Abstract
Introduction
Urinary stone disease is a major urological condition. Endourologic techniques have influenced the clinical approach and outcomes. Open surgery holds a historic importance in the management of most conditions. However, complex kidney stone burden may be amenable to successful results with open stone surgery. In this article, we report our eighteen cases of complex urinary stone disease who underwent open stone removal.
Material and methods
A total of 1701 patients have undergone surgical treatment for urinary stone disease in our clinic between July 2012 and July 2016, comprising eighteen patients who underwent open stone surgery. Patients’ demographic data, stone analysis results, postoperative clinical data, and stone status were evaluated retrospectively. The choice of surgical approach is mostly dependent on the surgeon’s preference. In two patients, open surgery was undertaken because of perioperative complications.
Results
We did not observe any Clavien-Dindo grade 4 or 5 complications. Three patients were managed with a course of antibiotics due to postoperative fever. One patient had postoperative pleurisy, one patient had urinoma, and two patients had postoperative ileus. Mean operation time was 84 (57–124) minutes and mean hospitalization time was 5.5 (3–8) days. Stone-free status was achieved in 15 patients (83.3%).
Conclusions
Endourologic approaches are the first options for treatment of urinary stone disease. However, open stone surgery holds its indispensable position in complicated cases and in complex stone burden. Open stone surgery is also a valid alternative to endourologic techniques in all situations.
Keywords: urinary stone disease, open stone surgery, complex stone disease
INTRODUCTION
Urinary stone disease has been well known since ancient times [1]. Before the endourology era, the main approach has relied on conservative surveillance or open stone removal. Since the technical advancements of surgical instruments and the evolvement of the main clinical approach to stone disease through endourologic options, contemporary management of the disease consists mainly of minimally invasive techniques [2, 3]. Open surgery for most urinary stones currently holds only a historical importance. However, mainly in endemic areas, urologists still faced patients with complex urinary stone disease. The main appearance of the complex urinary stone disease occurs as high stone burden and anatomical anomalies of the collecting system [4, 5] (Figure 1). In these patients, several minimally invasive interventions with consequent Shock Wave Lithotripsy (SWL) sessions may be required. Open surgery, despite its more invasive nature, can be offered as an initial treatment option to these patient groups for a high stone clearance rate with fewer interventions. Hence, the aim of this retrospective study is to evaluate the success and complications of open stone surgery in contemporary endourologic practice. In this article, we report 18 complex urinary stone disease cases that have undergone open surgery in our clinic with satisfactory results and low complication rates.
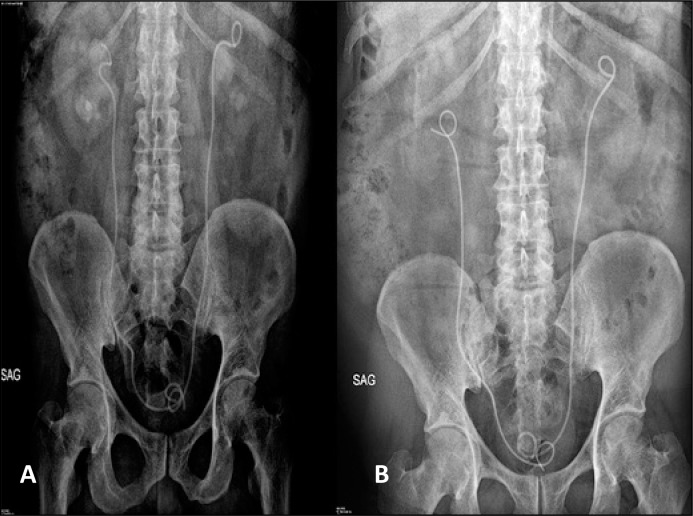
Figure 1.
A. Preoperative KUB X-Ray of the patient have massive pelvicalyceal stone burden with steinstrasse at the right ureter. B. After postoperative first year KUB X-Ray of the same patient after right open pyelolithotomy and nephrolithotomy with ureterolithotomy.
MATERIAL AND METHODS
Between July 2012 and July 2016, 1701 patients underwent surgical treatment of urinary stone disease. Among them, 322, 1361, and 18 patients underwent percutaneous nephrolithotomy (PCNL), ureterorenoscopy (URS), and open stone surgery, respectively. Retrograde intrarenal surgery (RIRS) was initiated in our clinic at the end of 2015. Therefore, a relatively low number of patients who underwent RIRS procedures were not included in this retrospective cohort. Patients’ data were evaluated retrospectively. All patients were evaluated for any hematologic or internal disease and a plain Kidney-Ureter-Bladder (KUB) X-Ray, Intravenous Urography (IVU), and Non-Contrast Computerized Tomography (NCCT) scan of the abdomen were obtained before surgery. Urine cultures were obtained routinely. Patients with positive cultures were operated after proper antibiotic therapy and sterilization of urine. Patients with negative urine cultures were operated under second-generation cephalosporin prophylaxis. Among our patient cohort, some patients hold unique importance; one patient had a pelvic kidney and one patient had a horseshoe kidney (Figure 2), two patients underwent left and right open pyelolithotomy in different sessions (Figure 3), one patient had previous URS history with forgotten Double J (DJ) ureteral stent which was broken in the middle by a bladder stone (Figure 4). In two patients, open surgery was undertaken due to failure to obtain percutaneous access and total ureteral stripping. In the remaining patients, the surgical approach was determined based on surgeons’ experience and with patients’ informed consent. Surgeries were performed by four different surgeons in our institution and all surgeons had more than 10 years of experience in urology. High stone burden with Cumulative Stone Diameter (CSD) exceeding 5 cm, rotation anomaly, concurrent ureteropelvic junction obstruction and staghorn stones involving all calyces were considered for open surgery. Demographic data of our patient group is summarized in Table 1.
Figure 2.
A. Pelvicalyceal radio-lucent stone in the left pelvic kidney. Image is obtained at the pyelogram phase of IVU. B. NCCT scan of the same patient showing location of the kidney and the urinary stone.
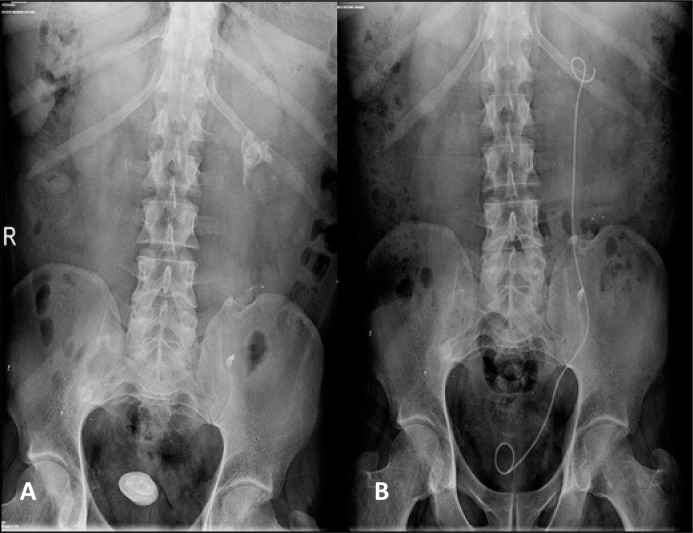
Figure 3.
A. Preoperative KUB X-Ray of the patient who had undergone emergency bilateral ureteral double pigtail stent placement due to acute renal failure in a foreign health center. B. Postoperative KUB X-Ray of the same patient after two consequent open pyelolithotomy sessions for left and right kidney stones.
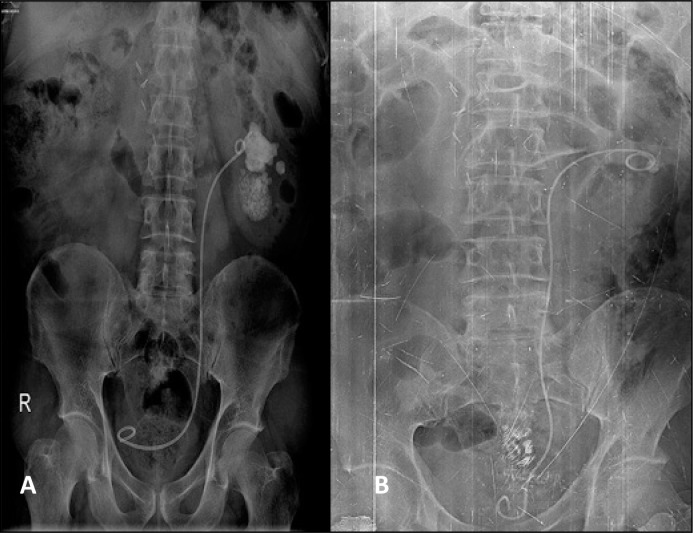
Figure 4.
A. Preoperative KUB X-Ray showing forgotten and broken DJ ureteral stent with bladder and kidney stone of the patient who had previous left URS history. The patient had administered to a foreign hospital and undergone an unsuccessful DJ catheter removal. B. Postoperative KUB X-Ray of the same patient after open cystolithotomy and left pyelolithotomy with DJ catheter removal.
Table 1.
Demographic and preoperative clinical characteristics of the open stone surgery patients
| Mean Age | 48.3 (20–66) |
| Male / Female | 13 / 5 |
| Mean Body Mass Index | 29.7 (20.4–32.8) |
| Bilateral Kidney Stone | 4 |
| Kidney Location or Rotation Anomaly | 4 |
| Concurrent Ureter Stone | 1 |
| Previous URS or PCNL History | 7 |
| Previous SWL History | 2 |
| Previous Open Stone Surgery | 1 |
| Preoperative Mean Stone CSD (cm) | 9.83 (2.5 22.2) |
| Preoperative Mean Stone Volume (cm3) | 49.71 (8.17–57.25) |
All surgeries were carried out in an extraperitoneal fashion using a subcostal flank approach. Nephrotomy procedures were carried out under cold ischemia with incision of Brodel’s line posteriorly. Simultaneous pyeloplasty and pyelolithotomy cases were carried out with combining dismembered pyeloplasty and extended pyelolithotomy techniques. Thorough description of these techniques is beyond the scope of this article but is explained extensively in classical textbooks. An ultrasound and KUB X-ray was performed in all patients before discharge.
Stone analyses were obtained from 15 patients during the postoperative period and compared with previous stone analysis results when available. Eleven out of 18 patients had stone analysis preoperatively which included 4 whewellite stones, 3 whewellite and weddellite stones and 4 cystine stones. Nine out of 18 patients had metabolic analysis preoperatively. None of the patients in our cohort had renal tubular acidosis. Five patients had enteric hyperoxaluria and 4 patients had hypercalciuria and hypocitraturia.
Abdominal NCCT scans and renal ultrasound were performed at postoperative first month and stone status was evaluated by scan results. Patients were followed up in three-month periods during the first year. Creatinine levels, complete blood count and urinary analysis were obtained during follow-ups. Stone status was evaluated by renal ultrasound and we proceeded to further imaging modalities when required after first month follow-up. Preoperative and postoperative stone burdens were calculated by CSD (cm) of the stone on the KUB film and the total volume of the stone (cm3) was calculated from axial images with coronal reconstructions of NCCT scan with length x height x width x π x 1/6 formula [6, 7]. All NCCT scans were performed by a 64-detector CT machine (Aquilion 64, Toshiba, Tokyo, Japan) with 1 mm slice thickness. Radiologic measurements were determined using digital calibers of the software of our hospital (ExtremePACS, Ekstrem Bir, Ankara, Turkey). After NCCT scans, sagittal and coronal reformatted images were obtained with 1 mm slice thickness. Even though the exact prediction power of the formula for asymmetrical stones was criticized, considering the massive stone burden of our patient group, we concluded that the calculated volume using the algebraic formula was sufficient [8].
RESULTS
After surgery, we did not observe any Clavien-Dindo grade 4 or 5 complications. No patient needed perioperative or postoperative blood transfusion with a mean postoperative decrease in hemoglobin value of 1.8 (0.3–4.7) mg/dl. Estimated blood losses were 650 cc and 400 cc in two patients who underwent open nephrotomy. In other patients the estimated blood losses were negligible. Two patients had persistent fever and one patient had a urinary tract infection confirmed by culture. These patients were managed according to the approach of the Hospital Infections Board of our hospital. One patient was managed with thoracentesis due to pleural effusion whose biochemical analysis was compatible with transudate fluid and did not recur. One patient had urine leakage from the operation site and was managed with prolonged transurethral catheterization. Two patients had prolonged ileus and were managed conservatively. Cold ischemia times were 12 and 19 minutes in two nephrolithotomy cases. Stone-free state was achieved in 15 (83.3%) patients, mean total operation time was 84 (57–124) minutes and mean hospitalization time was 5.5 (3–8) days. Among 15 patients who had postoperative stone analysis, 6 of them had cystine stones, 2 of them had uric acid stones, 3 of them had whewellite stones and 4 of them had whewellite and weddellite stones. Medical therapy was initiated due to stone analysis results and metabolic analysis undertaken. At 18 months of follow-up time, we did not observe any secondary ureteropelvic junction obstruction or incisional flank hernia. Under appropriate general measures and medical therapy, stone recurrence rate was 11.1% (2 patients). Surgery types and postoperative complications of our patient group are summarized in Tables 2 and 3.
Table 2.
Surgical treatment types of the patients who undergone surgical treatment for the urinary stone disease
| Endourologic Treatment Left Percutaneous Nephrolithotomy Right Percutaneous Nephrolithotomy Left Ureterorenoscopy with Laser Lithotripsy Right Ureterorenoscopy with Laser Lithotripsy |
175 (10.3%) 147 (8.6%) 693 (40.7%) 668 (39.3%) |
| Open Surgery Left Pyelolithotomy Right Pyelolithotomy Left Pyelolithotomy with Pyeloplasty Right Pyelolithotomy with Pyeloplasty Right Pyelolithotomy with Nephrolithotomy and Ureterolithotomy Right Nephrolithotomy |
11 (0.7%) 3 (0.2%) 1 (0.05%) 1 (0.05%) 1 (0.05%) 1 (0.05%) |
Table 3.
Postoperative complications of the open stone surgery procedures
| Urine extravasation | 1 |
| Urinary Infection | 2 |
| Incision Site Fat Necrosis and Surgical Site Infection | 1 |
| Postoperative Ileus | 2 |
| Transudative Pleurisy | 1 |
DISCUSSION
Urinary stone disease was mentioned and treatment of the condition was also described in ancient texts from Persian, Greek, Egyptian and Indian civilizations [1, 9]. Today, one in every 11 individuals experience stone disease during their life and total economic burden of the disease accounts for more than $10 billion expenditures annually, according to the US data [10, 11]. An increasing prevalence of the disease was reported, especially in the older population, with a plateau of 85.000 cases per year incidence in young people according to the UK data [3]. In the endourology era, most the patients with stone disease are treated with minimally invasive techniques such as SWL, URS, RIRS, PCNL, and other such new procedures. Current urologic practice mainly relies on endourologic techniques and minimally invasive methods are the first choice in every suitable clinical situation. On the other hand, even though it has a more invasive nature and diminished role in daily practice, open surgery may still offer a high clinical success and less total intervention numbers compared with endourologic approaches with acceptable complication rates.
The results of open surgery in contemporary practice have been reported either as case reports [12], single or multi-institution case series [13] or reviews [14]. In their report, Paik and Resnick have reported their 5-year experience with 42 open stone surgery patients and concluded with high stone clearance rates with low morbidity. Their main indications for open stone surgery were complex stone burden, treatment failures with less-invasive modalities in patient’s medical history, anatomical collective system anomalies and comorbid conditions [15]. Same indications are prevalent in other reports, applicable to clinical practice and have their place in clinical guidelines [2]. In their review, El-Husseiny and Buchholz underlined the vivid shifting to endourologic procedures in clinical practice reported in articles after the 1980s. In this review, possible cost-effective applications of open surgery in developing countries were reported [14]. Open surgery was also offered as a cost-effective treatment modality for developing countries with respectively low urinary stone prevalence [16]. In their report including 43 urinary stone patients, Esen et al. compared patients who were managed with SWL monotherapy, SWL and PCNL combination therapy or open stone surgery. They concluded that, considering its more invasive nature, open surgery would be an effective treatment modality [17]. We would like to mention that the surgeons who participated in these reports were trained mostly before the endourology era and probably were more experienced in open stone surgery compared with today’s urologists. Buchholz et al. made an important review on the role of open stone surgery cases in surgical education. After discussing the important role of open surgery in the past and the shifting to endourologic or laparoscopic approaches in present practice, the authors underlined the inconvenience of introducing proficient open surgery training during the residency period. In this review, the authors have offered centralization to achieve a satisfactory case load in order to provide proper surgical training on open stone surgery [13]. Heers and Turney analyzed the Hospital Episode Statistics database of the UK and reported a significant increase in the number of performed ureterorenoscopies with a concurrent decline in open surgery. They have also reported a decrease in hospitalization times and increase in the number of day cases with the common application of endourologic treatments [3].
Previous reports comparing complications between patients who underwent PCNL and open surgery usually concluded in favor of PCNL in terms of complications and postoperative pain [18, 19]. Even though higher complication rates after PCNL in patients who had previous open renal surgery was reported by a meta-analysis, PCNL can also be performed successfully on such patients [20, 21]. In our case series, we have observed a high stone clearance rate, which would be impossible with endourologic interventions during only one session. Our complication rates were acceptable and none of the patients required a second look intervention. Our postoperative stone-free rate is arguably low. However, this is the result of the high stone burden of our patient group. At postoperative assessment, we observed a significant success to remove urinary stones and CSD of residual fragments were lower than 1 cm (Figure 5). This low stone-free rate is mostly affected by small stone fragments, which were entrapped in deep calyxes and were not palpable during surgery (Figure 6). Open surgical approach to patients with complex stones, comorbidities, orthopedic problems and in case of complications or failure of access to collective system in endourologic procedures is also accepted in contemporary practice. We also recommend informing patients about open surgery as an option even though it is not the first method of choice and we believe that this information is a part of patients’ rights. Patients hold the right to know that open surgery is still available in the treatment of their disorders and should be able to choose with informed consent. We can also speculate on the cost-effectiveness of open stone surgery in low-income countries.
Figure 5.
Removed stones from the patient whose preoperative KUB X-Ray is shown in Figure 1A.
Figure 6.
A. Preoperative KUB X-Ray of the patient with a large renal pelvis stone and several small ones in the lower pole calyces. B. Postoperative KUB X-Ray of the same patient after open left stone removal showing minimally residual stone disease.
Another advantage of open surgery is its irreplaceable role in case of complications during endourologic procedures. Two of our patients underwent open surgery as a result of surgical complication. We witnessed uncontrollable bleeding in the first patient and then we carried out a fast-retroperitoneal exploration with consequent bleeding control and stone removal. In the second patient, open surgery was a result of total ureteral stripping during semi-rigid ureterorenoscopy.
The main short-comings of our study are its retrospective fashion, low patient number, selection of patients by purely clinical decisions instead of systematic classifications and possible missing of recurrences during follow-ups. Even though the correlation of renal ultrasound with NCCT at first month follow-up strengthen the diagnostic value, further follow-ups were mostly relied on renal ultrasound which is not as sensitive as NCCT. Thus, some recurrences might have been missed.
From an educational standpoint, open surgery holds some advantages. Firstly, open surgical skills can be transferred from case to case. For instance, one who learned to carry out open pyeloplasty can further undertake proximal ureterolithotomy, pyelolithotomy and even extended pyelolithotomy reaching several calyces. Open nephrotomy, which is mostly abandoned in contemporary practice, can be undertaken with an approach akin to open partial nephrectomy. Therefore, even though open stone surgery is often not observed in current urological residency programs, we can conclude that an open extirpative and reconstructive surgery experience would be enough to undertake open stone surgery procedures when needed.
CONCLUSIONS
In current clinical guidelines and evidence, endourologic approaches are still superior to open surgery in most terms. However, open surgery holds its indispensable position for managing complex cases in selected patients and in case of severe complications. It is also a time-tested option in virtually all patients with urinary stone disease. We also think that it is a part of patients’ rights to know that open surgery is still a valid option. Several advantages of open stone surgery such as high stone clearance rates and low total operation times is well known and prospective, case-matched and randomized studies are needed to compare open stone surgery with endourologic techniques in terms of postoperative complications, pain scores, outcomes and cost-effectiveness in patients with complex stone burden.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Tefekli A, Cezayirli F. The history of urinary stones: in parallel with civilization. ScientificWorld Journal. 2013:423964. doi: 10.1155/2013/423964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Türk C, Petřík A, Sarica K, et al. EAU Guidelines on Diagnosis and Conservative Management of Urolithiasis. Eur Urol. 2016;69:468–474. doi: 10.1016/j.eururo.2015.07.040. [DOI] [PubMed] [Google Scholar]
- 3.Heers H, Turney BW. Trends in urological stone disease: a 5-year update of Hospital Episode statistics. BJU Int. 2016;118:785–789. doi: 10.1111/bju.13520. [DOI] [PubMed] [Google Scholar]
- 4.Honeck P, Wendt-Nordahl G, Krombach P, et al. Does open stone surgery still play a role in the treatment of urolithiasis? Data of a primary urolithiasis center. J Endourol. 2009;23:1209–1212. doi: 10.1089/end.2009.0027. [DOI] [PubMed] [Google Scholar]
- 5.Nadu A, Schatloff O, Morag R, Ramon J, Winkler H. Laparoscopic surgery for renal stones: is it indicated in the modern endourology era? Int Braz J Urol. 2009;35:9–17. doi: 10.1590/s1677-55382009000100003. [DOI] [PubMed] [Google Scholar]
- 6.Ito H, Kawahara T, Terao H, et al. The most reliable preoperative assessment of renal stone burden as a predictor of stone-free status after flexible ureteroscopy with holmium laser lithotripsy: a single-center experience. Urology. 2012;80:524–528. doi: 10.1016/j.urology.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Ackermann D, Griffith DP, Dunthorn M, Newman RC, Finlayson B. Calculation of stone volume and urinary stone staging with computer assistance. J Endourol. 1989;3:355–359. [Google Scholar]
- 8.Finch W, Johnston R, Shaida N, Winterbottom A, Wiseman O. Measuring stone volume - three-dimensional software reconstruction or an ellipsoid algebra formula? BJU Int. 2014;113:610–614. doi: 10.1111/bju.12456. [DOI] [PubMed] [Google Scholar]
- 9.Shah J, Whitfield HN. Urolithiasis through the ages. BJU Int. 2002;89:801–810. doi: 10.1046/j.1464-410x.2002.02769.x. [DOI] [PubMed] [Google Scholar]
- 10.Scales CD, Jr., Smith AC, Hanley JM, Saigal CS. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160–165. doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scales CD, Jr, Tasian GE, Schwaderer AL, Goldfarb DS, Star RA, Kirkali Z. Urinary Stone Disease: Advancing Knowledge, Patient Care, and Population Health. Clin J Am Soc Nephrol. 2016;11:1305–1312. doi: 10.2215/CJN.13251215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moslemi MK, Safari A. A huge left Staghorn kidney, a case report of inevitable open surgery: a case report. Cases J. 2009;2:8234. doi: 10.4076/1757-1626-2-8234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buchholz NN, Hitchings A, Albanis S. The (soon forgotten) art of open stone surgery: to train or not to train? Ann R Coll Surg Engl. 2006;88:214–217. doi: 10.1308/003588406X95075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Husseiny T, Buchholz N. The role of open stone surgery. Arab J Urol. 2012;10:284–288. doi: 10.1016/j.aju.2012.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paik ML, Resnick MI. The role of open stone surgery in the management of urolithiasis. Tech Urol. 1997;3:96–99. [PubMed] [Google Scholar]
- 16.Eze KC, Irekpita E, Salami TA. Cost-effectiveness of extracorporeal shock wave lithotripsy in a poor resource setting: The Okada, Nigeria experience. Niger Med J. 2016;57:44–48. doi: 10.4103/0300-1652.180568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Esen AA, Kirkali Z, Güler C. Open stone surgery: is it still a preferable procedure in the management of staghorn calculi? Int Urol Nephrol. 1994;26:247–253. doi: 10.1007/BF02768205. [DOI] [PubMed] [Google Scholar]
- 18.Yuhico MP, Ko R. The current status of percutaneous nephrolithotomy in the management of kidney stones. Minerva Urol Nefrol. 2008;60:159–175. [PubMed] [Google Scholar]
- 19.Rittenberg MH, Koolpe H, Keeler L, McNamara T, Bagley DH. Pain control: comparison of percutaneous and operative nephrolithotomy. Urology. 1985;25:468–471. doi: 10.1016/0090-4295(85)90452-2. [DOI] [PubMed] [Google Scholar]
- 20.Khorrami M, Hadi M, Sichani MM, et al. Percutaneous nephrolithotomy success rate and complications in patients with previous open stone surgery. Urol J. 2014;11:1557–1562. [PubMed] [Google Scholar]
- 21.Hu H, Lu Y, Cui L, et al. Impact of previous open renal surgery on the outcomes of subsequent Page 6/12 percutaneous nephrolithotomy: a meta-analysis. BMJ Open. 2016;6:e010627. doi: 10.1136/bmjopen-2015-010627. [DOI] [PMC free article] [PubMed] [Google Scholar]