Diabetes mellitus is a growing public health concern and a chronic metabolic disease worldwide. The most common clinical manifestations at the onset of diabetes are blurry vision, weight loss, polyuria, polydipsia, and polyphagia. Neurological symptoms are rare but have been reported to be associated with initial presentation of type 2 diabetes, especially hyperglycemic hyperosmolar nonketotic syndrome (HHNS). Hemichorea-hemiballism (HCHB) is a spectrum of involuntary, continuous, nonpatterned movements involving one side of the body that is usually caused by a variety of hereditary neurological diseases, metabolic disorders, post-rheumatic fever sequelae, strokes, and other vascular diseases. Herein, we report the case of a man with left-side arm hemichorea (HC) who presented with HHNS and had resolution of his symptoms when his blood glucose was back under control. This case report highlights the association between HC and HHNS and reinforces the need to recognize HHNS promptly, especially in elderly patients who present with a neurological complaint.
Presentation
A 72-year-old Caucasian man presented with a 2-week history of progressive writhing movements of his left arm, with occasional sudden amplitude excursions, associated with polyuria, polydipsia, and unintentionally weight loss of 10 lb. On admission, his vital signs included a body temperature of 96.5°F, blood pressure of 124/80 mmHg, heart rate of 70 bpm, and respiration rate of 18 breaths/min. His physical examination was positive for sporadic twisting movements of the left forearm and hand, signs of lower-extremity peripheral vascular disease, and decreased sensation of vibration in a sock distribution.
Initial laboratory test results included a serum random glucose of 873 mg/dL, A1C of 13.2%, serum osmolality of 335 mOsm/kg, anion gap of 24 mEq/L, and venous pH of 7.35. A head CT scan showed signs of small-vessel ischemic disease without evidence of acute intracranial pathology (Figure 1). Given these findings, the patient was admitted to the intensive care unit and started on insulin infusion and intravenous fluids.
FIGURE 1.
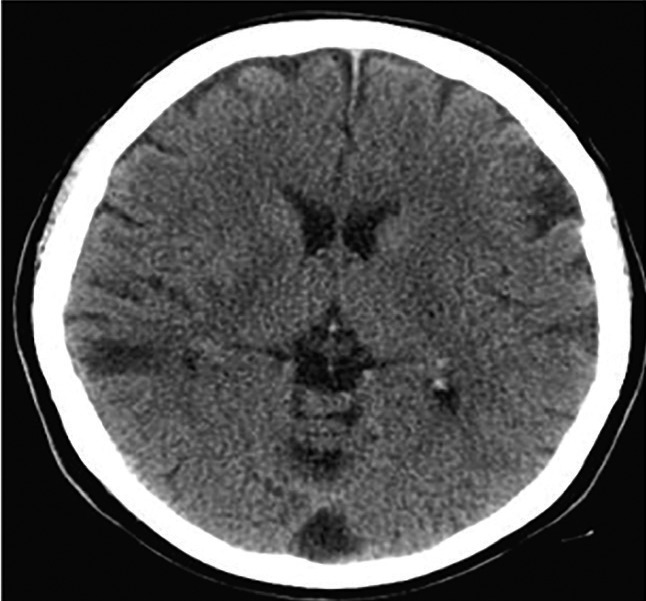
Head CT scan shows chronic small-vessel ischemic disease.
A brain MRI ordered as part of the initial evaluation showed no acute cerebral abnormalities. An electroencephalogram and lumbar puncture were ordered to rule out seizures and cerebrospinal fluid infection, respectively, and both yielded normal results.
Within a few days, the patient’s glucose decreased to 170 mg/dL and his left forearm movements had almost disappeared; by day 5, the HC was completely resolved.
One-month follow-up occurred via a telephone call because the patient had decided to go to a different provider closer to his home for future care. He reported that he had continued to be asymptomatic.
Questions
Why is it important to screen patients who present with movement disorders for diabetes?
What radiological clues help in identifying HC as part of HHNS, and are those finding necessary to make a diagnosis?
What could explain the link between HHNS and HCHB?
Commentary
Chorea secondary to hyperglycemia was first reported in 1960 (1). Most of the cases reported to date have been secondary to HHNS in type 2 diabetes patients, and some have been the first indication of hyperglycemia (2). The average age of onset for HC secondary to HHNS is 71 years, with a female-to-male ratio of 1.8:1. Most cases occur in Asian women and the elderly (2,3). The mean A1C on presentation is 14%. Typically, in patients with HHNS chorea, hyperintensities of the contralateral basal ganglia are found on T1-weighted MRI with hypointensities found on T2-weighted MRI. However, the lack of these findings does not rule out this syndrome.
The exact pathophysiology of HCHB remains unclear (4). Hyperglycemia induces cerebral hypoperfusion and activates the anaerobic pathway, causing a decrease in the level of gamma-aminobutyric acid (GABA) in basal ganglia neurons, which in turn causes a reduction in acetylcholine synthesis. GABA is the main inhibitory neurotransmitter in the basal ganglia (4,5). Hyperviscosity induced by hyperglycemia causes a disruption of the blood-brain barrier, triggering a transient ischemic event in vulnerable striatal neurons. This could cause the astrocytic hypertrophy and edema that result in the characteristic MRI changes (6,7). Putaminal petechial hemorrhage has been also suggested as a possible mechanism for HCHB, given the findings of hyperintensity found on brain CT scans (8).
Overall, the prognosis of HHNS-induced chorea is excellent, with rare exceptions (9), and depends on proper identification of undiagnosed diabetes and adequate control of blood glucose. Additionally, typical neuroleptic drugs and sometimes benzodiazepines are useful in the treatment of choreic movements (4). A follow-up brain MRI after 6 months will usually show resolution of the initial findings, but these abnormalities may persist for years.
Clinical Pearls
HC associated with HHNS is a rare manifestation of type 2 diabetes that usually occurs in female Asian and elderly individuals.
Patients who present with movement disorders should be screened for diabetes.
Brain imaging generally shows contralateral basal changes to the side of neurological findings. However, a lack of abnormalities on imaging is not uncommon.
Prompt diagnosis and treatment of hyperglycemia leads to complete resolution of symptoms.
Conclusion
This case underscores the importance of recognizing atypical manifestations of diabetes to initiate prompt evaluation, avoid long-term complications, and decreased hospital-related health costs.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Bedwell SF. Some observations on hemiballismus. Neurology 1960;10:619–622 [DOI] [PubMed] [Google Scholar]
- 2.Prabhu S, Ramya N. Movement disorders and diabetes: a study of South India. Internet J Neurol 2012;14 [Google Scholar]
- 3.Song CG, Yang X, Xing GH, Zhao CS. Hemichorea associated with nonketotic hyperglycemia in a female. Neuro Endocrinol Lett 2012;33:489–492 [PubMed] [Google Scholar]
- 4.Chang CV, Felicio AC, Godeiro CDO Jr, et al. Chorea-ballism as a manifestation of decompensated type 2 diabetes mellitus. Am J Med Sci 2007;333:175–177 [DOI] [PubMed] [Google Scholar]
- 5.Nath J, Jambhekar K, Rao C, Armitano E. Radiological and pathological changes in hemiballism-hemichorea with striatal hyperintensity. J Magn Reson Imaging 2006;23:564–568 [DOI] [PubMed] [Google Scholar]
- 6.Slabu H, Savedia-Cayabyab S, Senior P, Arnason T. Permanent haemichorea associated with transient hyperglycemia. BMJ Case Rep 2011. (DOI: 10.1136/bcr.08.2011.4641) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shan DE, Ho DM, Chang C, Pan HC, Teng MM. Hemichorea-hemiballism: an explanation for MR signal changes. Am J Neuroradiol 1998;19:863–870 [PMC free article] [PubMed] [Google Scholar]
- 8.Chang MH, Chian HT, Lai PH, Sy CG, Lee SS, Lo YY. Putaminal petechial haemorrhage as the cause of chorea: a neuroimaging study. J Neurol Neurosurg Psychiatry 1997;63:300–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oh SH, Lee KY, Im JH, Lee MS. Chorea associated with non-ketotic hyperglycemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI study: a meta-analysis of 53 cases including four present cases. J Neurol Sci 2002;200:57–62 [DOI] [PubMed] [Google Scholar]


