Abstract
OBJECTIVES
To examine the effects of a telephone-delivered intervention, Family Intervention: Telephone Tracking—Caregiver (FITT-C), on community support and healthcare use by dementia caregivers.
DESIGN
Randomized, controlled trial.
SETTING
Academic medical center.
PARTICIPANTS
Dyads (n = 250) of distressed informal dementia caregivers and care recipients.
INTERVENTION
Caregivers were randomly assigned to receive the FITT-C (n = 133) or telephone support (TS; n = 117). Both groups received 16 telephone contacts from a master’s-level therapist over 6 months. The FITT-C intervention provided psychoeducation, problem solving, and other directive approaches based on assessment of critical areas (e.g., mood, behavior, family functioning, social support). TS provided supportive therapeutic strategies.
MEASUREMENTS
Outcome variables were caregiver report of community support service use, number of visits to the emergency department (ED) for caregivers and care recipients, and hospital stays for caregivers during the interventions.
RESULTS
Intervention groups did not differ in demographic characteristics, use of support services, or use of healthcare resources at baseline. Caregivers who received the FITT-C used community support services at end of treatment significantly more than those receiving TS (P = .02). FITT-C caregivers had a significantly lower rate of ED visits (rate difference 9.5%, P = .048) and hospital stays (rate difference 11.4%, P = .01) over the 6-month course of the intervention than TS caregivers. Care recipient use of community or medical resources did not differ according to group.
CONCLUSION
An entirely telephone-delivered intervention was effective in increasing caregiver engagement in community resources and reducing caregiver use of hospital-based healthcare resources. Results highlight the potential effect of FITT-C on healthcare use.
Keywords: caregiver, dementia, healthcare use, telephone intervention
The main source of support for individuals with dementia is family caregivers, who provide 90% of in-home care. Dementia caregivers are at risk of chronic stress, anxiety, depression, poor quality of life, sleep problems, cognitive impairment, and decline in health habits.1–3 Higher caregiver burden is associated with greater severity of these factors,4 and greater burden is observed in live-in caregivers than in those who live apart from the care recipient.5
Although many community support services are available to caregivers, few individuals take advantage of these programs, or they wait until crisis before seeking help. In a previous study, 70% to 80% of 241 dementia caregivers did not attend support groups or use respite services;6 78% of those who did not lived with the recipient, and 77% were spouses. Nonusers were older and more depressed and received less social support than users. Qualitative studies indicate that dementia caregivers are reluctant to use community-based services because they do not think they need them or lack knowledge of services or because the care recipient is opposed to it.7 Support services have the potential to reduce caregiver burden and, when engaged in early, are associated with delayed nursing home placement.8
Dementia caregivers tend to have a high rate of acute medical care use, which is associated with caregiving stressors. 9 For example, emergency department (ED) visits are correlated with depression, care recipient behavior problems, and care recipient functioning.10 One study found that family members of individuals with Alzheimer’s disease (AD) had greater medical burden scores and used more ED and outpatient services than age-matched family members of individuals without AD.11 Mood and anxiety disorders, insomnia, substance abuse or dependence, cardiovascular disease, and rheumatoid arthritis were also more common in family members of individuals with AD than in family members of individuals without AD. Evidence from a 6-year longitudinal study showed that more comorbid conditions and greater dependence of individuals with dementia were associated with greater caregiver healthcare use, including hospital stays.12
Psychosocial interventions reduce depression and caregiver distress.13,14 A multisite study that compared an active intervention with an education control condition found significantly better caregiver perceived health at 6 months with the intervention.15 Medicare-eligible caregivers who received a dementia case management program had lower likelihood of any hospitalizations than a comparison group.16 Some interventions have been associated with delayed nursing home placement, but little is known about the specific effects of psychosocial caregiver interventions on healthcare and community support service use.
The Family Intervention: Telephone Tracking—Caregiver (FITT-C) was developed using focus groups and in preliminary studies.17,18 In a randomized study of 250 dementia caregivers, FITT-C reduced depressive symptoms and negative caregiver reactions to care recipient behavior problems.19 Because the intervention encouraged caregivers to engage in self-care activities, the current study examined whether there were group differences in use of healthcare resources and community support services. It was hypothesized that individuals who received FITT-C would use fewer healthcare resources and engage in more community support services than a control condition: telephone support (TS). Finally, the study examined whether emotional factors that FITT-C improves (caregiver depressive symptoms, burden, reaction to behavioral symptoms) were correlated with community service use and healthcare use.
METHODS
Study Design and Procedures
This study was part of a randomized, controlled trial examining the efficacy of a telephone-based intervention (FITT-C) on caregiver well-being. A complete description of study procedures and baseline data (including the Consolidated Standards of Reporting Trials flow diagram) were previously published.19 Caregivers were randomized to FITT-C (n = 133) or TS (n = 117) using urn randomization. Caregivers were blinded to intervention condition and told that the purpose of the study was to examine two support programs for dementia caregivers. Face-to-face assessments were conducted at baseline (before randomization), at which time all caregivers received a resource packet containing educational materials about dementia services and resources for dementia caregiving.
The FITT-C and TS conditions were both entirely telephone-based. Initial calls were 60 minutes long, and follow-up calls were 15 to 30 minutes long, depending on the severity of caregiver problems. Outcome measures were caregiver report of community support service use, total number of visits to the ED, total visits to the doctor, and total hospital stays for caregivers and care recipients (hospital stay data not available for care recipients) during the intervention period. The Rhode Island Hospital institutional review board approved study procedures. All caregivers signed informed consent, and care recipients signed when appropriate.
Participants
Participants were 250 informal dementia caregivers (aged 62.7 ± 13.0; 78% female; 95% Caucasian) and their care recipients. They were recruited through community advertising and physician referral. Caregivers were required to have been providing supervision or assistance for at least 6 months for at least 4 hours per day and to endorse at least two of nine negative experiences associated with caregiving (overwhelmed, sad mood, frustration, loss of family or friend contact, family conflict, neglecting health, too many demands of caregiving, exhaustion, neglecting own needs or other responsibilities). Caregivers were required to be primarily English speaking and have access to a telephone. Caregivers were excluded for major acute medical illness or cognitive impairment. Care recipients were required to have a formal diagnosis of dementia made by a specialist, live in the community, and have no plan for long-term care placement within 6 months. The Clinical Dementia Rating Scale (CDR)20 was used to characterize dementia severity in care recipients. Care recipients with other major medical conditions affecting independent functioning were excluded.
Intervention Groups
The FITT-C intervention was designed to reduce depression and burden in dementia caregivers. Trained master’s level therapists (mental health counselors, social workers, nurses) contacted caregivers 16 times over the telephone over 6 months, providing information about dementia, recommendations for resources, and emotional support. Caregivers were encouraged to attend to their own physical, emotional, and social needs. To reinforce these goals, therapists reviewed various coping strategies to ameliorate ongoing problems. Complete details have been previously published.18,19
TS consisted of an approach based on a nondirective therapy condition.21 The goal of TS was to provide nondirective support for caregivers through empathic and reflective listening, open-ended questioning, and venting techniques. Trained therapists conducted 16 telephone contacts over 6 months. Although TS contacts did not involve providing information about dementia or caregiving, if caregivers expressed inaccurate knowledge, therapists provided accurate information.
Outcome Measures
A research assistant who was blind to group assignment recorded healthcare resource use and community support services over the telephone at baseline and monthly throughout the intervention by administering a questionnaire (Appendix S1). Questions covered the caregiver and care recipient. The number of times in the past month that the caregiver or care recipient used community support services was assessed. Healthcare resource use included caregiver doctor visits, ED visits, and hospitalizations, and care recipient doctor visits and ED visits. Out-of-pocket costs were also recorded.
Additional measures administered to caregivers at baseline and 6 months included the Zarit Burden Interview,22 a measure of caregiver burden; the Center for Epidemiologic Studies Depression Scale,23 a measure of depression; and the Revised Memory and Behavior Problem Checklist,24 which measures frequency of care recipient behavior problems and caregiver reaction to problem behaviors.
Statistical Analyses
Descriptive statistics and independent-samples t-tests were used to characterize the sample and examine differences between treatment groups. Significant between-group differences were noted for education, but education was not associated with any of the outcomes of interest, and interpretation of the findings did not differ between analyses with and without adjustment for education. For that reason and for ease of interpretation, analyses were conducted without education as a covariate. Independent-samples t-tests were conducted to examine between-group differences in community support service use at baseline (the month before the intervention) and during the final month of treatment (6-month time point). Community support service use was calculated by summing the number of times individuals used each of 11 components of community support services before treatment and at the end of treatment. Follow-up analyses were conducted if there were overall group differences to determine which types of resources differed between the groups. Bivariate correlations were conducted to examine associations between community resource and primary outcome measures in caregivers in each group separately.
For healthcare resource use, independent-samples t-tests were conducted to examine group differences in use of doctor and ED visits (caregiver and care recipient) and hospitalizations (caregiver only) at baseline and for the monthly average for each of these variables over the 6 months of the intervention. Absolute differences in rate of hospital stays and ED visits between treatment groups and 95% confidence intervals were also calculated.
Follow-up correlational analyses were conducted to examine whether demographic variables and changes in depression, burden, and caregiver reaction to problem behaviors from baseline to 6 months were related to healthcare resource use. Change scores were created by calculating the difference between baseline and 6-month scores in these variables (6 months–baseline), with negative scores representing positive outcomes (e.g., decrease in depression, burden). Independent-samples t-tests were also used to compare out-of-pocket costs throughout the intervention, and chi-square analyses were used to examine group differences in nursing home placement by the end of the intervention. Significance was defined as α < .05.
RESULTS
Sample Characteristics and Attrition
As published previously, 15% (n = 38) of the original 250 caregiver–care recipient dyads dropped out of the study by 6-month follow up, with no significant group differences in attrition.16 Additional participants were excluded because of missing data on primary outcomes, including baseline healthcare resources and community support services data (n = 11) and 6-month community support services data (n = 6); 199 participants were retained for analyses (FITT-C, n = 105; TS, n = 94).
Most caregivers were female (78.4%) and Caucasian (96.0%), and they had an average age of 63.1 ± 12.5 and an average 14.9 ± 2.7 years of education. Most care recipients were Caucasian (96.0%), approximately half were female (55.3%), and they had an average age of 77.8 ± 9.9 and an average 13.0 ± 4.4 years of education. The majority of care recipients had mild dementia (CDR 1; 65.8%). Independent-samples t-tests revealed that caregivers in FITT-C had significantly more years of education (15.3 ± 2.8; t(197) = 2.23, P = .03) than those in TS (14.5 ± 2.5). There were no other differences in caregiver or care recipient demographic characteristic between FITT-C and TS participants.
Community Support Services
Caregivers
There were no differences at baseline between caregivers assigned to FITT-C (4.6 ± 10.9) and those assigned to TS (4.3 ± 7.5) (t(197) = 0.21, P = .83) in the mean number of times that community support services were used. The most commonly used support services among caregivers at baseline were the Internet (44.7%), legal services (22.6%), Alzheimer’s Association (20.6%), support groups (16.6%), and spiritual services (16.6%). At baseline, community support service use by caregivers was associated with greater depression (correlation coefficient (r) = 0.15, P = .04) and worse caregiver reaction to problem behaviors (r = 0.16, P = .03).
At the end of treatment, caregivers receiving FITT-C were significantly more likely to use community support services (8.5 ± 11.7) than caregivers receiving TS (5.1 ± 7.0) (t(173.61) = 2.46, P = .02) (Table 1). In other words, FITT-C caregivers used community resources an average of approximately eight times during the final month of the intervention, whereas TS caregivers used resources approximately five times. At the end of treatment, caregivers in the FITT-C group were more likely to contact the Alzheimer’s Association (P = .04) and seek legal services (P = .02) than caregivers in the TS group (Table 1).
Table 1.
Caregiver and Care Recipient Community Services Use at Baseline and End of Intervention
| Service | Family Intervention: Telephone Tracking—Caregiver, n = 105 | Telephone Support, n = 94 | ||
|---|---|---|---|---|
|
|
|
|||
| Baseline | 6 Months | Baseline | 6 Months | |
|
| ||||
| Mean ± Standard Deviation | ||||
| Caregiver | ||||
|
| ||||
| Total | 4.56 ± 10.86 | 8.47 ± 5.14a | 4.28 ± 7.54 | 5.14 ± 7.05a |
|
| ||||
| Support group | 0.12 ± 0.36 | 0.21 ± 0.55 | 0.36 ± 0.83 | 0.38 ± 1.04 |
|
| ||||
| Alzheimer’s Association | 0.52 ± 2.96 | 0.53 ± 1.45a | 0.38 ± 1.03 | 0.19 ± 0.74a |
|
| ||||
| Department of Elderly Affairs | 0.09 ± 0.34 | 0.30 ± 1.23 | 0.10 ± 0.39 | 0.05 ± 0.27 |
|
| ||||
| Government service | 0.07 ± 0.25 | 0.16 ± 1.01 | 0.18 ± 0.59 | 0.02 ± 0.21 |
|
| ||||
| Legal advice | 0.22 ± 0.46 | 0.36 ± 0.80a | 0.37 ± 0.76 | 0.14 ± 0.45a |
|
| ||||
| Internet | 2.36 ± 6.08 | 2.52 ± 5.96 | 2.01 ± 6.13 | 1.48 ± 4.60 |
|
| ||||
| Transportation | 0.05 ± 0.40 | 0.20 ± 1.95 | 0.03 ± 0.23 | 0.19 ± 1.13 |
|
| ||||
| Spiritual counseling | 0.46 ± 1.21 | 1.49 ± 4.45 | 0.50 ± 1.63 | 0.59 ± 1.45 |
|
| ||||
| Resource packet | 0.37 ± 2.97 | 1.55 ± 2.48 | 0.05 ± 0.27 | 1.41 ± 2.69 |
|
| ||||
| Respite care | 0.09 ± 0.50 | 0.87 ± 4.46 | 0.24 ± 1.09 | 0.47 ± 2.56 |
|
| ||||
| Food delivery | 0.22 ± 1.96 | 0.28 ± 2.10 | 0.04 ± 0.20 | 0.21 ± 1.48 |
|
| ||||
| Care recipient | ||||
|
| ||||
| Total | 2.71 ± 5.76 | 6.79 ± 13.72 | 2.74 ± 7.22 | 5.11 ± 10.68 |
|
| ||||
| Support group | 0.02 ± 0.20 | 0.00 ± 0.00 | 0.06 ± 0.25 | 0.03 ± 0.23 |
|
| ||||
| Alzheimer’s Association | 0.02 ± 0.14 | 0.04 ± 0.39 | 0.06 ± 0.29 | 0.04 ± 0.41 |
|
| ||||
| Department of Elderly Affairs | 0.03 ± 0.22 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 |
|
| ||||
| Government service | 0.02 ± 0.20 | 0.00 ± 0.00 | 0.04 ± 0.20 | 0.00 ± 0.00 |
|
| ||||
| Legal advice | 0.07 ± 0.25 | 0.07 ± 0.29 | 0.13 ± 0.42 | 0.02 ± 0.15 |
|
| ||||
| Internet | 0.06 ± 0.36 | 0.05 ± 0.49 | 0.06 ± 0.52 | 0.00 ± 0.00 |
|
| ||||
| Transportation | 1.39 ± 4.51 | 2.36 ± 8.04 | 1.16 ± 4.60 | 2.22 ± 5.76 |
|
| ||||
| Spiritual counseling | 0.22 ± 0.84 | 0.88 ± 4.22 | 0.32 ± 1.16 | 0.38 ± 1.27 |
|
| ||||
| Resource packet | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.01 ± 0.10 | 0.00 ± 0.00 |
|
| ||||
| Respite care | 0.54 ± 2.54 | 0.89 ± 3.89 | 0.61 ± 2.15 | 0.32 ± 2.22 |
|
| ||||
| Food delivery | 0.35 ± 2.43 | 0.87 ± 4.18 | 0.29 ± 2.58 | 0.43 ± 2.52 |
Values presented are the mean number of times per month each service was used.
Significant group differences in service use.
At 6 months, greater caregiver community resource use was significantly associated with more-frequent problem behaviors (r = 0.26, P = .01) and worse caregiver reaction to problem behaviors (r = 0.21, P = .04) in FITT-C; there was no such pattern for TS. Depressive symptoms and caregiver burden were not related to caregiver use of community support services at 6 months.
Care Recipients
At baseline, there were no differences in community support service use between care recipients in FITT-C and TS (t(177.66) = −0.33, P = .97). The most commonly used services at baseline were transportation (11.1%), spiritual services (9.5%), respite services (9.0%), and legal services (8.5%). At end of treatment, there were no differences between groups for care recipient use of community resources (t(197) = 0.96, P = .34).
Healthcare Resource Use
Caregivers
At baseline, there were no differences between caregivers in FITT-C and TS for doctor visits (t(140.24) = −1.24, P = .22), hospital stays (t(131.80) = 1.22, P = .23), or ED visits (t(144.68) = 1.04, P = .30).
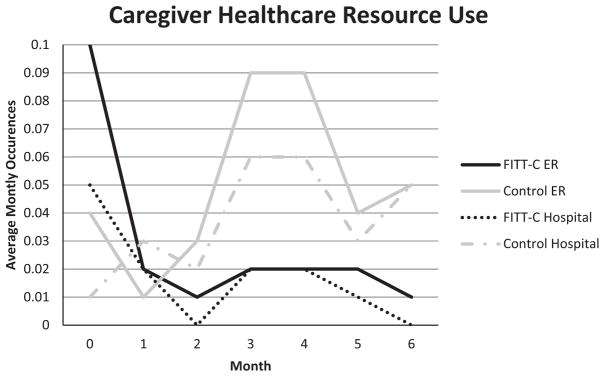
FITT-C caregivers had fewer average monthly hospital stays (0.01 ± 0.04 over the 6 months of the intervention) than TS caregivers (0.04 ± 0.10) (t(122.81) = −2.69, P = .006). FITT-C caregivers also had fewer average monthly ED visits (0.02 ± 0.06) than TS caregivers (0.05 ± 0.13) (t(122.96) = −2.45, P = .02) (Figure 1). There were no between-group differences in average monthly doctor visits (t(197) = 0.16, P = .88).
Figure 1.
Caregiver healthcare resource use from baseline and months 1–6 of follow-up: average monthly healthcare resource use (hospitalizations, emergency department visits) at baseline (labeled 0; month before start of treatment) and months 1–6 of treatment. Each data point represents the number of instances in that month averaged across participants in the group.
Caregivers who received the intervention had fewer hospital admissions (absolute risk reduction = 11.4%, 95% confidence interval (CI) = 0.023–0.25, P = .01) and fewer ED visits (absolute risk reduction = 9.5%, 95% CI = 0.01–0.19, P = .048) than those who received TS.
Predictors of Healthcare Resource Use
At baseline, none of the caregiver healthcare resource use variables was associated with caregiver demographic factors, caregiver burden, depression, or problem behavior frequency or caregiver reaction scores. Older age was associated with more doctor visits regardless of treatment group (r = 0.16, P = .02).
Follow-up analyses were conducted to examine whether changes in depression, burden, and caregiver reaction to problem behaviors were related to healthcare resource use. In the entire sample, decrease in depression over the intervention was associated with fewer hospitalizations at 6 months (r = 0.18, P = .02). A decrease in caregiver burden over the intervention was associated with fewer ED visits at 6 months (r = 0.17, P = .02). Less-negative caregiver reaction to problem behaviors was associated with fewer ED visits (r = 0.16, P = .03) and hospitalizations (r = 0.17, P = .02) at 6 months.
When examining the two groups separately, a reduction in depression predicted fewer ED visits (r = 0.23, P = .03) and hospitalizations (r = 0.23, P = .03) at 6 months in TS, and a reduction in burden predicted fewer ED visits at 6 months (r = 0.21, P = .04) in FITT-C.
Care Recipients
At baseline, there were no between-group differences for care recipients in ED visits (t(197) = −0.45, P = .65) or doctor visits (t(197) = 0.83, P = .41). There were also no group differences over the 6-month intervention in monthly ED visits (t(197) = ;0.22, P = .83) or monthly doctor visits (t(193.22) = 0.16, P = .88). Having more average monthly doctor visits was associated with older age (r = 0.35, P < .001).
Out-of-Pocket Costs
At baseline, caregivers had spent an average of $190.88 ± 534.21 out of pocket on formal care for the care recipient in the preceding month, with no group differences (P(179.67) = 1.89, P = .06). At 6 months, caregivers had spent an average of $274.43 ± 901.68 out of pocket on formal care for the care recipient in the preceding month, also with no between-group differences (t(197) = −0.34, P = .73. There were no group differences for total out-of-pocket costs during the intervention between groups (t(176) = −0.07, P = .92), although 14 FITT-C participants and seven TS participants were excluded because of missing data, which precluded examination of their total out-of-pocket costs. In the entire sample, the average 6-month total out-of-pocket cost was $1,312.08 ± 3,738.20.
Nursing Home Placement
Twelve (6.0%) participants were placed in a nursing home during the study, with no group differences in rate of placement (χ2 (n = 199) = .16, P = .70).
DISCUSSION
An entirely telephone-delivered psychosocial intervention (FITT-C) resulted in dementia caregivers using community support services more and healthcare resources less than those in an active control condition. Caregivers who received the FITT-C had 9.5% fewer ED visits and 11.4% fewer hospital stays than caregivers receiving TS.
FITT-C caregivers used more community support services than TS caregivers by the end of the intervention. Most frequently used services were Alzheimer’s Association contact and legal services. For FITT-C caregivers, greater use of resources was associated with more-frequent care recipient problem behaviors and greater caregiver reaction scores. These relationships suggest that individuals with the highest levels of distress in the FITT-C group were most likely to seek out community support. There were no significant relationships found for those receiving TS.
Few studies have addressed the effect of a dementia caregiver intervention on community support use, despite considerable evidence that dementia caregivers are reluctant to use these services. A previous study found that a consumer-driven care coordination intervention resulted in greater use of support services by dementia caregivers and care recipients.25 Although the FITT-C intervention involved problem-solving and encouragement to engage in community support, study therapists did not provide any care coordination or make any arrangements for caregivers. Both caregiver groups received resource packets containing information about support services, suggesting that provision of education alone may not be enough to bring about behavior change. Rather, it may be the combination of education and a directive approach that affects resource use.
Although the use of community support services of caregivers who received the intervention increased significantly, the overall rate of service use was low. Therefore, it may be important to enhance the FITT-C with motivational interviewing or other health coaching techniques. Because there are numerous community supports available to dementia caregivers, it may be particularly cost effective to link psychosocial interventions and community support programs. There is evidence that collaboration between primary care providers and local chapters of the Alzheimer’s Association delays nursing home placement.26
Results showing that FITT-C caregivers had fewer hospitalizations and ED visits are consistent with reports of improved perceived health after psychosocial caregiver interventions.15 Although data to examine the costs associated with healthcare use were not available, these findings may represent cost savings, particularly given high costs associated with ED use. Other than delaying nursing home placement, no studies have examined the effect of a caregiver psychosocial intervention on healthcare use. The FITT-C intervention has been shown to reduce depression in dementia caregivers.19 The present study found that improvement in depressive symptoms was associated with fewer ED visits of caregivers who received the FITT-C. There was an association between more ED visits and higher burden in caregivers receiving TS. These findings suggest that depression and burden are important targets for caregiver interventions designed to reduce healthcare use and health expenditures, but the current study did not have enough statistical power to address whether changes in primary outcomes (depression and burden) mediated healthcare use. Future research should explore this.
There were no group differences in average monthly doctor visits for caregivers. The strongest predictor of doctor visits for caregivers was age, which makes sense given the relationship between age and medical burden. There were no group differences for any of the outcomes for care recipients. This is not entirely unexpected given that care recipients were not the direct target of the intervention. With longer follow-up, indirect effects of the intervention might become apparent. No difference was found between the interventions in nursing home placement, although few participants were placed during the intervention, and follow-up was short, at only 6 months. Finally, the analysis did not reveal any differences between the intervention groups in out-of-pocket costs. It was not possible to differentiate healthcare-related costs and support services costs, so a cost-benefit analysis could not be conducted. Future studies could examine whether any costs of support services justify the emotional or burden-related benefit to dementia caregivers.
Overall findings from this analysis provide additional evidence of the efficacy of the FITT-C intervention. Next steps involve testing the intervention in a community effectiveness trial, which will better reflect real-world conditions. It is anticipated that this trial will assess training and supervision of community therapists, intervention uptake, and cost-benefit analysis. The FITT-C is envisioned as a potentially cost-effective, accessible intervention that community or state agencies could deliver.
Because this was a secondary data analysis, the study was not powered for outcome variables presented in this study. Although this is not a concern for variables that were found to be significant, it is possible that the study lacked power to detect group differences in out-of-pocket costs and nursing home placement. Another limitation of this study is the lack of racial diversity, which limits the generalizability of findings. There is evidence that different racial groups respond to caregiver interventions and may interact with community resources and healthcare services differently.13 It is anticipated that community implementation of FITT-C would yield more information about responses in diverse populations. The 6-month follow-up was short, so it is unknown whether the intervention had lasting effects. Finally, caregiver health was not measured at baseline, so it is unknown whether there were any baseline differences between the groups.
Overall, a telephone-based psychosocial intervention increased caregiver use of community support services and decreased caregiver use of hospital-based services.
Supplementary Material
Table 2.
Emergency Visits, Hospitalizations, and Doctor Visits for Caregivers and Care Recipients
| Visits | Family Intervention: Telephone Tracking—Caregiver, n = 105 | Telephone Support, n = 94 | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Baseline | 1 to 6 Months | Total, n | ≥1 Occurrences, % | Baseline | 1 to 6 Months | Total, n | ≥1 Occurrences, % | |
|
|
|
|||||||
| Mean±SD | Mean±SD | |||||||
| Caregiver | ||||||||
|
| ||||||||
| ED | 0.10 ± 0.47 | 0.02 ± 0.06a | 10 | 8.6 | 0.04 ± 0.20 | 0.05 ± 0.13a | 29 | 18.1 |
|
| ||||||||
| Hospital | 0.05 ± 0.29 | 0.01 ± 0.04a | 7 | 6.7 | 0.01 ± 0.10 | 0.04 ± 0.10a | 24 | 18.1 |
|
| ||||||||
| Doctor | 1.23 ± 1.64 | 0.85 ± 0.89 | 524 | 83.8 | 1.66 ± 3.00 | 0.71 ± 0.61 | 407 | 88.3 |
|
| ||||||||
| Care recipient | ||||||||
|
| ||||||||
| ED | 0.10 ± 0.33 | 0.08 ± 0.16 | 46 | 26.7 | 0.12 ± 0.35 | 0.08 ± 0.17 | 44 | 26.6 |
|
| ||||||||
| Doctor | 2.85 ± 4.67 | 1.32 ± 1.35 | 819 | 96.2 | 2.37 ± 3.16 | 1.30 ± 1.05 | 720 | 96.8 |
Baseline scores reflect the month before the intervention; 1- to 6-month scores reflect average monthly visits.
Significant group differences.
SD = standard deviation; ED = emergency department.
Acknowledgments
We acknowledge our talented group of study therapists: Cynthia Banna, Deborah D’Andrea, Crystelle Egan, Melinda Matuza, Margaret Trippel, and Isabel Trombetti. We would also like to thank Michael Alosco, Kristi Emerson, Suzanne Foster-Sanda, Debbie Javorsky, Gary Epstein-Lubow, Kelley O’Connor, Colleen Slavin, and Beth Springate for their many contributions to the study. Finally, the study would not have been possible without the participants, who offered their time and were willing to share their caregiving experiences.
Financial Disclosure: This research was supported by Grant NR010559 from the National Institute of Nursing Research. This trial was registered with clinicaltrials.gov (NCT00735800).
Conflict of Interest: Dr. Tremont serves on the advisory board for the Nordic Technology Group. Dr. Ott has received research support from Eli Lilly, Avid, Merck, TauRx, Roche, and Long Term Care Group and speaking honoraria and travel expenses from the National Highway Transportation Safety Administration and Medscape. He serves on the Data Safety Monitoring Board for Accera. Dr. Papandonatos has served as consultant for Long Term Care Group.
Author Contributions: GT: Study concept and design, acquisition of subjects and data, analysis and interpretation of data, preparation of manuscript. JD: Study concept and design, interpretation of data, preparation of manuscript. BRO: Study concept and design, acquisition of subjects and data, analysis, preparation of manuscript. RG: Analysis and interpretation of data, preparation of manuscript. CC: Analysis and interpretation of data, preparation of manuscript. GP: Study concept and design, analysis and interpretation of data, preparation of manuscript. RHF, PG, DB: Study concept and design, preparation of manuscript.
Sponsor’s Role: The National Institute of Nursing Research provided funds for this research but had no role in the conduct of the study, analyses, or production of the manuscript.
Footnotes
Portions of this manuscript were presented at the 2014 meeting of the Alzheimer’s Association International Conference, Copenhagen, Denmark.
Additional Supporting Information may be found in the online version of this article:
Appendix S1. Questionnaire.
Please note: Wiley-Blackwell is not responsible for the content, accuracy, errors, or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.Fonareva I, Oken BS. Physiological and functional consequences of caregiving for relatives with dementia. Int Psychogeriatr. 2014;26:725–747. doi: 10.1017/S1041610214000039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferrara M, Langiano E, Di Brango T, et al. Prevalence of stress, anxiety and depression in with Alzheimer caregivers. Health Qual Life Outcomes. 2008;6:93. doi: 10.1186/1477-7525-6-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brodaty H, Donkin M. Family caregivers of people with dementia. Dialogues Clin Neurosci. 2009;11:217–228. doi: 10.31887/DCNS.2009.11.2/hbrodaty. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fazio PD, Ciambrone P, Cerminara G, et al. Depressive symptoms in caregivers of patients with dementia: Demographic variables and burden. Clin Interv Aging. 2015;10:1085–1090. doi: 10.2147/CIA.S74439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raccichini A, Castellani S, Civerchia P, et al. The caregiver’s burden of Alzheimer patients: Differences between live-in and non-live-in. Am J Alzheimers Dis Other Demen. 2009;24:377–383. doi: 10.1177/1533317509340025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robinson K, Buckwalter K, Reed D. Differences between dementia caregivers who are users and nonusers of community services. Public Health Nurs. 2013;30:501–510. doi: 10.1111/phn.12041. [DOI] [PubMed] [Google Scholar]
- 7.Brodaty H, Thomson C, Thompson C, et al. Why caregivers of people with dementia and memory loss don’t use services. Int J Geriatr Psychiatry. 2005;20:537–546. doi: 10.1002/gps.1322. [DOI] [PubMed] [Google Scholar]
- 8.Gaugler JE, Kane RL, Kane RA, et al. Early community-based service utilization and its effects on institutionalization in dementia caregiving. Gerontologist. 2005;45:177–185. doi: 10.1093/geront/45.2.177. [DOI] [PubMed] [Google Scholar]
- 9.Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 10.Schubert CC, Boustani M, Callahan CM, et al. Acute care utilization by dementia caregivers within urban primary care practices. J Gen Intern Med. 2008;23:1736–1740. doi: 10.1007/s11606-008-0711-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suehs BT, Shah SN, Davis CD, et al. Household members of persons with Alzheimer’s disease: Health conditions, healthcare resources use, and healthcare costs. J Am Geriatr Soc. 2014;63:435–441. doi: 10.1111/jgs.12694. [DOI] [PubMed] [Google Scholar]
- 12.Zhu CW, Scarmeas N, Ornstein K, et al. Health-care use and cost in dementia caregivers: Longitudinal results from the predictors caregiver study. Alzheimers Dement. 2015;11:444–454. doi: 10.1016/j.jalz.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Belle SH, Burgio L, Burns R, et al. Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: A randomized, controlled trial. Ann Intern Med. 2006;145:727–738. doi: 10.7326/0003-4819-145-10-200611210-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mittelman MS, Haley WE, Clay OJ, et al. Improving caregiver well-being delays nursing home placement of patients with Alzheimer disease. Neurology. 2006;67:1592–1599. doi: 10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]
- 15.Basu R, Hochhalter AK, Stevens AB. The impact of the REACH II intervention on caregivers’ perceived health. J Appl Gerontol. 2015;35:590. doi: 10.1177/0733464813499640. [DOI] [PubMed] [Google Scholar]
- 16.Shelton P, Schraeder C, Dworak D, et al. Caregivers’ utilization of health services: Results from the Medicare Alzheimer’s disease demonstration, Illinois site. J Am Geriatr Soc. 2001;49:1600–1605. [PubMed] [Google Scholar]
- 17.Tremont G, Davis JD, Bishop DS, et al. Telephone-delivered psychosocial intervention reduces burden in dementia caregivers. Dementia. 2008;7:503–520. doi: 10.1177/1471301208096632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tremont G, Davis JD, Papandonatos GD, et al. Psychosocial telephone intervention for dementia caregivers: A randomized, controlled trial. Alzheimers Dement. 2015;11:541–548. doi: 10.1016/j.jalz.2014.05.1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tremont G, Davis J, Papandonatos G, et al. A telephone intervention for dementia caregivers: Background, design, and baseline characteristics. Contemp Clin Trials. 2013;36:338–347. doi: 10.1016/j.cct.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morris JC. Clinical Dementia Rating Scale (CDR): Current version and scoring rules. Neurology. 1993;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 21.Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive behavioral therapy in the treatment of generalized anxiety disorder. J Consult Clin Psych. 1993;61:611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- 22.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 23.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 24.Teri L, Logsdon R, Uomoto J, et al. Assessment of behavior problems in dementia: The revised memory and behavior problems checklist. Psychol Aging. 1992;7:622–631. doi: 10.1037//0882-7974.7.4.622. [DOI] [PubMed] [Google Scholar]
- 25.Bass DM, Judge KS, Snow AL, et al. Caregiver outcomes of partners in dementia care: Effect of a care coordination program for veterans with dementia and their family members and friends. J Am Geriatr Soc. 2013;61:1377–1386. doi: 10.1111/jgs.12362. [DOI] [PubMed] [Google Scholar]
- 26.Fortinsky RH, Kulldorff M, Kleppinger A, et al. Dementia care consultation for family caregivers: Collaborative model linking an Alzheimer’s association chapter with primary care physicians. Aging Ment Health. 2009;13:162–170. doi: 10.1080/13607860902746160. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.