Abstract
The multidrug-resistance-1 (MDR1) gene encodes an ATP-dependent efflux transporter that is highly expressed in the colon. In mice, loss of MDR1 function results in colitis with similarities to human inflammatory bowel diseases (IBD). Here, we show that MDR1 has an unexpected protective role for the mitochondria where MDR1-deficiency results in mitochondrial dysfunction with increased mitochondrial ROS (mROS) driving the development of colitis. Exogenous induction of mROS accelerates, whilst inhibition attenuates colitis in vivo; these effects are amplified in MDR1-deficiency. In human IBD, MDR1 is negatively correlated to SOD2 gene expression required for mROS detoxification. To provide direct evidential support, we deleted intestinal SOD2 gene in mice and showed an increased susceptibility to colitis. We exploited the GWA datasets and found many (~5%) of IBD susceptibility genes with direct roles in regulating mitochondria homeostasis. As MDR1 primarily protects against xenotoxins via its efflux function, our findings implicate a distinct mitochondrial toxin + genetic susceptibility interaction leading to mitochondrial dysfunction, a novel pathogenic mechanism that could offer many new therapeutic opportunities for IBD.
Introduction
Inflammatory bowel diseases (IBD) are complex immune-mediated conditions that can be subclassified into the clinically distinct entities of Crohn’s disease (CD) and ulcerative colitis (UC) 1,2. Both are debilitating relapsing inflammatory conditions, which affect an estimated 4 million people in the United States and Europe with increasing prevalence in the developing world 3. CD is characterised by discontinuous aphthous mucosal ulcerations and inflammation occurring most commonly in the distal small intestine (ileum) and variably across the intestinal tract2. UC affects only the large bowel (colon) in a confluent manner and is characterised by superficial mucosal inflammation4. Increasingly evident both in clinical and molecular studies is the concept that IBD involves multiple distinct and also, common pathogenic mechanisms. The powerful genomewide association (GWA) studies implicate more than 200 genetic susceptibility loci including genes in biological pathways regulating innate (e.g. NOD2 and autophagy) and adaptive (e.g. Th17, MHC) immune responses, cytokine production, lymphocyte activation and bacterial response5,6.
One major mechanistic theme that is shared between UC and CD is the role of intestinal epithelial dysfunction and injury7. The intestinal epithelium is uniquely in contact with high concentrations of bacteria with their metabolic products, immune-active ligands, damage-associated molecular products (DAMPs), xenobiotics and environmental toxins8. Thus, a central component of IBD pathogenesis is the deregulation of protective mechanisms that maintain cellular homeostasis and resultant epithelial dysfunction. MDR1 is a key mediator of one such mechanism9 by actively extruding more than 4000 diverse products, including xenotoxins, out of the intracellular environment10. MDR1 belongs to the ATP-binding cassette, ABC-transporter family of transmembrane transporters. These proteins bind ATP and use the energy to drive the transport of various molecules across all cell membranes. Genetic variations in this family of genes contribute to several human disorders including cystic fibrosis, neurological diseases, retinal degeneration, anaemia, cholesterol and bile transport defects9.
Epithelial cells of the distal intestinal tract have very high MDR1 expression reflecting the importance of its cytoprotective role at the gut luminal interface 11. In the mouse, the mdr1a gene encodes PgP170. Constitutive genetic deletion of this gene results in chronic spontaneous colitis as the mutants age with ~50% penetrance when >6 months of age12. Interestingly, the mdr1a-deficient mice display no other spontaneous clinical phenotype, underlining the dominant physiologic role of mdr1a in the gut. Its importance in colonocytes is further highlighted by the lack of rescue from colitis when mdr1a-deficient mouse were reconstituted with mdr1a+ bone marrow stem cells12. In human IBD, several studies have shown a downregulation of intestinal MDR1 expression13,14. MDR1 has been linked to IBD in early human candidate genetic studies with disease-associated variants associated with low MDR1 expression15. These findings implicate the loss of MDR1 function as a contributory factor in the pathogenesis of IBD.
Although an underlying increase in intestinal permeability is considered as the dominant factor for the development of mdr1a-deficient colitis, the preceding steps leading to this late stage are not fully clarified16. In this study, we show for the first time that MDR1 confers a protective role to the gut epithelial mitochondria and that MDR1 deficiency results in mitochondrial dysfunction driving the development of colitis. The mitochondria play a key role in many physiologic processes such as energy production, regulation of cell death and immune response. Given that MDR1 is critically positioned at the interface between mitochondria and the luminal environment, this protective mechanism opens up a fresh perspective in how deregulation of mitochondria homeostasis influences the development of colitis.
Results
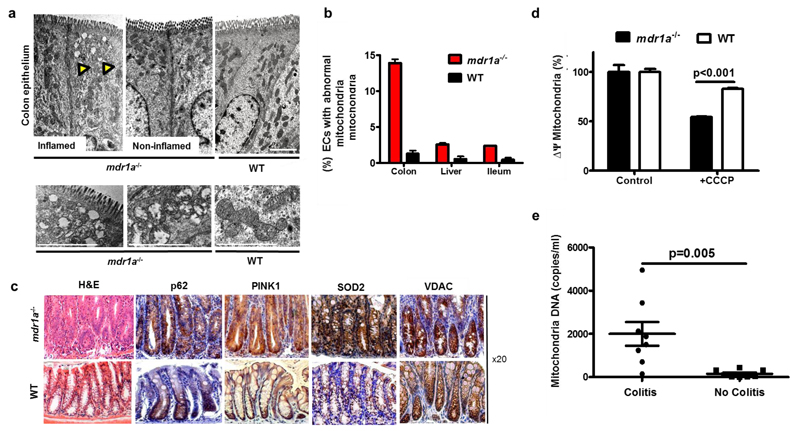
Mdr1a-deficient colonic epithelium shows an accumulation of damaged mitochondria
Using transmission electron microscopy, we showed that the mdr1a-deficient mice displayed a preferential accumulation of damaged and degenerating mitochondria in colonic epithelial cells (CECs) in the inflamed colon (Fig 1a). CECs harbouring these mitochondrial abnormalities were found in higher frequencies in mdr1a-deficient mice compared to non-inflamed colon, ileum and liver in wild type (WT) mice (14% vs. <2% overall frequency) (Figs 1b and S1a). These features were not present in il10-deficient mice CECs, a spontaneous chronic colitis control group with a defined inflammatory mechanism17 (Fig S1b) and only in necrotic CECs during acute dextran-sulphate sodium colitis (DSS). Immunohistochemistry analysis of mdr1a-deficient colons revealed increased colonic epithelial p62, PTEN-induced kinase 1 (PINK1) and superoxide dismutase-2 (SOD2) staining (Fig 1c). p62 is a ubiquitin-binding protein that promotes autophagic degradation of protein aggregates recognises damaged mitochondria and recruits them to the isolation membrane through its interaction with LC318. PINK1 is involved in specific autophagic clearance of damaged mitochondria (or mitophagy) 19; whereas SOD2 plays a role in detoxifying mitochondrial reactive oxygen species (ROS). Furthermore, isolated CECs confirmed higher p62, increased microtubule-associated protein 1 light chain 3-β, LC3-I to phosphatidylethanolamine (PE)-conjugated or LC3-II ratio indicative of heightened autophagy; and parkin expression in mdr1a-deficiency (Fig S2a). Parkin translocates to mitochondria upon dissipation of mitochondria membrane potential and cooperates with PINK1 during mitophagy. CEC voltage-dependent anion channel (VDAC) expression and mitochondria DNA were similar to WT, suggesting that these changes were not due to changes in mitochondria content (Figs 1c and S2b). Mitochondria isolated from mdr1a-deficient CECs were more sensitive to mitochondrial membrane damage by carbonyl cyanide m-chorophenyl hyrdrazone, CCCP, a known damaging agent (Fig 1d). Furthermore, we detected increased circulating plasma mitochondrial DNA, a known inflammatory DAMP in mdr1a-deficient mice with colitis (Fig 1e). The mdr1a-deficient colons have increased epithelial cell turnover and death respectively (Figs S2c, d). MDR1-deficient mice exhibited clear evidence of colonic epithelial mitochondrial damage with increased epithelial dysfunction and cell-death.
Figure 1. Damaged mitochondria accumulate within mdr1a-deficient colonic epithelium:
(a) Representative TEM (n=6 per group) of colonic epithelium. Scale bar 2µm. Yellow arrows denoting damaged mitochondria. (b) Quantitative analyses of CEC containing damaged mitochondria (n=6/group). (c) Representative H&E and immunohistochemistry of colon (p62, PINK-1, SOD2 and VDAC) (n=6/group). (d) Loss of mitochondria membrane potential, JC-1 fluorescence in isolated mitochondria (n=6/group) (e) Plasma qPCR of mitochondrial DNA mdr1a-/- mice with colitis vs. no colitis (n=8/group). WT – wild-type. All data represent mean± SEM.
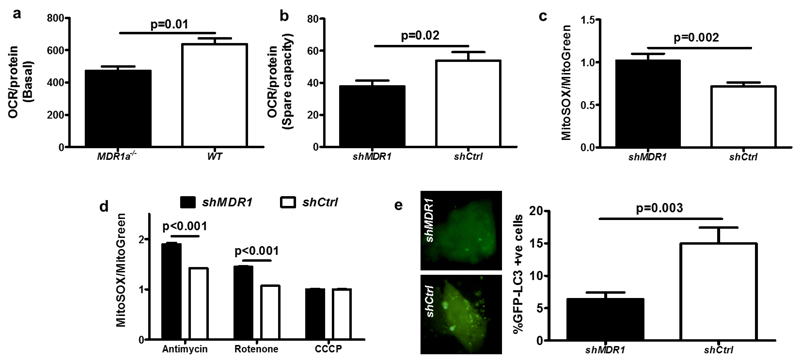
MDR1 deficiency results in mitochondria dysfunction
To study the functional consequence of MDR1 deficiency on the mitochondria, we investigated the cellular energetics of primary colonic explants of mdr1a-/- and WT mice. We found lower basal O2 consumption rate (OCR) in mdr1a-/- colon consistent with impaired mitochondrial function and energy production (Figs 2a). We further knocked down MDR1 expression in vitro by transducing short hairpin MDR1 (shMDR1) in the human T84 CEC cell line (Figs S3a). Although we found no differences in OCR (Figs S3b), MDR1 deficiency in T84 CECs resulted in lower spare respiratory capacity (SRC) (Fig 2b). SRC is the extra mitochondrial capacity available in a cell to produce energy under conditions of increased work and stress and is thought to be important for long-term cell survival and function 20. Dysfunctional or damaged mitochondria produce increased levels of ROS and the mitochondria are the major source of ROS for most cells21. In line with our observations in mdr1a-deficient mouse CECs, we found increased levels of mROS in shMDR1 T84 CECs at baseline (Fig 2c); and following artificial induction with rotenone and antimycin by fluorescence of MitoSOX (a mitochondrial superoxide indicator) (Fig 2d). Furthermore, we showed that MDR1-knockdown resulted in higher p62 and SOD2 protein expressions following rotenone treatment in shMDR1 CECs (Fig S3c). We transfected LC3-GFP and found reduced autophagy (Fig 2e); and LC3-II protein after inhibition of its degradation by bafilomycin (Fig S3d) in shMDR1 relative to shCtrl CECs. This suggests a depressed clearance that compounds mitochondria dysfunction. Degenerating mitochondria in CECs are notably present in mice models with primary autophagy (Irgm and Atg16l1)22,23, secondary autophagy impairments due to defective ER-stress 24 and NLRP6 inflammasome activity 25. Our data collectively show that loss of MDR1 results in mitochondria dysfunction with impaired bioenergetics, increased mROS production and perturbed autophagic clearance.
Figure 2. MDR1 deficiency results in mitochondria dysfunction:
(a) Oxygen consumption rate, OCR (pmol/minute) in primary colonic explant in mdr1a-deficient vs. WT respectively (n=4). (b) Spare respiratory capacity (SRC) of T84 shMDRI and shCtrl (5 replicates). (c) Normalised MitoSOX/Mitotracker Green fluorescence T84 shMDR1 vs. shCtrl, (n=11/group, representative of 3 independent experiments. (d) Relative MitoSOX/Mitotracker Green fluorescence to respective untreated group in T84 shMDR1 vs. shCtrl (n=8/treatment group, representative of 3 independent experiments). (e) Quantification of GFP-LC3 shMDR1 vs. shCtrl (n=12 slides/group). %GFP-LC3+ve cells/number of cells in 10 fields (X40 microscopy). All data represent mean± SEM.
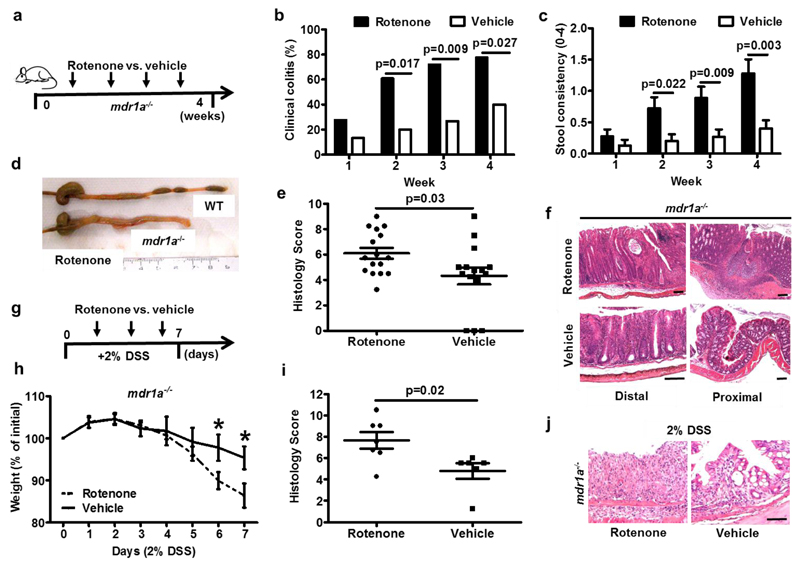
Experimental induction of colonic mitochondria ROS influences the development of colitis in MDR1a-deficiency
We then sought to investigate if induction of mROS can accelerate the development of colitis in mdr1a-deficiency. We developed an in vivo protocol to test this further by directly administrating rotenone with low dose DSS (0.25%) into the colon of mdr1a-deficient and WT mice. We chose rotenone to specifically focus on the effects of mROS and to test its early effects prior to full induction of DSS colitis. Rotenone is primarily an inhibitor of mitochondrial complex I of electron transport chain which results in increase mROS production and at higher doses, cellular bioenergetic deficit26. Rotenone is a well-described triggering factor for rodent models of Parkinson’s disease and is administered systemically (by injection) and/or orally27. Given that direct colonic administration in vivo is a new approach, we titrated the colonic rotenone concentration to 100μM (equating to ~1mg/kg) without systemic ill effects, notably respiratory, neurological and motor deficits (Fig S4a). Drug dosing data derived from rodent rotenone-induced Parkinson’s disease ranged between 2.5-15mg/kg systemically to 0.25-100mg/kg orally26 with increased mortality is observed in the former approach. Within 24 hours of 100µM rotenone administration, we found that this is sufficient to trigger increased leukocyte infiltration and colitis in mdr1a-deficient mice, which are not present in WT mice (Figs S4b, c) associated with increased CEC death in mdr1a-deficient colon (Figs S4d, e). We expanded our protocol where we directly administered 500µl of 100µM of rotenone 3 times/week over 4 weeks in the absence of DSS (Fig 3a). In mdr1a-deficient mice with no prior evidence of colitis, we found that this accelerated the onset of colitis compared to vehicle (Fig 3b, c). In mdr1a-deficiency, rotenone-treated mice have more severe colitis compared to the vehicle group (Fig 3d-f). Isolated CECs from rotenone-treated mdr1a-deficient mice have higher pro-inflammatory il6 and tnf-α gene expressions (Fig S4f). In addition to triggering spontaneous colitis, exogenous induction of mucosal mROS using rectal rotenone treatment (Fig 3g) rendered the mdr1a-deficient mice more susceptible to acute DSS colitis exhibiting more severe clinical and histologic evidence of inflammation (Fig 3h-j). To investigate the effects of rotenone on the epithelial barrier, we further showed that shMDR1 compared to shCtrl CECs have an increased sensitivity to rotenone, CCCP and cisplatin-induced cell death (Figs S5a, b) and displayed an increased loss of barrier function as measured by transepithelial electric resistance following culture with rotenone (Fig S5c). In line with our in vivo data, we also showed that mROS-induced by rotenone triggered increased colonic epithelial IL-8 production induced by flagellin and bacterial CpG (these ligands chosen as our T84 CECs express TLR5 and TLR9) (Fig S6d), indicating that mROS triggers CEC-death and innate inflammatory responses. Collectively, these data suggest that abnormal mucosal mROS driven by an exogenous trigger can influence the onset and severity of colitis in a genetically susceptible host, in this respect, MDR1-deficiency.
Figure 3. Experimental induction of mROS accelerates spontaneous colitis in mdr1a-deficiency and in acute DSS-colitis:
(a) Experimental protocol of 4-week colonic administration of rotenone vs. vehicle (3x/week). (b) Prevalence of clinical colitis in rotenone vs. vehicle treated mdr1a-/- at weekly intervals (n=18 and 15 mice treated with rotenone and vehicle respectively). (c) Stool consistency measurements in rotenone vs. vehicle treated mdr1a-/- at weekly intervals. (d) Representative images of mdr1a-/- and WT whole colons treated with colonic rotenone. (e) Histology scores of rotenone vs. vehicle treated mdr1a-/- colons. (f) Representative H&E distal and proximal colons; and histology scores of rotenone vs. vehicle treated mdr1a-/-, black scale bars 100 µm. (g) Experimental protocol of colonic rotenone vs. vehicle – 3 times during 7-day 2% DSS in drinking water. (h) Daily percentage of change from initial weight in rotenone vs. vehicle treated mdr1a-/- acute DSS colitis (n=7/group). (i, j) Representative histology scores and H&E colons of rotenone vs. vehicle treated mdr1a-/- (n=7/group) in acute DSS colitis, black scale bar 50µm. All data represent mean± SEM.
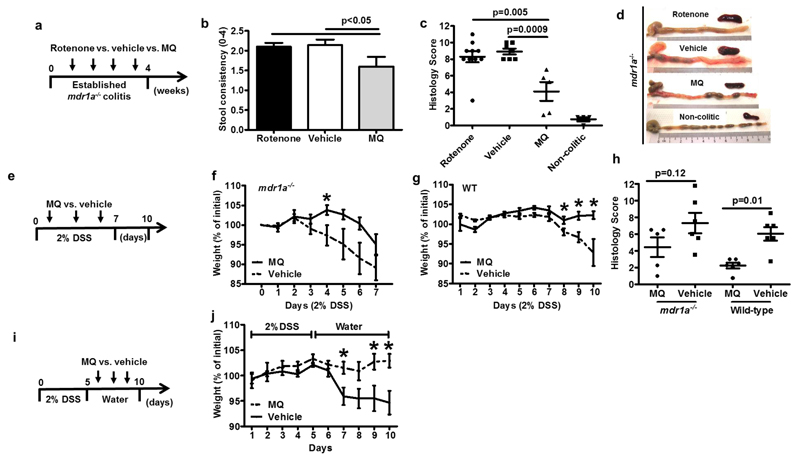
Inhibition of mitochondria ROS effects attenuates and promotes recovery from colitis in vivo
Next we investigated whether inhibiting the effects of mROS can prevent or attenuate the development of colitis. Mitoquinone (MitoQ) is a mitochondrial specific antioxidant with coenzymeQ10 covalently attached to a triphenylphosphonium molecule, which selectively accumulates within the mitochondria. MitoQ protects the mitochondria membrane from mROS-induced lipid peroxidation and acts as a ROS-scavenger28. We first investigated the effect of mROS inhibition in mdr1a-deficient chronic colitis. Here, we tested the effects of colonic MitoQ (10µM), rotenone and vehicle only in mdr1a-deficient mice with clinical evidence of chronic colitis (10-12 weeks old, all with chronic diarrhoea) (Fig 4a). Colonic MitoQ improved colitis in mdr1a-deficient mice (Figs 4b-d, S6a). In contrast to earlier data from mdr1a-deficient mice with no colitis, rotenone surprisingly, did not further exacerbate chronic colitis. We think this may be due to the intrinsic nature of mdr1a-deficient colitis model where the main driving factor is increased barrier permeability. Hence, colonic mitochondrial dysfunction in this setting acted as a triggering factor and once barrier function was compromised resulting in colitis, rotenone has a lesser role to worsen colitis in this model. Here, the histologic severity scores in both rotenone and control groups were 8 and 9.5 respectively out of the maximal score 12. The high baseline made it difficult to test for an exacerbating role for rotenone. In acute DSS-colitis, colonic MitoQ delayed the onset in mdr1a-deficient mice (Fig 4f) and significantly attenuated colitis in WT mice (Figs 4g, S6b). In both settings, there were histologic improvements in the severity of colitis (Fig 4h). We also showed that MitoQ improved clinical recovery following 5 days of DSS challenge (Figs 4i, S6c). In this setting, we tested only WT mice, as mdr1a-deficient mice were too unwell after DSS-induction. Two recent studies corroborate the protective effects of MitoQ in acute DSS colitis (although via oral route) 29,30. Inhibiting the effects of mROS is therefore beneficial in acute and chronic colitis as well as during the recovering phase of colitis.
Figure 4. Inhibition of mitochondria ROS effects attenuates and promotes recovery from colitis:
(a) Experimental protocol of 4-week colonic administration of rotenone vs. vehicle vs. MQ (3x/week) in mdr1a-/- with established chronic colitis. (b) Stool consistency measurements in rotenone vs. vehicle treated vs. MQ in mdr1a-/- at weekly intervals. (c) Histology colitis scores of rotenone vs. vehicle vs. MQ vs. non-colitic mdr1a-/- mice. (d) Representative whole colons and spleen sizes of and H&E of rotenone vs. vehicle vs. MQ vs. non-colitic mdr1a-/- mice. (e) Experimental protocol of colonic MQ vs. vehicle – 3x administrations during 7-day 2% DSS colitis protocol. (f, g) Daily percentages change from initial weight clinical colitis in MQ vs. vehicle in mdr1a-/- (n=6/group) and and WT mice (n=6/group) respectively. (h) Histology colitis scores in MQ vs. vehicle treated mdr1a-/- and WT mice, scale bar 50µm. (i) Experimental protocol of colonic MQ vs. vehicle treatment after 5 days of 2% DSS colitis protocol in WT mice. (j) Daily percentages of change from initial weight in MQ vs. vehicle treated WT, (n=8/7 respectively). All data represent mean± SEM.
MDR1 and SOD2 genes are differentially expressed in human IBD and intestinal epithelial specific deletion of SOD2 leads to increased susceptibility to experimental colitis
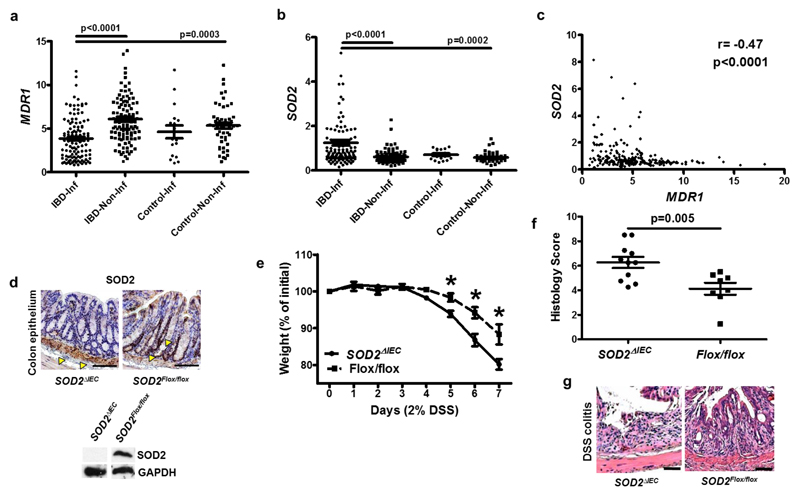
To further investigate the role of MDR1 and mROS in human IBD, we performed an in silico analysis of our IBD colonic microarray dataset (Gene Expression Omnibus GSE11223 and GSE20881) derived from a cohort of 67 individuals with UC, 53 with CD, 14 non-IBD colitis and 31 healthy controls13,31. Colonic gene microarray expression data were available from 118 inflamed IBD, 110 non-inflamed IBD and 50 healthy non-IBD colonic biopsies. In addition to significant downregulation of MDR1 expression in inflamed vs. non-inflamed IBD intestinal biopsies and inflamed IBD vs. healthy non-IBD intestinal biopsies (p<0.0001 and 0.0003 respectively); we interestingly found differential expression of SOD2 expression (upregulated) in both analyses (p<0.001 and 0.0002) (Fig 5a, b). MDR1 negatively correlated with SOD2 (r= -0.47, p<0.0001) in line with our earlier findings in mdr1a-deficient mice and shMDR1 CECs (Fig 5c). It is essential to determine whether primary ROS-mediated mitochondria dysfunction acts causally to promote the development of colitis. Furthermore, there may be factors such as variability in tissue penetration and retention that cannot be completely accounted for in the colonic rotenone exposure model. Therefore we genetically deleted the SOD2 gene from the intestinal epithelium by crossing SOD2floxed/floxed mice with mice expressing Cre-recombinase under the control of the intestinal-epithelial-specific villin promoter to SOD2IEC-KO mice (Fig 5d). Constitutive deletion of SOD2 gene in mice resulted in death early after birth from cardiac and liver failure32. In our study, SOD2IEC-KO mice were born in normal Mendelian ratio and had no overall abnormalities in the morphology of ileum and colon. Although they did not exhibit spontaneous colitis, SOD2IEC-KO developed more severe colitis following DSS treatment compared to SOD2floxed/floxed littermates (Fig 5e-g). Our data in SOD2IEC-KO mice provides evidential support for the loss of mitochondrial homeostasis in CECs as a specific factor in determining susceptibility to colitis.
Figure 5. MDR1 and SOD2 genes are differentially expressed in human IBD and intestinal epithelial specific deletion of SOD2 leads to increased susceptibility to experimental colitis:
(a-b) In silico analysis of MDR1 and SOD2 from 120 IBD patients (67 UC, 53 CD, 17 non-IBD colitis and 31 healthy controls); IBD-Inf = Inflamed IBD gut biopsies, IBD-Non-Inf = Non-inflamed IBD gut biopsies; Control-Inf = Non-IBD colitis and Control-Non-Infl =Non-inflamed gut biopsies from non-IBD individuals. (c) Spearman’s correlation test of MDR1 and SOD2 expression in 120 IBD patients. (d) Representative immunohistochemistry and Western blotting of SOD2 of colons (a) of SOD2IEC-KO and SOD2flox/flox of CECs, black scale bars 100 µm, yellow arrows showing SOD2 staining. (e) Daily percentages of weight change from initial weight in acute 2% DSS colitis comparing SOD2IEC-KO vs. SOD2flox/flox (n=12/8 respectively). (f) Histology colitis scores in SOD2IEC-KO vs. SOD2flox/flox mice (n=12/8 respectively). after 2% DSS colitis. (g) Representative H&E staining in SOD2IEC-KO vs. SOD2flox/flox mice after 2% DSS colitis, black scale bars 100 µm. All data represent mean± SEM.
Associations of genes regulating mitochondrial function with human IBD
Finally, to demonstrate clinical relevance of mitochondrial dysfunction as a new mechanistic factor in IBD, we exploited data from the latest meta-analysis of GWA studies of all European ancestry IBD patients vs. European controls (22,575 CD, 20,417 UC and 53,536 controls) 6. The most significant loci in the regions of ABCB1 (encoding MDR1) and SOD2 genes showed associations with p=3.19 x 10-3 and 3.04 x 10-3 respectively (below genome-wide significance). We performed an independent unbiased analysis (using GO term for mitochondria, GO:0005739 using the Mitominer program http://mitominer.mrc-mbu.cam.ac.uk/release-3.1) and identified 29 (5.0%) additional genes involved in mitochondria function within the subset of 574 (out of total 22 353) genes within 100kb of a genome-wide significant IBD locus from the same meta-analysis dataset above (Table S1). The top three positional candidate gene associations are: SLC25A28 (p=1.70 x 10-26) encoding mitoferrin-2, VARS encoding valine-tRNA ligase (p=4.83 x 10-26) and RNF5 (p=9.47 x 10-24) encoding E3 ubiquitin-protein ligase RNF5 are involved in mitochondria iron, tRNA transport and ubiquitination respectively33–35. Notable also, are the associations of the HSPA1-A, -B and –L (p=1.88 x 10-23) genes that encode the heat shock protein 70, which is integrally involved in the mitochondria unfolded protein responses (mtUPR), crucial for mitochondria protein homeostasis and biogenesis36. This suggests that the mitochondria’s contribution is likely more important than previously recognised in IBD.
Discussion
In this study, we define a key mitochondrial protective mechanism conferred by MDR1. Here, we present clear evidence of increased mitochondrial damage and consequential dysfunction following MDR1-deficiency with increased susceptibility to colitis driven by mitochondrial dysfunction in vivo. We therefore highlight a cogent model to further support mitochondrial dysfunction as an important mechanistic component in the pathogenesis of IBD (reviewed by Novak and Mollen) 37. We show conceptually that at the dynamic colonic mucosal interface in particular, mitochondria homeostasis requires tight regulation to prevent the deleterious downstream effects on epithelial integrity, activation of pro-inflammatory responses and release of mitochondria DAMPs as bona fide inflammatory triggers. The mitochondria participate in a broad range of innate responses to viral, bacterial and cellular damage38. Recently mitochondria have an increasingly recognized role in inflammation38 and are implicated in human diseases with underlying inflammatory pathologies, such as diabetes39, multiple sclerosis40, lung fibrosis41 and cardiovascular disease42.
Our data suggest an intricately linked picture, where MDR1 protects against damaging mitochondrial factors arising from the luminal environment via its efflux properties in addition to exerting an influence on key homeostatic responses such as energy production and autophagy. The compositional factors within the lumen in this context; and alternatively, mechanisms that affect the functionality of MDR1 have not yet been studied in detail. As an ATP-dependent efflux transporter, gut energy deficiency is a likely important factor. In the colon, mitochondria rely on the gut microbiota and their production of short chain fatty acid for energy 43 and CEC energy deficiency has been previously purported to be an IBD mechanism. Mouse lines with mitochondria genomic variants linked to high ATP production are protected against induced colitis 44. Whilst analysis of cellular bioenergetics in primary explants showed impairment in energy production, our in vitro CEC data indicate a more modest effect without the contribution of the luminal flora, with decreased CEC spare respiratory capacity in the presence of diminished MDR1 activity. The lack of baseline OCR differences ex vivo and in vitro may reflect fundamental differences in genetic knock-down rather than knock-out, inherent bioenergetic properties of colonic 'cancer' cell line and in vitro conditions that provided a more stable environment for mitochondrial function. In mouse, colonisation of specific gut commensals can influence the level of MDR1 gene expression45. Hence, it is conceivable that a primary effect of MDR1-deficiency on mitochondrial bioenergetics is potentiated by factors present in the luminal environment in the colon, chiefly the microbiota. In IBD, high levels of mitochondria damage, notably within the electron transport chain have been shown in CECs 46 and the resident luminal microbiota are strongly implicated in the pathogenesis of IBD8.
The evidence to support directly harmful effect of the microbiota on the mitochondria is noteworthy. Individuals with IBD have higher levels of anaerobic sulphate reducing bacteria, which can produce metabolites that can damage the mitochondria, inhibit cytochrome C and short chain fatty acid oxidation47. Within the gut flora, several clinically relevant pathogens including enteropathogenic E. coli 48 Helicobacter pylori49 and Salmonella typhimurium 50 target effector proteins to the mitochondria. Infection with Citrobacter rodentium has been shown to disrupt mitochondrial function and structure in mice 51. These lines of evidence suggest that the gut mitochondria occupy a distinct position as they are more exposed to damaging luminal factors, more so than in other tissues. Hence, it follows that different protective mechanisms are shaped to counter this challenge. In a proteomic analysis across 14 different mouse tissues, Pagliarini et al., demonstrated that intestinal epithelial mitochondria have a distinct proteomic profile and notably, have higher expression of ABC transporters 52. MDR1 (although part of the ABC superfamily) is not expressed on the mitochondria membrane53 but the closely analogous functions of these transporters highlight the importance of this protective role for the mitochondria in the gut.
Beyond the microbiota, the role of luminal mitochondrial toxins as triggers in IBD is unknown but seems plausible. Findings from Parkinson’s disease (PD), a condition characterized by marked mitophagy impairment 54,55 provides insight into how this might work in IBD pathogenesis. Here an environmental mitochondrial toxin, N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) represents a clear trigger for clinical PD. Like rotenone, MPTP is a complex I inhibitor of the electron transport chain that can induce acute PD that is indistinguishable from idiopathic PD56–58. Current literature suggests that rotenone may possess potential effects on the direct aggregation of protein aggregates such as α-synuclein (SNCA), ubiquitin and GAPDH; alterations of dopamine metabolism; and microglial activation via NFKB activation26. There maybe off-target actions too but given its dominant effect on mitochondria respiratory function, these may be difficult to detect. Even though the role for autophagy in general is clearly established in IBD, mitophagy has not yet been fully studied in this context 5,59. Strikingly and on further analysis however, genes involved in mitophagy (PARK7 chr1p36; p=4.8x10-9 for UC; and LRRK2 chr12q12; p=6.2x10-21 for CD) are strongly associated with IBD in GWA studies. In parallel, defective mitophagy has been demonstrated in colonic epithelial cells derived from Irgm1-deficient mice, implicating this pathway in another IBD-associate gene polymorphism23. Like the virus-plus-susceptibility gene interaction that determines CD susceptibility as proposed by Cadwell et al. in 2010, we put forward the concept of mitochondrial toxin-plus-genetic susceptibility60. In this regard, we show that rotenone can accelerate the development of spontaneous colitis in the susceptible mdr1a-deficient model and in acute-induced DSS colitis, a setting when a second ‘hit’ along with rotenone exacerbates the severity of colitis. We believe that this is the first description of such kind although the protective effects of mitochondrial specific anti-oxidant (MitoQ) and more generally, anti-oxidants such as ascorbic acid have been described in experimental colitis29,30 61.
Mitochondrial dysfunction via ROS production is a major mediator of inflammation and can directly modulate the NLRP3 inflammasome, NFKB and MAPK signalling pathways62,63. Mitochondrial ROS also promote the cytosolic release of mtDNA, which mediates NLRP3 inflammasome activation and can directly trigger TLR9 signalling on neutrophils64–66. Accumulation of dysfunctional mitochondria perpetuate the production of mROS, amplifying innate inflammatory responses such as type I interferon67 and endotoxin induced IL-1β production68. Mitochondrial ROS inhibits autophagy, the major process for removal of damaged mitochondria64. Defective autophagy in turn allows for the escape of pro-inflammatory mitochondrial DAMPs 66 65. Our published colonic microarray study showing that gene-sets regulating the mitochondria (p=4.7×10−25) and oxido-reductase functions (p=1.4×10−13) were most differentially expressed comparing distal (where UC invariably affects) vs. proximal colon in UC. Further in silico analyses showed a negative correlation between MDR1 and SOD2, and our data showing increased susceptibility to DSS colitis following intestinal epithelial specific deletion of the SOD2 gene strongly supports the causal importance of ROS-detoxification.
IBD pathogenesis is complex and encompasses multiple factors, which may trigger disease onset, heighten susceptibility, potentiate severity and/or promulgate non-resolution of inflammation. These factors combine to shape the many phenotypes of IBD. In this context, our data importantly highlight the mitochondria’s contribution as a new ‘jigsaw’ piece, a hitherto underexplored focus within this complex framework of factors. Specific pharmacologic MDR1 augmentation is a translational challenge due to induction of drug resistance as one known problem. However, our studies open up a new landscape of potential therapeutic approaches targeting downstream effects of mROS-DAMP, cellular bioenergetics and mitophagy as clear examples. Furthermore, we show that 5% of genes highlighted by IBD GWA studies are functionally linked to the maintenance of mitochondria health. Hence, the focus on mitochondrial dysfunction has broad translational applications, which will lead to many new mechanistic perspectives and therapeutic opportunities in IBD.
Materials and Methods
Mouse
The FVB/129 mdr1a-/- and wild type mouse lines were purchased from Taconic. C57/BL6 mice carrying floxed allele flanking SOD2 gene was provided by Dr Shimizu, Chiba University, Japan and re-derived in University of Edinburgh. Villin-Cre recombinase C57/BL6 mice were purchased from Jackson laboratory. All colonies were maintained in specific pathogen free conditions (specifically Helicobacter-free) in University of Edinburgh. II10-deficient mice were maintained at University of North Carolina, Chapel Hill.
Electron microscopy
Mouse or human colonic samples were flushed with sterile phosphate buffered saline (PBS) and immediately transferred into 3% EM grade glutaraldehyde solution in 0.1M Sodium Cacodylate buffer, pH 7.3, for 2 hours before further processing. For quantification of abnormal mitochondria, viable cells with 5 or more abnormal mitochondria were classified as ‘abnormal’. A percentage against total number of IECs (minimum of 100 IECs in >5 images) was calculated per mouse.
Mitochondria studies
Mitochondria from CECs or mouse tissues were performed using Dounce homogenisers (30-40 strokes in 2 different gradients of homogenisers) extracted using Mitochondria Isolation Kit (Sigma-Aldrich, MITOISO1). For JC-1 assay, the mitochondria pellets were re-suspended in 100µl storage buffer + 1900µl JC-1 assay buffer + JC-1. Mitochondria suspensions were placed in clear-bottom black 96 wells plate: untreated, Antimycin 10µg/ml, rotenone 10µM and CCCP 10µM. JC-1 fluorescence was measured using the plate reader at 590nM. The rate of mitochondria membrane depolarisation was measured as the loss of JC-1 fluorescence after 1 hour. Measurements were normalised to the untreated group. For mROS studies, T84 CECs were plated and grown in 96 well tissue culture plates for at least 24-48 hours and to ~70% confluence. Cells were cultured in MitoSOX (2.5µM) or mitotracker Green (100nM) for 30 minutes and then washed in pre-warmed PBS before further culture with Antimycin (20µg/ml), rotenone (10µM) or CCCP (10µM). Relative fluorescence (RF) was quantified using the plate reader at Ex/Em 510/580 and 490/516 for MitoSOX and Mitotracker Green respectively. MitoSOX/MitoGreen RF readings were normalised to untreated MitoSOX/Mitotracker Green cells only.
Cellular energetics studies
Colon and ileum were harvested and placed in DMEM/F12 medium. A 3x3mm intestinal section was cut and mounted in Seahorse XF24 culture plate with the apical side of the lumen orientated upwards and maintained in position by an Islet Microcapture screen. The explants were washed twice with Seahorse Assay Media, supplemented with 1mM Pyruvate and 10mM Glucose (pH 7.4 at 37°C). These explants were placed into Seahorse analyzer within 1 hour of tissue harvest. We measured oxygen consumption rate (OCR) following addition antimycin/rotenone; providing mitochondrial function. The raw data were normalised to protein content using the Bradford quantification. T84 shMDR1 and shCtrl CECs were plated on Seahorse XF 24 cell culture plates. For the mitochondria stress test oligomycin was added added at 2µM, followed by 1µM FCCP then antimycin and rotenone (1µM each). Data was normalised to protein content measured by sulforhodamine B staining (Sigma S1402) to adjust for cell density.
Induction and histologic grading of colitis
Colonic rotenone or vehicle were administered using a flexible rectal tube following brief general anaesthesia with isofluorane. A volume of 500µl were used in a head-down position for at least 2 minutes before removal of anaesthesia and then immediately check for any complications. The rotenone concentration of 100 μM (volume of 500μl) equates to approximately 1mg/kg. In prior optimisation, we have tested that this volume completely filled the mouse colon to provide total exposure. Acute colitis was induced by 2-3% DSS (MP Biomedicals Ltd) in drinking water ad libitum for 7-10 days. Mice were monitored daily for weights, presence of diarrhoea and blood. In chronic rotenone treatment, mice were assessed at the end of every week. Specifically, we quantified stool consistency: Well-formed/normal = 0, Pasty/semi-formed = 1, Pasty = 2, Diarrhoea that does not adhere to anus = 3, Diarrhoea that adheres to anus = 4. For histology, each colonic sample was graded semi-quantitatively (Scores 0-3 per component): A. Degree of epithelial hyperplasia and goblet cell depletion. B. Leukocyte infiltration in the lamina propria. C. Area of tissue affected. D. Presence of markers of severe inflammation (such as crypt abscesses, submucosal inflammation and presence of ulcers). For colitis scores, the mean of proximal and distal colon scores was calculated.
Quantification of mitochondrial DNA
Plasma samples were obtained by cardiac puncture following CO2 euthanasia. Following sampling, blood samples were spun at 5 000x G for 10 minutes at 4C. DNA was extracted using Qiagen DNA Blood mini kit. Primer sequences for Cytochrome C oxidase sub-unit I (mCOI, Forward 5-GCCCCAGATATAG-CATTCCC-3; Reverse, 5-GTTCATCCTGTTCCTGCTCC-3) with qPCR performed using 2x SYBR Green Fast mix (Applied Biosystems). qPCR reactions were conducted in an ABI7900 Fast Real-Time PCR System (Applied Biosystems) with the following thermal profile: 1 cycle 95C for 20 sec; 40 cycles of 95C for 3 sec and 60C for 30 sec. mtDNA levels were quantified based on the following calculation: c = Q × VDNA/VPCR × 1/Vext; where c is the concentration of DNA in plasma (copies/µl); Q is the quantity (number of copies) of DNA determined by the qPCR system; VDNA is the total volume of eluted plasma DNA solution obtained after extraction (40µl); VPCR is the volume of plasma DNA used for PCR (40µl); and Vext is the volume of plasma extracted (200µl). Quantification was achieved relative to a known concentration of PCR amplicon obtained from DNA extracted from mouse CEC mitochondria using method previously reported.
Microarray dataset and analysis
Full detail of tissue acquisition and process are previously detailed 13. The whole data set is available at Gene Expression Omnibus (http://www.ncbi.nlm.nih.gov/geo/ (accessed 18 July 2008)6) accession: GSE11223 and GSE20881.
Genetic analyses
The presented data was derived from the meta-analysis of all European ancestry IBD patients vs. European controls 6. Analysis was done in R 3.2.2 (R Foundation for Statistical Computing, Vienna, Austria) using the Genomic Ranges package33. The UCSC hg19 Known Gene transcripts were filtered to keep only those with an associated Entrez Gene ID. For each Gene ID the earliest start and latest end position was taken from all of the transcripts for that gene. All p values within 100kb of each range were then associated with the respective Gene ID.
shRNA knockdown studies and transfection
T84 cells (purchased from ATCC) cells expressing MDR1 were transfected with MDR1 and control shRNA plasmids (SABiosciences) and selected using G418 (600ug/ml). Cells were cultured in DMEM/F12medium with 10% foetal calf serum, 100U/ml penicillin and 100ug/ml streptomycin. GFP-LC3 plasmid was transfected by Lipofectamine method (1:2 ratio) with GFP-plasmid controls to confirm transfection efficiency. Transfection was carried out on shMDR1 and shCtrl CECs grown on glass coverslips, which were then fixed with 4% paraformaldehyde and then viewed under fluorescence microscope.
Colonic epithelial cell isolation
Colons were removed and immediately placed in cold sterile PBS. Colons were opened longitudinally and further washed with buffer (154mM NaCl + 1mM dithiothreitol, DTT) three times. These were then placed in 5mL dissociation buffer (130mM NaCl, 1mM Na2EDTA, 10mM HEPES, 10% FCS, 1mM DTT) in a bijou and placed on a shaker at 140rpm at 37°C for 15 mins. Dissociated cells were placed in 15mL Falcon tube on ice. Incubation in dissociation buffer was repeated with another 2 x 5mL. Dissociated cells were spun at 2,500rpm for 10min at 4°C. Pellet was washed with PBS, spun at 5000rpm for 5min at 4°C.
Supplementary Material
Acknowledgements
This work was supported by MRC grant G0701898, Crohn’s and Colitis UK M16-1, ECCO IBD Investigator’s Award 2010, Chief Scientist Office ETM/75 awarded to GTH; NIH grants P01 DK 094779 and R01 DK053347 awarded to RBS; Wellcome Trust Investigator Award WT100981MA to NMM; Wellcome Trust grant WT096497 to DAD and AGR; Wellcome Trust WT097943 to NAK; Wellcome Trust Biomedical Vacation Scholarship 202597/Z/16/Z to ETSC; EU FP-7 grants 305676-2 and 305479-2 to JS.
Footnotes
Authors’ contributions
GTH planned and carried out experiments, analysed data and wrote the manuscript. REA performed the in vitro cell line work, transfection studies and gene/protein expression studies. RNC, ETSC, REA and NM planned, carried out and analysed the mitochondria Seahorse experiments. BL planned and assisted in mouse colitis studies, performed histologic analysis and TEM work. DAD set up the mitochondria DNA qPCR work and performed data analysis. NAK recruited IBD subjects and prepared plasma samples for human mitochondrial DNA work, and performed additional in silico microarray and genetic analyses. CLN carried out original work of human IBD microarray work. TS generated SOD2 mouse mutants. RBS provided C57/BL6 transgenic strains (mdr1a-/- and il10-/-). RBS, AGR, JPI and JS provided intellectual input into planning of experiments, data analysis and contributed to the writing of the manuscript. All authors reviewed and approved the final manuscript.
References
- 1.Danese S, Fiocchi C. Ulcerative colitis. The New England journal of medicine. 2011;365:1713–1725. doi: 10.1056/NEJMra1102942. [DOI] [PubMed] [Google Scholar]
- 2.Boyapati R, Satsangi J, Ho GT. Pathogenesis of Crohn's disease. F1000prime reports. 2015;7:44. doi: 10.12703/P7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Molodecky NA, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54.e42. doi: 10.1053/j.gastro.2011.10.001. quiz e30. [DOI] [PubMed] [Google Scholar]
- 4.Ho G-T, Boyapati R, Satsangi J. Ulcerative colitis. Medicine. 2015;43:276–281. [Google Scholar]
- 5.Jostins L, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–124. doi: 10.1038/nature11582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu JZ, et al. Association analyses identify 38 susceptibility loci for inflammatory bowel disease and highlight shared genetic risk across populations. Nature genetics. 2015;47:979–986. doi: 10.1038/ng.3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCole DF. IBD candidate genes and intestinal barrier regulation. Inflammatory bowel diseases. 2014;20:1829–1849. doi: 10.1097/MIB.0000000000000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sartor RB, Wu GD. Roles for Intestinal Bacteria, Viruses, and Fungi in Pathogenesis of Inflammatory Bowel Diseases and Therapeutic Approaches. Gastroenterology. 2016 doi: 10.1053/j.gastro.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dean M, Rzhetsky A, Allikmets R. The human ATP-binding cassette (ABC) transporter superfamily. Genome research. 2001;11:1156–1166. doi: 10.1101/gr.184901. [DOI] [PubMed] [Google Scholar]
- 10.Ambudkar SV, et al. Biochemical, cellular, and pharmacological aspects of the multidrug transporter. Annual review of pharmacology and toxicology. 1999;39:361–398. doi: 10.1146/annurev.pharmtox.39.1.361. [DOI] [PubMed] [Google Scholar]
- 11.Thiebaut F, et al. Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues. Proceedings of the National Academy of Sciences of the United States of America. 1987;84:7735–7738. doi: 10.1073/pnas.84.21.7735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Panwala CM, Jones JC, Viney JL. A novel model of inflammatory bowel disease: mice deficient for the multiple drug resistance gene, mdr1a, spontaneously develop colitis. Journal of immunology (Baltimore, Md. : 1950) 1998;161:5733–5744. [PubMed] [Google Scholar]
- 13.Noble CL, et al. Regional variation in gene expression in the healthy colon is dysregulated in ulcerative colitis. Gut. 2008;57:1398–1405. doi: 10.1136/gut.2008.148395. [DOI] [PubMed] [Google Scholar]
- 14.Langmann T, et al. Loss of detoxification in inflammatory bowel disease: dysregulation of pregnane X receptor target genes. Gastroenterology. 2004;127:26–40. doi: 10.1053/j.gastro.2004.04.019. [DOI] [PubMed] [Google Scholar]
- 15.Onnie CM, et al. Associations of allelic variants of the multidrug resistance gene (ABCB1 or MDR1) and inflammatory bowel disease and their effects on disease behavior: a case-control and meta-analysis study. Inflammatory bowel diseases. 2006;12:263–271. doi: 10.1097/01.MIB.0000209791.98866.ba. [DOI] [PubMed] [Google Scholar]
- 16.Resta-Lenert S, Smitham J, Barrett KE. Epithelial dysfunction associated with the development of colitis in conventionally housed mdr1a-/- mice. American journal of physiology. Gastrointestinal and liver physiology. 2005;289:G153–162. doi: 10.1152/ajpgi.00395.2004. [DOI] [PubMed] [Google Scholar]
- 17.Kim SC, et al. Variable phenotypes of enterocolitis in interleukin 10-deficient mice monoassociated with two different commensal bacteria. Gastroenterology. 2005;128:891–906. doi: 10.1053/j.gastro.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 18.Pankiv S, et al. p62/SQSTM1 binds directly to Atg8/LC3 to facilitate degradation of ubiquitinated protein aggregates by autophagy. The Journal of biological chemistry. 2007;282:24131–24145. doi: 10.1074/jbc.M702824200. [DOI] [PubMed] [Google Scholar]
- 19.Youle RJ, Narendra DP. Mechanisms of mitophagy. Nature reviews. Molecular cell biology. 2011;12:9–14. doi: 10.1038/nrm3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi SW, Gerencser AA, Nicholls DG. Bioenergetic analysis of isolated cerebrocortical nerve terminals on a microgram scale: spare respiratory capacity and stochastic mitochondrial failure. Journal of neurochemistry. 2009;109:1179–1191. doi: 10.1111/j.1471-4159.2009.06055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brookes PS, Yoon Y, Robotham JL, Anders MW, Sheu SS. Calcium, ATP, and ROS: a mitochondrial love-hate triangle. American journal of physiology. Cell physiology. 2004;287:C817–833. doi: 10.1152/ajpcell.00139.2004. [DOI] [PubMed] [Google Scholar]
- 22.Adolph TE, et al. Paneth cells as a site of origin for intestinal inflammation. Nature. 2013;503:272–276. doi: 10.1038/nature12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu B, et al. Irgm1-deficient mice exhibit Paneth cell abnormalities and increased susceptibility to acute intestinal inflammation. American journal of physiology. Gastrointestinal and liver physiology. 2013;305:G573–584. doi: 10.1152/ajpgi.00071.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaser A, et al. XBP1 links ER stress to intestinal inflammation and confers genetic risk for human inflammatory bowel disease. Cell. 2008;134:743–756. doi: 10.1016/j.cell.2008.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elinav E, et al. NLRP6 inflammasome regulates colonic microbial ecology and risk for colitis. Cell. 2011;145:745–757. doi: 10.1016/j.cell.2011.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xiong N, et al. Mitochondrial complex I inhibitor rotenone-induced toxicity and its potential mechanisms in Parkinson's disease models. Crit Rev Toxicol. 2012;42:613–632. doi: 10.3109/10408444.2012.680431. [DOI] [PubMed] [Google Scholar]
- 27.Johnson ME, Bobrovskaya L. An update on the rotenone models of Parkinson's disease: their ability to reproduce the features of clinical disease and model gene-environment interactions. Neurotoxicology. 2015;46:101–116. doi: 10.1016/j.neuro.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Murphy MP, Smith RA. Targeting antioxidants to mitochondria by conjugation to lipophilic cations. Annual review of pharmacology and toxicology. 2007;47:629–656. doi: 10.1146/annurev.pharmtox.47.120505.105110. [DOI] [PubMed] [Google Scholar]
- 29.Wang A, et al. Targeting mitochondria-derived reactive oxygen species to reduce epithelial barrier dysfunction and colitis. The American journal of pathology. 2014;184:2516–2527. doi: 10.1016/j.ajpath.2014.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dashdorj A, et al. Mitochondria-targeted antioxidant MitoQ ameliorates experimental mouse colitis by suppressing NLRP3 inflammasome-mediated inflammatory cytokines. BMC medicine. 2013;11:178. doi: 10.1186/1741-7015-11-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Noble CL, et al. Characterization of intestinal gene expression profiles in Crohn's disease by genome-wide microarray analysis. Inflammatory bowel diseases. 2010;16:1717–1728. doi: 10.1002/ibd.21263. [DOI] [PubMed] [Google Scholar]
- 32.Li Y, et al. Dilated cardiomyopathy and neonatal lethality in mutant mice lacking manganese superoxide dismutase. Nature genetics. 1995;11:376–381. doi: 10.1038/ng1295-376. [DOI] [PubMed] [Google Scholar]
- 33.Lawrence M, et al. Software for computing and annotating genomic ranges. PLoS Comput Biol. 2013;9:e1003118. doi: 10.1371/journal.pcbi.1003118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhong B, et al. The ubiquitin ligase RNF5 regulates antiviral responses by mediating degradation of the adaptor protein MITA. Immunity. 2009;30:397–407. doi: 10.1016/j.immuni.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 35.Ryan MT, Hoogenraad NJ. Mitochondrial-nuclear communications. Annu Rev Biochem. 2007;76:701–722. doi: 10.1146/annurev.biochem.76.052305.091720. [DOI] [PubMed] [Google Scholar]
- 36.Rath E, Haller D. Mitochondria at the interface between danger signaling and metabolism: role of unfolded protein responses in chronic inflammation. Inflammatory bowel diseases. 2012;18:1364–1377. doi: 10.1002/ibd.21944. [DOI] [PubMed] [Google Scholar]
- 37.Novak EA, Mollen KP. Mitochondrial dysfunction in inflammatory bowel disease. Front Cell Dev Biol. 2015;3:62. doi: 10.3389/fcell.2015.00062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.West AP, Shadel GS, Ghosh S. Mitochondria in innate immune responses. Nature reviews. Immunology. 2011;11:389–402. doi: 10.1038/nri2975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Szendroedi J, Phielix E, Roden M. The role of mitochondria in insulin resistance and type 2 diabetes mellitus. Nature reviews. Endocrinology. 2012;8:92–103. doi: 10.1038/nrendo.2011.138. [DOI] [PubMed] [Google Scholar]
- 40.Witte ME, Mahad DJ, Lassmann H, van Horssen J. Mitochondrial dysfunction contributes to neurodegeneration in multiple sclerosis. Trends in molecular medicine. 2014;20:179–187. doi: 10.1016/j.molmed.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 41.Bueno M, et al. PINK1 deficiency impairs mitochondrial homeostasis and promotes lung fibrosis. The Journal of clinical investigation. 2015;125:521–538. doi: 10.1172/JCI74942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nisoli E, Clementi E, Carruba MO, Moncada S. Defective mitochondrial biogenesis: a hallmark of the high cardiovascular risk in the metabolic syndrome? Circulation research. 2007;100:795–806. doi: 10.1161/01.RES.0000259591.97107.6c. [DOI] [PubMed] [Google Scholar]
- 43.Donohoe DR, et al. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell metabolism. 2011;13:517–526. doi: 10.1016/j.cmet.2011.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bar F, et al. Mitochondrial gene polymorphisms that protect mice from colitis. Gastroenterology. 2013;145:1055–1063.e1053. doi: 10.1053/j.gastro.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 45.Hooper LV, et al. Molecular analysis of commensal host-microbial relationships in the intestine. Science (New York, N.Y.) 2001;291:881–884. doi: 10.1126/science.291.5505.881. [DOI] [PubMed] [Google Scholar]
- 46.Santhanam S, et al. Mitochondrial electron transport chain complex dysfunction in the colonic mucosa in ulcerative colitis. Inflammatory bowel diseases. 2012;18:2158–2168. doi: 10.1002/ibd.22926. [DOI] [PubMed] [Google Scholar]
- 47.Szabo C. Hydrogen sulphide and its therapeutic potential. Nature reviews. Drug discovery. 2007;6:917–935. doi: 10.1038/nrd2425. [DOI] [PubMed] [Google Scholar]
- 48.Nagai T, Abe A, Sasakawa C. Targeting of enteropathogenic Escherichia coli EspF to host mitochondria is essential for bacterial pathogenesis: critical role of the 16th leucine residue in EspF. The Journal of biological chemistry. 2005;280:2998–3011. doi: 10.1074/jbc.M411550200. [DOI] [PubMed] [Google Scholar]
- 49.Ashktorab H, et al. Bax translocation and mitochondrial fragmentation induced by Helicobacter pylori. Gut. 2004;53:805–813. doi: 10.1136/gut.2003.024372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hernandez LD, Pypaert M, Flavell RA, Galan JE. A Salmonella protein causes macrophage cell death by inducing autophagy. J Cell Biol. 2003;163:1123–1131. doi: 10.1083/jcb.200309161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ma C, et al. Citrobacter rodentium infection causes both mitochondrial dysfunction and intestinal epithelial barrier disruption in vivo: role of mitochondrial associated protein (Map) Cellular microbiology. 2006;8:1669–1686. doi: 10.1111/j.1462-5822.2006.00741.x. [DOI] [PubMed] [Google Scholar]
- 52.Pagliarini DJ, et al. A mitochondrial protein compendium elucidates complex I disease biology. Cell. 2008;134:112–123. doi: 10.1016/j.cell.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Paterson JK, Gottesman MM. P-Glycoprotein is not present in mitochondrial membranes. Experimental cell research. 2007;313:3100–3105. doi: 10.1016/j.yexcr.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith WW, et al. Kinase activity of mutant LRRK2 mediates neuronal toxicity. Nature neuroscience. 2006;9:1231–1233. doi: 10.1038/nn1776. [DOI] [PubMed] [Google Scholar]
- 55.Bonifati V, et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science (New York, N.Y.) 2003;299:256–259. doi: 10.1126/science.1077209. [DOI] [PubMed] [Google Scholar]
- 56.Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic Parkinsonism in humans due to a product of meperidine-analog synthesis. Science (New York, N.Y.) 1983;219:979–980. doi: 10.1126/science.6823561. [DOI] [PubMed] [Google Scholar]
- 57.Betarbet R, et al. Chronic systemic pesticide exposure reproduces features of Parkinson's disease. Nature neuroscience. 2000;3:1301–1306. doi: 10.1038/81834. [DOI] [PubMed] [Google Scholar]
- 58.Panov A, et al. Rotenone model of Parkinson disease: multiple brain mitochondria dysfunctions after short term systemic rotenone intoxication. The Journal of biological chemistry. 2005;280:42026–42035. doi: 10.1074/jbc.M508628200. [DOI] [PubMed] [Google Scholar]
- 59.Franke A, et al. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn's disease susceptibility loci. Nature genetics. 2010;42:1118–1125. doi: 10.1038/ng.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cadwell K, et al. Virus-plus-susceptibility gene interaction determines Crohn's disease gene Atg16L1 phenotypes in intestine. Cell. 2010;141:1135–1145. doi: 10.1016/j.cell.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yan H, Wang H, Zhang X, Li X, Yu J. Ascorbic acid ameliorates oxidative stress and inflammation in dextran sulfate sodium-induced ulcerative colitis in mice. Int J Clin Exp Med. 2015;8:20245–20253. [PMC free article] [PubMed] [Google Scholar]
- 62.Bulua AC, et al. Mitochondrial reactive oxygen species promote production of proinflammatory cytokines and are elevated in TNFR1-associated periodic syndrome (TRAPS) The Journal of experimental medicine. 2011;208:519–533. doi: 10.1084/jem.20102049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou R, Yazdi AS, Menu P, Tschopp J. A role for mitochondria in NLRP3 inflammasome activation. Nature. 2011;469:221–225. doi: 10.1038/nature09663. [DOI] [PubMed] [Google Scholar]
- 64.Nakahira K, et al. Autophagy proteins regulate innate immune responses by inhibiting the release of mitochondrial DNA mediated by the NALP3 inflammasome. Nature immunology. 2011;12:222–230. doi: 10.1038/ni.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang Q, et al. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010;464:104–107. doi: 10.1038/nature08780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Oka T, et al. Mitochondrial DNA that escapes from autophagy causes inflammation and heart failure. Nature. 2012;485:251–255. doi: 10.1038/nature10992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tal MC, et al. Absence of autophagy results in reactive oxygen species-dependent amplification of RLR signaling. Proceedings of the National Academy of Sciences of the United States of America. 2009;106:2770–2775. doi: 10.1073/pnas.0807694106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Saitoh T, et al. Loss of the autophagy protein Atg16L1 enhances endotoxin-induced IL-1beta production. Nature. 2008;456:264–268. doi: 10.1038/nature07383. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.