Abstract
Objectives
A prospective randomised controlled trial to investigate the efficacy of electromagnetic transduction therapy (EMTT) for treatment of patients with non-specific low back pain.
Design
Two groups with non-specific low back pain were either treated with conventional therapy alone over 6 weeks or in combination with 8 sessions of EMTT.
Results
In both intervention groups the low back pain related pain and the degree of disability decreased significantly at follow-up visits. Combination of EMTT and conventional therapy proved significant superior to conventional therapy alone.
Conclusion
EMTT is a promising treatment in patients with non-specific low back pain.
Keywords: PEMF, Low back pain, EMTT, Conservative treatment, Electromagnetic fields, ODS
1. Introduction
Low back pain (LBP) is the most common ailment of musculoskeletal system among working age adults. It is affecting about 80% of the population at least once at some point in life.1, 2 It is not only recognized as a significant medical disease problem, but also regarded as major cause for work absences in industrialised societies. Both results in huge costs for national economics and health care systems because of long lasting and cost intensive treatment options especially in chronic cases. These treatments in chronic cases include non-invasive as well as invasive or minimally invasive modalities, which are associated with high risks of adverse effects and increased morbidity.
The classification of low back pain is complicated by the varying presentation and complex nature of pain. The European evidence-based guidelines on behalf of the COST B13 working group have defined low back pain as discomfort and pain, localized below the costal margin and above the inferior gluteal with or without leg pain. The most common diffuse pain without radiating beyond the buttocks is classified as nonspecific low back pain.3 Pain that radiates down the leg and changes in severity in response to specific maneuvers is defined as radicular pain. The third category of this diagnostic triage is of spinal origin and is called serious spinal pathology. Red flags such as violent trauma, fever, a history of malignant tumor or structural deformity indicate further clinical diagnostics.3 Low back pain is also distinguished by duration in acute (less than 6 weeks), sub-acute (6–12 weeks) and chronic (12 weeks or more) pain, which has gained international acceptance.
The initial treatment for acute nonspecific low back pain is typically conservative, including non-opioid analgesics, physiotherapy, thermotherapy and if necessary short course of muscle relaxants. Moon et al. showed a significant reduction of low back pain by lumbar stabilisation and dynamic strengthening exercise.4 To stay as active as possible and to return early to normal activities, including work seems to be the best treatment option. Further conservative methods for treating nonspecific low back pain are for example traction treatment, manual therapy and transcutaneous electrical nerve stimulation (TENS). Back school is related to treatment of subacute low back pain or secondary prevention of chronic low back pain. In addition, minimal invasive treatment methods, such as selective nerve root blocks and epidural injection up to surgery interventions may be used, if no response to conservative methods is seen. Invasive options normally start with minimal invasive techniques. Excellent evidence was shown by percutaneous lysis of adhesions in chronic radiculopathy.5, 6
A promising technology for non-invasive treatment of musculoskeletal disorders are pulsed electromagnetic fields (PEMF). PEMF are selected low-frequency electromagnetic fields without ionizing or thermal effect.7 In 1979, the Food and Drug Administration (FDA) approved PEMF as effective and safe for the treatment of bone fractures and nonunions.8 The growing interest in their mechanisms of action leads to numerous in vitro trials confirming their effectiveness in up-regulating anti-inflammatory adenosine receptor A2A and A3 under exposure of PEMF, reducing PGE2 and pro-inflammatory cytokine IL-6 and IL-8 and inhibiting factor NF-kB transcription in human chondrocytes and osteoblasts.9 Furthermore PEMF increased proliferation and enhanced osteogenic differentiation of mesenchymal stem cells (MSCs) isolated from human bone in several in vitro studies.10, 11 These results confirmed the effectiveness of pulsed electromagnetic fields in stimulating activity and differentiation of specific cell cultures of the musculoskeletal system. PEMF devices are approved by the FDA to fuse broken bones, reduce tissue and joint pain and support muscle function. However most controlled randomized clinical trials failed to show significant effects and the interest for PEMF waned within the last 2 decades. Presumed reasons therefore are inadequate electromagnetic field power and missing dynamic oscillating. Electromagnetic transduction therapy (EMTT) is a promising new technology of treatment based on PEMF with magnetic field strength between 80 and 150 mT and oscillating frequencies of 120 Hz of each impulse. EMTT acts via electromagnetic transduction. This treatment is also classified as a soft tissue engineering therapy. Impulses are emitted by a high-speed generator to build up a voltage up to 30 kV which is released in nanoseconds and an impulse release frequency of 3 Hz. The very short duration of each impulse ensures full electrophysical reaction without any temperature increase in the tissue.
So far, a clinical study of EMTT combined with conventional non-invasive treatment modalities on low back pain has not been performed. The aim of this randomized controlled trial was to investigate if EMTT has a significant effect on non-specific low back pain if applied as an adjunct to standardized non-invasive care.
2. Methods
The study was implemented between February 2016 and August 2016. Participants with non-specific low back pain were randomly assigned to receive either conventional non-invasive treatment with physiotherapy and analgesic drugs (k-group; n = 44) or a combination of conventional non-invasive treatment plus EMTT (EMTT-group; n = 44) for 6 weeks (Table 1). Because of surgery intervention one participant was excluded from k-group during the trial. The allocation was done in a blinded manner concealed in permuted blocks of four to eight with the use of a computer-generated random list. Concealment of randomization was guaranteed by non-transparent envelopes. The trial was in accordance with the standardized guidelines of good clinical practice from the International Conference on Harmonization.
Table 1.
Flow chart of a the randomized controlled trial in accordance to the CONSORT Statement.
 |
The study was registered in the German Clinical Trial register (DRK S 00011648) and approved by the local ethical committee. No X-ray or ultrasound guidance was necessary. All patients provided written informed consent. Inclusion and exclusion criteria are listed in Table 2. Physiotherapy included core stabilisation, isometric strengthening and physical therapy such as heat plus non-opiate analgesics (Ibuprofen 2 × 800 mg/d and Metamizol 4 × 500 mg/d over 6 weeks) according to the low back pain treatment recommendations. Patients in the EMTT group received identical non-invasive intervention during the 6 weeks. In addition, EMTT was applied twice per week with a total of 8 sessions with the Cellactor MT1 device (Storz Medical AG, Tägerwilen, Switzerland). Each treatment was done over 20 min at 80mT with an impulse frequency of 3 Hz and an electric power of 30 kV. After 6 weeks all participants were allowed to use up to 1600 mg of Ibuprofen and 2000 mg of Metamizol per day on demand as a rescue medication. No other therapies were allowed.
Table 2.
Inclusion and exclusion criteria.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
2.1. Primary outcome measures
The primary endpoint measure was the change of disability, using the Oswestry disability index score (ODS) (0–100% disability; minimal disability (=0%) to either bed-bound or exaggerating symptoms (=100%)12) and the change in subjective pain sensation quantified by scoring on the 10-point visual analogue rating scale (VAS) 12 weeks after last intervention compared to baseline. The change in pain sensation was defined as change of non-specific low back pain while doing daily activities. The pressure level that just elicited unbearable pain was related to a VAS score 10. In order to keep the multiple level of alpha, both primary efficacy criteria had to be statistically significant. Primary outcome measures were analyzed with last value carried forward (LVCF), replacement of missing values and correction for interfering analgesic therapy.
2.2. Secondary outcome measures
The secondary endpoint was measured by the change in VAS and ODS 6 weeks after last interventions.
2.3. Safety criteria
All subjects with at least one intervention of EMTT were included in the safety population. Patients were followed throughout the study and all local tissue effects and adverse events were recorded.
2.4. Statistical analysis
The sample size calculation was based on the model of stochastic superiority within the parametric student t-test or non-parametric Wilcoxon-Mann-Whitney test for the primary and secondary outcome measure, depending on the distribution of the data. To analyse the distribution of the two treatment groups, we used the shapiro wilk test. The following stipulations were made: relevant Mann-Whitney (MW) effect size = 0.64 for superiority of the intervention, alpha (one-sided) = 0.025, and beta (power) = 0.10. Due to usual ambiguities of the study (dropout etc.) the sample size for the study was enhanced to N = 44 per group. To analyse a possible correlation between ODS and VAS score on the one hand and age of the participants and duration of low back pain on the other hand the Pearson product moment correlation coefficient and Spearman rank correlation coefficient was used. In order to keep the multiple level of alpha, efficacy of the combined therapy is confirmed if both primary criteria of effectiveness (ODS and VAS score) show a statistically significant result. A value of p < 0.025 (one-sided) was considered statistically significant.
3. Results
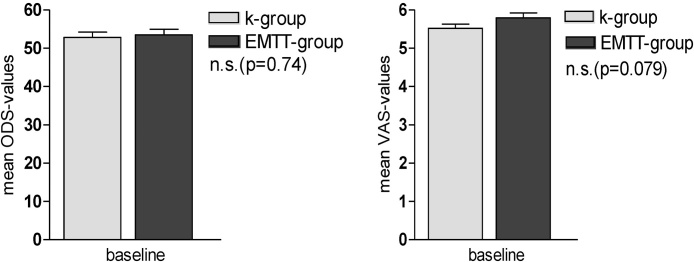
In total 87 patients with non-specific low back pain were treated as randomized according to the study protocol with either conventional physiotherapy plus analgesics (k-group) or in combination with electromagnetic transduction therapy (EMTT-group). All patients were treated as allocated and randomized. We used the Wilcoxon-Mann-Whitney test to analyse both groups at baseline. Across the two groups, no significant difference was found with regards to primary criteria VAS values (p = 0.403) nor for ODS values at baseline (p = 0.463) as well as biometric data (Table 3; Fig. 1).
Table 3.
Demographic data at baseline.
| Subject Demographics | |||
|---|---|---|---|
| k-group | EMTT-group | p-value | |
| No Pts | 43 | 44 | |
| Female | 26 | 21 | >0.05 |
| Age (years) | 59.02 ± 11.2 | 61.93 ± 10,34 | >0.05 |
| VAS | 5,64 ± 0.92 | 5.8 ± 0.82 | >0.05 |
| ODS | 52.8 ± 9.11 | 53.48 ± 9.85 | >0.05 |
Fig. 1.
VAS and ODS score at baseline.
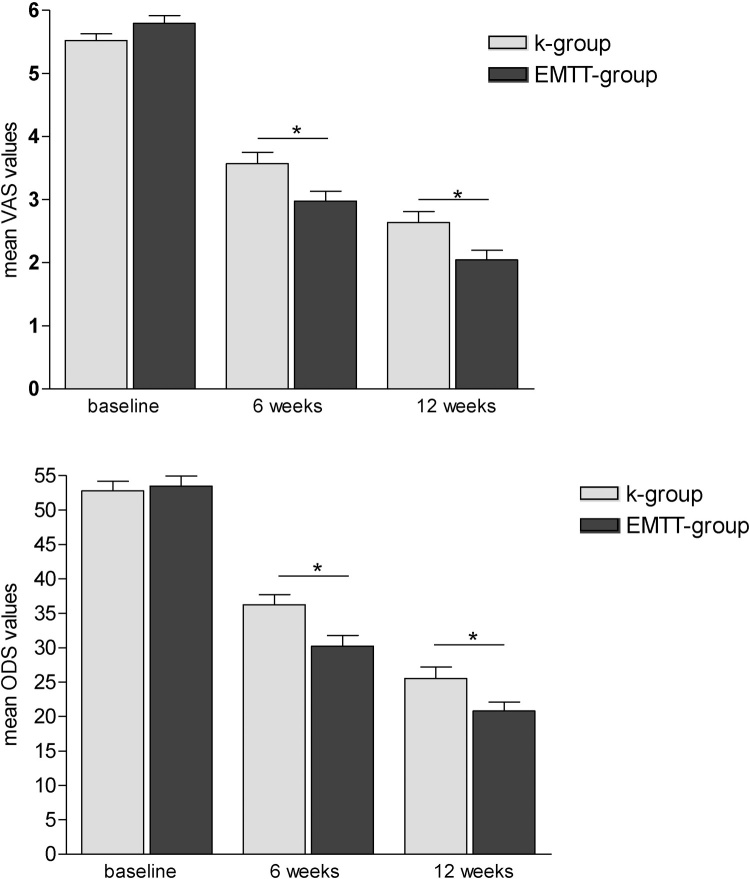
3.1. Analyses within k-group and EMTT-group
In this study protocol the k-group was treated with physiotherapy plus analgesics. The subjective pain perception was analyzed and found to improve significantly at 6 and 12 weeks after last intervention compared to baseline. The VAS score decreased by 36.7% from 5.64 ± 0.92 at baseline to 3.57 ± 1.21 after 6 weeks (p < 0.001) and by 48.8% to 2.98 ± 1.05 after 12 weeks (p < 0.001). A significant improvement of ODS, as a parameter for disability, was also noted after 6 weeks with an oswestry disability index score of 36.25 ± 9.75 and after 12 weeks of 30.23 ± 10.29, compared with ODS score of 52.80 ± 9.11 at starting point. Likewise, the combined therapy with EMTT in the EMTT-group showed significant improvement of VAS score and ODS score within the group at both follow up visits after last intervention. The VAS values decreased significantly by 64.7% during the period of 12 weeks from 5.80 ± 0.82 at baseline to 2.64 ± 1,16 after 6 weeks (p < 0.001) and 2.05 ± 1.01 after 12 weeks (p < 0.001). Compared to baseline the ODS score also decreased significantly by 61.07% in total after EMTT plus physiotherapy and analgesics. Means dropped form 53.48 ± 9.85 at baseline to 25.55 ± 10.89 (p < 0.001) after 6 weeks and to 20.82 ± 8.59 (p < 0.001) after 12 weeks (Fig. 2).
Fig. 2.
VAS and ODS values at baseline, 6 and 12 weeks in k-group and EMTT-group.
3.2. Analyses between control-group and EMTT-group
The in-between group difference analysis of conservative physiotherapy plus analgesics (k-group) versus combined therapy with pulsed electromagnetic fields (EMTT-group) shows significantly better outcome in favor of the EMTT-group. At baseline indeed there are no statistical significant differences between both parametric treatment groups based on VAS (p = 0.272) and ODS (p = 0.737), measured by student t-test. After 6 weeks, the ODS of patients treated with conventional non-invasive treatment and EMTT in combination (25.55 ± 10.9) decreased significantly more compared with conventional non-invasive treatment alone (36.25 ± 9.75; p < 0.001). Also 12 weeks after last intervention the disability of patients with low back pain measured by ODS was significant lower in EMTT-group (20.82 ± 8.59) compared with k-group (30.22 ± 10.29; p < 0.001).
Analogous to the results of the ODS evaluation the VAS score was significant lower in EMTT-group after 6 weeks (2.636 ± 1163) and 12 weeks (2.045 ± 1.011) in relation to k-group after 6 weeks (3.568 ± 1.208; p < 0.001) und 12 weeks (2.977 ± 1.045; p < 0.001). These findings are illustrated by Fig. 3.
Fig. 3.
Mean VAS and ODS scores of k-group versus EMTT-group at baseline, 6 and 12 weeks after treatment.
3.3. Correlation of VAS and ODS with age and duration of illness
We used the Pearson product moment correlation coefficient and Spearman rank correlation coefficient to verify if there were any significant relationships between patient age or duration of low back pain bevor treatment and subjective pain sensation or disability. We found no significant correlation between VAS baseline scores either for patient age (p = 0.56; p = 0.51) nor for duration of low back pain (p = 0.26; p = 0.22). At baseline there are also no significant relationships between disability using the Oswestry low back pain disability score and age (p = 0.72; p = 0.65) or duration of illness (p = 0.074; p = 0.046) of any patient.
The analysis of safety criteria showed no clinically relevant adverse event but some skin erythema right after treatment which disappears within 1 h after end of treatment. No device related adverse event occurred within the study period. At the final study endpoint no patients reported about aby side effect due to the EMTT.
4. Discussion
Musculoskeletal system disorders (MSDs) are the most commonly encountered problems in orthopaedics and physiotherapy practice all over the world and low back pain is the most prevalent of musculoskeletal presentations encountered in clinical practice with corresponding deformities and huge economic loss especially in chronic cases with a pain history longer than 12 weeks. Therefore it is crucial to establish new effective and non-surgical treatment modalities with minimal side effects.
This randomized controlled trial provides reliable evidence in primary and secondary endpoint that electromagnetic transduction therapy could effectively reduce pain intensity and improve the physical functioning of non-specific low back pain patients.
Several in vitro trials document evident biochemical pathways stimulated by electromagnetic impulses including stimulating osteoblast growth activity,13 neovasculogenesis, release of growth factors and improvement of blood supply. The proangiogenic effect of PEMF might be a main reason for pain and disability reduction. In this context clinical trials showed an increase in tissue blood flow in the lumbopelvic region and improved lumbopelvic stability after core training among patients with chronic non-specific low back pain.14
EMTT acts via electromagnetic transduction resulting in engineering a larger treatment area up to 30 cm in diameter. One of the most important physical parameters of PEMF is defined as strength of electromagnetic field measured in Millitesla (mT). In earlier times, different PEMF devices and technologies were designed but most clinical trials failed to proof efficacy. Furthermore, basic research is still lacking to verify biological relevant effects by missing the physical parameters needed to reach to induce significant biological reaction and activate repair mechanism. Our data show that 80mT is a promising electromagnetic strength to initiate significant clinical effects. Another important parameter of the investigated device seems to be the high oscillating frequency with a single EMTT impulse. With other electromagnetic devices, single static rectangular impulses are used to treat patients still without relevant clinical evidence. Therefore the MT1 device used in this prospective randomized controlled trial fulfils the promising criteria needed to perform electromagnetic transduction with evident biological effects.
This study reports for the first time, evidence level 2a results of a combined therapy of conservative therapy and EMTT to treat low back pain. It was found that both treatment modalities have a synergetic effect on outcome by increasing significantly the results based on disability and subjective pain sensation compared with common conservative therapy alone. These results suggest that PEMF therapy is beneficial in reducing pain and disability in patients with back pain and should be made part of holistic care for back pain. Previous research has shown that patients with low back pain who engage in moderate to high levels of physical activity have better prognosis in terms of pain, disability, and quality of life than those who fail to maintain adequate levels of physical activity.15 In this regard, EMTT is an important form of treatment to support physical activity without relevant side-effects.
Finally two limiting aspect of this trial have to be discussed. First aspect is the effect of placebo effect size due to a device related enhanced placebo effect.16, 17 The EMTT machine could induce such a placebo effect. The real placebo effect size has to be determined in further trial focusing on placebo research only as well as the real placebo effect in EMTT treatments by a double blinded prospective placebo controlled study design. The second limitation is the short follow up period of 12 weeks after last intervention. Long term effects have also to be analyzed with another trial with follow up intervals longer than 6 month after intervention.
Further studies have to evaluate the effect of EMTT also as a stand-alone treatment option for low back pain as well as EMTT in combination with invasive interventions.
Conflicts of interest
The author declares no conflict of interest.
Acknowledgments
The study was supported by Storz Medical AG (Tägerwilen, Switzerland) by providing the treatment devices within the study time. The sponsor did not have influence on handling of subjects, data collection, data analysis or preparation of the manuscript.
Contributor Information
André Krath, Email: andre.krath@uksh.de.
Ludger Gerdesmeyer, Email: Gerdesmeyer@aol.com.
References
- 1.Hoy D., Bain C., Williams G. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64:2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 2.van Tulder M., Koes B., Bombardier C. Low back pain: best practice & research. Clin Rheumatol. 2002;16:761–775. doi: 10.1053/berh.2002.0267. [DOI] [PubMed] [Google Scholar]
- 3.van Tulder M., Becker A., Bekkering T. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J. 2006;15(Suppl. 2):S169–S191. doi: 10.1007/s00586-006-1071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moon H.J., Choi K.H., Kim D.H. Effect of lumbar stabilization and dynamic lumbar strengthening exercises in patients with chronic low back pain. Ann Rehab Med. 2013;37:110–117. doi: 10.5535/arm.2013.37.1.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerdesmeyer L., Lampe R., Veihelmann A. Chronic radiculopathy: use of minimally invasive percutaneous epidural neurolysis according to Racz. Schmerz. 2005;19:285–295. doi: 10.1007/s00482-004-0371-x. [DOI] [PubMed] [Google Scholar]
- 6.Gerdesmeyer L., Wagenpfeil S., Birkenmaier C. Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: a randomized, double-blind, placebo-controlled trial. Pain Physician. 2013;16:185–196. [PubMed] [Google Scholar]
- 7.Rubik B. Bioelectromagnetics & the future of medicine. Adm Radiol J. 1997;16:38–46. [PubMed] [Google Scholar]
- 8.Bassett C.A. Fundamental and practical aspects of therapeutic uses of pulsed electromagnetic fields (PEMFs) Crit Rev Biomed Eng. 1989;17:451–529. [PubMed] [Google Scholar]
- 9.Vincenzi F., Targa M., Corciulo C. Pulsed electromagnetic fields increased the anti-inflammatory effect of A(2)A and A(3) adenosine receptors in human T/C-28a2 chondrocytes and hFOB 1.19 osteoblasts. PloS One. 2013;8:e65561. doi: 10.1371/journal.pone.0065561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaivosoja E., Sariola V., Chen Y., Konttinen Y.T. The effect of pulsed electromagnetic fields and dehydroepiandrosterone on viability and osteo-induction of human mesenchymal stem cells. J Tissue Eng Regen Med. 2015;9:31–40. doi: 10.1002/term.1612. [DOI] [PubMed] [Google Scholar]
- 11.Jansen J.H., van der Jagt O.P., Punt B.J. Stimulation of osteogenic differentiation in human osteoprogenitor cells by pulsed electromagnetic fields: an in vitro study. BMC Musculoskelet Disord. 2010;11:188. doi: 10.1186/1471-2474-11-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Little D.G., MacDonald D. The use of the percentage change in Oswestry Disability Index score as an outcome measure in lumbar spinal surgery. Spine. 1994;19:2139–2143. doi: 10.1097/00007632-199410000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Li J.K., Lin J.C., Liu H.C., Chang W.H. Cytokine release from osteoblasts in response to different intensities of pulsed electromagnetic field stimulation. Electromagn Biol Med. 2007;26:153–165. doi: 10.1080/15368370701572837. [DOI] [PubMed] [Google Scholar]
- 14.Paungmali A., Henry L.J., Sitilertpisan P., Pirunsan U., Uthaikhup S. Improvements in tissue blood flow and lumbopelvic stability after lumbopelvic core stabilization training in patients with chronic non-specific low back pain. J Phys Ther Sci. 2016;28:635–640. doi: 10.1589/jpts.28.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pinto R.Z., Ferreira P.H., Kongsted A., Ferreira M.L., Maher C.G., Kent P. Self-reported moderate-to-vigorous leisure time physical activity predicts less pain and disability over 12 months in chronic and persistent low back pain. Eur J Pain. 2014;18:1190–1198. doi: 10.1002/j.1532-2149.2014.00468.x. [DOI] [PubMed] [Google Scholar]
- 16.Carvalho C., Caetano J.M., Cunha L., Rebouta P., Kaptchuk T.J., Kirsch I. Open-label placebo treatment in chronic low back pain: a randomized controlled trial. Pain. 2016;157:2766–2772. doi: 10.1097/j.pain.0000000000000700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jonas W.B., Crawford C., Colloca L. To what extent are surgery and invasive procedures effective beyond a placebo response? A systematic review with meta-analysis of randomised, sham controlled trials. BMJ Open. 2015;5:e009655. doi: 10.1136/bmjopen-2015-009655. [DOI] [PMC free article] [PubMed] [Google Scholar]