Abstract
Background
Tobacco use is a leading behavioral risk factor for morbidity and mortality, and the tobacco epidemic disproportionately affects low-socioeconomic status (SES) populations. Taxation is effective for reducing cigarette use, and it is an effective population-based policy for reducing SES-related tobacco disparities. However, progress in implementing cigarette excise taxes has stalled across the United States, and there is a dearth of research on the full spectrum of behavioral shifts that result from taxes, particularly among low-SES populations. This project documents the impact of Minnesota’s $1.75 cigarette tax increase implemented in 2013.
Methods
Data come from the 2014 Minnesota Adult Tobacco Survey. Descriptive analyses and Latent Class Analysis (LCA) were used to provide a typology of the tax impact.
Results
From the LCA, six classes were identified, and 42% of respondents were classified as reporting action-oriented behavioral change related to the tax—8% reported sustained smoking abstinence. We found differential behavior change across levels of SES. Low-SES and medium/high-SES individuals were equally likely to report complete tobacco cessation, but the prevalence of daily smokers who reported action-oriented behavior without sustained cessation was nearly double for low-SES individuals.
Conclusions
Smokers report a range of behavioral changes in response to cigarette taxes, with differences across SES. The majority of smokers, and particularly low-SES smokers, report behavioral steps toward quitting or achieving sustained tobacco cessation in response to cigarette taxes. Complementary population-based programs geared toward assisting individuals, especially low-SES individuals, to achieve continuous tobacco cessation could increase the reach and effectiveness of cigarette taxes.
Keywords: cigarette excise taxes, statewide tobacco taxation, stages-of-change perspective, tobacco-related disparities, health equity
1. Introduction
Tobacco use is a leading behavioral risk factor for disease worldwide and the number one preventable cause of morbidity and mortality in the United States (Lim et al., 2013; McAfee, Davis, Alexander, Pechacek, & Bunnell, 2013). The tobacco epidemic also disproportionately affects people of low socioeconomic status (SES). Smoking prevalence among U.S. adults who are at or above the federal poverty level is 17% versus 28% for those below the poverty line (Centers for Disease Control and Prevention, 2014). Smoking accounts for half of mortality disparities associated with SES among men, and a similar effect is emerging among women (Jha et al., 2006; Gregoraci et al., 2016). There are a range of mechanisms that underlie the relationship between SES and smoking, including direct and indirect effects associated with income and education. Mechanisms include: stress associated with social position and deprivation; limited access to health information and health education opportunities; differential levels of human capital and subsequent self-efficacy and agency; neighborhood and community effects (e.g., tobacco companies target low-income neighborhoods for outdoor and point-of-sale advertising); and dynamics associated with social networks (see Pampel, Krueger, & Denney, 2010).
Cigarette taxation that results in higher prices is one of the most effective population-level strategies for reducing tobacco use (Chaloupka, Yurekli, & Fong, 2012; Warner, 2014). Moreover, cigarette taxation can reduce SES-related smoking disparities among adults (Brown, Platt, & Amos, 2014; Siahpush, Wakefield, Spittal, Durkin, & Scollo, 2009). However, tax increases have become less common across the United States (Holmes, King, & Babb, 2016). Between 2010 and 2014, only six states increased their rate by $1.00 or more, and of those, only Minnesota and New York increased their tax rates by $1.50 or more (Holmes et al., 2016). These trends have negative implications for the Healthy People 2020 objective of increasing cigarette excise taxes by at least $1.50 per pack in all 50 states by 2020 (Holmes et al., 2016, p. 3), as well as continuing to reduce preventable tobacco-related morbidity and mortality (Marynak et al., 2016).
As smoking prevalence rates decline, research on the impact of cigarette taxes and how taxes should be implemented will be needed to achieve maximum effectiveness (Bader, Boisclair, & Ferrence, 2011). Specifically, further research is needed to (1) build on previous literature by outlining how cigarette taxes influence behavior change, and (2) to delineate the effects of taxes on smoking cessation among subpopulations. There is substantial documentation of price elasticity and estimates of broad population-based change in regards to smoking prevalence; for instance, a 10% increase in the price of cigarettes is associated with a three to five percent reduction in cigarette use (e.g., see Chaloupka, Cummings, Morley, & Horan, 2002; Chaloupka et al., 2012).
Yet there is a dearth of population-based research on the full spectrum of behavioral shifts—i.e., the full stages-of-change continuum and heterogeneity of responses along that continuum—that result from taxes, particularly among subpopulations such as the socioeconomically disadvantaged (Grace, Kivell, & Laugesen, 2014; Choi & Boyle, 2013). According to theory rooted in a stages-of-change perspective (see Weinstein, Sandman, & Blalock, 2008; Prochaska, Redding, & Evers, 2008), in general smokers change their behavior in successive stages (e.g., contemplation, action), and smokers move along a spectrum of behavioral change (forward and backward) as they work toward achieving maintenance (i.e., complete tobacco cessation). Delineating patterns of these behavioral changes would inform efforts to expand the effectiveness of statewide tobacco taxes, offering potential avenues to strategically reach priority subpopulations and further evidence supporting tax implementation as a form of tobacco control.
1.2 Current Study
In 2013 the state of Minnesota implemented a $1.75 (U.S. dollars) tax increase on cigarettes and little cigars, and an increased tax on other tobacco products from 70% to 95% of wholesale price. The implementation of these policies occurred approximately one year (a minimum of seven months) prior to a 2014 population-based survey of Minnesota adults (Minnesota Adult Tobacco Survey [MATS]), providing a unique opportunity to study smoking behavior change in response to a statewide tobacco tax. Utilizing methods geared toward classifying behavior patterns, we aim to document a detailed typology of tax responses in line with a stages-of-change perspective, focusing on responses for both current smokers and former smokers. We also assess how behavior changes in response to the tax are differentially distributed across low-SES and high-SES subpopulations. A central goal is to inform prevention programs geared toward expanding taxes’ effectiveness for reducing smoking prevalence and smoking-related disparities.
2. Methods
2.1 Data
Data come from the 2014 MATS, a statewide, cross-sectional telephone survey that assessed tobacco use among 9,304 Minnesotans aged 18 or older. A landline and cellphone random-digit-dial (RDD) sampling method was used. Sampling consisted of a two-step process: a household screening questionnaire to identify households, followed by sampling within the household. The combined response rate was 71%. The MATS survey is weighted to account for sampling and geographical stratification in order to ensure statewide representativeness (see ClearWay Minnesota & Minnesota Department of Health, 2014).
2.2 Sample
The study sample consisted of smokers at time of cigarette tax increase and who had smoked within the past 12 months, and individuals who had not smoked within the 12 months prior to MATS but reported quitting between 12 and 24 months prior (Overall sample n=1,569). We included former smokers because tobacco taxes can serve as a “commitment device” for cessation maintenance (e.g., Gruber & Koszegi, 2004), and because individuals quit in preparation for tax increases (e.g. Reed et al., 2008). List-wise deletion was used for missing data; less than 5% of the sample was removed. Supplementary analyses that used pair-wise deletion exhibited nearly identical results.
2.3 Measures
2.3.1 Self-reported response to tax
MATS included a question about the tax increase that asked, “Taxes on the purchase of tobacco products have increased in the past 12 months in Minnesota. What effects, if any, did this price increase have on your smoking?” Four subsequent questions asked if the tax helped respondents to: (1) think about quitting, (2) cut down on cigarettes, (3) make a quit attempt, and (4) maintain a quit. Following a stages-of-change perspective (see Weinstein et al., 2008; Prochaska et al., 2008), we scored each individual according to the highest ordered behavioral stage reported.
In accordance with theory and previous research (see Kingsbury et al., 2016), we used three mutually exclusive, ordered categories of “no action” (no response and contemplation), “action” (cigarette reduction and quit attempt), and “maintenance” (maintained quit attempt). Individuals labeled as maintenance reported their highest level of behavior change as “maintained a quit attempt”; alternatively, if the highest level of change reported was reduced amount of cigarettes or made a quit attempt, then respondents were labeled as “action.” If individuals reported no response or thought about quitting, they were labeled as “no action” in accordance with action being a distinct stage compared to contemplation and pre-contemplation (Prochaska et al., 2008).
2.3.2 Smoking-related behavior
Following past research (Choi & Boyle, 2013; Dunlop, Perez, & Cotter, 2011), we employed three measures of smoking behavior: current smoking status, smoking status 12 months prior to MATS, and engaging in price minimizing behaviors. Current smoking status was measured using established definitions of: (1) daily smoker (>100 cigarettes in lifetime and currently smoker every day), (2) smoking some days (>100 cigarettes in lifetime and currently smoke some days), (3) former smoker (>100 cigarettes in lifetime, does not smoke at all currently and has not smoked in past 30 days), and (4) current experimenter (<100 cigarettes in lifetime but has smoked in past 30 days). Prior smoking was measured as smoking status 12 months prior to survey: (1) smoking daily, (2) smoking some days, (3) not smoking at all, and (4) had quit 12 to 24 months prior to survey.
For price minimization behaviors, respondents were asked, “In the past 12 months, have you done any of the following things to try and save money on cigarettes: buy cheaper brand of cigarettes, roll own cigarettes, use other form of tobacco, use coupons/rebates/or other special promotions, buy cartons instead of individual packs, find less expensive places to buy cigarettes, smoke fewer cigarettes, shared fewer cigarettes with others, saved half a cigarette for later, or ‘other’.” The dichotomous measure captured whether respondents had engaged in one or no behaviors to save money on cigarettes in previous 12 months versus two or more money-saving behaviors in previous 12 months (0=no price minimization behavior; 1=price minimization behavior). The cutoff for two behaviors was chosen because more than one behavior was more indicative of price minimization compared to a single act (e.g., using a coupon once).
2.3.3 Socioeconomic status and demographics
Considering SES measures applied to public health (Oakes & Rossi, 2003), our main focus was on low SES, and we employed a three-stage process to create the measure. Following previous research (Pampel et al., 2010), we examined education and income separately for all analyses. Education and income exhibited similar relationships to all outcomes; consequently, we scaled education and income, creating a composite index. We used Stata 13’s default method, which created a mean score for a four-level education measure (1=less than high school, 2=high school degree/GED, 3=some college or technical degree, 4=college degree or beyond) and a four-level household income score (1=$35,000 or less, 2=$35,001–$50,00, 3=$50,001–$75,000, 4=more than $75,000; α = .60). Following previous research (e.g., Chapman, Fiscella, Kawachi, & Duberstein, 2010), we constructed a measure of low SES. We found individuals in the bottom 25% of the index distribution for the representative sample of Minnesota accurately captured individuals with both lower incomes and lower levels of education (1=low SES, 0=medium/high SES). Other key demographics included were gender (1=male, 0=female), race/ethnicity (1=white, 0=nonwhite), marital status (1=married, 0=not married), and a continuous measure of age.
2.4 Analytic Strategy
First, we examined prevalence of self-reported responses to the tax. We also examined differences across self-reported stages of change in terms of means and proportions for current smoking behavior, prior smoking behavior, price minimization behavior, socioeconomic status, and other demographics. We also examined if these relationships with the tax response remained significant in a multivariate ordered logistic regression model that used the tax response as the outcome (0=no action, 1=action, 2=maintenance), adjusting for all covariates included in the analysis.
We then employed a second round of analyses consisting of latent class analysis (LCA; see Collins & Lanza, 2010). LCA was used to classify behavioral response profiles that combined self-reported responses, current smoking behavior, prior smoking behavior, and price minimization. This second round of analyses allowed for a systematic assessment and prevalence estimate of a behavior-change typology in response to the tax. We report the selection criteria used for the latent class structure, item-response probabilities, and prevalence of classes, providing details on how we arrived at the classification results as well as the nature and prevalence of the behavior-change classes. Our primary focus for these analyses was on behavioral response patterns based on relevant smoking behavior for the entire population of Minnesota.1 Finally, we explored the differential response types across SES by examining the prevalence of latent classes across low-SES and medium/high-SES groups. For these LCA analyses, we tested for measurement invariance for item-response probabilities, as well as model fit differences for testing latent-class prevalence differences (see Collins & Lanza, 2010: 113–148).2
All analyses were conducted in Stata v.13.1, and all analyses used weights from MATS to ensure state representativeness. We used svy: mean and svy: tab with subgroups to compare smoking behaviors and demographics across levels of self-reported tax impact (with Stata’s default of Chi-square, F-ratios and adjusted Wald tests). We also corrected for multiple comparisons via the Bonferroni method in the descriptive analyses where applicable (all necessary comparisons demonstrated the significance tests remained unchanged, and therefore we do not report these results). LCA was conducted in Stata using doLCA plugin (see Lanza, Dziak, Huang, Wagner, & Collins, 2015).
3. Results
3.1 Self-reported Tax Responses
Approximately 41.8% (95% CI= 38.6, 45.0) exhibited no action, 37.8% (95% CI= 34.6, 40.9) reported action-oriented behavior (quit attempt or cigarette reduction), and 20.5% (95% CI= 17.9, 23.1) reported maintaining a quit attempt in response to the tax.
3.2 Differences across Smoking Behavior and Demographics
Differences existed across smoking status (χ2=358.31; p<.001), smoking status in the 12 months prior (χ2=120.69; p<.001), price minimization behavior (χ2=295.50; p<.001), and demographics in terms of reported responses to the tax (see Table 1). Current smokers reported higher rates of action in response to the tax compared to former smokers (current smokers=52% and 41% vs former smokers=9%), and former smokers reported higher rates of maintenance (former smokers=45% vs current smokers=7%, 23%, and 22%). Daily smokers in the prior 12 months reported higher rates of action in response to the tax (46%) compared to other prior smoking statuses (39%, 18%, and 5%). Smokers who had quit 12 to 24 months prior reported the highest rate of maintenance (40%). More price minimization behavior was related to action more than no action or maintenance (53% vs 34% and 3%, respectively).
Table 1.
Smoking-related Behavior and Demographics by Smokers’ Behavioral Response to Tax Increase
| Variables | Tax Response : | No Action (n =653) | Action (n =585) | Maintenance (n =331) | Odds ratio (95% CI)* |
|---|---|---|---|---|---|
|
| |||||
| Proportion or mean (95% CI) | |||||
| Current smoking status | |||||
| Current smoker/daily | .52 (.47, .57) | .74 (.70, .79) | .18 (.13, .24) | 0.10 (0.06, 0.18) | |
| Current smoker/some days | .13 (.10, .17) | .17 (.13, .21) | .18 (.12, .24) | 0.27 (0.14, 0.50) | |
| Former smoker | .30 (.25, .34) | .07 (.04, .09) | .60 (.53, .67) | Reference group | |
| Current experimenter | .05 (.03, .07) | .02 (.01, .04) | .04 (.02, .06) | 0.27 (0.11, 0.63) | |
| Smoking frequency 12 months ago | |||||
| Daily | .57 (.52, .62) | .77 (.72, .81) | .53 (.46, .60) | Reference group | |
| Some days | .14 (.11, .18) | .16 (.12, .20) | .17 (.12, .22) | 0.70 (0.45, 1.08) | |
| Not at all | .19 (.15, .23) | .07 (.04, .10) | .16 (.11, .21) | 0.40 (0.22, 0.75) | |
| Quit within past 2 years | .10 (.07, .13) | .01 (.00, .02) | .14 (.09, .19) | 0.42 (0.18, 0.99) | |
| >1 price minimization behavior (vs <=1) | .53 (.48, .58) | .92 (.89, .94) | .43 (.36, .50) | 3.48 (2.20, 5.51) | |
| Socioeconomic status (SES) | |||||
| Low SES | .34 (.30, .39) | .47 (.42, .52) | .45 (.38, .52) | Reference group | |
| Medium/high SES | .58 (.53, .63) | .44 (.39, .49) | .48 (.41, .55) | 0.66 (0.50, 0.87) | |
| Missing | .08 (.05, .10) | .09 (.06, .12) | .07 (.03, .11) | 0.71 (0.43, 1.17) | |
| White (vs non-white) | .83 (.79, .88) | .81 (.76, .85) | .83 (.78, .89) | 1.17 (0.82, 1.65) | |
| Male | .61 (.56, .66) | .51 (.46, .57) | .56 (.49, .63) | 0.77 (0.60, 0.98) | |
| Married (vs not married) | .45 (.40, .50) | .37 (.32, .42) | .34 (.27, .40) | 0.78 (0.60, 1.02) | |
| Age | 42.56 (41.12, 44.00) | 40.52 (39.07, 41.97) | 40.42 (38.29, 42.55) | 0.99 (0.99, 1.00) | |
Note. N=1569; estimates are derived using survey weights; bolded differences were statistically significant p<.05;
odds ratios are from a multivariate ordered logistic regression model with tax-response stages (0=no action, 1=action, 2=maintenance) as the outcome; 95% confidence intervals are in parentheses.
There were significant differences across tax responses for SES (χ2=26.70; p<.01), gender (χ2=11.53; p<.05), and marital status (χ2=15.08; p<.05). Low SES individuals reported high rates of action and low rates of no action relative to medium/high SES individuals (action=43% vs 33%, respectively; no action=35% vs 48%, respectively). Separate analyses that compared individuals missing SES to both low and high SES groups showed no significant differences; therefore, missing on SES data was not systematically related to outcomes. Males compared to females reported higher rates of no action (45% vs 37%, respectively). Married individuals reported higher rates of no action compared to unmarried individuals (48% vs 38%, respectively). Supplemental analyses showed demographic variables and smoking-related behaviors were interrelated. An important relationship was that former smokers were more likely to be married as well as high/medium SES. Subsequently, we examined the associations between smoking-related behavior measures and tax-related change adjusting for covariates, which is presented on the right-hand side of Table 1. All covariates were related to the tax response in the expected direction, and smoking-related variables (e.g., smoking status) remained significantly related to the tax response adjusting for all covariates.
3.3 Latent Class Selection Criteria
Table 2 presents model fit statistics. The G2 statistic was statistically significant in all models, and therefore p-values are not reported in Table 2. We concluded that the six-class model demonstrated the best fit based on AIC, BIC, adjusted BIC, and log-likelihood measures. The five- and seven-class models were the only other models with good fit statistics, such as entropy and G2, but we also relied heavily on class interpretability and item-response probabilities for selecting the six-class model (see Collins & Lanza, 2010). We found the six-class model was qualitatively important compared to the five-class model: a persistent smoker class was divided into two relatively large classes, with one class reporting a strong response the tax and the other showing no tax response. The seven-class model also pointed to retaining the six-class model, as the additional class in the seven-class model relative to the six-class model was extremely small and qualitatively inconsequential.
Table 2.
Summary of Latent Class Selection Criteria
| Number of Latent Classes | Number of Parameters Estimated | G2 | df | AIC | Adjusted Log-likelihood | |||
|---|---|---|---|---|---|---|---|---|
| BIC | BIC | value | Entropy R2 | |||||
| 1 | 9 | 2558.50 | 86 | 2576.50 | 2624.73 | 2596.14 | −6038.46 | 1.00 |
| 2 | 19 | 820.47 | 76 | 831.96 | 933.76 | 873.41 | −5156.19 | 0.90 |
| 3 | 29 | 368.37 | 66 | 426.37 | 581.76 | 489.64 | −4943.39 | 0.92 |
| 4 | 39 | 234.28 | 56 | 312.28 | 521.25 | 397.35 | −4876.34 | 0.85 |
| 5 | 49 | 156.02 | 46 | 254.02 | 516.57 | 360.91 | −4837.22 | 0.84 |
| 6 | 59 | 104.03 | 36 | 222.03 | 538.16 | 350.73 | −4811.22 | 0.76 |
| 7 | 69 | 59.71 | 26 | 197.71 | 567.42 | 348.22 | −4789.06 | 0.80 |
| 8 | 79 | 27.74 | 16 | 185.74 | 609.04 | 358.07 | −4773.08 | 0.79 |
P-values are not reported for G2
N=1569
3.4 Latent Classes: Prevalence and Characteristics
Table 3 displays prevalence estimates of the six latent classes and item-response probabilities. We found two classes with limited to no response to the tax: (1) current daily smokers who were daily smokers 12 months prior to MATS and who reported price minimization behavior—labeled “persistent smokers” (prevalence: 20%); and (2) individuals not smoking 12 months prior who reported a range of current smoking statuses and no price minimization behavior—labeled “past-year initiators” (prevalence: 9%). Two classes exhibited moderate responses to the tax: (1) former smokers who had quit between 12 and 24 months prior to MATS and who did not engage in price minimization—labeled “pre-tax quitters” (prevalence: 14%); and (2) nondaily smokers who smoked some days 12 months prior and who exhibited price minimization behavior but no definitive response to the tax—labeled “unchanged light smokers” (prevalence: 15%). Finally, two classes exhibited a high response to the tax: (1) current daily smokers who reported smoking daily in the 12 months prior, price minimization, and action in response to the tax—labeled “responsive daily smokers” (prevalence: 34%); and (2) former smokers who reported smoking daily 12 months prior, maintaining a quit attempt in response to the tax, and no price minimization—labeled “tax-driven quitters” (prevalence: 8%).
Table 3.
Six-Latent-Class Model of Smokers’ Behavioral Responses to Statewide Tobacco Tax Increase
| Low Tax Response | Moderate Tax Response | High Tax Response | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Latent class prevalence estimates: | Class labels: | Persistent Smokers | Past-year Initiators | Pre-tax Quitters | Unchanged Light Smokers | Responsive Daily Smokers | Tax-driven Quitters |
| .20 | .09 | .14 | .15 | .34 | .08 | ||
| Variables and item-response probabilities | |||||||
| Response to tax | |||||||
| No action | 0.82 | 0.87 | 0.57 | 0.24 | 0.15 | 0.03 | |
| Reduced cig. amount or quit attempt | 0.17 | 0.00 | 0.05 | 0.47 | 0.75 | 0.17 | |
| Maintained a quit attempt | 0.01 | 0.13 | 0.38 | 0.29 | 0.10 | 0.80 | |
| Current smoking status | |||||||
| Current smoker/everyday | 0.96 | 0.05 | 0.00 | 0.09 | 0.94 | 0.02 | |
| Current smoker/some days | 0.03 | 0.34 | 0.00 | 0.78 | 0.05 | 0.00 | |
| Former smoker | 0.00 | 0.37 | 1.00 | 0.02 | 0.01 | 0.98 | |
| Current experimenter | 0.00 | 0.24 | 0.00 | 0.10 | 0.00 | 0.00 | |
| Smoking frequency 12 months ago | |||||||
| Every day | 0.97 | 0.03 | 0.21 | 0.22 | 0.91 | 0.83 | |
| Some days | 0.00 | 0.41 | 0.01 | 0.53 | 0.08 | 0.15 | |
| Not at all | 0.03 | 0.56 | 0.27 | 0.25 | 0.01 | 0.02 | |
| Quit within past 2 years prior to tax | 0.00 | 0.00 | 0.51 | 0.00 | 0.00 | 0.00 | |
| Price minimization behaviors in past year | |||||||
| One or fewer | 0.20 | 0.92 | 1.00 | 0.10 | 0.00 | 0.77 | |
| Two or more | 0.80 | 0.08 | 0.00 | 0.90 | 1.00 | 0.23 | |
N=1569
Item-response probabilities >=.5 in bold to facilitate interpretation
All estimates are derived using survey weights
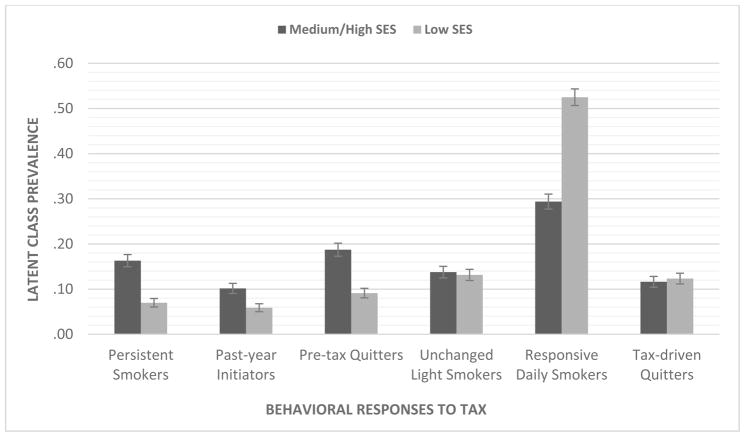
3.5 Latent Class Differences across Socioeconomic Status
The six-class structure was the best fit for both low-SES and medium/high-SES groups. Measurement invariance held across both SES groups by comparing a model that freely estimated item-response probabilities and one that constrained probabilities to be equivalent (Δ G2=45.56; Δ df=54). Comparing models that held class prevalence estimates equivalent and freely estimated class prevalence across SES groups showed that prevalence estimates differed across SES groups (Δ G2=2378.56; Δ df=5), which is visually presented in Figure 1. The most substantial difference was for “responsive daily smokers”: the prevalence estimate for the low-SES group was .52 compared to .29 for medium/high SES, suggesting that, among daily smokers, low-SES individuals were more likely to report cessation behavior in response to the tax than high-SES individuals. The low-SES group had lower prevalence estimates than the medium/high-SES group for pre-tax quitters, past-year initiators, and persistent smokers, and the magnitude of the differences were moderate.
Figure 1.
Latent Class Prevalence Differences across Socioeconoimc Status (SES)
4. Discussion
Over 55% of current and former smokers reported behavior change in response to Minnesota’s 2013 cigarette tax increase. These responses were indicative of behavioral steps toward becoming tobacco-free. More smokers reported steps toward cessation without achieving sustained cessation, but a nontrivial amount of former smokers reported maintaining cessation attributed to the tax.
LCA provided a systematic typology of tax responses. In accordance with a stages-of-change perspective, we found a full spectrum of behavioral responses. Six classes of behavioral responses were identified. The six-class typology extends previous population-based research on tobacco taxes by offering a classification schemata and population-level estimates of reported behavioral shifts. In our analysis, nearly half of current smokers at the time of the tax reported action-oriented behavioral change (42% of smokers included in LCA analyses), indicating the tax had a strong impact. The most prevalent class consisted of everyday smokers who tried to quit but did not achieve complete cessation, but a fraction of individuals reported sustained smoking abstinence in direct response to the tax.
Low-SES individuals reported higher rates of action-oriented behavior compared to medium/high-SES individuals. In LCA analyses, the prevalence of daily smokers who did not report sustained cessation but exhibited action-oriented behavior was nearly double for the low-SES group relative to the medium/high-SES group. The implication is that low-SES individuals potentially respond to cigarette excise taxes in a disproportionately strong manner, as low-SES individuals are equally likely to report maintenance and they are more likely to attempt to quit in response to tax increases compared to medium/high-SES individuals. This suggests low-SES individuals are more likely to take action but not reach sustained tobacco cessation in response to taxes. It is also important to note that there was a minor difference between SES groups in the prevalence of the “past-year initiator” class. The low-SES group was less likely to initiate smoking in the past year after the tax.
These combined findings support previous research demonstrating that tobacco taxes have a strong effect on cessation among low-SES populations (Brown et al., 2014; Bader et al., 2011; Gruber & Koszegi, 2004), and extends it by providing evidence that low-SES populations are more likely to attempt to quit in response to taxes compared to medium/high-SES populations. Even though the major response differential was not associated with complete tobacco cessation, it implies that taxes may serve as a cue to act or a commitment device (Choi & Boyle, 2013) to increase quit attempts in low-SES populations, potentially providing avenues to reduce disparities in smoking and tobacco-related illness (Siahpush et al., 2009). There are multiple barriers associated with a behavioral shift to maintenance, particularly for low-SES populations (Twyman, Bonevski, Paul, & Bryant, 2014), and these barriers need to be reduced in order for behavioral maintenance to occur (Prochaska et al., 2008).
4.1 Implications for Public Health Practice
Our finding that low-SES smokers were more likely to engage in behavioral steps toward cessation in response to the tax without achieving complete tobacco cessation has public health implications. Socioeconomically disadvantaged smokers are more likely to use cigarette expenditure minimizing strategies after a tax increase (Choi & Boyle, 2017), and as we found, low-SES individuals are more likely to be a member of a class of smokers that was more motivated to quit after a tax, more likely to engage in price minimization behavior, and less apt to become tobacco-free. Therefore, policies that take into account price minimization strategies could assist low-SES populations to achieve tobacco cessation, potentially by offering avenues for motivated individuals to continue behavioral progress toward cessation.
For example, certain tobacco products can promote steps toward cessation (Donny et al., 2015), and statewide policies can regulate these differential products in a strategic manner in order to promote tobacco cessation (Donny et al., 2014); and providing free or reduced-cost products (e.g., free nicotine replacement therapy via direct mail) can assist low-SES populations to achieve cessation (see Cunningham et al., 2016). In addition, individuals on Medicaid currently smoke at rates ranging from double to triple the national average (Ku, Bruen, Steinmetz, & Bysshe, 2016), and multiple programs have proven to help connect Medicaid recipients to cessations services (e.g., see Keller et al., 2011; Land et al., 2010). Another potential route to reach low-SES individuals who may respond strongly to tobacco taxes could be through Medicaid programs.
In terms of more general implications, a combination of population-based prevention strategies in conjunction with tobacco tax increases could yield the biggest impact on smoking cessation (Keller, Greenseid, Christenson, Boyle, & Schillo, 2015; Levy, Ellis, Mays, & Huang, 2013). Complementary programs implemented in conjunction with tax increases need to be concurrent, as there is a limited window of time within which complementary programs can be effective (Keller et al., 2015). These complementary programs should consider using media that encourages quit attempts (e.g., the “TIPS” campaign; see McAfee et al., 2013), as well as provide resources and access to cessation services (Keller et al., 2015; Slater et al., 2016; Haas et al., 2015). Programs could also attempt to alter multilevel and social processes that influence tobacco-related disparities (Twyman et al., 2014), as well as harness processes that are inherent in the quitting process such as social support and social contexts that provide pro-change mechanisms (Parks et al., 2016; Kingsbury et al., 2016). Since mechanisms that underlie the relationship between low-SES and smoking status include stress, social networks, neighborhood effects, and limited access to health education materials (Pampel et al., 2010), complementary programs need to address these multilevel risk factors through media, easily accessible counseling, and free cessation services.
4.2 Limitations
A limitation of the current study was the use of self-reported data. Answers could have been influenced by the survey instrument or problems with recall. In addition, these data were collected in Minnesota, which is a state with a strong tobacco prevention and control program. Future studies are needed to replicate our findings in other states and at the national level. It is possible our findings may not generalize to locations with different smoking norms or greater barriers to quitting. The design of our study did not allow for the examination of causal effects of the tax increase, and results should be interpreted in this vein. Future research should attempt to generate results from experimental or quasi-experimental studies in order to test and document causal effects of tax increases on the full spectrum of behavioral change outlined in the current study. For instance, pre- and post-test surveys in addition to using another state as a control group could serve as a quasi-experimental examination of how smoking-related behavioral change occurs in response to tax increases. Finally, future studies could consider other theoretical approaches beyond the stages-of-change perspective used to measure the tax impact in the current study; for example, future surveys could assess how the “3 Ts” approach (i.e., tension, triggers, and treatment) may help to measure tax-related behavior change (see West & Sohal, 2006).
5. Conclusion
Smokers report a range of behavioral changes in response to cigarette taxes. This study emphasizes how a substantial proportion of smokers report behavioral steps toward quitting or maintaining sustained tobacco cessation in response to statewide taxes. Low-SES populations report strong responses to cigarette taxes, both in terms of trying to quit as well as achieving complete cessation. A potential avenue for increasing the reach and effectiveness of cigarette taxes is the implementation of population-based programs geared toward helping individuals to achieve sustained tobacco cessation. Programs that address multilevel barriers to complete cessation in addition to harnessing pro-change mechanisms could offer the most potential for increasing the impact of taxes, especially if programs reach socioeconomically disadvantaged populations who are disproportionately affected by the tobacco epidemic.
Footnotes
We considered how demographics influenced class structure and differences across demographic breakdowns (race/ethnicity, gender, and age). Results were not included and these demographics did not dramatically alter the class structure. Adjusting for covariates slightly altered class prevalence; however, our research question concerned smoking-related behavior for all demographic groups.
We ran LCA models with and without missing SES data, as LCA in Stata can account for missing data in its estimation procedure. We found equivalent results; we report results that excluded individuals with missing SES data (N=1,432). Both sets of results are available upon request.
Contributor Information
Michael J. Parks, Health Promotion and Chronic Disease Division, Minnesota Department of Health, 85 7th Place E., St. Paul, MN 55101, USA.
John H. Kingsbury, Office of Statewide Health Improvement Initiative, Minnesota Department of Health, St. Paul, MN, USA.
Raymond G. Boyle, Department of Research Programs, Clear Way Minnesota, Minneapolis, MN, USA.
Kelvin Choi, Division of Intramural Research, National Institute on Minority Health and Health Disparities, Bethesda, MD, USA.
References
- Bader P, Boisclair D, Ferrence R. Effects of tobacco taxation and pricing on smoking behavior in high risk populations: A knowledge synthesis. International Journal of Environmental Research and Public Health. 2011;8:4118–4139. doi: 10.3390/ijerph8114118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T, Platt S, Amos A. Equity impact of population-level interventions and policies to reduce smoking in adults: A systematic review. Drug and Alcohol Dependence. 2014;138:7–16. doi: 10.1016/j.drugalcdep.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2005–2012. Morbidity and Mortality Weekly Report. 2014;63(2):29–34. [PMC free article] [PubMed] [Google Scholar]
- Chaloupka FJ, Cummings KM, Morley CP, Horan JK. Tax, price and cigarette smoking: Evidence from the tobacco documents and implications for tobacco company marketing strategies. Tobacco Control. 2002;11(suppl1):I62–72. doi: 10.1136/tc.11.suppl_1.i62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaloupka FJ, Yurekli A, Fong GT. Tobacco taxes as a tobacco control strategy. Tobacco Control. 2012;21(2):172–180. doi: 10.1136/tobaccocontrol-2011-050417. [DOI] [PubMed] [Google Scholar]
- Chapman BP, Fiscella K, Kawachi I, Duberstein PR. Personality, socioeconomic status, and all-cause mortality in the United States. American Journal of Epidemiology. 2009;171(1):83–92. doi: 10.1093/aje/kwp323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K, Boyle RG. Minnesota smokers’ perceived helpfulness of 2009 federal tobacco tax increase in assisting smoking cessation: A prospective cohort study. BMC Public Health. 2013;13:965–971. doi: 10.1186/1471-2458-13-965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi K, Boyle RG. Changes in cigarette expenditure minimising strategies before and after a cigarette tax increase. Tobacco Control. 2017 doi: 10.1136/tobaccocontrol-2016-053415. advanced online access. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ClearWay Minnesota, & Minnesota Department of Health. Minnesota Adult Tobacco Survey. 2014 Retrieved from http://www.mnadulttobaccosurvey.org/
- Collins LM, Lanza ST. Latent class and latent transition analysis. Hoboken, NJ: John Wiley & Sons, Inc; 2010. [Google Scholar]
- Cunningham JA, Kushnir V, Selby P, Tyndale RF, Zawertailo L, Leatherdale ST. Effect of mailing nicotine patches on tobacco cessation among adult smokers: A randomized clinical trial. JAMA Internal Medicine. 2016;176(2):184–190. doi: 10.1001/jamainternmed.2015.7792. [DOI] [PubMed] [Google Scholar]
- Donny EC, Denlinger RL, Tidey JW, Koopmeiners JS, Benowitz NL, … Hatsukami DK. Randomized trial of reduced-nicotine standards for cigarettes. New England Journal of Medicine. 2015;373:1340–1349. doi: 10.1056/NEJMsa1502403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donny EC, Hatsukami DK, Benowitz NL, Sved AF, Tidey JW, Cassidy RN. Reduced nicotine product standards for combustible tobacco: Building an empirical basis for effective regulation. Preventive Medicine. 2014;68:17–22. doi: 10.1016/j.ypmed.2014.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop SM, Perez D, Cotter T. Australian smokers’ and recent quitters’ responses to the increasing price of cigarettes in the context of a tobacco tax increase. Addiction. 2011;106:1687–1695. doi: 10.1111/j.1360-0443.2011.03492.x. [DOI] [PubMed] [Google Scholar]
- Grace RC, Kivell BM, Laugesen M. Predicting decreases in smoking with a cigarette purchase task: Evidence from an excise tax rise in New Zealand. Tobacco Control. 2014 doi: 10.1136/tobaccocontrol-2014-051594. advance online publication. [DOI] [PubMed] [Google Scholar]
- Gregoraci G, van Lenthe FJ, Artnik B, Bopp M, Deboosere P …, the DEMETRIQ consortium. Contribution of smoking to socioeconomic inequalities in mortality: A study of 14 European countries, 1990–2004. Tobacco Control. 2016 doi: 10.1136/tobaccocontrol-2015-052766. advanced online publication. [DOI] [PubMed] [Google Scholar]
- Gruber J, Koszegi B. Tax incidence when individuals are time-inconsistent: The case of cigarette excise taxes. Journal of Public Economics. 2004;88:1959–1987. [Google Scholar]
- Haas JS, Linder JA, Park ER, Gonzalez I, Rigotti NA, … Williams DR. Proactive tobacco cessation outreach to smokers of low socioeconomic status: A randomized clinical trial. JAMA Internal Medicine. 2015;175(2):218–226. doi: 10.1001/jamainternmed.2014.6674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes CB, King BA, Babb SD. Stuck in neutral: Stalled progress in statewide comprehensive smoke-free laws and cigarette excise taxes, United States, 2000–2014. Preventing Chronic Disease. 2016;13:150409. doi: 10.5888/pcd13.150409. http://dx.doi.org/10.5888/pcd13.150409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha P, Peto R, Zatonski W, Boreham J, Jarvis MJ, Lopez AD. Social inequalities in male mortality, and in male mortality from smoking: Indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet. 2006;368:367–370. doi: 10.1016/S0140-6736(06)68975-7. [DOI] [PubMed] [Google Scholar]
- Keller PA, Christiansen B, Kim SY, Piper ME, Redmond L, … Fiore MC. Increasing consumer demand among Medicaid enrollees for tobacco dependence treatment: The Wisconsin Medicaid Covers It campaign. American Journal of Health Promotion. 2011;25(6):392–395. doi: 10.4278/ajhp.090923-QUAN-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller PA, Greenseid LO, Christenson M, Boyle RG, Schillo BA. Seizing an opportunity: Increasing use of cessation services following a tobacco tax increase. BMC Public Health. 2015;15:354. doi: 10.1186/s12889-015-1667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku L, Bruen BK, Steinmetz E, Bysshe T. Medicaid tobacco cessation: Big gaps remain in efforts to get smokers to quit. Health Affairs. 2016;35(1):62–70. doi: 10.1377/hlthaff.2015.0756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingsbury JH, Parks MJ, Amato MS, Boyle RG. Deniers and admitters: Examining smoker identities in a changing tobacco landscape. Nicotine & Tobacco Research. 2016;18(11):2130–2137. doi: 10.1093/ntr/ntw110. [DOI] [PubMed] [Google Scholar]
- Land T, Warner D, Paskowsky M, Cammaerts A, Wetherell L, … Keithly L. Medicaid coverage for tobacco dependence treatments in Massachusetts and associated decreases in smoking prevalence. PLOS ONE. 2010;5(3):e9770. doi: 10.1371/journal.pone.0009770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Dziak JJ, Huang L, Wagner AT, Collins LM. LCA Stata plugin users’ guide (Version 1.2.1) University Park: The Methodology Center; Penn State: 2015. [Google Scholar]
- Levy DT, Ellis JA, Mays D, Huang AT. Smoking-related deaths averted due to three years of policy progress. Bulletin of the World Health Organization. 2013;91:509–518. doi: 10.2471/BLT.12.113878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, … Ezzati M. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 region, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2013;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marynak KL, Xu X, Wang X, Holmes CB, Tynan MA, Pechacek T. Estimating the impact of raising prices and eliminating discounts on cigarette smoking prevalence in the United States. Public Health Reports. 2016;131:536–543. doi: 10.1177/0033354916662211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAfee T, Davis KC, Alexander RL, Pechacek TF, Bunnell R. Effect of the first federally funded US antismoking national media campaign. Lancet. 2013;382:14–20. doi: 10.1016/S0140-6736(13)61686-4. [DOI] [PubMed] [Google Scholar]
- Oakes JM, Rossi PH. The measurement of SES in health research: Current practice and steps toward a new approach. Social Science & Medicine. 2003;56:769–784. doi: 10.1016/s0277-9536(02)00073-4. [DOI] [PubMed] [Google Scholar]
- Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annual Review of Sociology. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks MJ, Slater JS, Rothman AJ, Nelson CL. Interpersonal communication and smoking cessation in the context of an incentive-based program: Survey evidence from a telehealth intervention in a low-income population. Journal of Health Communication. 2016;21(1):125–133. doi: 10.1080/10810730.2015.1039677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: Jossey-Bass; 2008. pp. 97–121. [Google Scholar]
- Reed MB, Anderson CM, Vaughn JW, Burns DM. The effect of cigarette price increases on smoking cessation in California. Prevention Science. 2008;9:47–54. doi: 10.1007/s11121-008-0081-1. [DOI] [PubMed] [Google Scholar]
- Siahpush M, Wakefield MA, Spittal MJ, Durkin SJ, Scollo MM. Taxation reduces social disparities in adult smoking prevalence. American Journal of Preventive Medicine. 2009;36(4):285–291. doi: 10.1016/j.amepre.2008.11.013. [DOI] [PubMed] [Google Scholar]
- Slater JS, Nelson CL, Parks MJ, Ebbert JO. Connecting low-income smokers to tobacco treatment services. Addictive Behaviors. 2016;52:108–114. doi: 10.1016/j.addbeh.2015.10.013. [DOI] [PubMed] [Google Scholar]
- Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: A systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4:e006414. doi: 10.1136/bmjopen-2014-006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner KE. Death and taxes: Using the latter to reduce the former. Tobacco Control. 2014;23(suppl1):i4–6. doi: 10.1136/tobaccocontrol-2013-051079. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Sandman PM, Blalock SJ. The precaution adoption process model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: Jossey-Bass; 2008. pp. 123–147. [Google Scholar]
- West R, Sohal T. “Catastrophic” pathways to smoking cessation: Findings from national survey. BMJ. 2006;332:458–460. doi: 10.1136/bmj.38723.573866.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]