Abstract
Background
Computer-based interventions have been developed to improve cognitive performance after mild traumatic brain injury, however, a thorough evaluation of this body of research has not been addressed in the literature.
Objectives
To provide a synthesis and critical review of current research studies that have tested the efficacy of computer-based interventions on cognitive performance after mild traumatic brain injury.
Methods
A critical review was conducted by identifying relevant studies in the electronic databases PubMed/Medline, PsycInfo and CINAHL from 2011 to the present. Due to the limited number of publications focused exclusively on mild traumatic brain injury, research studies that assessed the impact of computer-based interventions on cognitive outcomes in populations with acquired brain injury were included.
Results
Of the 58 studies identified, only 10 publications included participants with mild traumatic brain injury. Overall, the identified studies did not use a standard method for assessing the severity of traumatic brain injury, many studies included participants with a wide variety of etiologies for acquired brain injury and used multiple measures of cognitive performance, which made comparisons difficult across studies. In addition to small sample sizes, the study samples were heterogeneous in regard to the number of prior traumatic brain injuries, time elapsed since injury, as well as age and gender distributions. Pre-injury comorbidities that may affect cognitive performance, such as depression, anxiety or learning disabilities, were often not assessed.
Discussion
There is weak evidence that computer-based interventions can improve working memory and cognitive function in individuals following mild traumatic brain injury. Due to the low-quality evidence, seminal questions remain regarding the optimal format, dosage, timing and duration of computer-based intervention for improving cognitive performance. Future studies should focus on using a strong research design, such as a prospective longitudinal, repeated measures study, with an adequate number of participants that meet mild traumatic brain injury criteria. Pre-injury comorbidities, cognitive reserve, time since injury, age and gender, should be addressed in the design as there may be differences in recovery time and mechanisms of cognitive plasticity among populations.
Conclusions
Overall, computer-based interventions appear promising as an approach to improve working memory in individuals with acquired brain injury. There is no evidence that currently available interventions are specific to mild traumatic brain injury. Well-designed research studies with adequate sample sizes are needed to assess the effect of computer-based interventions on cognitive performance after mild traumatic brain injury.
Keywords: concussion, mild-traumatic brain injury, post-concussion syndrome, cognitive impairment, cognitive interventions, cognitive rehabilitation
Introduction
Traumatic brain injury (TBI) is defined as a “physiological disruption of brain function resulting from traumatic force transmitted to the head.” 1 The injury is categorized as mild, moderate, or severe, based on clinical and imaging findings. By far, mild traumatic brain injury (mTBI) is the most common, occurring in 42 million people each year.2 Over one million emergency room visits occur each year in the United States due to mTBI and between 1.6-3.8 million sport-related mTBIs are diagnosed annually.3 Approximately 40% of individuals with mTBI have long-term disability and the Centers for Disease Control estimates that 5.3 million Americans are living with TBI-related disability.3 The high prevalence and rate of long-term disability make mTBI a significant public health issue.1
A constellation of symptoms may be reported by patients following mTBI including confusion, headache, dizziness, fatigue, reduced concentration, memory impairment, sleep disturbance, irritability, blurred vision, sensitivity to noise and light, anxiety and depression.4 In approximately one third of patients with mTBI these symptoms can persist beyond 6-12 months.5 There are several risk factors for persistent symptoms, including older age, female sex, previous head injury, severe initial injury and pre-existing psychological problems.1 One of the most distressing symptoms to patients with mTBI is cognitive impairment, which may include forgetfulness, difficulty thinking and memory problems.4
Nurses who manage patients with mTBI are focused on identifying patients who may be at risk of complications, promoting symptom management and return to pre-injury levels of functioning. All patients with mTBI should receive education about common post-injury symptoms with instructions to seek healthcare evaluation if the symptoms persist beyond one month.6 Although Cicerone and colleagues7 provided evidence-based recommendations for cognitive rehabilitation after TBI, there are no specific indications for patients with mTBI-related cognitive impairment. However, a previous study assessing a computer-based cognitive intervention reported some effectiveness in improving cognitive performance after mTBI.8 Assisting the patient and family to identify resources for symptom management is critical and can be a key issue for decreasing disability, particularly related to persistent cognitive impairment.4 At present, there are several computer-based cognitive rehabilitation resources that are easily accessible and may provide a resource for patients and families who are dealing with cognitive issues following mTBI. To evaluate current research studies that have tested the efficacy of computer-based interventions on cognitive performance after mild traumatic brain injury and provide a synthesis of the findings, a critical review was performed based on the following guiding questions: 1) What types of computer-based cognitive interventions have been evaluated in participants with mTBI?; 2) What measures were used to evaluate cognitive performance in participants with mTBI?; and 3) Are there individual characteristics identified that may influence the effectiveness of the intervention?
Methods
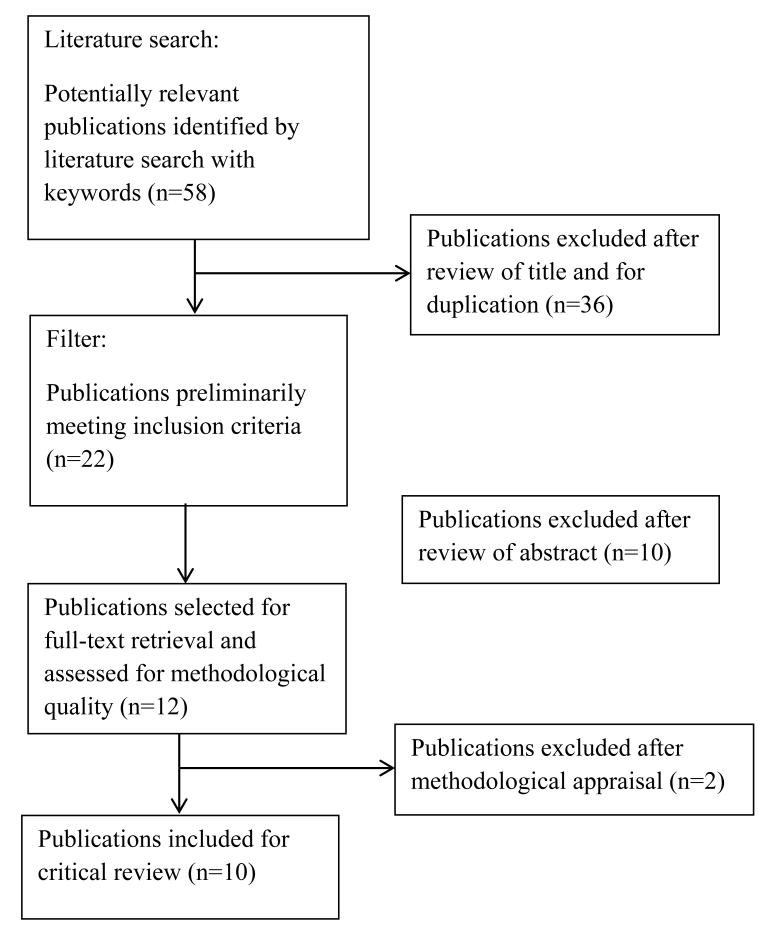
A critical review was conducted to examine the literature focused on studies testing computer-based cognitive rehabilitation programs for mTBI. A literature search was conducted using the electronic databases PubMed/Medline, PsycInfo and CINAHL from 2011 to the present, with the following key words: “mild traumatic brain injury,” “concussion”, “cognitive impairment,” “memory deficit,” “cognitive rehabilitation,” and “computer-based interventions.” From September, 2016 to December, 2016, manual searches were also completed using references from previously published studies and literature reviews. The time period between 2011 and the present was selected because of the major advances that have taken place since that time in designing computer-based cognitive rehabilitation programs for mTBI. Articles that were retrieved via these multiple search methods (PubMed=19; PsychInfo =21; CINAHL=8) were reviewed for duplication and for whether they met the following inclusion criteria: (1) research studies that involved human participants with a primary aim of assessing computer-based cognitive rehabilitation; (2) the study used cognitive outcome measures (such as working memory or executive function); and, (3) it was written in English (see Figure 1 for process of the literature selection). Of the 58 publications retrieved during the literature search, 36 did not meet inclusion criteria upon review of the abstract, thus a total of 22 articles were further reviewed. Upon full assessment of the publications, another 10 publications were excluded because they did not focus on computer-based cognitive interventions. Quality assessment of the full publications excluded another 2 articles because they were secondary analysis, leaving 10 publications. Thus, a total of 10 articles met the inclusion criteria and were included in the review (Supplemental Digital Content 1).
Figure 1.
Literature Review Process
Quality assessment was performed using the following GRADE criteria. Class I evidence included prospective randomized controlled trials. Randomized controlled trials with quasi-randomization of participants were considered class Ia studies. Class II evidence included prospective nonrandomized cohort studies, retrospective nonrandomized case control studies, and clinical series with controls that are well-designed. Class III evidence included clinical series without concurrent controls and case studies.
What types of computer-based cognitive interventions have been evaluated in participants with mTBI?
Akerlund and colleagues9 conducted a randomized controlled study in an outpatient rehabilitation center for acquired brain injury. In the study, participants completing rehabilitation were randomized to the experimental group which received 5 weeks of rehabilitation plus training with Cogmed QM for 30-45 minutes per day, 5 days per week, or the control group that only received standard cognitive rehabilitation. This was a mixed sample of participants with acquired brain injury who were in the subacute phase. While both groups improved working memory and cognition, the intervention group had significant improvements in working memory (p<.045) and cognition (p<.044) compared with the control group. This was a relatively small sample size and the cause of brain injury was not described in the sample description. However, a follow-up study by Bjorkdahl et al.10, which reported on the same sample, stated that there were 5 participants with TBI. The Bjorkdahl study was to evaluate whether the gain in working memory improved daily task performance, which it did not.
DeLuca et al.11 carried out a randomized study to evaluate a computer-based cognitive training program among 34 patients with TBI who were within 3-6 months post-injury. The participants who were randomized to the experimental group received cognitive training that was specific to their neurocognitive assessment findings plus standard neurorehabilitation. The authors reported significant improvements in all dimensions of cognition (p ranging from .03 - .001), function (p<.005) and depression (p<.009). This was a mixed sample of participants with mild and moderate TBI, the sample size was small and participants also received neurorehabilitation, making it difficult to ascertain the true benefit of the computer-based cognitive training. In addition, there was no description of blinding the study personnel who performed data collection.
Fernandez and colleagues12 carried out a descriptive longitudinal study to evaluate the effectiveness of RehaCom cognitive training among participants with acquired brain injury, 29 of whom had a TBI. The study found that all dimensions of neuropsychological status and memory improved (p<.05). Again, the sample size was small and description of the study sample did not include the severity of TBI. In addition, this study did not include a control group and was vulnerable on several levels of selection and measurement bias.
Johansson and Tornmalm13 examined the effects of an 8 week training session with CogMed QM among participants with acquired brain injury. This was also a mixed sample with only 5 participants with TBI and no description was provided on the severity of injury. All of the participants had received formal rehabilitation and there was no control group. After the 8 week training, participants had an improvement in working memory (p<.018), performance (p<.008) and performance satisfaction (p<.01) compared to baseline. Training results were not affected by age, time post-injury or diagnosis and the participants with the lowest working memory capacity had the most significant change in working memory. This was a small sample size and the study was vulnerable to many internal threats including selection and measurement bias.
Lebowitz and colleagues14 evaluated the feasibility and utility of using a software program of computer-based mental exercises, Cortex with InSight (Posit Science Corporation, San Francisco, California), for community-dwelling individuals with a history of TBI. Participants were given the software to use at home and instructed to use the software for 40 minutes per day. The study findings include a small effect size on neuropsychological assessment scores and behaviors. There was a wide time-span (6 months to 22 years) of time post-injury, and a control group was not included.
Li et al. 15-16 carried out two pilot studies on the effectiveness of Parrott software. The first study examined the effectiveness on attention and memory in a mixed sample of participants with acquired brain injury including TBI with memory and attention deficits.15 They found a statistically significant increase in attention (p<.005) and memory (p<.05). In the second study, they tested the relationship between global cognition and a performance-based task using the medication-box sorting test.16 In this study, there were 5 participants with TBI. Although global cognition scores were significantly increased (p=.03), the changes in attention and memory were not statistically significant, and there was no change in the medication-box sorting test.
Simmons et al. 17 tested a computer-based virtual reality intervention among participants with acquired brain injury recruited from an adult care center on upper extremity motor function and executive function. The intervention study was conducted using a three-level repeated measures design. The intervention was delivered by a licensed occupational therapist. There was significant improvement in the Executive Function Performance Test task completion (p=.02), particularly in the areas of cooking (p=.02) and medication management (p=.01). Participants were on average 11.4 years post-injury.
Yip and colleagues18 evaluated a 12-session virtual reality cognitive rehabilitation program among patients with acquired brain injury. This was a single-blind, pretest-posttest randomized controlled trial, with the assessors blinded to allocation of group assignment of individual participants. The virtual reality group showed a significant improvement in immediate recall (p<.05), performance of ongoing tasks (p<.01) as well as improvements in several measures of cognition and memory. This was a small sample size of a mixed sample of participants with acquired brain injury and no description was provided on the severity of injury.
Zickefoose et al.19 examined the timing of two computerized brain game software programs among participants with severe TBI with a mean time post-injury of 4 years. Two participants received either 4 weeks of Attention Process Training (APT-3) first or Lumosity games first and were observed for 30 minutes per day, 5 days per week. The participants then switched to the other intervention for another 4 weeks. All participants significantly improved on their level of difficulty on intervention tasks and there was a trend toward generalization to daily tasks. No matter which intervention the participants received, the most significant improvements were observed during the first month. This was an extremely small sample size and there were no controls or blinding procedures to assessment.
What measures were used to evaluate cognitive performance in participants with mTBI?
The Mini Mental Status Exam (MMSE) was used in three studies.11,12,18 The Cognitive Failures Questionnaire was used in two studies.13,14 The Wechsler Adult Intelligence Scale III and Barrow Neurological Institute Screen for Higher Cerebral Functions (BNIS) were used in one study.9 Also present in one study each were the Trail Making Test (TMT-A and B)12, Cognistat Assessment15, Montreal Cognitive Assessment (MoCA 7.1) and Medication-box sorting test16, Executive Function Performance Test17, and Test of Everyday Attention and Adapted version of the Neurological Assessment Battery19. Several studies used multiple measures of cognitive performance. In addition to the MMSE, DeLuca et al.11 used the Category Verbal Fluency (CVF), Letter Verbal Fluency (LVF), Reversal Motor Learning (RML), Attentive Matrices (AM), and Rey Auditory Verbal Learning Test. Yip et al.18 also used the Test of Nonverbal Intelligence, Self-Awareness of Deficit Interview, Cambridge Prospective Memory Test, Hong Kong List Learning Test, Frontal Assessment Battery, Word Fluency Test, and Color Trails Test.
Are there individual characteristics identified that may influence the effectiveness of the intervention?
Of the studies identified, most included samples of participants with acquired brain injury including TBI, therefore it was difficult to ascertain the effect of the intervention on mTBI outcomes. Specifically, there were no details provided on the type and severity of acquired brain injury in some publications.9,11,17-20 Other publications provided the number of participants with TBI but not the severity.12-16 One study included participants with prior TBI of at least one year and with ages ranging from 34-84 years.16 This wide time span since the injury as well as the age range could significant impact the results as participants are likely to develop adaptive behaviors over time and aging can have a direct impact on cognition. In addition, level of education and cognitive reserve have been found to influence cognitive outcomes following rehabilitation, which may affect results.8
Discussion
This critical review was conducted to evaluate the current evidence on computer-based cognitive rehabilitation programs for mTBI and examine the instruments used to evaluate cognitive performance as well as relevant cofactors that should be considered in future studies. Of the studies identified, two evaluated the CogMed QM software;9,13 two studies evaluated study-specific computer-based cognitive training software;11,14 and two studies evaluated Parrott software.15,16 Of the remaining, one study evaluated Rehacom;12 one study evaluated ProMotor Exercise Games;17 one study evaluated a virtual reality cognitive rehabilitation program;18 and one study used both Attention Process Training (APT-3) and Lumosity games.19 Two studies randomized participants to receive rehabilitation plus the intervention or rehabilitation alone.9,11 The remaining studies were pre-post test design.10,12-19
Overall, the was wide variation in the samples selected. Most studies included mixed samples of participant with acquired brain injury and did not focus solely on participants with mTBI. In addition, there was wide variation in the duration of time since injury and the age span among the participants. Due to the highly heterogeneous samples used in the identified studies, it is difficult to draw conclusions from the current evidence regarding the results specific to mTBI. In order to assess the effect of computer-based cognitive rehabilitation for mTBI, future studies should focus solely on samples with mTBI.
From this critical review of samples that included participants with acquired brain injuries, it appears that computer-based cognitive rehabilitation approaches have a modest benefit on improving working memory and other cognitive domains.9,11-14,18 However, the studies used different measures of cognition across studies, making precise comparisons impossible. For this reason, it would be beneficial to include common data elements, such as the NIH Toolbox or other instruments that are sensitive to change in cognitive performance after mTBI, in future studies.
Although several studies incorporated standard neurorehabilitation as part of the study, there was no description on the physical activity performed across studies. This may present a confounding variable as the level of physical activity has been shown to enhance cognitive rehabilitation. The effects of aerobic exercise training were evaluated in a small study by Chin et al.20 that included only three patients with mTBI. However, the results of the 12-week supervised vigorous exercise training (3 times per week for 30 minutes) were promising. Specifically, the authors reported significant improvements in the speed of information processing (p<.007), executive functioning (p=.011) and overall cognitive performance (p=.009). Future studies should control for physical activity in the studies conducted and at a minimum report on the variability and possibly control for physical activity level in the analysis.
Another element that was not reported across studies was the involvement of participants in other cognitive rehabilitation measures, such as reintegration. Components of reintegration, such as employment assistance programs, may also cause variability in reported findings. Twamley et al.21 evaluated a 12-week manualized compensatory cognitive training program (CogSMART) among 50 Veterans with mild to moderate TBI with an average age of 32 years and average time post-injury of 4 years. An employment specialist delivered the CogSMART intervention for 1 hour per week along with a standard 1-hour supported employment visit for 12 weeks. The study found that neurobehavioral symptoms and quality of life improved in the CogSMART group compared to the control group (p=.026; p=.009 respectively). Prospective memory was significantly improved in the CogSMART group (p=.031) compared with the control group and was strongest at 12 months. Other forms of cognitive rehabilitation or reintegration should also be measured in future studies.
Ultimately, nurses working with patients and families affected by mTBI need to be equipped with evidence-based knowledge on methods of improving cognitive performance after injury. High-quality research studies are needed to help inform whether computer-based cognitive interventions can effectively address cognitive impairment following mTBI. Specifically, more controlled studies need to be conducted among mTBI participants with attention to intervention format, dosage, and duration while using appropriate control groups. Study designs that evaluate the timing of the intervention, during the acute phase versus subacute or chronic phases, are critically needed to determine optimal implementation in clinical practice. Biobehavioral nursing research that examines the underlying mechanisms of variation in cognitive performance following mTBI may be the most informative in generating evidence to explain the efficacy of computer-based cognitive interventions at the individual-level.
Limitations of this review include the small number of studies that included participants with mTBI, the small sample sizes, lack of detail on injury severity and time since injury as well as insufficient detail on study protocols. Future studies that assess computer-based cognitive interventions in participants with mTBI need to pay special attention to the study design and methods in order to promote rigor and reproducibility. Adequately powered studies that target individuals with mTBI will advance this field and provide meaningful recommendations to affected patients and their family members.
Conclusions
Neuroscience nurses are often asked to inform patients and families about available resources to improve cognitive performance following mTBI. The purpose of this review was to critically evaluate the evidence on the efficacy of computer-based cognitive rehabilitation for mTBI. At this time, no recommendations can be made regarding the benefit of using computer-based cognitive interventions for mTBI cognitive impairment. The identified studies that assessed computer-based cognitive rehabilitation used mixed samples of participants with acquired brain injury and the interventions encompassed standard rehabilitation plus the computer-based intervention or a pre/post-test design only. Due to the wide variability in injury severity, time since brain injury and age ranges, it is difficult to draw any conclusions. Future studies should focus on participants with mTBI, consider selecting a certain age range and time since injury, and measure cognitive performance using common data elements. In addition, future studies should measure and control for physical activity and other forms of cognitive rehabilitation, such as reintegration therapy or training in the study. Although computer-based cognitive rehabilitation appear promising, there is no conclusive evidence that this approach will significantly improve cognitive performance in individuals with mTBI. More research will be necessary from well-designed studies that include appropriate control groups.
Supplementary Material
Acknowledgments
None
References
- 1.McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorak J, Echemendia RJ, Engebretsen L, Johnston K, Kutcher JS, Raftery M, et al. Consensus statement on concussion in sport: The 4th International Conference on Concussion in Sport held in Zurich, November 2012. British J Sports Med. 2013;47:250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 2.Gardner RC, Yaffe K. Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol Cell Neurosci. 2015;66:75–80. doi: 10.1016/j.mcn.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control. CDC's report to congress on traumatic brain injury epidemiology and rehabilitation. Washington, D. C: CDC; 2016. [Google Scholar]
- 4.Bergman K, Given B, Fabiano R, Schutte D, von Eye A, Davidson S. Symptoms associated with mild traumatic brain injury/concussion: The role of bother. J Neurosci Nurs. 2013;45(3):124–132. doi: 10.1097/JNN.0b013e31828a418b. [DOI] [PubMed] [Google Scholar]
- 5.Hou R, Moss-Morris R, Peveler R, et al. When a minor head injury results in enduring symptoms: a prospective investigation of risk factors for postconcussional syndrome after mild traumatic brain injury. J Neurol Neurosurg Psychiatry. 2012;83:217–23. doi: 10.1136/jnnp-2011-300767. [DOI] [PubMed] [Google Scholar]
- 6.Marshall S, Bayley M, McCullagh S, Velikonja D, Berrigan L, Ouchterlony D, Weegar K, mTBI Expert Consensus Group Updated clinical practice guidelines for concussion/mild traumatic brain injury and persistent symptoms. Brain Inj. 2015;29(6):688–700. doi: 10.3109/02699052.2015.1004755. [DOI] [PubMed] [Google Scholar]
- 7.Cicerone KD, Langenbahn DM, Braden C, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch Phys Med Rehabil. 2011;72:519–530. doi: 10.1016/j.apmr.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Chen SH, Thomas JD, Glueckauf RL, et al. The effectiveness of computer-assisted cognitive rehabilitation for persons with traumatic brain injury. Brain Inj. 1997;11:197–209. doi: 10.1080/026990597123647. [DOI] [PubMed] [Google Scholar]
- 9.Akerlund E, Esbjornsson E, Sunnerhagen KS, Bjorkdahl A. Can computerized working memory training improve impaired working memory, cognition and psychological health? Brain Inj. 2013;27(13–14):1649–1657. doi: 10.3109/02699052.2013.830195. [DOI] [PubMed] [Google Scholar]
- 10.Bjorkdahl A, Akerlund E, Svensson S, Esbjornsson E. A randomized study of computerized working memory training and effects on functioning in everyday life for patients with brain injury. Brain Inj. 2013;27(13–14):1658–1665. doi: 10.3109/02699052.2013.830196. [DOI] [PubMed] [Google Scholar]
- 11.De Luca R, Calabro RS, Gervasi G, et al. Is computer-assisted training effective in improving rehabilitative outcomes after brain injury? A case-control hospital-based study. Disabil Health J. 2014;7:356–60. doi: 10.1016/j.dhjo.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Fernandez E, Bringas ML, Salazar S, et al. Clinical impact of RehaCom software for cognitive rehabilitation of patients with acquired brain injury. MEDICC Rev. 2012;14:32–35. doi: 10.37757/MR2012V14.N4.8. [DOI] [PubMed] [Google Scholar]
- 13.Johansson B, Tornmalm M. Working memory training for patients with acquired brain injury: effects in daily life. Scand J Occup Ther. 2012;19(2):176–183. doi: 10.3109/11038128.2011.603352. [DOI] [PubMed] [Google Scholar]
- 14.Lebowitz MS, Dams-O'Connor K, Cantor JB. Feasibility of computerized brain plasticity-based cognitive training after traumatic brain injury. J Rehabil Res Dev. 2012;49(10):1547–1556. doi: 10.1682/jrrd.2011.07.0133. [DOI] [PubMed] [Google Scholar]
- 15.Li K, Robertson J, Ramos J, Gella S. Computer-based cognitive retraining for adults with chronic acquired brain injury: A pilot study. Occup Ther Health Care. 2013;27(4):333–344. doi: 10.3109/07380577.2013.844877. [DOI] [PubMed] [Google Scholar]
- 16.Li K, Alonso J, Chadha N, Pulido J. Does generalization occur following computer-based cognitive retraining? – An exploratory study. Occup Ther Health Care. 2015;29(3):283–296. doi: 10.3109/07380577.2015.1010246. [DOI] [PubMed] [Google Scholar]
- 17.Simmons CD, Arthanat S, Marci VJ. Pilot study: Computer-based virtual anatomical interactivity for rehabilitation of individuals with chronic acquired brain injury. JRRD. 2014;51(3):377–390. doi: 10.1682/JRRD.2013.05.0103. [DOI] [PubMed] [Google Scholar]
- 18.Yip BCB, Man DWK. Virtual reality-based prospective memory training program for people with acquired brain injury. NeuroRehabil. 2013;32:103–115. doi: 10.3233/NRE-130827. [DOI] [PubMed] [Google Scholar]
- 19.Zickefoose S, Hux K, Brown J, Wulf K. Let the games begin: a preliminary study using attention process training-3 and Lumosity brain games to remediate attention deficits following traumatic brain injury. Brain Inj. 2013;27(6):707–716. doi: 10.3109/02699052.2013.775484. [DOI] [PubMed] [Google Scholar]
- 20.Chin LMK, Keyser RE, Dsurney J, et al. Improved cognitive performance following aerobic exercise training in people with traumatic brain injury. Arch Phys Med Rehabil. 2015;96(4):754–759. doi: 10.1016/j.apmr.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Twamley EQ, Thomas KR, Gregory AM, Jak AJ, Bondi MW, Delis DC, Lohr JB. CogSMART Compensatory Cognitive training for traumatic brain injury. J Head Trauma Rehabil. 2015;30(6):391–401. doi: 10.1097/HTR.0000000000000076. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.