. Psychoonkologia. 1999;5:3–9. [Google Scholar]
- 30.Watson M, Greer S, Young J, Inayat Q, Burgess C, Robertson B. Development of a questionnaire measure of adjustment to cancer: the MAC scale. Psychol Med. 1988;18:203–209. doi: 10.1017/s0033291700002026. [DOI] [PubMed] [Google Scholar]