Abstract
Previous evidence suggests optical treatments hold promise for treating migraine and photophobia. We designed an optical notch filter, centered at 480 nm to reduce direct stimulation of intrinsically photosensitive retinal ganglion cells. We used thin-film technology to integrate the filter into spectacle lenses. Our objective was to determine if an optical notch filter, designed to attenuate activity of intrinsically photosensitive retinal ganglion cells, could reduce headache impact in chronic migraine subjects. For this randomized, double-masked study, our primary endpoint was the Headache Impact Test (HIT-6; GlaxoSmithKline, Brentford, Middlesex, UK). We developed two filters: the therapeutic filter blocked visible light at 480 nm; a 620 nm filter was designed as a sham. Participants were asked to wear lenses with one of the filters for 2 weeks; after 2 weeks when no lenses were worn, they wore lenses with the other filter for 2 weeks. Of 48 subjects, 37 completed the study. Wearing either the 480 or 620 nm lenses resulted in clinically and statistically significant HIT-6 reductions. However, there was no significant difference when comparing overall effect of the 480 and 620 nm lenses. Although the 620 nm filter was designed as a sham intervention, research published following the trial indicated that melanopsin, the photopigment in intrinsically photosensitive retinal ganglion cells, is bi-stable. This molecular property may explain the unexpected efficacy of the 620 nm filter. These preliminary findings indicate that lenses outfitted with a thin-film optical notch filter may be useful in treating chronic migraine.
Keywords: Intrinsically photosensitive retinal ganglion cells, Light sensitivity, Melanopsin, Migraine, Photophobia, Thin-film
1. Background
Over 90% of migraine sufferers report photophobia, an abnormal sensitivity to light, during an attack; many report that light can trigger a migraine attack, and some are chronically light sensitive [1,2]. Patients with chronic headache are particularly prone to visual symptoms and eye strain [3], and non-incandescent artificial indoor light can provoke headaches. [4]. To this point FL-41, a special tint, has been the only migraine-specific optical treatment. Originally developed to reduce light sensitivity attributed to fluorescent lighting, the FL-41 tint blocks blue-green light. In 1991 Good et al. found that FL-41 tinted spectacle lenses reduced migraine frequency from 6.2 to 1.6 per month in a cohort of children with migraines [5]. Despite demonstrated benefit in migraine, this tint has not gained widespread use. FL-41 also has been shown to reduce photophobia and blinking in benign essential blepharospasm, another condition associated with light sensitivity [6].
A fMRI study demonstrated that precision optical tints could reduce cortical hyper-excitation in migraine [7]. This study did not attempt to determine if use of these tints could reduce headache frequency or severity. Nevertheless, there appears to be evidence that optical treatments hold promise for treating migraine and photophobia.
The pathway that mediates photophobia begins with intrinsically photosensitive retinal ganglion cells (IPRGC) and trigeminal afferents [8,9]. These retinal cells do not require input from photoreceptors and have been shown to be responsible for circadian rhythm entrainment and the pupillary light reflex. These cells constitute a pathway separate from that of the visual pathway [10]. IPRGC contain the chromophore melanopsin [11]. Melanopsin has an action potential spectrum that peaks at 480 nm, in the blue-green region of the visible spectrum [12]. It is conceivable that the effectiveness of FL-41 may be attributed to its attenuation of those light wavelengths that activate IPRGC.
Despite its effectiveness, FL-41 was developed before the discovery of IPRGC and has drawbacks. FL-41 cannot be made dark enough to obtain maximal blocking at 480 nm without making the tint too dark for indoor use. For this reason, we designed an optical notch filter based on “thin-film” technology that minimizes light transmission at 480 nm. Our objective was to determine if this filter could reduce headache impact in a cohort of study subjects with chronic migraine.
2. Methods
The University of Utah Institutional Review Board approved this study and all study procedures were performed in compliance with prevailing USA Health Insurance Portability and Accountability Act standards and the Declaration of Helsinki. Study subjects provided informed consent before participation.
Study subjects with chronic migraine were recruited from the authors’ clinics. Subjects were included if they had a diagnosis of chronic migraine according to International Headache Society criteria (second edition of the International Classification of Headache Disorders; http://ihs-classification.org/en/). Subjects already using tinted lenses were excluded. Subjects taking medications with ocular side effects (for example, ethambutol, hydroxychloroquine, amiodarone) were excluded. Subjects were excluded if they had best-corrected visual acuity less than 20/40 or retinal diseases. Subjects who met the criteria for medication overuse were excluded.
2.1. Spectacle lenses
Conventional spectacle tints found in prescription and nonprescription eyewear consist of organic dyes. By contrast, thin-film coatings consist of very thin optically transparent layers deposited on the lens surface.
We designed two thin-film optical notch filters. The therapeutic filter was designed to block light around 480 nm, while a 620 nm filter was designed to act as a sham lens. We chose the 480 nm filter to attenuate stimulation of IPRGC. Because the human eye is maximally sensitive at 550 nm and our 480 nm filter is 70 nm shorter than 550 nm, we chose the 620 nm filter as a sham lens because it is 70 nm longer than 550 nm (Fig. 1). Coatings were applied to the front surfaces of prescription and non-prescription lenses, according to each subject’s requirements (Fig. 2).
Fig. 1.
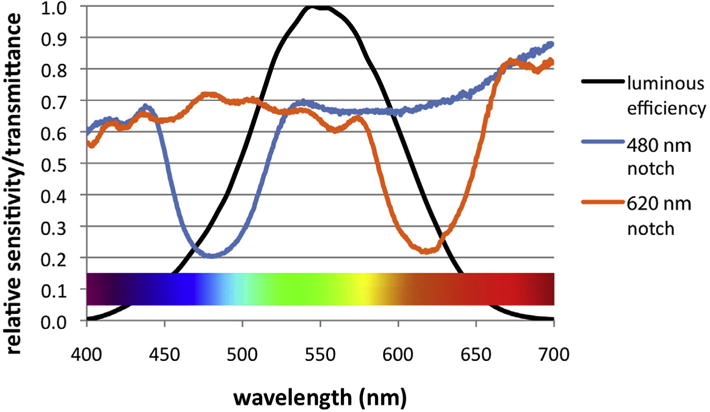
Transmission spectra for the therapeutic 480 nm and 620 nm spectacle lenses compared with the luminous efficiency or sensitivity of the human eye. Luminous efficiency is a measure of the sensitivity of the human eye at various wavelengths. The human eye is most sensitive in the yellow-green spectrum. Both notch filters had a neutral base tint that blocked most wavelengths of light by approximately 30%. Superimposed on this base tint, the 480 nm lenses blocked or “notched” wavelengths in the blue-green portion of the spectrum more deeply than other wavelengths. The 480 nm lenses blocked an average of 44% of visible light (weighted across the luminous efficiency curve) and blocked 68% of light weighted across the absorption spectrum of the melanopsin 11-cis isoform. The 620 nm lenses acted as an optical notch filter in the orange portion of the spectrum and blocked an average of 43% of visible light and 57% of light weighted across the absorption spectrum of the melanopsin all-trans isoform.
Fig. 2.

Study glasses. Each subject initially was randomized to wear either a 480 nm optical notch filter lens (right) or a 620 nm optical notch filter lens (left).
2.2. Study design and procedures
We planned a 12 week, prospective, randomized, doublemasked crossover study (Fig. 3). Only research team members without conflicts of interest interacted with research subjects and collected data.
Fig. 3.
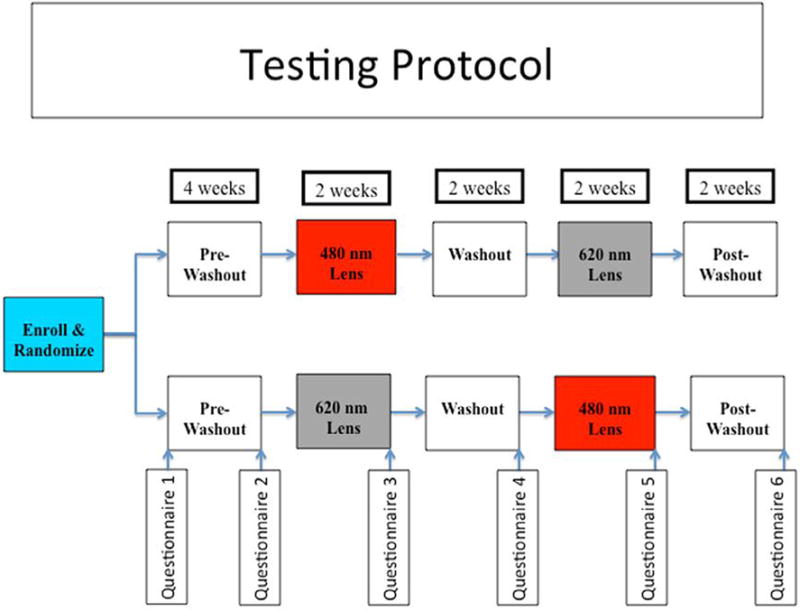
Testing protocol for the 12 week, prospective, randomized, double-masked crossover study. Subjects were randomized to wear the 480 nm or 620 nm thin-film optical notch filter spectacles. Prior to wearing the spectacles, each subject completed a 4 week “pre-washout” to determine baseline headache characteristics. After wearing one of the study lenses for 2 weeks (Period 1), subjects completed a 2 week washout, wearing no lenses, before crossing over to wear the other lenses for 2 weeks (Period 2). Finally, each subject completed a 2 week “post-washout” to look for carryover effects from wearing the study lenses. Note that no study lenses were worn during the pre-washout, the washout, or the post-washout periods. Questionnaires were administered at six time points throughout the study. (This figure is available in colour at www.sciencedirect.com.)
Subjects completed the Headache Impact Test (HIT-6; GlaxoSmithKline, Brentford, Middlesex, UK) (Supp. Fig. 1) and a photophobia questionnaire (Supp. Fig. 2) at six time points throughout the study. Subjects maintained daily headache diaries throughout the study (Supp. Fig. 3). Subjects completed the first set of questionnaires upon enrollment. They did not wear study lenses during the first 4 weeks. After 4 weeks, subjects completed a second set of questionnaires and then were assigned by block randomization to wear either the 480 nm therapeutic lenses or the 620 nm sham lenses. Subjects were instructed to wear the lenses during all waking hours for 2 weeks. Subjects then completed the third set of questionnaires and underwent a 2 week washout period during which they did not wear any study-related lenses. At the end of the washout, subjects completed the fourth set of questionnaires and crossed-over to lenses with the opposite coating for 2 weeks. After 2 weeks, subjects completed the fifth set of questionnaires. The final 2 weeks of the study was another washout period during which no study lenses were worn. At the end of the final washout period, the subjects completed the sixth and final set of questionnaires. Although the HIT-6 is designed to assess headache impact over the previous 4 weeks, at time points 2–5 subjects were instructed to answer the questions based on the previous 2 weeks.
Throughout the trial the investigators and the subjects were masked as to which glasses were being worn. Although the investigators did not monitor whether subjects were wearing the study lenses, subjects were asked to inform the investigative team if they were unable to wear the study lenses for at least 50% of their waking hours. Subjects who completed the entire trial either could keep the study lenses of their choice or receive a check for $US50.
2.3. Data analysis
We determined that 30 subjects would be required to achieve an 80% power for detecting a statistically significant change in the HIT-6. We set our target enrollment at 50, anticipating that some subjects would not complete the study.
A biostatistician developed a data analysis plan before having access to any study data. The primary endpoint was the HIT-6 score. Secondary endpoints included: proportion of days with severe headaches; proportion of days with headaches that made activity difficult, caused activity changes, or caused the subjects to go to bed; proportion of days with headaches requiring use of medication; and proportion of days with light sensitivity. Because the study lenses could potentially affect circadian rhythms, we also tracked the number of hours each subject slept throughout the study. Finally, we reviewed how many subjects chose to keep a study lens versus the $50. The primary statistical analysis was based on the results of Questionnaires 2 through 5 obtained immediately prior to and following the interventions of the two periods of the cross-over design. The analysis was performed using a mixed effects model with a random effect for patient, and fixed effects for treatment order and for the pre- and post-treatment measurements for each of the two periods. The primary estimate of the treatment effect was based on a comparison of the post-treatment values between the 2 periods in accordance with the cross-over design using each patient as their own control. Additional contrasts were used to estimate the mean changes from the pre-treatment to the post-treatment for the 2 interventions separately for the 2 periods, and to estimate carry-over effects.
To detect carryover effects, the biostatistician performed an analysis of covariance relating the HIT-6 recorded before lens #2 to the HIT-6 recorded at the end of lens #1. Because there were some outliers in the analysis of covariance, a non-parametric rank-sum test was performed for the same comparison.
3. Results
We enrolled 48 subjects. Thirty-seven completed all study procedures. Twenty-nine were women and eight were men, with an average age of 44 years (range 19–75). Baseline HIT-6 score of all 48 subjects was 65.4. Baseline HIT-6 score for the 37 subjects who completed the study was 64.5. Thirty-three of the 37 subjects completing the study (89%) had baseline HIT-6 scores ⩾60. According to the HIT-6 interpretation, patients with scores ⩾60 have headaches that have a “very severe impact” on their life [13].
Table 1 summarizes the HIT-6 data scores analysis, which indicates that wearing either the 480 nm or 620 nm lenses resulted in statistically significant HIT-6 score reductions. There was no significant difference when comparing the 480 nm and 620 nm lenses (p = 0.195).
Table 1.
Data analysis of HIT-6 scores. The effects of each of the lenses have been considered separately and together, both after baseline and after the washout period
| Effects | HIT-6 score reduction | p value |
|---|---|---|
| Period 1 | ||
| 480 nm vs. baseline | −4.3010 | 0.001 |
| 620 nm vs. baseline | −5.1053 | 0.0003 |
| Combined effect of 480 nm and 620 nm vs. baseline | −4.7031 | < 0.0001 |
| Period 2 | ||
| 480 nm vs. washout | −3.1053 | 0.025 |
| 620 nm vs. washout | −2.7447 | 0.0487 |
| Combined effect of 480 nm and 620 nm vs. washout | −2.9250 | 0.003 |
| Period 1 combined with Period 2 | ||
| Treatment effect 620 nm vs. 480 nm | −1.2595 | 0.195 |
HIT = Headache Impact Test (GlaxoSmithKline, Brentford, Middlesex, UK), vs. = versus.
Figure 4 displays the HIT-6 scores for the 37 subjects who completed the study. This graph illustrates improvements in HIT-6 recorded while wearing either the 480 nm or 620 nm lenses, as well as return to baseline when no study lenses were worn.
Fig. 4.
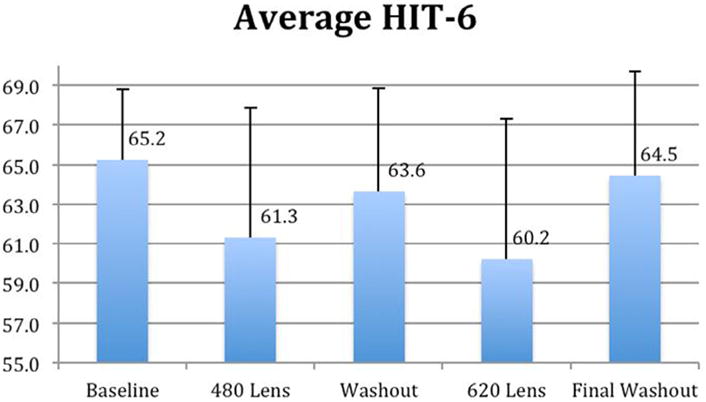
There were statistically significant reductions in Headache Impact Test (HIT-6) scores when either the 480 nm or 620 nm notch filter lenses were worn. HIT-6 scores returned to baseline levels during both washout periods, when no study lenses were worn. Although the 480 nm and 620 nm lenses were worn in random order, the data have been re-arranged here for simplicity. On average, wearing either the 480 nm or 620 nm lenses resulted in a 3.7 point reduction in HIT-6 score.
3.1. Washout period carry-over effects
We compared HIT-6 data obtained after subjects wore the first pair of spectacles with HIT-6 data obtained before the second pair of spectacles was worn to determine if there was any evidence for a “carry-over effect”. This analysis revealed a trend towards a carry-over effect (p = 0.09). The non-parametric rank-sum test, performed to control for apparent moderate outliers, revealed no evidence of carry-over effect (p = 0.97). Overall, we interpreted these results as inconclusive, indicating at most a slight suggestion of a carry-over effect during the washout phase.
Nine subjects moved out of the “very severe impact” HIT-6 category while wearing the 480 nm lenses, five moved out of this category with the 620 nm lenses, and five moved out of this category when they wore either lens. Smelt has suggested that for clinical research, a 5 or 6 point change in the HIT-6 is clinically relevant [14]. Ten subjects experienced at least a 6 point HIT-6 improvement when wearing the 480 nm lenses, 10 subjects experienced at least a 6 point improvement with 620 nm lenses, and three subjects experienced at least a 6 point improvement when wearing either lens.
Results for secondary outcomes were similar to the primary outcome for either the 480 nm or 620 nm spectacle lenses: subjects experienced significant reductions in all parameters when they wore either lens. There was no significant difference when comparing the effect of the two lenses for percentage of days with severe headache, days where activity had to be changed or the subject had to go to bed due to headache, or days requiring headache medication (Supp. Fig. 4–6). The percentage of days with light sensitivity declined significantly when wearing the 620 nm lenses, but not when wearing the 480 nm lenses (Supp. Fig. 7). There were no significant effects on hours slept while wearing either study lens (data not shown).
Fourteen subjects elected to keep the 480 nm lenses and 13 kept the 620 nm lenses. One subject requested that they be allowed to keep both pairs of lenses. Nine subjects chose to receive the $50 check.
3.2. Withdrawals
Eleven subjects did not complete the study. Four subjects failed to appear for subsequent study visits, and two could not complete the study in a timely fashion. One withdrew to “explore other study options”, one because of a change in employment, and one due to a residence change. One withdrew because of a perception that the lenses worsened headaches and one because the spectacle frame could not be adjusted comfortably.
4. Discussion
Our baseline data indicated that the majority of subjects experienced headaches that were having a “very severe impact” on their life. On average, the subjects achieved a statistically significant reduction in HIT-6 scores while wearing either the 480 nm or 620 nm lenses. Nineteen of the 37 subjects who completed the study moved out of the “very severe impact” category when wearing one or both lenses. Twenty-three subjects reported at least a 6 point improvement in HIT-6 scores while wearing one or both of the lenses.
Secondary outcomes also improved while wearing one or both lenses. Most subjects elected to keep their study lenses instead of receiving financial compensation for participation. These observations also indicate that many subjects found the lenses to be helpful in their migraine management.
All of the subjects in this study had significant photophobia and would therefore want to avoid noxious stimuli such as bright light. One may wonder if their salutary response to the study lenses was simply because the lenses made them more comfortable or if the lenses actually affected the underlying pathophysiology of their migraines. The work of Noseda et al. and the review by Digre and Brennan suggest that there is a robust connection between the activation of IPRGC and activation of the trigeminal nerve [8,9]. Migraine pain is thought to arise primarily from activation of the trigeminal nerve and its afferents in the dura, cranium, face, and eye [15]. For these reasons, we believe it is plausible that the study lenses affect the biology of headache.
The 620 nm lenses were designed to be “sham” lenses. When the study began, there was no reason to suspect that a filter at this wavelength would have a therapeutic effect. Our data could be consistent with the hypothesis that both the 480 and 620 nm notch filters had a true, therapeutic effect. We did not pre-specify this hypothesis in either our protocol or our analysis plan, and the crossover design prevented us from rendering a conclusive assessment of this hypothesis.
The challenge in making this conclusion is that because this pattern occurred simultaneously in both groups, this result could be interpreted as a “period effect”, which would be unrelated to the biological effect of the lenses. There are four potential sources of bias in period effects. These sources include placebo effects, regression to the mean, learning effects, and recovery from migraine. Because we observed declines in HIT-6 scores in two separate periods, with an increase in these scores in between, regression to the mean, learning effects and recovery can be discounted. However, our post hoc analysis does not permit us to entirely rule out the possibility of a placebo effect. As explained below, biologic mechanisms exist that could explain the therapeutic effects of the 620 nm lens.
In 2014, after completion of our study, Chellappa demonstrated that research subjects improved their performance of a cognitive task when they were exposed to long-wavelength light (589 nm) [16]. These authors hypothesized that the salutary effect of long-wavelength light is due to the bi-stable nature of the melanopsin photopigment found in IPRGC. The bi-stable nature of melanopsin may also explain the salutary effect of the 620 nm lenses in our subjects.
Bi-stable pigments such as melanopsin have two stable isoforms that are spectrally distinct (Supp. Fig. 8). One isoform is active and can elicit a physiologic response; the other is inactive. Different wavelengths of light (λ1 and λ2) trigger a conformational change between the two isoforms. In the case of melanopsin, it is 480 nm light that isomerizes melanopsin from its active to its inactive state and triggers the phototransduction cascade in the IPRGC. In addition to a possible natural slow thermal relaxation back to the cis state, exposure to 590 nm light drives melanopsin from its inactive, all-trans isoform to its active, 11-cis isoform [17].
The bi-stable nature of melanopsin may explain the salutary effect of the 620 nm notch filter; by limiting exposure of IPRGC to longer wavelength light, inactive melanopsin molecules cannot readily return to their active, 11-cis isoform. Although our notch filter was not at the peak sensitivity of 11-trans isoform of melanopsin (which is approximately 590 nm), the spectral sensitivity curve was sufficiently broad (Supp. Fig. 9) to experience reduced exposure through the 620 nm notch filter.
At this time it is not clear why some subjects preferred the 480 nm lenses, some preferred the 620 lenses, and some perceived benefit from wearing both lenses. Other researchers have observed that migraine patients appear to be sensitive to both red and blue wavelengths, although these observations were made before our current understanding of the physiology that underpins photophobia [2,18]. It also remains unknown if a notch filter centered closer to 590 nm would be more effective than the 620 nm notch. Further study will be required to address these and other questions posed by our results. We are currently conducting a similar, open-label study in subjects aged 8–18 years (ClinicalTrials.gov NCT01942486).
Most migraine preventatives are typically used for a period of 6-12 weeks before efficacy can be assessed. We were recruiting from a single site and using a crossover design because of limited funding. We therefore chose to limit study length in hopes of receiving improved subject compliance with the protocol, more accurate diaries, and fewer dropouts. For this and other reasons, our findings should be considered preliminary. A future investigation is being planned in which subjects will undergo treatment for a period of 12 weeks.
5. Conclusions
Although light sensitivity is an almost universal experience in migraine, little attention has been paid to addressing this facet of the disease. For many patients, their only treatment option for photophobia has been light avoidance. Although there is anecdotal evidence for the efficacy of FL-41 tint in the treatment of migraine [5] and there is functional MRI evidence for the effect of precision optical tints [7], to our knowledge neither of these treatments has undergone clinical testing for adult migraine. With improvement of our understanding of the physiology that underlies photophobia, we have developed thin-film spectacle coatings for the treatment of migraine and photophobia. Our results indicate that wearing spectacle lenses outfitted with a thin-film optical notch filter may be a useful adjunct in the treatment of chronic migraine.
Supplementary Material
Acknowledgments
The authors thank Tecport Optics (Orlando, FL, USA) for technical assistance and for supplying the thin-film coatings used on all spectacle lenses. The authors thank Patrick Shaw and the staff of the John A. Moran Eye Center Optical Shop for cutting and mounting the lenses and for adjusting the spectacle frames for our subjects. Clinical research coordinator Ms. Barbara Hart assisted with subject recruitment, retention, examination and organization. Dr. Tom Greene and Chong Zhang from the University of Utah Study Design and Biostatistics Center assisted with statistical analyses. Ms. Susan Schulman provided medical writing services.
Disclosures
This investigation was supported in part by: Axon Optics, LLC, Salt Lake City, UT, USA; Tecport Optics, Orlando, FL, USA; NIH T35HL007744 (RNH, AS); The University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 8UL1TR000105 (formerly UL1RR025764); and by an unrestricted grant from Research to Prevent Blindness, New York, New York, USA, to the Department of Ophthalmology and Visual Sciences, University of Utah, Salt Lake City, Utah. JG was supported by the University of Utah, Office of Undergraduate Research, Undergraduate Research Opportunities Program (UROP). RNH and AS were supported by the Medical Student Research Program at the University of Utah School of Medicine, funded by NIH/NHLBI Training Grant # T35 HL007744 (PI: Jerry Kaplan, PhD) and University of Utah institutional support.
Role of the funding sources: Drs. Katz and Blair are managers of Axon Optics, one of the funding sources for the manuscript. Because of their conflicts of interest, they recused themselves from recruitment, data collection, data analysis, and interpretation of the data. They did participate in the study design, writing of the manuscript and the decision to submit for publication. The other funding sources had no role in the design, in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Appendix A. Supplementary material
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jocn.2015.09.024.
Footnotes
Conflicts of Interest
Conflict of Interest statement: Drs. Katz and Blair have equity interests in and hold management positions in Axon Optics, a limited liability corporation that markets eyewear for the treatment of migraine and photophobia. Drs. Katz, Blair, Digre and Warner are inventors on a patent pending for the thin-film coatings described in this manuscript and stand to receive royalties on any commercial sales of products based on these coatings. The other authors have no conflicts of interest. Because of their conflicts of interest, Drs. Katz, Blair, Digre and Warner recused themselves from subject recruitment, data collection, data analysis, and data interpretation.
References
- 1.Evans RW, Seifert T, Kailasam J, et al. The use of questions to determine the presence of photophobia and phonophobia during migraine. Headache. 2008;48:395–7. doi: 10.1111/j.1526-4610.2007.00920.x. http://dx.doi.org/10.1111/j.1526-4610.2007.00920.x. [DOI] [PubMed] [Google Scholar]
- 2.Main A, Dowson A, Gross M. Photophobia and phonophobia in migraineurs between attacks. Headache. 1997;37:492–5. doi: 10.1046/j.1526-4610.1997.3708492.x. [DOI] [PubMed] [Google Scholar]
- 3.Vincent AJ, Spierings EL, Messinger HB. A controlled study of visual symptoms and eye strain factors in chronic headache. Headache. 1989;29:523–7. doi: 10.1111/j.1526-4610.1989.hed2908523.x. [DOI] [PubMed] [Google Scholar]
- 4.Wilkins AJ, Nimmo-Smith I, Slater AI, et al. Fluorescent lighting, headaches and eyestrain. Light Res Technol. 1989;21:11–8. [Google Scholar]
- 5.Good PA, Taylor RH, Mortimer MJ. The use of tinted glasses in childhood migraine. Headache. 1991;31:533–6. doi: 10.1111/j.1526-4610.1991.hed3108533.x. [DOI] [PubMed] [Google Scholar]
- 6.Blackburn MK, Lamb RD, Digre KB, et al. FL-41 tint improves blink frequency, light sensitivity, and functional limitations in patients with benign essential blepharospasm. Ophthalmology. 2009;116:997–1001. doi: 10.1016/j.ophtha.2008.12.031. http://dx.doi.org/10.1016/j.ophtha.2008.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang J, Zong X, Wilkins A, et al. FMRI evidence that precision ophthalmic tints reduce cortical hyperactivation in migraine. Cephalalgia. 2011;31:925–36. doi: 10.1177/0333102411409076. http://dx.doi.org/10.1177/0333102411409076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Digre KB, Brennan KC. Shedding light on photophobia. J Neuroophthalmol. 2012;32:68–81. doi: 10.1097/WNO.0b013e3182474548. http://dx.doi.org/10.1097/WN0.0b013e3182474548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noseda R, Kainz V, Jakubowski M, et al. A neural mechanism for exacerbation of headache by light. Nat Neurosci. 2010;13:239–45. doi: 10.1038/nn.2475. http://dx.doi.org/10.1038/nn.2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gooley JJ, Lu J, Fischer D, et al. A broad role for melanopsin in nonvisual photoreception. J Neurosci. 2003;23:7093–106. doi: 10.1523/JNEUROSCI.23-18-07093.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hattar S, Lucas RJ, Mrosovsky N, et al. Melanopsin and rod-cone photoreceptive systems account for all major accessory visual functions in mice. Nature. 2003;424:76–81. doi: 10.1038/nature01761. http://dx.doi.org/10.1038/nature01761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown TM, Allen AE, al-Enezi J, et al. The melanopic sensitivity function accounts for melanopsin-driven responses in mice under diverse lighting conditions. PLoS One. 2013;8:e53583. doi: 10.1371/journal.pone.0053583. http://dx.doi.org/10.1371/joumal.pone.0053583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dowson AJ. Assessing the impact of migraine. Curr Med Res Opin. 2001;17:298–309. [PubMed] [Google Scholar]
- 14.Smelt AF, Assendelft WJ, Terwee CB, et al. What is a clinically relevant change on the HIT-6 questionnaire? An estimation in a primary-care population of migraine patients. Cephalalgia. 2014;34:29–36. doi: 10.1177/0333102413497599. http://dx.doi.org/10.1177/0333102413497599. [DOI] [PubMed] [Google Scholar]
- 15.Goadsby PJ, Lipton RB, Ferrari MD. Migraine-current understanding and treatment. N Engl J Med. 2002;346:257–70. doi: 10.1056/NEJMra010917. [DOI] [PubMed] [Google Scholar]
- 16.Chellappa SL, Ly JQ, Meyer C, et al. Photic memory for executive brain responses. Proc Natl Acad Sci U S A. 2014;111:6087–91. doi: 10.1073/pnas.1320005111. http://dx.doi.org/10.1073/pnas.1320005111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mure LS, Cornut PL, Rieux C, et al. Melanopsin bistability: a fly’s eye technology in the human retina. PLoS One. 2009;4:e5991. doi: 10.1371/journal.pone.0005991. http://dx.doi.org/10.1371/journal.pone.0005991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilkins AJ, Patel R, Adjamian P, et al. Tinted spectacles and visually sensitive migraine. Cephalalgia. 2002;22:711–9. doi: 10.1046/j.1468-2982.2002.00362.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


