Abstract
Purpose
Fractures of the base of the middle phalanx are particularly challenging. Dorsal fracture-subluxations/dislocations of the proximal interphalangeal joint (PIPJ) are relatively common, but the volar fracture-subluxation/dislocation, the so-called ‘central slip fracture’, is quite rare. The current study presents our experience with operatively treated patients with central slip fracture subluxation/dislocation with a minimum of one-year follow-up. We hypothesized that the majority of patients with a central slip fracture subluxations/dislocations have poor outcomes
Methods
13 patients with central slip fracture subluxations/dislocation were identified from departmental billing records between 2003 and 2013. Nine patients completed the study follow up exam and eight were included in the final analysis. Clinical data assessed included age at injury, sex, mechanism of injury, injured digit, type of treatment, additional intervention(s), complications, length of follow-up, and range of motion follow-up. Fluoroscopic images and Quick DASH surveys were obtained at study follow up.
Results
All patients underwent at least one surgery and 7 of 8 underwent open reduction. The average age at the time of injury was 41 years (range 25–60 years). All injuries were closed. The average follow up was 43 months (Range 17–67 months). Average passive and active range of motion of the proximal interphalangeal joint at follow up was 62 and 54 degrees respectively. Six of eight developed radiographic evidence of arthritic change and four patients experienced an outcome that required additional interventions.
Conclusions
Patients should be counseled about the outcomes following surgical treatment of this uncommon, difficult injury.
Introduction
Phalanx fractures are common injuries of the hand, accounting for 41% of hand fractures and up to 2.9% of emergency department visits1,2. Simple, non-displaced phalanx fractures can be treated non-operatively and typically have excellent outcomes. In contrast, articular fractures, especially those associated with joint subluxation or dislocation, are more difficult to treat and may require surgery in order to optimize outcome. Specifically, fractures of the base of the middle phalanx are particularly challenging and can lead to proximal interphalangeal joint (PIPJ) instability. Dorsal fracture-subluxations/dislocations of the PIPJ are relatively common, but the volar fracture-subluxation/dislocation, the so-called ‘central slip fracture’3, is quite rare.
In contrast to volar dislocations of the PIPJ without an associated fracture of the dorsal base of the middle phalanx4–6, central slip fracture subluxations/dislocations and their outcomes have been rarely reported in the literature3,7–10. Imatami et al. recommended open reduction and internal fixation with Kirshner-wires (K-wires) after reviewing their experience with eight central slip fractures without an associated dislocation. Though none of their patients regained their pre-operative range of motion, they reported satisfactory outcomes and none of their patient underwent additional procedures3. Rosenstadt et al. reported good or excellent outcomes with closed reduction and trans-articular K-wire fixation in 13 central slip fracture dislocations9.
Our experience in the care of these injuries has been less successful and we hypothesized that the majority of patients with a central slip fracture subluxations/dislocations have poor outcomes. The current study presents our experience in the operative treatment of patients with a central slip fracture subluxations/dislocations at a minimum of one-year follow-up.
Methods
After Institutional Review Board approval, we used departmental billing records to identify patients with a ‘central slip’ fracture-subluxation/dislocation utilizing ICD-9 code 834.02 and CPT codes 26746, 26776, 26785. There were 562 patients identified between 1/1/2003 and 12/31/2013. All charts were reviewed and 13 patients met our inclusion criteria, which included a minimum follow-up of one-year after surgery and complete medical and radiographic records. We excluded isolated volar dislocations of the PIP joint without fracture of the dorsal base of the middle phalanx and patients treated without surgery. Of the 13 patients identified, we excluded four patients who could not be located for follow-up and one patient who sustained an open central slip fracture.
We assessed the following clinical data: age, sex, mechanism of injury, injured digit, type of treatment, additional intervention(s), complications, length of follow-up, and range of motion at follow-up. We assessed fluoroscopic images for joint reduction and the presence of arthrosis, which was defined as joint space narrowing and/or osteophyte formation, at follow-up. At the follow-up evaluation, one member of the research team performed a physical examination including active and passive range of motion of the PIP joint, pain assessment, and the Quick Disability of the Arm, Shoulder, and Hand (DASH) questionnaire11. Frequency of pain was categorized as daily, weekly, monthly, or less than once per month. Pain severity was rated on a scale from zero to ten with zero representing no pain and ten representing severe pain.
In general, the post-operative protocol following open reduction and internal fixation with K-wires is to immobilize the affected finger in a splint with the K-wire in place for four to eight weeks and monitor clinical and radiographic healing and joint congruity at office visits every two weeks. K wires are removed once solid radiographic healing is evident. Once the K-wire is removed the patient is slowly advanced from gentle active range of motion exercises (no passive range of motion) to full active and passage of range of motion. For patients treated with a dynamic external fixator, early range of motion exercises are initiated at two weeks and clinical and radiographic healing and joint congruity are monitored at office visits every two weeks similar to the protocol outlined by Ruland et al12. The fixator is removed between four and six weeks. There was heterogeneity in the operative treatment of the 6 patients treated with ORIF (table 2). The five patients who did not undergo salvage procedures completed a Quick DASH at the time of their follow up visit (Patients 1, 2,3, 4, and 5). Four patients returned for follow-up fluoroscopic evaluation (Patients 1,2,4, and 5). There were 3 salvage procedures including two fusions (patients 7 and 8) and one revision amputation (patient 6). These patients did not return for repeat radiographs at greater than one year from treatment.
Table 2.
Interventions
| Table 2 | Surgery | Time to Surgery (days) | Complications | Second Procedure | Third Procedure |
|---|---|---|---|---|---|
| 1 | ORIF: k wire, suture anchor | 10 | No | No | No |
| 2 | ORIF: k wire | 9 | No | No | No |
| 3 | ORIF: k wire, suture anchor | 28 | No | No | No |
| 4 | ORIF: k wire, screw | 41 | No | No | No |
| 5 | ORIF: screw | 11 | Persistent boutonniere deformity | No | No |
| 6 | ORIF: k wires | 60 | Limited ROM 4th digit | Revision amputation | No |
| 7 | External fixation + screw | 93 | Persistent PIPJ Subluxation | Arthrodesis | No |
| 8 | External fixation | 11 | Persistent PIPJ subluxation | ORIF | Arthrodesis |
Results
Six of the eight patients sustained a fracture-subluxation of the middle phalanx and two sustained a fracture-dislocation. The central slip (CS) fragment was one large piece in six patients and comminuted in two patients. Six patients were initially treated with open reduction and internal fixation (ORIF). One patients was initially treated with open reduction, screw fixation, and external fixation, One patient was initially treated with closed reduction and external fixation12. The average age at the time of injury was 41 years (range 25–60 years). All injuries were closed. The small finger (5) was the most commonly injured digit (Table 1). Six of the eight patients had no associated injuries (Patients 2, 3, 4, 5, 7, and 8). Patient 1 had a subtrochanteric femur fracture at presentation and patient 6 had ipsilateral fourth and fifth carpal-metacarpal dislocations, a fourth metacarpal neck fracture, and proximal dorsal hand soft tissue wound. The median interval between time of injury and time of intervention was 19.5 days (range 11–93 days). K-wires were removed at an average of 38 days (range 28–54 days) after treatment. External fixators were utilized in two patients (Patients 7 and 8) both of whom were younger than 40. All patients older than 40 years of age were treated with ORIF (Table 2). Average follow up was 43 months (Range 17–67 months). The average passive and active range of motion at follow up were 62 degrees (20–82 degrees) and 54 degrees (26–80 degrees) respectively.
Table 1.
Demographics and Radiographic Findings
| Table 1 | Age (years) |
Gender* | Mechanism of Injury | Injured digit† | Arthritis at Study Follow up | Imatami Type |
|---|---|---|---|---|---|---|
| 1 | 36 | M | MVC | RF | Yes | III |
| 2 | 53 | F | Caught in Door | SF | Yes | I |
| 3 | 57 | F | Fall | SF | Yes | I |
| 4 | 46 | F | Caught in Door | SF | No | III |
| 5 | 60 | F | Fall | SF | Yes | I |
| 6 | 25 | M | Crush | RF | NA‡ | I |
| 7 | 25 | M | Unknown | RF | NA | III |
| 8 | 25 | M | Softball | SF | NA | III |
M - Male; F - Female;
LF-Long Finger; RF-Ring Finger; SF-Small Finger
NA-Not Applicable
Radiographic Follow-up
At the time of K wire removal or external fixator removal, the PIPJ was reduced in four patients (Patients 1, 2, 4, and 6), subluxated in three patients (Patients 3, 5, and 8), and dislocated in one (Patient 8). At the time of follow up, the PIPJ was reduced in three of the five patients (Patients 1,2, and 4) and subluxated in two patients (Patients 3 and 5) who did not undergo salvage procedures. Six of eight patients had radiographic evidence of arthritis prior to their salvage procedures (Patients 7 and 8) or at follow-up (Patients 1, 2, 3, and 5). One patient had radiographic PIPJ arthritis prior to treatment for the central slip fracture subluxation (Patient 3). Patient 4 did not have radiographic evidence of arthritis at follow up.
Quick DASH
The average QuickDASH score was 4.6 (Range 0–11.3). QuickDASH scores were obtained from all patients who did not undergo salvage procedures, after all treatment had been completed. Four of the six patients who did not undergo salvage procedures reported occasional pain in the affected digit, most commonly less than once per month (Patients 1,2,4, and 5). The same patients reported decreased function in the affected digit compared to the contralateral. In the remaining two patients, Patient 3 reported no pain and equal function in the affected digit compared to the contralateral.
Poor Outcomes
Four patients experienced a poor outcome that required additional intervention. One patient had a boutonniere deformity with a 40-degree contracture of the PIP joint. Splinting was ineffective in resolving this deformity but the patient did not want additional surgery (Patient 5). Three patients were treated with a salvage procedure to address pain and limited motion. One had a revision amputation (Patient 6) and two had PIPJ arthrodeses (Patients 7 and 8).
Discussion
The central slip fracture is a challenging injury. The pathomechanics of a volar PIPJ fracture-dislocation differs from a pure dislocation. Based on cadaveric experiments, Spinner and Choi hypothesized that pure volar dislocations occur as a result of a volar and a varus or valgus force (ulnar or radial angulation), which disrupts a collateral ligament and may prevent closed reduction. In contrast, the fracture-dislocation may occur when an axial and volarly directed force is applied to the PIPJ, which may avulse the central slip from the middle phalanx, with or without associated collateral ligament damage13. The fracture may be a small avulsion fragment or represent a significant portion of the dorsal base of the middle phalanx and, as a result, obtaining and maintaining alignment of the fracture and the joint is difficult.
The literature offers conflicting guidance regarding the management central slip fractures. The first description of the central slip fracture appeared in Spinner and Choi’s series of five patients with volar dislocations of the PIPJ. In their series, one 18-year-old patient sustained a central slip fracture dislocation after a fall. He was treated with open reduction with K-wires transfixing the central slip fragment and PIPJ. The trans-articular wire was removed at three weeks and the trans-fragment wire was removed at 6 weeks post-operatively. In this case, the patient recovered full range of motion at 10 months post-operatively.
Imatami et al. reviewed eight patients with central slip fractures and proposed three types of “central slip attachment fractures” with associated treatment recommendations. In their series, no patient experienced a dislocation and they do not comment on associated joint subluxation. Type 1, or avulsion-type, injuries occur because of distracting and volarly directed forces on the PIPJ. Type 2, or split-type, injuries occur as a result of distally and dorsally directed forces applied to the PIPJ, which results in a longitudinal shear force and a triangular fracture fragment attached to the central slip. Type 3, or split-depression-type, injuries occur when an axially and volarly directed force on the PIPJ results in joint depression and shear of the dorsal rim of the middle phalanx. They recommended ORIF with K-wires for all three types with the addition of bone graft to restore the PIPJ articular surface in type 3 fractures3. All of the patients in our cohort had type 1 or type 3 central slip injuries and the majority underwent open reduction and fixation (Table 1).
To date, the study by Rosenstadt et al. remains the only case series of central slip fracture dislocations with follow-up greater than one year. They reviewed 13 fractures treated with closed reduction and percutaneous K-wire fixation, when possible, with an average follow up time of 55 months. They divided their cohort into patients with acute and chronic injuries. Seven of the nine patients with acute injuries were treated with closed reduction and percutaneous K-wire fixation. Five of seven were treated with a trans-articular K-wire. Two of nine underwent open reduction and internal fixation with trans-articular K-wires and either a trans-fragment K-wire or a pull-out wire. At follow up, five of nine patients with acute injuries experienced an extension lag at the PIPJ and four of nine had a poor or fair result. They recommended closed reduction with percutaneous trans-articular K-wire fixation citing an average post-operative PIPJ range of motion of 87% of normal in the patients treated acutely.
Our experience in the treatment of central slip fracture subluxations/dislocation is similar to that reported by Rosenstadt et al as we also report unsatisfactory outcomes overall, regardless of intervention type. Six of our patients developed arthritic changes and four ultimately required a salvage procedure (amputation or arthrodesis) or had a boutonniere deformity. Average passive and active range of motion in our cohort was limited and worse than that reported by Rosenstadt et al, though it should be noted poor range of motion was not associated with disability as indicated by the QuickDASH scores in patients who did not undergo salvage procedures. There are several possible factors contributing to poor outcomes in patients with operatively treated central slip fractures including delayed diagnosis, patient age, the inherent severity of the central slip fracture, and operative treatment itself.
Delayed diagnosis was common in our cohort. The median time from injury to treatment was 19.5 days. Patients 3 and 4 did not obtain a clinic appointment until several weeks post-injury, Patient 7 experienced a delay in diagnosis due to ipsilateral hand trauma, and Patient 8 presented several months after his injury with a chronically dislocated PIPJ. After low energy trauma such as a mechanical fall or catching a finger in a door, patients may not recognize the severity of the injury until symptoms persist for weeks. The delay in prompt treatment may result in a poor outcome. Patients who underwent operative treatment within two weeks (Patients 1,2, and 5) had greater active and passive ROM than those patients with a delay in treatment greater than two weeks (Patients 3 and 4). However, given the small number of patients in study and that both groups contain patients who underwent salvage procedures (arthrodesis or amputation), who were excluded from the calculation, it is unclear how to interpret these averages. Further investigation is warranted to determine if earlier treatment affects outcome.
Patient age may also contribute to poor outcome following operative treatment. Three of the five patients younger than 40 years of age underwent a salvage procedure. However, once again we are unable to draw any firm conclusions from this study because of the small number of patients. Further investigation is warranted to determine the extent to which age affects outcomes.
Surgical treatment, especially open treatment, may lead to more extensive scar tissue, limited recovery of range of motion, and poor functional results. We could not successfully obtain fracture reduction with closed treatment in seven of our eight patients, thus leading to open reduction and fixation. Lastly, the nature of the central slip fracture may predispose patients to poor results. The size of the central slip fragment and extent of cartilage and soft tissue damage is not always readily apparent on injury radiographs.
There are several limitations to our study. We have only reviewed operatively treated central slip fractures. Due to ambiguity in the billing records, we were unable to identify the number of non-operatively treated central slip fracture subluxations/dislocations in the study period. As a result, we are unable to comment on the outcomes of non-operative treatment for these injuries. Given the rare incidence of the central slip fracture subluxation/dislocation and our small sample it was not possible to determine to what degree open treatment, age of the patient, nature of the fracture, and diagnostic delay contribute to poor outcomes and additional study is warranted. Another limitation is the use of fluoroscopy to assess joint congruity and presence of arthritis. Although it is routine in our practice to obtain fluoroscopic views in the office setting, there is no doubt that fluoroscopy is inferior to standard radiographs. Additionally, our sample is heterogeneous, comprised of patients of different ages, injury mechanisms, time intervals from injury to treatment, and treatment modalities. This heterogeneity was unavoidable given the rare incidence of the central slip fracture and it does limit the generalizability of our study.
In summary, outcomes following surgical treatment of the volar fracture subluxation/dislocation are poor. Although patients who did not undergo salvage procedures reported limited disability, range of motion was poor and some patients required salvage procedures due to pain and limited motion. We believe the nature of the injury and delayed presentation contribute to these outcomes. With the limitations of the study in mind, we recommend acute closed reduction and trans-articular pinning if possible, based on our experience and review of the literature. We do feel younger patients with closed injuries treated promptly will have more satisfactory outcomes than older patients with more chronic injuries however, no matter the presentation, we recommend lengthy discussion with the patient to discuss the difficult nature of this fracture and the expected poor outcomes following surgical treatment. Most patients develop arthritis in the short (six months to one year) to mid-term (one to two year) time frame and some patients will require salvage procedures.
Figure 1.
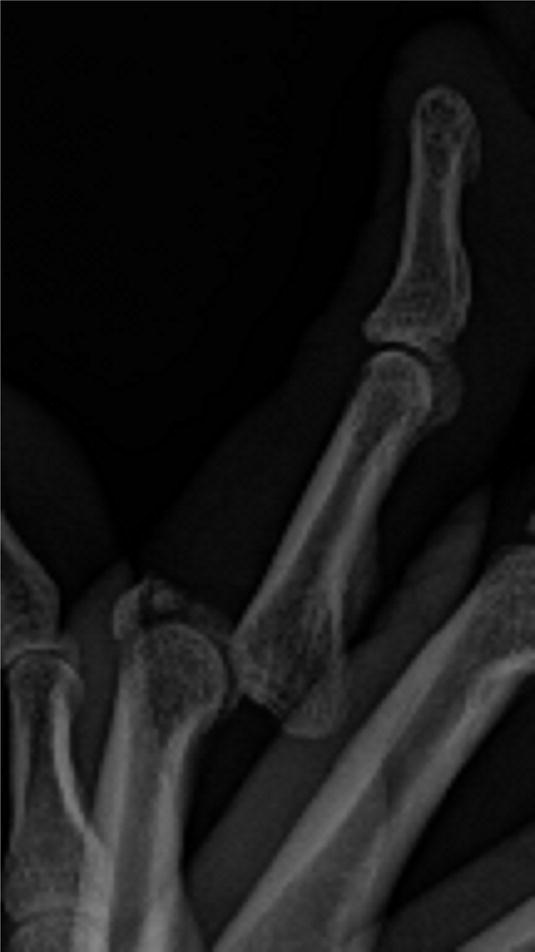
A Central Slip Fracture Dislocation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Level of Evidence V Therapeutic
References
- 1.De Jonge J, Kingma J, Van Der Lei B, Klasen H. Phalangeal Fractures of the Hand An analysis of gender and age-related incidence and aetiology. J Hand Surg Br Eur Vol. 1994;19(2):168–170. doi: 10.1016/0266-7681(94)90157-0. [DOI] [PubMed] [Google Scholar]
- 2.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg. 2001;26(5):908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 3.Imatami J, Hashizume H, Wake H, Morito Y, Inoue H. The central slip attachment fracture. J Hand Surg Br Eur Vol. 1997;22(1):107–109. doi: 10.1016/S0266-7681(97)80032-0. [DOI] [PubMed] [Google Scholar]
- 4.Johnson FG, Greene MH. Another Cause of Irreducible Dislocation of the Proximal Interphalangeal Joint of a Finger. J Bone Jt Surg Am. 1966;48(3):542–544. [PubMed] [Google Scholar]
- 5.Meyn MAJ. Irreducible Volar Dislocation of the Proximointerphalangeal Joint. Clin Orthop. 1981;158 [PubMed] [Google Scholar]
- 6.Jones NF, Jupiter JB. Irreducible palmar dislocation of the proximal interphalangeal joint associated with an epiphyseal fracture of the middle phalanx. J Hand Surg. 1985;10(2):261–264. doi: 10.1016/s0363-5023(85)80118-0. [DOI] [PubMed] [Google Scholar]
- 7.Kilgore ES, Jr, Newmeyer WL, Brown LG. Post-Traumatic Trapped Dislocations of the Proximal Interphalangeal Joint. J Trauma Acute Care Surg. 1976;16(6) doi: 10.1097/00005373-197606000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Baugher WH, McCue FC. Anterior fracture-dislocation of the proximal interphalangeal joint. A case report. J Bone Jt Surg Am. 1979;61(5):779–778. [PubMed] [Google Scholar]
- 9.Rosenstadt BE, Glickel SZ, Lane LB, Kaplan SJ. Palmar fracture dislocation of the proximal interphalangeal joint. J Hand Surg. 1998;23(5):811–820. doi: 10.1016/S0363-5023(98)80155-X. [DOI] [PubMed] [Google Scholar]
- 10.Wilson JN, Rowland SA. Fracture-Dislocation of the Proximal Interphalangeal Joint of the Finger. J Bone Jt Surg Am. 1966;48(3):493–502. [PubMed] [Google Scholar]
- 11.Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 12.Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. J Hand Surg. 2008;33(1):19–25. doi: 10.1016/j.jhsa.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 13.Spinner M, Choi BY. Anterior Dislocation of the Proximal Interphalangeal Joint. J Bone Jt Surg Am. 1970;52(7):1329–1336. [PubMed] [Google Scholar]


