Highlights
-
•
Idiopathic SEL is very rare, since no predisposing factors can be identified.
-
•
SEL should be included in the differential diagnosis when patients present with progressive spinal neurological compromise.
-
•
MRI is the imaging modality of choice.
-
•
Decompressive laminectomy and debulking of the fatty lesion is the main treatment modality.
Keywords: Spinal cord compression, Epidural lipomatosis, Paraplegia, Review
Abstract
Introduction
Spinal epidural lipomatosis (SEL) is a rare condition that presents with progressive spinal cord or nerve root compression. It is commonly reported in patients receiving long-term exogenous steroid therapy or in patients with endogenous steroid overproduction. The occurrence of this condition as an idiopathic entity is rarely reported.
Case presentation
The authors present the clinical course and outcome of a 16-year-old male student, who presented with progressive spastic paraparesis of a one-year duration caused by idiopathic spinal epidural lipomatosis. Magnetic resonance imaging (MRI) study of the thoracic spine revealed marked compression of the spinal cord from a large dorsally located extradural mass extending from the T-4 to T-12 vertebral bodies. The patient underwent posterior thoracic laminoplasty from the T4 to T10 vertebral levels. He experienced gradual neurological, and he was able to walk without assistant by the end of 3-month follow-up period from surgery.
Conclusion
Idiopathic SEL is very rare, since no predisposing factors can be identified, and should be included in the differential diagnosis when patients present with spinal neurological compromise. MRI is the imaging modality of choice, and decompressive laminectomy and debulking of the fatty lesion is the main treatment modality in patients with progressive course of the disease..
1. Introduction
Spinal epidural lipomatosis (SEL) is a rare condition, characterized by the excessive deposition of normal unencapsulated adipose tissue in the surrounding epidural space of the spinal canal, leading to spinal compression [1]. Although rare, it has been suggested that the main cause of symptomatic SEL is the use of exogenous steroids, as first described by Lee et al. [1], [2]. Since SEL causes compression on the spinal cord, it can produce symptoms that are indistinct from those of spinal stenosis and degenerative spine disease [1]. Since that time, awareness of this condition has increased among clinicians, leading to the diagnosis of more cases, with the aid of imaging coupled with clinical features [1]. Symptoms depend mainly on the level of compression in the spinal cord [3]. SEL is more common in males than in females, with a ratio of 3:1 (i.e., 75% of SEL reported cases involve male patients) [4], [5]. In SEL reported cases, it has been found that the mean age for the occurrence of SEL is 43 years. However, there is a tendency for this disease to occur in younger male patients [4], [5].
We report a case of idiopathic SEL in a healthy, non-obese, slim adolescent, affecting the thoracic region, including his clinical and imaging features, by which the patient presented for treatment in our academic center. We will discuss the current trends in the diagnosis and treatment of SEL with a review of the literature.
2. Case report
A 16-year-old high school male student was admitted to King Abdulaziz University Hospital with complaints of progressive weakness and ascending numbness of the lower limbs. This student is a healthy professional basketball player, who had been experiencing difficulty jumping over the course of one year. The weakness progressed gradually in an ascending fashion to involve the lower limbs. His presenting paraparesis was followed, a few months later, by a progressive ascending numbness in the lower limbs as well. His symptoms had worsened rapidly over the period of three months preceding his admission to our hospital, to the extent that he had difficulty in urination and became confined to a wheelchair. His past medical history was negative, with no history of drug intake, particularly corticosteroids. Over the course of the year prior his admission, he was evaluated in several clinics using electrophysiological and magnetic resonance imaging (MRI) studies and cerebrospinal fluid analysis, which were reported within normal. Several working diagnoses were proposed, including ascending motor paralysis, transverse myelitis, and tropical myelitis.
Physical examination on admission revealed a well-nourished male patient who weighed 60 kg and measured 160 cm tall (body mass index of 24). There was no spinal deformity; one café au lait spot measured 10 mm in the lower thoracic region was noted. There was marked plantar flexion deformity of his feet with an associated hyperextended inverted toe. Neurological examination of his cognitive function and cranial nerves were within normal ranges. Motor examination of the lower limbs revealed a significant hypertonia and weakness, which were mostly distal with grade 2–3 and 4 proximal. He had bilaterally hyperactive deep tendon reflexes in the lower limbs with Babinski signs and sustained ankle clonus. Sensory examination revealed hypoesthesia and impaired proprioception in lower limbs, with decreased sensation up to the level of the 5th thoracic dermatome. The motor and sensory examination of the upper limbs was normal.
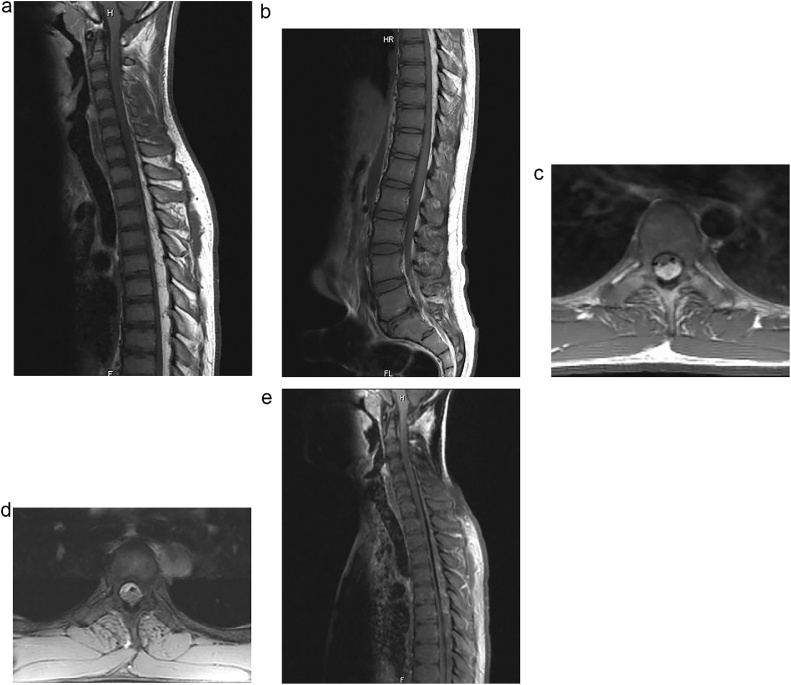
On investigation, routine laboratory blood tests including complete blood count, liver function, and renal function analysis were within normal ranges. A repeat MRI study of the thoracic spine revealed marked compression of the spinal cord from a large dorsally located extradural mass extending from the T-4 to T-12 vertebral bodies (Fig. 1). This mass had a maximum thickness of 10 mm in the middle, tapering at both the T-4 and T-12 vertebral bodies, and the spinal cord appeared to be displaced and compressed anteriorly against the posterior aspect of the vertebrae, with a significant reduction in the AP diameter of the spinal cord. Despite the marked compression, there was no spinal cord signal abnormality. The epidural lipomatous mass followed the normal fat signal in both pre-and post-suppression techniques. The post contrast images did not reveal any significant enhancement. There was no evidence of disk or vertebral column signal changes, and brain MRI study was normal.
Fig. 1.
Sagittal T1-weighted MRI scans of the cervical-thoracic (A) and thoracic-lumbar (B) regions demonstrating a hyperintense epidural posterior lesion, extending from T1 to T12 vertebral level. Axial T1 (C) and T2-weighted (D) MRI scans demonstrated marked spinal cord compression. The epidural lesion was isointense on the sagittal T1 fast suppression sequence (E).
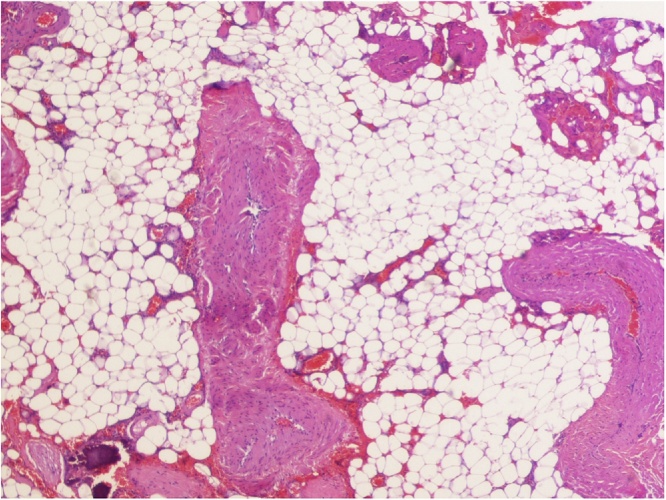
The patient underwent posterior thoracic laminoplasty from T4 to T10 vertebral levels. A dorsally located and relatively vascular firm epidural fatty tissue was encountered, which was not infiltrating the bone or the dura; it was dissected easily and completely removed in one piece. Histological examination of the operative specimen demonstrated vascularized mature fibro-fatty tissue consistent with the diagnosis of lipomatosis (Fig. 2). The patient had an uneventful postoperative period; within a week, he was experiencing gradual improvement in his paraparesis, his numbness had diminished, and he was able to walk with support. He was discharged on the 9th postoperativeday.
Fig. 2.
Photomicrograph of the histopathological examination of the surgical specimen demonstrated mature adipose tissue with surrounding fibrous tissue (H & E, X400).
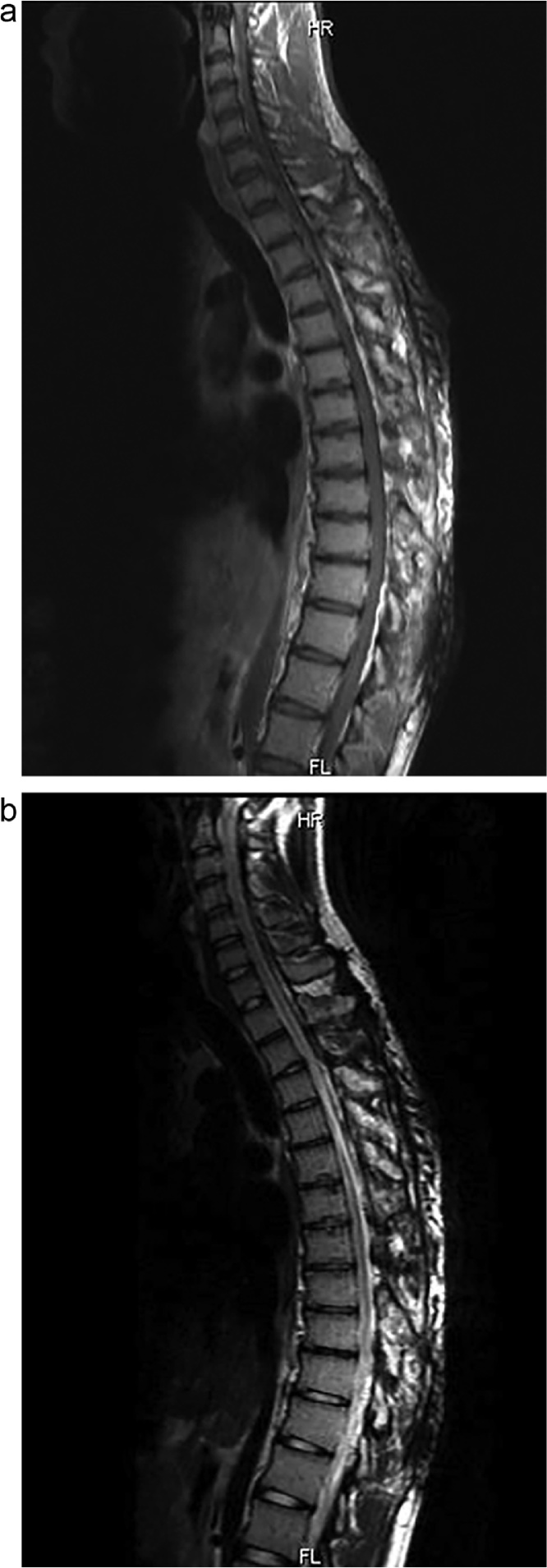
He continued to show progressive neurological improvement with extensive outpatient physiotherapy program and was able to walk unassisted after 3 months. His sphincter function had recovered with adequate spinal cord decompression on follow-up MRI scan (Fig. 3). At 4-year follow-up, his examination revealed a completely recovered neurological function.
Fig. 3.
Postoperative sagittal T1 (A) and T2-weighted (B) MRI images after laminoplasty and complete excision of SEL demonstrating no recurrence.
3. Discussion
Spinal epidural lipomatosis, particularly of the idiopathic type and located in the thoracic spinal region, is a rare occurrence. We conducted a comprehensive review of the available English literature on SEL occurring in the thoracic region, noting the most common associations of SEL and summarizing the current trends in management.
Our case is unique in that it is one of the few cases to report idiopathic SEL affecting the thoracic region in a non-obese, healthy adolescent patient. Moreover, idiopathic SEL is rarely reported in adolescents and children of 16 or less year of age in general. A case by Lee et al., was reported in a 16-year-old female, who presented with chest pain [6]. A literature review revealed only 13 cases that matched the characteristics of our present case. These studies are illustrated in Table 1.
Table 1.
Reported cases of myelopathy resulting from idiopathic spinal epidural lipomatosis.
| Author(s), Year | Age, Sex | Levels | Treatment | Outcome |
|---|---|---|---|---|
| Quint et al., 1988 [10] | 34, M | T4-T8 | Laminectomy | Improved |
| Stern et al., 1994 [11] | 75, M | T6-T8 | Laminectomy and excision of SEL | Improved |
| Selmi et al., 1994 [5] | 20, M | T3-T10 | Laminectomy | CR |
| Hughes & Jones, 1996 [12] | 21, M | T3-T10 | Laminectomy | CR |
| Iplikcioglu et al., 1998 [13] | 18, F | T3-T7 | Laminectomy | CR |
| Citow & Kranzler, 2000 [14] | 54, M | T1-T10 | Laminectomy | Improved |
| Kawai et al., 2002 [15] | 26, M | T4-T8 | Hemilaminectomy and excision of SEL | CR |
| Scarsbrook et al., 2005 [16] | 28, M | T1-T10 | Laminectomy and excision of SEL | CR |
| Shah et al., 2005 [17] | 37, F | T3-T8 | Laminectomy | Improved |
| Akhaddar et al., 2007 [18] | 24, M | T4-T9 | Laminectomy | CR |
| López-González & Resurrección Giner, 2008 [19] | 55, M | T3-T7 | Laminectomy and excision of SEL | Improved |
| Rajput et al., 2010 [20] | 18, M | T5-T7 | Laminectomy and excision of SEL | Improved |
| Lee et al., 2011 [6] | 16, F | T4-T9 | Facetectomy and ESL debulking | CR |
| Present case | 16, M | T4-T10 | Laminoplasty and complete excision of SEL | CR |
Abbreviations: NS: Not specified; CR: Complete recovery.
Koch et al. believe that the underlying pathogenesis of SEL is unknown [7]. Direct compression of the nervous structures and ischemia are the two most important mechanisms involved in producing neurological symptoms [7]. Specifically, the ischemic and necrotic appearance of the fatty tissue attests to the role of ischemia [7]. After a review of the literature, it has been found that SEL falls into five categories: exogenous steroid use (the most common cause of SEL), endogenous excess secretion of steroids, Cushing syndrome, obesity, and the idiopathic group [1].
Back pain is the most common symptom associated with SEL and the first presenting symptom in most cases [4]. Moreover, progressive lower limb weakness has also been reported to be common in SEL patients [4]. Other symptoms such as sensory symptoms (i.e., paresthesia, numbness, radicular symptoms, and sphincter malfunction) can be present but remain rare [4]. Objective findings in physical examination include weakness, change in tendon reflexs, and decreased pain sensation [4]. Nevertheless, symptoms depend solely on the level of compression; compression in the thoracic region will produce myelopathic symptoms, while compression in the lumbar region will result in radiculopathic symptoms [4].
Since the report of the first SEL case, myelography and computed tomography (CT) scan have been the main imaging modalities for the diagnosis of SEL [8] However, MRI scan is more sensitive and specific than myelography and CT scan, since the latter demonstrate signs that can be misleading in diagnosing SEL [8]. SEL appears with an almost characteristic appearance: increased signal intensity on T1-weighted images and intermediate signal intensity on T2-weighted images [4].
When correlating spinal level involvement with SEL causes, it was found that cases of SEL resulting from obesity had the highest percentage of lumbosacral involvement. However, there were no identifiable trends with other causes [1]. Moreover, there have been no reported cases of SEL affecting the cervical spine alone; rather, reported cases usually mention the involvement of the cervical spine when the whole spine is affected [1].
The main treatment options offered to patients with SEL are conservative therapy and surgical intervention [4]. Conservative therapy is usually beneficial for SEL cases that result from steroid use and obesity, through the tapering of steroid used and weight loss, respectively [4]. Cases of endogenous endocrinopathy-induced SEL must be treated first before attempting to decompress the spine [4]. Finally, in idiopathic cases, where there is no identifiable cause, conservative therapy alone has no role in treatment [4].
Meanwhile, surgical intervention is considered a second-line treatment in all SEL categories except for idiopathic cases [9]. However, when a neurological compromise is encountered, a decompressive laminectomy – or, as in our present case, laminoplasty in children and adolescents – and excision of the compressive fatty tissue is the only modality of treatment [9].
4. Conclusions
SEL is a rare disease causing spinal cord compression due to accumulation of adipose tissue, which is commonly reported with endogenous or exogenous steroid excess or obesity. Idiopathic SEL, in which no predisposing factors can be identified, is very rare, particularly in healthy children and adolescents. The diagnosis is made, with high accuracy, with the use of MRI accompanied by different sequence modalities. Asymptomatic individuals are treated conservatively, but those who present with progressive neurological deficiencies should be treated urgently with spinal cord decompression and removal of the fatty tissue, preferably through laminoplasty for children and adolescents.
SCARE guidelines
This work has been reported in line with the SCARE criteria [21].
Conflicts of interest
There are no conflicts of interest to disclose.
Sources of funding
This work was completed without financial support.
Ethical approval
This case was submitted for ethical approval.
Consent
Written informed consent was obtained from the patients for publication of this case report and accompanying images.
Author contributions
Rumaiza Al-Yafeai, Hussein Malibary, Saleh Baeesa: Management of the case.
Rumaiza Al-Yafeai, Yazid Maghrabi, Saleh Baeesa: Study design, data collection and writing.
Rumaiza Al-Yafeai, Yazid Maghrabi, Hussein Malibary, Saleh Baeesa: Writing and revision.
Saleh Baeesa: Revision of the manuscript.
Guarantor
Saleh S. Baeesa.
Contributor Information
Rumaiza Al-Yafeai, Email: smilyrose3000@hotmail.com.
Yazid Maghrabi, Email: yazid.maghrabi@gmail.com.
Hussein Malibary, Email: hmalibary@hotmail.com.
Saleh Baeesa, Email: sbaeesa@kau.edu.sa.
References
- 1.Fogel G.R., Cunningham P.Y., 3rd, Esses S.I. Spinal epidural lipomatosis: case reports, literature review and meta-analysis. Spine J. 2005;5(2):202–211. doi: 10.1016/j.spinee.2004.05.252. [DOI] [PubMed] [Google Scholar]
- 2.Lee M., Lekias J., Gubbay S.S., Hurst P.E. Spinal cord compression by extradural fat after renal transplantation. Med. J. Aust. 1975;1(7):201–203. doi: 10.5694/j.1326-5377.1975.tb111328.x. [DOI] [PubMed] [Google Scholar]
- 3.Chan J.Y., Chang C.J., Jeng C.M., Huang S.H., Liu Y.K., Huang J.S. Idiopathic spinal epidural lipomatosis – two cases report and review of literature. Chang Gung Med. J. 2009;32(6):662–667. [PubMed] [Google Scholar]
- 4.Fassett D.R., Schmidt M.H. Spinal epidural lipomatosis: a review of its causes and recommendations for treatment. Neurosurg. Focus. 2004;16(4):E11. [PubMed] [Google Scholar]
- 5.Selmi F., Davies K.G., Sharma R.R., Redfern R.M. Idiopathic spinal extradural lipomatosis in a non-obese otherwise healthy man. Br. J. Neurosurg. 1994;8(3):355–358. doi: 10.3109/02688699409029626. [DOI] [PubMed] [Google Scholar]
- 6.Lee S.B., Park H.K., Chang J.C., Jin S.Y. Idiopathic thoracic epidural lipomatosis with chest pain. J. Korean Neurosurg. Soc. 2011;50(2):130–133. doi: 10.3340/jkns.2011.50.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koch C.A., Doppman J.L., Watson J.C., Patronas N.J., Nieman L.K. Spinal epidural lipomatosis in a patient with the ectopic corticotropin syndrome. N. Engl. J. Med. 1999;341(18):1399–1400. doi: 10.1056/NEJM199910283411814. [DOI] [PubMed] [Google Scholar]
- 8.Sivakumar K., Sheinart K., Lidov M., Cohen B. Symptomatic spinal epidural lipomatosis in a patient with Cushing’s disease. Neurology. 1995;45:2281–2283. doi: 10.1212/wnl.45.12.2281. [DOI] [PubMed] [Google Scholar]
- 9.Fessler R.G., Johnson D.L., Brown F.D., Erickson R.K., Reid S.A., Kranzler L. Epidural lipomatosis in steroid-treated patients. Spine. 1992;17(2):183–188. doi: 10.1097/00007632-199202000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Quint D.J., Boulos R.S., Sanders W.P., Mehta B.A., Patel S.C., Tiel R.L. Epidural lipomatosis. Radiology. 1988;169(2):485–490. doi: 10.1148/radiology.169.2.3174998. [DOI] [PubMed] [Google Scholar]
- 11.Stern J.D., Quint D.J., Sweasey T.A., Hoff J.T. Spinal epidural lipomatosis: two new idiopathic cases and a review of the literature. J. Spinal Disord. 1994;7(4):343–349. [PubMed] [Google Scholar]
- 12.Hughes J.P., Jones E.W. Case of the month: inside a thin man—an engrossing problem. Br. J. Radiol. 1995;68(806):213–214. doi: 10.1259/0007-1285-68-806-213. [DOI] [PubMed] [Google Scholar]
- 13.Iplikcioglu A.C., Berkman M.Z., Sengoz A. Idiopathic spinal epidural lipomatosis. Acta Neurochir. (Wien) 1998;140(4):405–406. doi: 10.1007/s007010050116. [DOI] [PubMed] [Google Scholar]
- 14.Citow J.S., Kranzler L. Thoracic epidural lipomatosis with associated syrinx: case report. Surg. Neurol. 2000;53(6):589–591. doi: 10.1016/s0090-3019(00)00230-5. [DOI] [PubMed] [Google Scholar]
- 15.Kawai M., Udaka F., Nishioka K., Houshimaru M., Koyama T., Kameyama M. A case of idiopathic spinal epidural lipomatosis presented with radicular pain caused by compression with enlarged veins surrounding nerve roots. Acta Neurol. Scand. 2002;105:322–325. doi: 10.1034/j.1600-0404.2002.1c194.x. [DOI] [PubMed] [Google Scholar]
- 16.Scarsbrooka A.F., Taylora N., Yavarib A., Phillipsc A.A. Epidural lipomatosis simulating a spinal extradural haematoma. Clin. Radiol. Extra. 2005;60(2):23–26. [Google Scholar]
- 17.Shah J.A., Flynn P., Choudhari K.A. Idiopathic spinal epidural lipomatosis. Br. J. Neurosurg. 2005;19(3):265–267. doi: 10.1080/02688690500210086. [DOI] [PubMed] [Google Scholar]
- 18.Akhaddar A., Ennouali H., Gazzaz M., Naama O., Elmostarchid B., Boucetta M. Idiopathic spinal epidural lipomatosis without obesity: a case with relapsing and remitting course. Spinal Cord. 2008;46:243–244. doi: 10.1038/sj.sc.3102099. [DOI] [PubMed] [Google Scholar]
- 19.Lopez-Gonzalez A., Resurreccion Giner M. Idiopathic spinal epidural lipomatosis: urgent decompression in an atypical case. Eur. Spine J. 2008;17(Suppl. 2):S225–S227. doi: 10.1007/s00586-007-0465-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rajput D., Srivastava A.K., Kumar R. Spinal epidural lipomatosis: an unusual cause of relapsing and remitting paraparesis. J. Pediatr. Neurosci. 2010;5(2):150–152. doi: 10.4103/1817-1745.76117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]