Abstract
The purpose of this pilot study was to explore the feasibility of an intervention designed to facilitate partner support for lifestyle change among overweight and obese adults with serious mental illness (SMI). Fifteen adults with SMI enrolled in a lifestyle intervention at community mental health centers participated with a self-selected partner in an additional 12-week intervention component designed to facilitate social support for health behavior change. Participants reported that the program was useful, convenient, and helped them reach their goals. Approximately two-thirds (66%) of participants were below their baseline weight at follow-up, including 27% achieving clinically significant weight loss. Participants reported significant increases in partner support for exercise and use of persuasive social support strategies. Partner support interventions that promote exercising together and positive communication may be effective for helping individuals with SMI initiate and sustain health behavior change necessary to reduce cardiovascular risk.
Keywords: Serious mental illness, Lifestyle intervention, Social support, Weight loss
Introduction
Obesity is nearly twice as prevalent in people with serious mental illness (SMI) compared to people without mental illness (Scott and Happell 2011), and is associated with cardiometabolic disorders and a reduced life expectancy of 8–32 years in this population (Colton and Manderscheid 2006; Walker et al. 2015). Although the probability of attaining normal body weight is low for individuals who are obese (Fildes et al. 2015), significant reductions in cardiovascular risk factors can be attained from modest amounts of weight loss (Wing et al. 2011). A series of randomized controlled trials of lifestyle interventions have demonstrated that individuals with SMI can achieve clinically significant weight loss by making positive changes in diet and exercise (Bartels et al. 2013, 2015; Daumit et al. 2013; Green et al. 2015). However, the long-term maintenance of weight loss remains elusive for the vast majority of obese individuals, even among those who receive gold standard behavioral treatments (Diabetes Prevention Program Research 2009). Developing new approaches to increasing the potency and long-term effectiveness of lifestyle interventions targeting weight loss and decreased cardiovascular risk in individuals with obesity and SMI is a public health priority (Suetani et al. 2015).
Bolstering natural support may be an effective solution to increasing the potency and long-term effectiveness of lifestyle interventions targeting weight loss and improved cardiovascular health in individuals with SMI. Research with general population samples has shown that family members and friends positively influence health behavior change in a variety of ways including practical support, verbal encouragement, exercising together, and by offering choices and options for healthy behaviors (Gorin et al. 2014; Latkin and Knowlton 2015). Randomized controlled trials have shown that enrolling family and friends in weight loss programs leads to greater weight loss for participants, with the added benefit of weight loss among partners (Wing and Jeffery 1999; Gorin et al. 2014). Support partners have been successfully trained to increase positive forms of social support (e.g., persuasion) while decreasing negative social support (i.e., criticism) toward participants enrolled in a lifestyle intervention (Sorkin et al. 2014). However, lifestyle interventions for overweight and obese individuals with SMI have yet to systematically leverage close relationships, such as family members, friends, and significant others, to support healthy eating and exercise behaviors in daily life where these behaviors take place.
Facilitating support from friends and family members for health behavior change could be beneficial for individuals with SMI who experience challenges to healthy eating and physical activity, including negative perceptions of healthy eating (Barre et al. 2011) and a lack of exercise self-efficacy (Shiner et al. 2008). Health promotion coaches delivering lifestyle interventions to individuals with SMI have identified the potential benefits of significant others as facilitators and reinforcers of healthy food choices and exercise behaviors in daily life (e.g., evenings and weekends) (Aschbrenner et al. 2015). Participants with SMI enrolled in lifestyle interventions have reported that friends and family members were essential to their success by providing reminders and encouraging messages, and by joining them in making healthy dietary changes and exercising (Aschbrenner et al. 2013; Yarborough et al. 2015).
In a prior proof of concept study we explored the initial feasibility of developing and implementing a partner support intervention (Fit Together) for overweight and obese individuals with SMI to augment and extend the evidence-based In SHAPE healthy lifestyle program (Aschbrenner et al. 2016). Participants enrolled in the In SHAPE program were presented with the option to nominate a friend or family member to participate in an intervention component designed to increase social support for their health goals in their home and social environments. Feedback from the initial pilot study led to the refinement of Fit Together, including the addition of a more interactive format to dyadic health promotion learning sessions. Building on this formative work, the primary purpose of the present feasibility pilot study was to evaluate the acceptability and potential health benefits of the refined Fit Together model. As the Fit Together program is designed to facilitate social support for health behavior change, we also examined whether there were changes in this hypothesized intervention mechanism of action.
Methods
Participants
The study was conducted in collaboration with two community mental health agencies in the Northeastern United States. Health coaches from the In SHAPE lifestyle intervention approached participants by telephone or in person who had been enrolled in the program at least 3 months to inquire whether they would be interested and willing to be contacted by our research team to learn about a new study of an additional program component designed to increase support for health behavior change from friends or family in their daily lives. Participants were eligible for the Fit Together study if they were age 18 or older; had a chart diagnosis of schizophrenia, schizoaffective disorder, major depressive disorder, or bipolar disorder; and a body mass index (BMI) ≥ 25. Excluded persons had medical contraindication to weight loss; pregnant or planning to become pregnant within the next 6 months; prior or planned bariatric surgery; or current diagnosis of an active alcohol-use or substance-use disorder. Research staff described the study to referred In SHAPE participants and invited them to attend a screening appointment at the community mental health center where their cognitive status was assessed (using the Mini-Mental State Examination cut-off score < 24) along with their perception of the availability of a close friend, family member or significant other who would be willing to participate in the study as a self-selected support partner. Support partners had to be 18 years of age or older and have at least weekly in-person contact with the participant. There were no BMI criteria for the participants’ support partners.
Fit Together Intervention
Fit Together was designed to augment the evidence-based In SHAPE healthy lifestyle intervention for individuals with SMI by increasing support from participants’ family members, friends, and significant others for the fitness and weight loss goals they set in the In SHAPE program. In SHAPE is an individualized fitness intervention consisting of weekly 1-hour supported exercise sessions with a certified personal fitness trainer at a local fitness facility, education and guidance on healthy eating and nutrition, and support for coping with mental health symptoms that interfere with health behavior change (Van Citters et al. 2010). In two separate RCTs, In SHAPE achieved reduced cardiovascular risk in approximately half of participants, defined as either ≥5% weight loss or clinically significant increase in walking distance (Bartels et al. 2013, 2015). One challenge for many In SHAPE participants has been finding the support needed to continue making health behavior changes while transitioning from intensive one-on-one contact with the health coach. Fit Together was designed to augment and extend the In SHAPE individualized health coaching model with a complementary component designed to facilitate natural supports for healthy eating and exercise from participants’ friends and family members as needed in home and social environments. The long term goal beyond the scope of this feasibility research is to evaluate the potential of Fit Together to help participants sustain lifestyle changes after participation in a lifestyle intervention.
The Fit Together intervention consisted of 12 weekly 1-hour dyadic sessions run concurrently with the In SHAPE program with a Fit Together health coach who facilitated and reinforced partner support for the fitness and weight loss goals that participants set in the In SHAPE program. The Fit Together coach provided the participant-partner pair with basic education about healthy eating, exercise, and weight loss. This included acknowledging additional challenges to health behavior change and weight loss experienced by people with SMI (e.g., depressive symptoms, psychiatric medications), while emphasizing that many people with SMI are able to lose weight and improve their cardiovascular health through healthy eating and increased exercise. The coach helped the participant-partner pair identify social support strategies for health behavior change, including practical support (e.g., transportation to gym, reminders to exercise), emotional support (e.g., encouragement, positive feedback), and informational support (e.g., guidelines about healthy eating). The pair identified shared health goals where there was opportunity for collaborative behavior change.
The pairs were also taught communication skills to increase positive support and problem solving strategies to resolve challenges through role-play exercises. To encourage exercising together, participants and their support partners received free gym memberships and wearable physical activity tracking devices (Fitbit Zips). The Fitbit Zip is an accelerometer that tracks steps and distance walked worn by clipping to clothing. Participants and support partners could view their steps on the Fitbit LCD display and compare their daily steps. To overcome negative perceptions about healthy eating, nutrition guidelines were introduced through a series of food-centered activities. Each activity was designed to help participants and their support partners discover that planning and sharing healthy meals and snacks could be a mutually beneficial and positive experience.
The Fit Together coach held a bachelor’s degree in psychology and participated in a 2-day In SHAPE training with instruction on healthy eating strategies and nutrition as well as training in motivational interviewing and tailoring wellness plans to meet the needs of persons with SMI. The coach also participated in a half-day training on the principles of behavioral family therapy (Mueser and Glynn 1999), including dyadic communication skills training. Throughout the study, the Fit Together coach received weekly 60-minute supervision sessions with the study’s principal investigator, a researcher with expertise in health promotion for individuals with SMI. The coach communicated any concerns about participants’ involvement in the Fit Together program as well as their successes to the In SHAPE health coach on a weekly basis.
The participant-partner pairs received the 12-week Fit Together program in an uncontrolled pre-post design in order to evaluate the acceptability and potential health benefits of the intervention. The once weekly dyadic sessions with the Fit Together coach lasted 1 h. Participants were not compensated for participating in the Fit Together intervention, but did receive $20 for completing a 2-hour baseline assessment and $30 for completing a post-intervention assessment. Support partners received $10 for completing a 45-min baseline assessment and $20 for completing a post-intervention assessment.
Data Collection
Measures were included to assess the acceptability and possible benefits of the intervention. Acceptability data were collected from a satisfaction and feedback form that each participant-partner pair completed at the end of the intervention. Participants and their partners were assessed at baseline and post-intervention. Demographic characteristics were obtained from both participants and their support partners using self-report. Participant outcomes included cardiorespiratory fitness, weight loss, body mass index, self-reported physical activity, and stage of change for weight loss related behaviors. Measures of perceived social support for health behavior change were included to explore the hypothesized intervention mechanism of action underlying health behavior change. Data were collected on the support partners’ weight, body mass index, and self-reported exercise to explore possible secondary benefits of the intervention.
Primary Outcome Measures
Weight and Body Mass Index (BMI)
Weight was measured in pounds (lbs.) on a flat, even surface with the use of a high-quality, calibrated digital scale, with the participant wearing indoor clothing and no shoes. Change in weight (lbs.) over time was reported. The proportion of participants who achieved ≥5% decrease from baseline weight was calculated because that is an accepted standard for clinically significant loss (Blackburn 1995), and is associated with improvements in cardiovascular risk factors in overweight and obese individuals (Wing et al. 2011). BMI was calculated by the formula: Weight (kg)/Height(m)2.
Cardiorespiratory Fitness
Cardiorespiratory fitness was assessed with the 6-Minute Walk Test (6-MWT), which measures the distance an individual can walk in 6 min (Balke 1963). In obese adults, the 6-MWT is a reliable and valid measure of cardiovascular fitness with acceptable test–retest and discriminant validity, and has been used to assess fitness levels among adults with a variety of chronic health conditions (Beriault et al. 2009; Larsson and Reynisdottir 2008). Change in this measure was reported as change in feet compared to baseline. An increase in distance of >50 m (about 164 feet) on the 6-MWT is considered clinically meaningful among people with medical conditions such as heart failure, chronic obstructive pulmonary disease, and pulmonary arterial hypertension (Rasekaba et al. 2009). Given the high rates of chronic comorbid medical conditions among individuals with SMI, we used the >50 m criteria to assess clinically significant increases in cardiorespiratory fitness among study participants.
Physical Activity
Physical activity was measured using the short-form International Physical Activity Questionnaire (IPAQ) (Faulkner et al. 2006). The reliability and validity of the IPAQ for use among persons with SMI is comparable to that in the general population (Faulkner et al. 2006). Summary scores were calculated for vigorous and moderate physical activities obtaining an estimate of weekly metabolic equivalent expenditure (MET) minutes of vigorous physical activity. Self-report data were also collected on number of days per week participants exercised.
Stage of Change for Weight Loss Related Behaviors
The weight loss behavior stage of change scale was used to assess participants’ readiness to change dietary and exercise behaviors (Sutton et al. 2003). Participants rated their perceived stage of change ranging from 1 = pre-contemplation to 5 = maintenance for each of four behavioral domains: (1) fruits and vegetables; (2) fat intake; (3) portion control; and (4) physical activity. An average score was calculated for each domain. This measure has been used to assess stage of change among overweight and obese individuals treated for chronic disease in a clinical trial (Logue et al. 2005).
Exploratory Secondary Measures
Measures of social support included the Sallis Social Support Surveys (Sallis et al. 1987), Health Related Social Control (Stephens et al. 2013), and the Important Others Questionnaire (Williams et al. 2006) in relation to the supportive behaviors of partners. The Sallis Support scales have adequate reliability and validity and have been utilized in previous weight loss studies (Gorin et al. 2014). Two versions of the Sallis scales were administered—one for diet and one for physical activity—with participants asked to rate the behaviors of their partner participating in the study over the past 3 months. Participants rated items on a 5-point Likert scale ranging from 1 = none to 5 = very often. Subscales used in the present study included Encouragement for Healthy Eating, Discouragement for Healthy Eating, and Participation in Exercise. Partner encouragement of healthy eating included five items (e.g., “encouraged me not to eat high-salt, high-fat foods when I’m tempted to do so,” “discussed my eating habit changes with me).” Partner discouragement for healthy eating included five items (e.g., “ate high fat, or high salt foods in front of me,” “offered me foods I am trying not to eat”). Partner participation in exercise included nine items (e.g., “exercised with me,” “gave me encouragement to stick with my exercise program”). An average score was calculated for each subscale.
Two types of health-related social control were assessed with a measure used in prior studies of partner support for lifestyle change (Stephens et al. 2013; Sorkin et al. 2014). Persuasive social support strategies involving efforts to prompt or persuade another person to improve his or her health behaviors have been found to elicit positive health behavior change (Stephens et al. 2009), whereas control strategies that involve the use of pressure, such as criticizing or expressing doubts about the person’s health behavior, have been found to undermine behavior change (Martire et al. 2013). Participants were asked to indicate the frequency with which their partner used social persuasion (3 items) and social pressure (4 items) to influence their health behaviors. Responses were made on a six-point scale (0 = not at all, 5 = everyday), and an average score was calculated for each domain. An example of a persuasion item is: “Over the past month, how often did your partner let you know that your poor food choices or physical inactivity worry them?” An example of a pressure item is: “Over the past month, how often did your partner restrict you from making poor food choices?”
An adapted version of the Important Other Climate Questionnaire (IOCQ) assessed participants’ perceptions of autonomy supportive behaviors from their partners (Williams et al. 2006). Autonomy support for health-related change involves acknowledging personal values, providing choice and relevant information, and minimizing controlling behaviors (Williams et al. 2009). The adapted IOCQ consists of 15 items that were rated 1 = not at all true to 7 = very true. Two subscales were calculated: (1) autonomy support (9 items) and (2) direct support (6 items). A sample item for autonomy support included: “My partner conveys confidence in my ability to make changes towards my goals.” A sample item for direct support included: “My partner has been problem solving about my plans to achieve my goals.” An average score was calculated for each domain.
Data Analysis
Statistical analyses were performed using SPSS software, version 22.0. Descriptive statistics, including means and frequencies, were used to summarize program attendance and participant satisfaction ratings. A series of paired sample t-tests were used to test differences between the baseline scores and the post-treatment scores for primary and secondary outcome measures.
All authors certify their responsibility for the manuscript. None of the authors report any financial conflicts of interest. The Committees for the Protection of Human Subjects at Dartmouth College and the New Hampshire Department of Health and Human Services approved this study.
Results
Participants
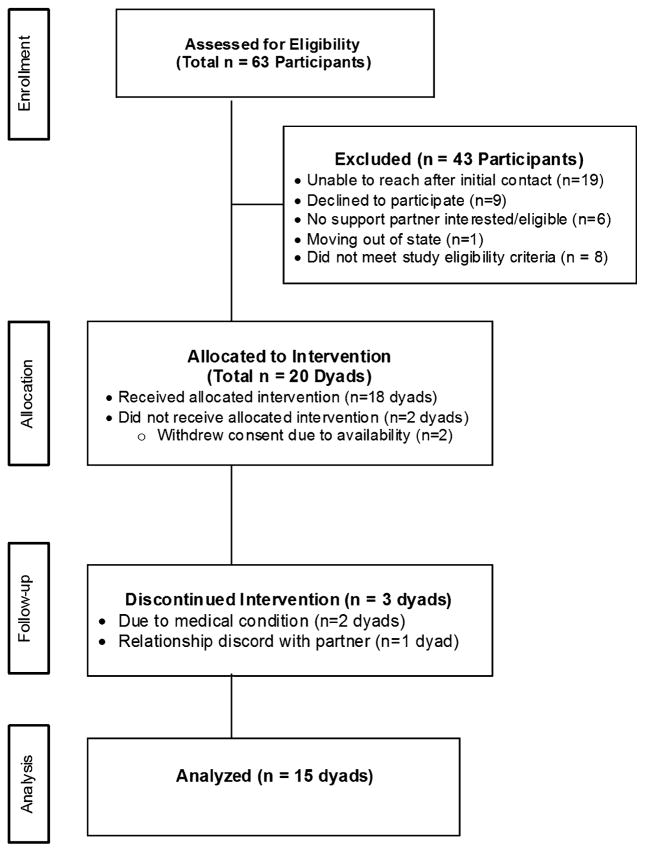
A total of 63 In SHAPE participants were referred to the Fit Together study by In SHAPE health coaches (see Consort diagram, Fig. 1). Among those participants referred to the program, we were unable to reach 19 participants to have an initial conversation about the study. The 19 referrals we were unable to reach included participants who were not well engaged in the In SHAPE program with the hopes that social support would increase their engagement. After conducting the eligibility screening, a total of 20 dyads (i.e., participant-partner pairs) were allocated to the intervention. As shown in Fig. 1, two dyads withdrew before starting the Fit Together intervention and three dyads discontinued their participation in the intervention for various reasons. A total of 15 participant-partner pairs completed the 12-session Fit Together intervention.
Fig. 1.
Participant enrollment, allocation, follow-up, and analysis
The demographic characteristics of participants and their support partners are presented in Table 1. The average age of the participants was 39.6 years (SD = 12.5), whereas the mean age of their support partners was 49.6 years (SD = 13.6). Most participant-partner pairs were comprised of partners who were friends (33%), parents (27%), and significant others (23%), with a smaller proportion of spouses (11%) and only one adult child support partner (6%). Half of the participant-partner pairs were living together at the time of the study. Over half of the participant-partner pairs (56%) reported daily face-to-face contact, with 39% of pairs having at least weekly contact and one pair reporting face-to-face contact 2–3 times per month.
Table 1.
Characteristics of participants and partners
| Characteristic | Participants (N = 18) | Partners (N = 18) |
|---|---|---|
| Age (years), mean (±SD) | 39.6 (12.5) | 49.6 (13.6) |
| Female, n (%) | 10 (56) | 13 (72) |
| White, n (%) | 15 (83) | 14 (78) |
| Hispanic or Latino, n (%) | 1 (6) | 1 (6) |
| Education, ≥High School, n (%) | 15 (83) | 12 (66) |
| Married, n (%) | 2 (11) | 5 (27) |
The BMI and obesity classification of participants and partners by relationship type is presented in Table 2. Participants had a mean BMI of 43.1 kg/m2 (SD = 10.3), with 61% of participants meeting the criteria for Class III obesity (BMI ≥40), which is considered morbidly obese. In contrast, partners had a mean BMI of 30.2 kg/m2 (SD = 6.5) with over half of support partners (56%) classified as normal weight or overweight (not obese).
Table 2.
Body mass index and obesity classification of participants and partners by relationship type
| Partners by relationship type | |||||
|---|---|---|---|---|---|
|
|
|||||
| Participants (N = 18) | Partners (N = 18) | Family member (N = 8) | Significant other (N = 4) | Friend (N = 6) | |
| Baseline body mass index (kg/m2), mean (±SD) | 43.1 (±10.3) | 30.2 (±6.5) | 28.6 (5.6) | 32.2 (8.1) | 30.8 (7.1) |
| Classification of overweight and obesity by BMI, n (%) | |||||
| Normal weight (18.5–24.9) | 0 (0) | 3 (17) | 2 (25) | 0 (00) | 1 (17) |
| Overweight (25.0–29.9) | 2 (11) | 7 (39) | 3 (38) | 2(50) | 2 (33) |
| Obesity class I (30.0–34.9) | 2 (11) | 5 (28) | 2 (25) | 1 (25) | 2 (33) |
| Obesity class II (35.0–39.9) | 3 (17) | 1 (5) | 1 (12) | 0 (0) | 0 (0.0) |
| Obesity class III (40.0+) | 11 (61) | 2 (11) | 0 (0) | 1 (25) | 1 (17) |
Satisfaction
Participant-partner pairs rated their satisfaction with the program (see Table 3). On average, both participants and their support partners appraised Fit Together positively and the majority reported that the program was useful, convenient, and helped them reach their goals (see Table 3). All (100%) of the support partners and 93% of participants rated the Fitbit wearable activity tracker as very useful, whereas 53% of the participants and their partner pairs found the gym membership to be very useful, respectively. Approximately three-quarters of participants (74%) and 93% of support partners were very likely to recommend the program to others.
Table 3.
Participant and partner satisfaction with the Fit Together program
| Item | Number (%) of participants selecting each response | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Not at All | Somewhat | Very | ||||
|
|
|
|
||||
| PPT | Partner | PPT | Partner | PPT | Partner | |
| Did program help you with your goals? | 0 (0%) | 1 (7%) | 4 (27%) | 4 (27) | 11 (73%) | 10 (66%) |
| How easy was it for you to understand? | 0 (0%) | 2 (0%) | 6 (40%) | 2 (13%) | 9 (60%) | 13 (87%) |
| How useful was the social support plan? | 1 (7%) | 0 (0%) | 3 (20%) | 1 (7%) | 11 (73%) | 14 (93%) |
| How useful were the nutrition sessions? | 1 (7%) | 0 (0%) | 2 (13%) | 1 (7%) | 12 (80%) | 14 (93%) |
| How helpful were the role-play practice? | 4 (27%) | 1 (7%) | 7 (46%) | 5 (33%) | 4 (27%) | 9 (60%) |
| How helpful was the Fitbit activity tracker? | 0 (0%) | 0 (0%) | 2 (13%) | 0 (0%) | 13 (87%) | 15 (100%) |
| How useful was the gym membership? | 5 (33%) | 3 (20%) | 2 (13%) | 4 (27%) | 8 (53%) | 8 (53%) |
| How convenient was the program? | 1 (7%) | 0 (0%) | 5 (33%) | 4 (27%) | 9 (60%) | 11 (73%) |
| How satisfied are you with the program? | 1 (7%) | 0 (0%) | 1 (7%) | 0 (0%) | 13 (86%) | 15 (100%) |
| Are you likely to recommend the program? | 2 (13%) | 0 (0%) | 2 (13%) | 1 (7%) | 11 (74%) | 14 (93%) |
Primary Outcomes
Table 4 provides a summary of the results for the paired samples t-tests comparing scores from baseline to post-intervention. Results show that at the end of the 12-week intervention, participants showed significant improvements in readiness to change physical activity, t(14) = -2.46, p < 0.05, and dietary fat, t(14) = −2.70, p < 0.05. Although changes in weight and BMI from baseline to post-intervention were not statistically significant, approximately two-thirds (66%) of participants lost weight. Over one quarter (27%) of participants achieved clinically significant weight loss (≥5%), and 40% of participants who lost any weight achieved clinically significant weight lost (≥5%). Overall changes in cardiorespiratory fitness measured by the 6-MWT from baseline to post-intervention were not statistically significant. There were no significant changes in weight or BMI for support partners.
Table 4.
Mean scores on primary and secondary outcome variables at baseline and post-intervention (3-month follow-up)
| Outcome | Baseline | Post-intervention | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| M | SD | M | SD | t | p | |
| Primary outcomes | ||||||
| Participants | ||||||
| Fitness and weight loss | ||||||
| Weight (lbs.) | 266.0 | 79.6 | 260.7 | 86.4 | 1.95 | 0.072 |
| Body mass index (kg/m2) | 43.6 | 11.3 | 42.7 | 12.4 | 1.98 | 0.067 |
| Cardiorespiratory fitness 6 MWT distance (feet) | 1384.6 | 268.6 | 1420.2 | 365.1 | −0.409 | 0.689 |
| Physical activity | ||||||
| Readiness to change physical activity | 2.5 | 1.1 | 3.2 | 1.1 | −2.46 | 0.027 |
| Exercise number of days per week | 2.4 | 1.5 | 2.8 | 1.9 | −0.581 | 0.571 |
| IPAQ total vigorous score | 446.4 | 770.2 | 178.6 | 334.2 | −0.360 | 0.724 |
| Readiness to change dietary behaviors | ||||||
| Dietary fat | 3.2 | 1.2 | 4.0 | 1.1 | −2.70 | 0.017 |
| Portion control | 3.0 | 1.1 | 3.4 | 1.1 | −1.16 | 0.265 |
| Fruit and vegetable servings | 3.5 | 0.99 | 3.8 | 0.67 | −1.00 | 0.334 |
| Support partners | ||||||
| Weight loss | 183.1 | 39.9 | 183.7 | 43.6 | −0.348 | 0.733 |
| Exercise number of days per week | 3.0 | 2.8 | 3.7 | 2.7 | −0.950 | 0.358 |
| Secondary outcomes | ||||||
| Social support for diet and exercise behaviors | ||||||
| Encouragement for healthy eating | 18.3 | 4.7 | 19.4 | 4.5 | −1.27 | 0.223 |
| Discouragement of healthy eating | 11.9 | 3.5 | 12.4 | 4.3 | −0.370 | 0.717 |
| Participation in exercise | 33.6 | 11.0 | 38.6 | 10.7 | −2.60 | 0.021 |
| Health related social control | 1.3 | 1.4 | 1.5 | 1.0 | −0.820 | 0.443 |
| Persuasion | 1.3 | 1.7 | 2.3 | 1.3 | −2.85 | 0.029 |
| Pressure | 1.3 | 1.6 | 1.0 | 0.87 | 0.956 | 0.376 |
| Autonomy support | 5.6 | 1.1 | 5.7 | 1.4 | −0.582 | 0.570 |
| Direct support | 5.1 | 1.5 | 5.7 | 1.5 | −1.55 | 0.143 |
Secondary Outcomes
Participants reported significant changes in partner support for exercise over the study period, t(14) = −2.60, p < 0.05. However, there were no significant changes in either of the subscales related to partner support for eating behaviors. Participants reported a significant increase in persuasive social support strategies over the study period, t(14) = 2.86, p < 0.05. Changes in autonomy and direct support were not statistically significant.
Discussion
This feasibility pilot study investigated a novel social support intervention designed to augment a healthy lifestyle intervention for overweight and obese individuals with SMI. Overall, participants and their partners indicated high satisfaction with the Fit Together program. Participants reported significant changes in partner support for exercise over the study period. Although changes in weight were not statistically significant in this small sample, approximately two-thirds (66%) of participants were below their baseline weight at the 12-week post-intervention assessment, and 27% of participants achieved clinically significant weight loss (≥5%) over the 12-week period. There were no significant changes in weight or BMI for support partners.
The finding that 27% of Fit Together participants achieved clinically significant weight loss is consistent with results from randomized controlled trials of the In SHAPE intervention (Bartels et al. 2013, 2015), but the results here were achieved in half the time (3 vs. 6 months). Findings from this pilot study suggest that augmenting lifestyle interventions for individuals with SMI with support from family and friends in participants’ home and social environments where health behaviors take place may enhance intervention potency. This could ultimately lead to the development of lifestyle interventions that mobilize natural support for health behavior change in participants’ day-today environments, thus decreasing long-term reliance on professional coaching services in this at-risk population.
Several prior studies targeting partner support for weight loss in general population samples have required that support partners be classified as overweight (BMI ≥ 25) and/or be interested in losing weight (Wing and Jeffery 1999; Gorin et al. 2013; Sorkin et al. 2014). However, given the high rates of obesity and comorbid medical conditions among individuals with SMI, we hypothesized that many participants would have close friends or family members who would be willing and interested to support the participant’s health goals without necessarily having a self-interest in losing weight. The average baseline BMI of support partners in this study was substantially lower than participants’ baseline BMI (30.2 ± 6.5 vs. 43.1 ± 10.3, respectively), and the majority of partners (56%) met the BMI criteria for normal weight or overweight (not obese) at baseline. These individuals were likely motivated to join Fit Together to support the participants (who were mostly morbidly obese) due to concerns about their health risks, rather than being incentivized to pursue their own health goals. Advancing health promotion intervention models that cast a wide net with respect to the goals, needs, and preferences of potential support partners may be appropriate for high-risk individuals.
A secondary aim of this study was to explore changes in social support for health behavior change. Participants reported that partner support for exercise significantly increased over the study period, which included participant-partner pairs exercising together. Prior research in general population samples has found that couples are highly concordant for health behaviors, and that both men and women are more likely to make a positive health behavior change if their partner also makes that change (Jackson et al. 2015). The Fit Together coach encouraged the participant-partner pair to identify shared health goals. The pairs were given free gym memberships and Fitbit wearable activity trackers to incentivize shared physical activity. Almost all of participants and support partners, 87% and 100%, respectively, reported that the Fitbits were “very helpful” in promoting physical activity. This high satisfaction with using wearable devices for activity tracking is consistent with prior studies among people with SMI (citation 2015). The use of existing low cost and widely available fitness technologies that enable participants to see one another’s achievements and challenge each other to go further may be an ideal tool for facilitating shared physical activity in partner-support interventions targeting lifestyle change.
Participants reported significant increases in their partner’s use of persuasive social support strategies. Persuasive social support (often referred to as positive social support) is a form of health related social control that involves efforts to prompt or persuade another person to improve his or her health behaviors as opposed to using pressure, such as criticizing or expressing doubts about the person’s health behavior (Stephens et al. 2013; Sorkin et al. 2014). The Fit Together intervention incorporated communication skills training based on principles and techniques of social skills training with families and couples coping with mental illness (Mueser et al. 1994; Mueser and Glynn 1999). Behavioral techniques, including modeling, behavioral rehearsal, positive reinforcement, and home assignments were used to teach the participant-partner pair more effective ways to express positive feelings (e.g., recognizing success, expressing gratitude), make requests (e.g., going to the gym together, help with transportation), and express negative feelings (e.g., feeling disappointed) as they related to health behavior changes. Partner communication about health behavior changes such as smoking cessation and weight loss has been the focus of prior studies in general population samples (Rohrbaugh et al. 2012; Romo and Dailey 2014), and recent intervention studies have attempted to teach partners more effective ways to talk with participants about negative and positive health behaviors (Patten et al. 2011; Sorkin et al. 2014; McDonnell et al. 2015). Equipping support partners and participants with effective communication skills for giving and receiving support for health behavior change may be a key mechanism of successful partner-support lifestyle interventions for obese individuals with SMI.
Some limitations of this feasibility pilot study include generalizability and inadequate statistical power. First, our sample was small involving only volunteers that were self-selected, thus limiting the generalizability of the findings. Participation was limited to participants who were already enrolled in a lifestyle intervention and who had a partner who was willing and eligible to participate in the study. We were unable to make initial contact with 19 of the In SHAPE participants referred to the study. These referrals included participants who were not engaged in the In SHAPE program with the hopes that social support would increase their engagement. It is possible that participants enrolled in the Fit Together study were generally more engaged and motivated to make health behavior changes. Future research could include strategies for making initial contact with potential support candidates first who could then help re-engage participants who may stand to benefit from a social support component to a lifestyle intervention. Despite the relatively high number of referred individuals who were excluded from the Fit Together study (n = 43), only 14% of participants were excluded due to the self-selected partner declining to participate (n = 6). Our sample was representative of the local population but was racially homogeneous. How differences in variables related to culture, race, and ethnicity might have an impact on the viability of the intervention in a more diverse sample of people with SMI is unknown. Second, this study was not designed to perform formal hypothesis testing and thus, the results should be interpreted with caution. The number of participants is consistent with the intent of pilot studies as an initial step in exploring the feasibility and potential benefits of a novel intervention (Leon et al. 2011). Future studies with larger sample sizes and randomized designs are needed to evaluate the effectiveness of partner-support interventions in improving health outcomes for individuals with SMI.
Conclusions
Developing new approaches to increasing the potency and long-term effectiveness of lifestyle interventions targeting weight loss and decreased cardiovascular risk among overweight and obese individuals with SMI is a public health priority. This pilot study investigated a novel partner support intervention designed to augment a healthy lifestyle intervention for overweight and obese individuals with SMI. The majority of participants reported that the program was useful, convenient, and helped them reach their goals, almost one-third of participants achieved clinically significant weight loss, and significant increases in partner support for exercise and use of persuasive social support strategies were observed. Participants recruited for this study may represent individuals with SMI who are highly motivated to change their health behaviors, thus limiting the generalizability of this study to similarly motivated individuals. Recruitment and retention in social support components to lifestyle interventions could be strengthened in future studies by collaborative efforts by providers to inform participants about the study and by leveraging social support partners as allies in efforts to increase participant engagement in program sessions and lifestyle change behaviors. Social interventions that promote exercising together and positive communication may be effective for helping individuals with SMI initiate and sustain health behavior change necessary to reduce cardiovascular risk.
References
- Aschbrenner K, Carpenter-Song E, Mueser K, Kinney A, Pratt S, Bartels S. A qualitative study of social facilitators and barriers to health behavior change among persons with serious mental illness. Community Mental Health Journal. 2013;49(2):207–212. doi: 10.1007/s10597-012-9552-8. [DOI] [PubMed] [Google Scholar]
- Aschbrenner K, Mueser K, Bartels S, Carpenter-Song E, Pratt S, Barre LK, et al. The other 23 hours: A qualitative study of fitness provider perspectives on social support for health promotion for adults with mental illness. Health and Social Work. 2015;40(2):91–99. doi: 10.1093/hsw/hlv006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschbrenner K, Mueser KT, Naslund JA, Gorin AA, Kinney A, Daniels L, et al. Feasibility study of increasing social support to enhance a healthy lifestyle intervention for individuals with serious mental illness. Journal of the Society for Social Work and Research. 2016;7(2):289–313. doi: 10.1086/686486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balke B. Report Civil Aeromedical Research Institute US. 1963. A simple field test for the assessment of physical fitness. REP 63–6; pp. 1–8. [PubMed] [Google Scholar]
- Barre LK, Ferron JC, Davis KE, Whitley R. Healthy eating in persons with serious mental illnesses: Understanding and barriers. Psychiatric Rehabilitation Journal. 2011;34(4):304–310. doi: 10.2975/34.4.2011.304.310. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Jue K, Wolfe RS, et al. Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatric Services. 2013;64(8):729–736. doi: 10.1176/appi.ps.003622012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Naslund JA, Wolfe R, et al. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. The American Journal of Psychiatry. 2015;172(4):344–352. doi: 10.1176/appi.ajp.2014.14030357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beriault K, Carpentier AC, Gagnon C, Menard J, Baillargeon JP, Ardilouze JL, et al. Reproducibility of the 6-minute walk test in obese adults. International Journal of Sports Medicine. 2009;30(10):725–727. doi: 10.1055/s-0029-1231043. [DOI] [PubMed] [Google Scholar]
- Blackburn G. Effect of degree of weight loss on health benefits. Obesity Research. 1995;3(Suppl 2):211s–216s. doi: 10.1002/j.1550-8528.1995.tb00466.x. [DOI] [PubMed] [Google Scholar]
- Citation A. Feasibility of popular m-health technologies for activity tracking among individuals with serious mental illness. Telemedicine Journal and e-Health. 2015;21(3):213–216. doi: 10.1089/tmj.2014.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Preventing Chronic Disease. 2006;3(2):A42. [PMC free article] [PubMed] [Google Scholar]
- Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, et al. A behavioral weight-loss intervention in persons with serious mental illness. The New England Journal of Medicine. 2013;368(17):1594–1602. doi: 10.1056/NEJMoa1214530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner G, Cohn T, Remington G. Validation of a physical activity assessment tool for individuals with schizophrenia. Schizophrenia Research. 2006;82(2–3):225–231. doi: 10.1016/j.schres.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Fildes A, Charlton J, Rudisill C, Littlejohns P, Prevost AT, Gulliford MC. Probability of an obese person attaining normal body weight: Cohort study using electronic health records. American Journal of Public Health. 2015;105(9):e54–e59. doi: 10.2105/AJPH.2015.302773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Powers TA, Koestner R, Wing RR, Raynor HA. Autonomy support, self-regulation, and weight loss. [Randomized Controlled Trial Research Support, N.I.H., Extramural] Health Psychology. 2014;33(4):332–339. doi: 10.1037/a0032586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Raynor HA, Fava J, Maguire K, Robichaud E, Trautvetter J, et al. Randomized controlled trial of a comprehensive home environment-focused weight-loss program for adults. [Randomized Controlled Trial Research Support, N.I.H., Extramural] Health Psychology. 2013;32(2):128–137. doi: 10.1037/a0026959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CA, Yarborough BJ, Leo MC, Yarborough MT, Stumbo SP, Janoff SL, et al. The STRIDE weight loss and lifestyle intervention for individuals taking antipsychotic medications: A randomized trial. The American Journal of Psychiatry. 2015;172(1):71–81. doi: 10.1176/appi.ajp.2014.14020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SE, Steptoe A, Wardle J. The influence of partner’s behavior on health behavior change: The English longitudinal study of ageing. JAMA Intern Med. 2015 doi: 10.1001/jamainternmed.2014.7554.. [DOI] [PubMed] [Google Scholar]
- Larsson UE, Reynisdottir S. The six-minute walk test in outpatients with obesity: Reproducibility and known group validity. Physiotherapy Research International. 2008;13(2):84–93. doi: 10.1002/pri.398. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Knowlton AR. Social network assessments and interventions for health behavior change: A critical review. Behavioral Medicine. 2015;41(3):90–97. doi: 10.1080/08964289.2015.1034645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Davis LL, Kraemer HC. The Role and interpretation of pilot studies in clinical research. Journal of Psychiatric Research. 2011;45(5):626–629. doi: 10.1016/j.jpsychires.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logue E, Sutton K, Jarjoura D, Smucker W, Baughman K, Capers C. Transtheoretical model-chronic disease care for obesity in primary care: A randomized trial. Obesity Research. 2005;13(5):917–927. doi: 10.1038/oby.2005.106. [DOI] [PubMed] [Google Scholar]
- Martire LM, Stephens MA, Mogle J, Schulz R, Brach J, Keefe FJ. Daily spousal influence on physical activity in knee osteoarthritis. Annals of Behavioral Medicine. 2013;45(2):213–223. doi: 10.1007/s12160-012-9442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonnell KK, Hollen PJ, Heath J, Andrews JO. Recruiting family dyads facing thoracic cancer surgery: Challenges and lessons learned from a smoking cessation intervention. European Journal of Oncology Nursing. 2015 doi: 10.1016/j.ejon.2015.08.006.. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Glynn SM. Behavioral family therapy for psychiatric disorders. Oakland: New Harbinger Publications; 1999. [Google Scholar]
- Mueser KT, Glynn SM, Liberman RP. Behavioral family management for serious psychiatric illness. New Directions for Mental Health Services. 1994;62:37–50. doi: 10.1002/yd.23319946206. [DOI] [PubMed] [Google Scholar]
- Patten CA, Smith CM, Brockman TA, Decker PA, Hughes CA, Nadeau AM, et al. Support-person promotion of a smoking quitline: A randomized controlled trial. American Journal of Preventive Medicine. 2011;41(1):17–23. doi: 10.1016/j.amepre.2011.03.012. [DOI] [PubMed] [Google Scholar]
- Rasekaba T, Lee AL, Naughton MT, Williams TJ, Holland AE. The six-minute walk test: A useful metric for the cardiopulmonary patient. Internal Medicine Journal. 2009;39(8):495–501. doi: 10.1111/j.1445-5994.2008.01880.x. [DOI] [PubMed] [Google Scholar]
- Rohrbaugh MJ, Shoham V, Skoyen JA, Jensen M, Mehl MR. We-talk, communal coping, and cessation success in a couple-focused intervention for health-compromised smokers. Family Process. 2012;51(1):107–121. doi: 10.1111/j.1545-5300.2012.01388.x. [DOI] [PubMed] [Google Scholar]
- Romo LK, Dailey RM. Weighty dynamics: Exploring couples’ perceptions of post-weight-loss interaction. Health Communication. 2014;29(2):193–204. doi: 10.1080/10410236.2012.736467. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine. 1987;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- Scott D, Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues in Mental Health Nursing. 2011;32(9):589–597. doi: 10.3109/01612840.2011.569846. [DOI] [PubMed] [Google Scholar]
- Shiner B, Whitley R, Van Citters AD, Pratt SI, Bartels SJ. Learning what matters for patients: Qualitative evaluation of a health promotion program for those with serious mental illness. Health Promotion International. 2008;23(3):275–282. doi: 10.1093/heapro/dan018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorkin DH, Mavandadi S, Rook KS, Biegler KA, Kilgore D, Dow E, et al. Dyadic collaboration in shared health behavior change: The effects of a randomized trial to test a lifestyle intervention for high-risk Latinas. [Randomized Controlled Trial Research Support, N.I.H., Extramural] Health Psychology. 2014;33(6):566–575. doi: 10.1037/hea0000063. [DOI] [PubMed] [Google Scholar]
- Stephens MA, Fekete EM, Franks MM, Rook KS, Druley JA, Greene K. Spouses’ use of pressure and persuasion to promote osteoarthritis patients’ medical adherence after orthopedic surgery. Health Psychology. 2009;28(1):48–55. doi: 10.1037/a0012385. [DOI] [PubMed] [Google Scholar]
- Stephens MA, Franks MM, Rook KS, Iida M, Hemphill RC, Salem JK. Spouses’ attempts to regulate day-to-day dietary adherence among patients with type 2 diabetes. Health Psychology. 2013;32(10):1029–1037. doi: 10.1037/a0030018. [DOI] [PubMed] [Google Scholar]
- Suetani S, Whiteford HA, McGrath JJ. An urgent call to address the deadly consequences of serious mental disorders. JAMA Psychiatry. 2015;72(12):1166–1167. doi: 10.1001/jamapsychiatry.2015.1981. [DOI] [PubMed] [Google Scholar]
- Sutton K, Logue E, Jarjoura D, Baughman K, Smucker W, Capers C. Assessing dietary and exercise stage of change to optimize weight loss interventions. Obesity Research. 2003;11(5):641–652. doi: 10.1038/oby.2003.92.. [DOI] [PubMed] [Google Scholar]
- Van Citters AD, Pratt SI, Jue K, Williams G, Miller PT, Xie H, et al. A pilot evaluation of the In SHAPE individualized health promotion intervention for adults with mental illness. Community Mental Health Journal. 2010;46(6):540–552. doi: 10.1007/s10597-009-9272-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams GC, Lynch MF, McGregor HA, Ryan RM, Sharp D, Deci EL. Validation of the” Important Other” climate questionnaire: Assessing autonomy support for health-related change. Families, Systems, and Health. 2006;24(2):179. [Google Scholar]
- Williams GC, Niemiec CP, Patrick H, Ryan RM, Deci EL. The importance of supporting autonomy and perceived competence in facilitating long-term tobacco abstinence. Annals of Behavioral Medicine. 2009;37(3):315–324. doi: 10.1007/s12160-009-9090-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. Journal of Consulting and Clinical Psychology. 1999;67(1):132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- Wing RR, Lang W, Wadden TA, Safford M, Knowler WC, Bertoni AG, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–1486. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarborough BJ, Stumbo SP, Yarborough MT, Young TJ, Green CA. Improving lifestyle interventions for people with serious mental illnesses: Qualitative results from the STRIDE study. Psychiatric Rehabilitation Journal. 2015 doi: 10.1037/prj0000151. [DOI] [PMC free article] [PubMed] [Google Scholar]