Abstract
New evidence suggests that reductions in sedentary behavior may increase physical activity and improve health. These findings point to new behavioral targets for intervention and new ways to think about intervening to increase overall physical activity in the population. This report provides a knowledge update reflecting the rapid accumulation of new evidence related to sedentary behavior and health among adults. Recent observational studies suggest that leveraging the time-inverse relationship between sedentary and active behaviors by replacing sitting with standing, light or moderate-intensity activity can have important health benefits, particularly among less active adults. Clinical studies are providing evidence of the probable physiologic mechanisms underlying these associations, as well as insights into the cardiometabolic impact of breaking up and reducing sedentary behavior. In contrast to the well-established behavioral theories that guide the development and dissemination of evidence-based interventions to increase moderate-vigorous intensity physical activity (MVPA), much less is known about how to reduce sedentary time in order to increase daily activities. It has become clear that the environmental, social and individual level-determinants for sedentary time are distinct from those linked to the adoption and maintenance of MVPA. As a result, novel intervention strategies that focus on sitting and lower intensity activities by leveraging the surrounding environment (e.g., workplace, school, home) as well as individual-level cues and habits of sedentary behavior are being tested to increase the potency of interventions designed to increase overall physical activity. Herein we summarize the solutions-oriented research across the behavioral research framework, with a focus on highlighting areas of synergy across disciplines and identifying gaps for future research.
Keywords: sedentary behavior, exercise, behavior change, Epidemiology, clinical studies, intervention
Introduction
Behaviors done while sitting or reclining that require little energy expenditure (i.e., sedentary behaviors), are ubiquitous in modern societies. Western populations spend an average of 8.5 hours/day—nearly 60 hours/week—sedentary (12). Higher levels of sedentary behavior are associated with increased risk for type 2 diabetes, cardiovascular disease, some cancers and mortality, even after accounting for participation in recommended amounts of moderate-vigorous intensity activity (i.e., ≥3 METs) e.g., (6, 27). In daily life sedentary behaviors are tightly linked in a zero-sum time-use relationship with overall physical activity (13), getting up out of your chair invariably results in increased physical activity, albeit typically of a low intensity. The evidence linking sitting to poor health therefore suggests that health benefits may be derived from many lower intensity physical activities of everyday living if they displace or disrupt prolonged sitting. For clarity and contrast, we refer to recommended amounts of moderate-vigorous intensity activity as “exercise” and use the terms sitting and sedentary behavior interchangeably throughout this paper (60). To date, efforts to increase physical activity in the population have largely focused on increasing moderate-vigorous intensity activity (60), with little attention to reducing sedentary behavior or increasing lower intensity physical activity. Thus, efforts that target sedentary behavior as a means to increase physical activity is a new behavioral leverage-point that could help us increase overall physical activity and induce health benefits within the population.
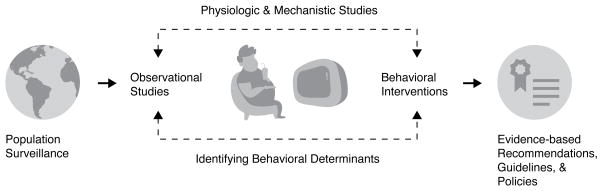
The compelling evidence linking sedentary behavior to poor health has stimulated intensive research across the spectrum of public health and biomedical research disciplines. Figure 1 borrows from the framework presented by Owen et al., (58) to illustrate the dynamic and synergistic research ecosystem that has developed across diverse fields including epidemiology, physiology, medicine, and behavioral science, which have collectively evolved into a coherent evidence-base that has started to inform public health policy (10). Importantly, it is becoming clear that the environmental, social and individual level-factors that positively or negatively influence how much time is spent in sedentary behavior (i.e., the determinants of behavior) time are distinct from the factors linked to the adoption and maintenance of exercise (43). For example, environmental and contextual factors (i.e., external cues, personal habits) may play an even larger role in determining sedentary behavior than for exercise (18, 58). As a result, novel intervention strategies that leverage the surrounding environment (e.g., workplace, school, home) as well as individual-level cues and habits of sedentary behavior are now being tested to increase the potency of behavioral interventions designed to increase overall daily activity (18, 47, 48). These findings suggest a number of new intervention approaches that could be important adjuncts to efforts to increase moderate-vigorous intensity lifestyle activities or aerobic exercise (24, 42) by harnessing powerful additional health benefits of lower intensity physical activities of everyday living.
Figure 1.
Framework for the science of sedentary behavior encompassing epidemiological, physiological, behavioral and translational research disciplines
This report is based on a Symposium entitled, “Targeting Sitting to Increase Activity and Improve Health” from the 2016 American College of Sports Medicine Meeting and provides a state of knowledge update reflecting the rapid accumulation of new evidence related to sedentary behavior and health among adults. This is not intended to be a systemic review of all studies in each of these research areas, but rather our objectives are to discuss the integration and synergies between the aforementioned research disciplines that are illustrated in Figure 1. We focus on summarizing important new findings within the rapidly advancing science in each of these important areas of inquiry, and discuss how strategies to decrease sedentary time complement and extend existing strategies to increase exercise. We also identify the current research gaps and discuss how each of these distinct areas of research can inform each other to promote evidence-based public health and policy approaches to target sitting and improve population health.
Observational Epidemiologic Studies Linking Sedentary Behavior to Poor Health
In the last decade, a large body of observational evidence has emerged indicating that excessive daily sitting time and sedentary television viewing are associated with early mortality and poor health. This evidence has been summarized in several recent meta-analyses e.g., (6, 29, 67). For example, Biswas and colleagues reported a 22% increased mortality risk among those reporting more sedentary time, based on 14 prospective studies published since 2008 (6). Additional meta-analyses have found increased risk for colon and endometrial cancer, type 2 diabetes and CVD (6, 67) and six additional causes of death have been linked to high amounts of television viewing (39). All of the meta-analyses evaluated results after adjustment for time spent in exercise. In a harmonized meta-analysis of 13 prospective studies, Ekelund and colleagues reported that exercise at levels two to three times greater than the current recommendations (>35.5 MET-hrs/wk, or 60–75 min/day or walking) were needed to eliminate the excess mortality risk associated with sitting more than 8 hrs/d and to substantially lower risk from TV viewing more than 5hrs/day (27). Collectively, this evidence indicates that recommended levels of exercise (7.5–15 MET-hrs/wk) do not fully protect against the hazards of too much sitting, and that the adverse effects of sitting are stronger for those who were physically inactive (i.e., no exercise) compared to those who are active (6). Previous research has reviewed this evidence and identified important gaps, including a need for better measures of sitting and understanding why associations are stronger for TV as compared to other sitting measures (6, 27). The next logical question becomes what type and intensities of physical activity should be promoted to replace sedentary behaviors in order to increase daily activity and achieve health benefits?
Estimating the health impact of replacing sedentary time
A number of epidemiologic studies have now examined whether there are benefits for replacing sedentary time with a broad range of physical activities. In 2009, Mekary and colleagues applied substitution models, an approach that statistically estimated the health impact of replacing an equal amount of time in one type of behavior with an equal amount of time in another while holding the effects of each type of activity and total time constant (55). Although this method can only estimate the potential benefits of reducing sedentary time, not the actual impact of changing behavior on health, it provides useful insight, particularly about hard disease end-points that are not typically evaluated in experimental trials. Numerous cross-sectional studies and several prospective studies over the past five years have used this approach, and we highlight a few papers that reflect important findings of this new research.
In the largest isotemporal study to date involving over 150,000 individuals and 20,000 deaths, Matthews and colleagues reported a 42% mortality reduction for replacing 1 hr/d of sitting with 1 hr/d of exercise among low-active individuals (<2 hours/day of total activity) and a 20% mortality benefit for replacing sitting with 1 hr/d of light-intensity activity. For more active individuals (i.e., ≥2 hours/day of total activity), the only mortality benefit was a 9% lower risk for replacing 1/hr day of sitting with exercise (52). Similar analyses were conducted in NHANES, a nationally representative survey of US adults using hip-worn accelerometer-derived measures of sedentary time and activity and reported mortality benefits for replacing sedentary with light and moderate-intensity activity (28, 51). Matthews et al. again found that replacing 1 hr/d of sedentary time with 1 hr/d of either light or moderate-vigorous intensity activity was associated with 18% and 42% lower mortality, respectively among less active adults, as determined by median split of < 5.8 hrs/d of total activity (51). For more active adults, who were already at 50% lower risk, there was no mortality benefit for replacing sedentary time with additional light or moderate-vigorous activity (51), findings consistent with dose-response relations with mortality for moderate-vigorous intensity exercise (1, 30) and cardiorespiratory fitness (7). A consistent finding across these studies is that less active people benefit the most from replacing sedentary behavior with both light and moderate-vigorous intensity physical activity.
Investigators have also used isotemporal models to estimate the impact of replacing sitting with stepping/walking or standing, as standing has also been linked with lower mortality (37). In a large sample of Australian adults, Stamatakis et al. showed mortality benefits for replacing sitting with either standing (4% lower risk) or walking (10% lower risk) based on self-report questionnaires (71). In a cross-sectional study using the activPAL monitor, Healy et al. showed beneficial impact of replacing sitting with either standing or stepping on HDL cholesterol and triglycerides. However, for BMI and waist circumference replacing sitting with stepping was beneficial while replacement with standing was not (32). These findings are consistent with the experimental evidence described below that shows benefits of replacing sitting with standing for cardiometabolic risk factors, despite little difference in energy expenditure.
As our measurement tools that capture the full waking day (as well as sleep) expand, statistical methodology to deal with such data is an important area of future research. Compositional data have also been used to estimate behavioral trade-offs in relation to disease biomarkers (16) and have reported similar conclusions as the isotemporal analyses, showing benefits for replacing sedentary with light activity and typically stronger associations for replacement with moderate-vigorous intensity (11, 16). It is not currently known whether there are optimal distributions of active and sedentary time for specific health outcomes. There are likely thresholds at both the low and high end of the intensity spectrum; as an extreme example, 16 hours of continuous sitting and 16-hrs of running are both infeasible and likely associated with poor health outcomes. To date, questionnaire-based measures have been unable to measure the full intensity spectrum with enough precision to estimate these balance points, but this is an important area of future research that may be feasible using activity monitors. Additionally, although results from these studies have begun to explore the health trade-offs between sedentary and active behaviors, it is important to note that all of the studies described above have employed statistical models to estimate the probable health benefits of replacing sitting for activity, but not the health effects of actual changes in behavior.
Changes in sedentary time in relation to health
A few prospective studies have measured total sitting time and television viewing at multiple time-points allowing researchers to estimate the health effects of increasing or decreasing sedentary behavior over time. In the largest study to date, Keadle et al. evaluated older (50–71y) US adults, who reported television viewing time at two time-points (8 years apart) who then were followed for mortality for an additional 6 years (38). Compared to adults who consistently watched television < 3 h/day, those who increased viewing time from less than 3 h/day to 3–4 h/day had an 18% greater mortality risk and those who increased from < 3 to more than 5 h/day had a 45% greater risk (38). Conversely, reducing television viewing from 5+ h/day to either 3–4 h/d or less than 3 h/day was associated with 10–15% lower mortality. Importantly, these results were adjusted for many possible confounding factors as well as changes in exercise over time. Two studies have examined changes in overall sitting and mortality. In a cohort of older Spanish adults, Leon-Munoz et al. reported a 14% reduction in all-cause mortality among those who decreased sitting time, though the association did not reach statistical significance (46). In the Women’s Health Initiative study, Lee et al. compared women who maintained high levels of sitting (>10 h/day) over 6 years to women who reduced sitting to <9 h/day over time and found that women who reduced their sitting had a 35% lower mortality (45). These findings are consistent with several prospective studies that demonstrated increasing sedentary time and televising viewing are associated with adverse changes in cardiovascular disease and breast cancer biomarkers (e.g., (76, 77)).
Prospective epidemiologic studies remain the primary source of information about the link between sedentary behavior and risk for developing or dying from disease. Results from these natural experiments that prospectively investigate changes in sedentary behavior provide a preliminary estimate of the mortality benefits that might be expected from efficacious interventions. Future intervention studies targeting television viewing or sedentary time in relation to intermediary biomarkers will help to contextualize these findings in a mechanistic framework. In the next section we describe results from experimental studies that provide insight into the biological mechanisms underlying these associations suggested by the observational literature.
Physiologic and Mechanistic Studies: Solutions-based Experimental Studies
Epidemiological evidence has been fundamental to the generation of specific hypotheses relating to excessive sedentary behavior, particularly the importance of reducing the overall volume of sitting time as well as avoidance of prolonged periods of unbroken sitting. In recognition that excessive sitting is a highly prevalent risk behavior, human experimental studies have begun to address the impact of prolonged sitting time on cardio-metabolic health parameters (3). The notion that prolonged sitting may have deleterious biological consequences is not considered to be ‘new’ science, since decades of experimental research into inactivity physiology has provided the platform upon which mechanistic investigations can be pursued to further elucidate the impact of prolonged sitting. Specifically, human studies involving bed rest and space flight, along with animal experimental models whereby physically inactive states have been imposed, have been able to characterize numerous biological and physiological responses. These include muscle atrophy, muscle insulin resistance, reduced capacity to use fat as a substrate or produce ATP, a shift in muscle fibers toward fast-twitch glycolytic type, ectopic fat storage and increased central and peripheral adiposity (4, 74); and in animals, suppressed lipoprotein lipase activity in skeletal muscle (5).
Building on these insights from inactivity physiology research, the recent sedentary behavior research is nuanced by an emphasis on experimental models that are solutions-focused that is, understanding the impact of various counter-measures to offset the deleterious health impacts of prolonged sitting. This focus is consistent with the broadly-stated recommendations that several countries have already started to promulgate within their physical activity guidelines to reduce the total time spent sitting, and in the case of Australian guidelines, to regularly interrupt sitting time (10). From a behavioral perspective, activity is defined as being the reciprocal of sedentary behavior (sitting). Invariably, the counter-measures employed in such studies to interrupt prolonged sitting necessitate standing and/or movement. Several randomized trials employing cross-over study designs have consistently shown clinically meaningful acute improvements in postprandial glucose metabolism following the initiation of frequent (every 20–30 min) short (2–3 min) interruptions during prolonged sitting involving either light-intensity or moderate-intensity ambulation, standing, or simple resistance activities (3). Some have also demonstrated improved responses in blood pressure (23, 44, 79, 80), lipid metabolism (22, 26, 33), hemostatic markers (34) and endothelial function (63, 73). In a recent meta-analysis of experimental studies, Chastin et al. (15) confirmed beneficial effects on glycemic control with interruptions in sitting involving both light-intensity physical activity and moderate-vigorous intensity physical activity. While the meta-analysis showed that interrupting prolonged sitting with short periods of standing did not appear to be a sufficient activity to induce acute benefits, this conclusion was based on only two studies. One more recent experimental study of overweight adults showed that replacing 2.5 hours of sitting with standing, over the course of a simulated 8-hr workday, was associated with significant improvements in blood pressure and glucose (19, 79).
Although the evidence from human experimental studies targeting reducing and interrupting prolonged sitting time is supportive of the epidemiological evidence, much still remains to be understood. To date, most experimental studies have focused on healthy or overweight/obese adults, attention should be directed at elucidating the effects in other population sub-sets, specifically those with existing chronic disease and older adults, who are the most sedentary age-group. Interestingly, two recent studies have demonstrated that the beneficial effects of breaking up prolonged sitting time on postprandial glycemia may be more pronounced in those with existing states of dysglycemia (22, 33). A randomized cross-over trial in 24 adults with type 2 diabetes demonstrated marked (~30–40%) improvements in postprandial glucose, insulin and C-peptide when 8 hours of prolonged sitting was interrupted every 30 mins with 3 min bouts of light-intensity walking, and separately also for 3 min bouts of simple resistance activities (calf raises, half-squats, gluteal contractions and knee raises) (22). Similarly, sizeable (~8–16 mmHg) reductions in blood pressure were observed for both counter-measures relative to uninterrupted sitting, with the effects being more pronounced with the simple resistance activity interruptions (23). Another laboratory-based study in 22 overweight/obese dysglycemic postmenopausal women at high risk of type 2 diabetes, showed that compared to 7.5 hrs of prolonged sitting, interrupting sitting every 30 mins for 5 mins with either standing (in a fixed position) or separately, light-intensity walking, significantly reduced postprandial glucose, insulin and nonesterified fatty acids (33). Collectively, these findings suggest that frequently breaking up prolonged sitting with light-intensity physical activities and even standing, may be of particular benefit to those who are already affected by disturbances in glucose metabolism. Furthermore, frequent interruptions in prolonged sitting involving simple resistance activities or standing may have practical advantages in specific settings such as the workplace.
These experimental studies provide important physiologic insight into the risks of sedentary time and possible types and intensities of physical activity that may mitigate the risks of sedentary behavior. Well-controlled studies can also help answer practical questions from a mechanistic standpoint, such as how frequent should breaks be? or can I sit longer if I run? Ultimately, the next critical step is to examine the transience of these physiological adaptations over time through daily exposure to reducing and frequently breaking up prolonged sitting time with brief periods of activity on various health risk markers in experimental and intervention studies.
Re-thinking behavioral determinants and frameworks to address sedentary behavior
Based on the experimental and observational evidence of the risks of sedentary behaviors, behavioral scientists have begun to test interventions that aim to reduce overall sitting time and change patterns of sedentary accumulation (i.e., breaks). Broadly, this research aims to identify; 1) if there are health benefits of reducing or breaking up sitting time; 2) how these benefits compare to traditional exercise interventions; and 3) whether interventions can be developed that promote sustained increases in both low and moderate-vigorous intensity activity. In many ways this work is an extension of seminal exercise trials in the 1990’s that showed similar improvements in cardiorespiratory fitness and blood pressure from a lifestyle exercise program that promoted integrating moderate-intensity activity into daily routines as compared to a traditional structured exercise program (24). The intervention efforts related to sedentary behavior have extend this work by identifying new behavioral targets (i.e., sitting, breaks from prolonged sitting), different behavioral determinants, and focusing on promoting standing, and lower intensity activity in addition to moderate intensity activity.
The many factors that influence health-related behaviors, like participation in regular exercise or sedentary behaviors, are commonly placed within a social-ecological framework, which posits that behavior is determined by multiple interacting factors at the individual, social, environmental (both micro- and macro-level), and policy levels. These frameworks inform our efforts to understand the factors that can influence our behavior as well as the theoretical underpinnings for our strategies to change behavior (53). Over the last 30 years we have developed a strong empirical evidence-base describing the various factors which positively and negatively influence the adoption and maintenance of exercise, especially at the individual (e.g., beliefs, health status, motivation) and social (e.g., norms, modeling) levels (40). These strategies to modify beliefs and attitudes to change behavior have been relatively successful in improving exercise behaviors and are now commonplace in population-level evidence-based programs. Interestingly, many of these same factors do not seem to predict sedentary behavior (9, 62).
The evidence available on how to effectively intervene on sedentary behavior is in its infancy compared to exercise, but much progress has been made recently. We review this evidence below, with an emphasis on how determinants- and thus intervention strategies for- sedentary behavior are unique from intervention targeting purposeful exercise. Owen et al. (2010) argued that the ubiquitous, habitual, and socially-reinforced nature of sedentary behaviors are likely to point to unique determinants that are not shared with our traditional strategies used to increase exercise participation (58). As a result, when theories and intervention approaches developed for exercise behavior have been employed to modify sedentary behavior they have been less successful (61). This may be due in part, to differences in motivational processes between exercise and sedentary behavior. The decision to exercise is often planned and effortful (at least initially) whereas the choice to sit is often spontaneous and effortless. Future theories may need to account for the ubiquitous and habitual nature of sedentary behavior in order to produce sustainable, individual-level reductions in sedentary time and therefore increases in daily physical activity.
At the environmental level, new research suggests that the determinants of sedentary behavior are unique in home, school, and workplace environments as compared to exercise; therefore, the behavioral strategies employed to reduce sedentary behavior in these diverse contexts must also be unique (21, 43). For example, macro-environmental features (i.e., built environment) have consistently been shown to be an important determinants of exercise, and the provision of physical structures (e.g., parks, sidewalks) and neighborhood destinations (e.g., mixed land use) are important to support active lifestyles (64, 65). Exercise promotion has largely focused on environmental changes within this exterior built-environment (e.g., walking paths, parks). These macro-environmental features remain an important public health focus and may play an important role in both promoting exercise and reducing sitting time (e.g., replacing sedentary driving with active transport) (65). However, on the basis of available evidence, micro-environments that make up the immediate contexts in which we live, work, and play, appear to be more important for reducing sedentary behavior. For example, in the home environment, strategies have focused on television viewing reduction (e.g., (57)). In school environments, the focus has been on broader interventions targeting changes to the school environment to increase overall activity and decrease sedentary time (e.g., (66)). Furthermore, it is likely that environmental factors that influence sedentary time are closely tied to the social and temporal contexts in which they occur, suggesting a need to consider motivational processes that vary between and within days as well.
Collectively, research suggests that simply targeting exercise behaviors will not result in an automatic decline in sedentary behavior (61). A major challenge for efforts to increase overall activity is understanding how the determinants of exercise and sedentary behavior are similar and different across the levels of the social-ecological model and ultimately developing evidence-based approaches to target both behaviors. In the next sections, we highlight new research that seeks to understand how to intervene effectively on sedentary behavior. First, we review the determinants of sedentary behavior within micro-environments, with a special focus on strategies within workplace environments where adults accumulate a high volume of sedentary time. Second, we highlight new research that considers time-varying motivational processes and dual-process approaches to identify determinants of sedentary time. Third, we present preliminary evidence that illustrates how sensitivity to the temporal dimension of sedentary behavior can produce novel intervention approaches.
New Behavioral Interventions: Changing the micro-environment where we work and live
Changes in sedentary time may need to focus on more micro-environmental changes within the home, school and workplace. Jobs requiring moderate-vigorous physical activity have reduced by 58% in the last 50 years and occupational physical activity has decreased by an estimated 142 kcal/day (17). Employed adults spend an average of 7.8 hr/day at work, which accounts for the largest portion of the day, excluding sleep (12). Workplace sedentary behavior is an important behavioral target of interest given the emerging physiological evidence and the ubiquity of sitting in most workplace environments. The evidence on workplace intervention has focused on contextual/environmental factors as primary strategies for reducing sedentary behavior.
Individual-level approaches focused on reducing sedentary behavior in the workplace have included primarily the use of computer prompts or walking or other physical activity-based interventions; however, these approaches have largely been unsuccessful (61, 69). Some have argued that, given the demands of the workplace to remain engaged in work activities, strategies must focus on environmental provisions that allow postural changes and increased activity without harming productivity. The most common environmental approach has been the use of ‘activity-permissive’ workstations (i.e., treadmill desks, pedal desks, height-adjustable workstations). Neuhaus et al. reported the results of a meta-analysis of 38 studies with a pooled effect size of 77 min reduction in sedentary time/8-h workday (56). However, other health-related outcomes showed no impact. The efficacy of the interventions reviewed was highly variable, and the authors noted large variations in study quality and the vast majority of the studies only reported short-term outcomes (≤3 months). More recently, Tew et al. conducted a systematic review of controlled trials (both randomized and nonrandomized) of the efficacy of height-adjustable workstations only on occupational sitting time (72). All studies included a control condition with no environmental change and all studies showed significant reductions in occupational sitting relative to control. However, it should be noted that the authors rated all of the studies of low methodological quality with high risk for selection bias (i.e., due to nonrandomized designs). Given the dependency among workers within worksites, it has not been feasible to adequately test the efficacy of activity permissive workstations when the unit of observation is the individual. Recently, two important cluster-randomized trials have addressed this limitation by selecting worksites as the unit of randomization (20, 31). Both studies delivered programs that targeted individual, social, environmental, and policy factors, alongside the installation of sit-stand workstations, to reduce sedentary time. Danquah et al., in a 3-month intervention among 317 Danish public and private health workers across 19 worksites observed 48 min/8-hr workday reductions relative to a usual practice control (20). Healy et al., in a 12-month intervention of 231 Australian public health workers across 14 worksites observed 45 min/8-hr workday reductions relative to a usual practice control (31). These most recent studies have addressed many of the critical issues identified by a recent Cochrane Review on the efficacy of activity-permissive workstations (69) and have provided promising evidence that workplace interventions incorporating sit-stand workstations along with complementary multi-level strategies can produce sizeable reductions in sedentary time. These changes, when viewed alongside risk estimates from epidemiological studies, are likely to lead to improvements in health outcomes. However, important limitations still exist related to the long-term efficacy of this approach at sustaining behavior change, the translation of this approach in diverse types of worksite, and the cost-effectiveness of this approach relative to other health promotion activities.
Modifying environments remains an important strategy for reducing sedentary behavior in work, home, and school environments. These structural changes are likely necessary for sustained behavior change to occur, as without these changes it is difficult for individuals to reduce sedentary behavior substantially while still carrying out the desired activities within that context (e.g., maintaining productivity at work, leisure pursuits or household tasks at home, desk-based work at school). But they might not be sufficient.
New Behavioral Determinants: Targeting motivational processes
Although environmental changes to the workplace may elicit sustainable changes in behavior, they are also context dependent and unlikely to translate to other important behavioral domains. Furthermore, environmental changes alone do not address the basic motivational processes that that are needed to modify behavior. New approaches are needed that address sedentary time from an individual (motivational) level. Below we identify two main gaps that should be addressed in efforts to induce sustainable, individual-level changes in sedentary time.
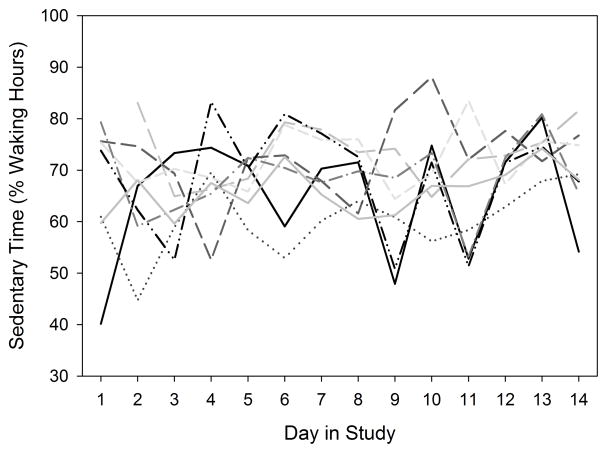
First, the temporal dimension of sedentary behavior, or the manner in which these behaviors vary within and between days, has largely been overlooked in prior work. At a descriptive level, it is clear that sedentary behavior varies as a function of the social calendar. College students engage in more sedentary behaviors from Tuesday through Friday than from Saturday through Monday (18). A similar pattern emerged with the Raine study cohort of young adults in Australia who had a lower ratio of sedentary behavior to light physical activity on Fridays and Saturdays (54). This cohort also revealed an interesting within-day temporal pattern such that sedentary behavior was most likely before 7am or after 8pm. At the other end of the lifespan, older adults exhibit a more equivocal pattern. They report being more sedentary mid-week than on weekends but this pattern did not replicate with objective measures (48). Variance decompositions consistently indicate that roughly half of the variance in daily sedentary time is attributable to between-person sources and the remaining variance can be attributed to within-person sources. Figure 2 shows that the strength of intentions to limit sedentary time varies from day to day as well. These daily fluctuations in the strength of both intentions and plans to limit sedentary time are negatively associated with daily fluctuations in sedentary behavior (18, 48). These associations indicate a substantive nature to the within-person variation and call for more attention to explain and control that variation. Such variation may also require more frequent within-person sampling or increase total sample size requirement in future studies. Thus, consideration of the temporal context of behavior can both increase predictive power and facilitate targeting of interventions to high-risk days or times. For the most part, contemporary behavioral theories do not account for time-varying motivational processes. The major exceptions in the health domain are recent proposals to extend behavioral theories using feedback principles from engineering; these dynamic approaches have recently been applied with sedentary behavior (2, 70).
Figure 2.
Illustration of day-to-day fluctuation in sedentary time in 8 individuals
The second major barrier to progress in understanding and modifying sedentary behavior is the emphasis on a limited range of motivational processes. Health behavior theories typically assume that people make rational choices about their behavior based on the beliefs about their capabilities, the difficulty of the behavior, and the value of outcomes associated with the behavior. Core explanatory constructs in these theories include intentions, efficacy beliefs, and behavioral feedback. These constructs are all reflective in nature; that is, they are effortful and relatively slow processes because they require rule-based cognitive processing or elaboration of the expected utility of behavioral options (14, 36). The capacity for reflective processing to self-regulate is widely thought to be finite so people often struggle to sustain this kind of effortful self-regulation for extended periods of time (35).
In contrast, there are parallel motivational processes which are described as automatic or impulsive because they are effortless and relatively fast in comparison to reflective processes. These automatic processes are based on associations that are learned (i.e., conditioned) over time between a behavior and experienced outcomes. These processes are often initiated automatically when people encounter cues that they have learned to associate with behavioral scripts, that is, when people have habits. Consider this oversimplified example: when a person with a strong habit for watching television enters their home, the mere sight of the remote control may increase the odds of turning on the television without any effortful processing on her or his part. Masking the cue – in this case, hiding the remote control – may be sufficient to eliminate the behavioral advantage of strong habits for sedentary behavior.
Dual-process models of motivation and behavior are based on the idea that reflective and automatic processes operate in parallel. All else being equal, automatic processes will govern a substantial share of human behavior but habits (and other automatic processes) can be overridden with effortful reflective processes (78). Automatic processes are an emerging priority for health behavior researchers (49, 68). Daily sedentary behavior has been associated with both reflective and automatic processes at both extremes of the adult lifespan (18, 48). Regardless of age, people with stronger habits for sitting spend more time engaged in sedentary behavior but daily fluctuations in both intentions and planning to limit sedentary behavior can interrupt those habits and reduce sedentary behavior.
Based on these findings, an opportunity has arisen to push beyond the status quo and enrich theories as they relate to sedentary behavior with both a temporal dimension and attention to automatic motivational processes. The most generative theories will account for where people engage in sedentary behavior as well as when and why they engage in that behavior. Detailed recalls that reveal the context of previous day activity and sedentary time (i.e., time use data, previous day recalls) may be particularly valuable in developing such theories (12, 50). Elaborating on these additional features of sedentary behavior will open new intervention possibilities.
Emerging intervention approaches to target sedentary behavior
Several intervention approaches that reinforce “natural” breaks in sedentary time have been tested (e.g., printing to a printer on a different floor) and shown to induce modest changes in sitting time. (61) An exciting recent development in sedentary behavior intervention design has been the just-in-time approach, which capitalizes on the temporal features of sedentary behavior. Just-in-time interventions are triggered when sedentary behavior exceeds a pre-determined threshold (e.g., 90 minutes without standing for at least one minute). In one of the earliest examples with sedentary behavior, feedback from the computer keyboard and mouse were used to identify extended periods of sedentary behavior and trigger intervention prompts (75). This approach may be effective for desk workers while they are at their desks but it is context-limited. Others have tried to loosen this spatial leash by using smartphones to trigger notifications when extended periods of inactivity have been detected (8, 59). Although it is difficult to detect sedentary behavior “in the wild” with smartphones alone, prompts triggered by extended periods of inactivity have proven to be effective at reducing sedentary time. For example, Bond and colleagues recently reported that prompts for 3-minute breaks after 30 minutes of inactivity or 6-minute breaks after 60 minutes of inactivity reduced daily sedentary behavior by 47.2 or 44.5 minutes, respectively (whereas prompts for 12-minute breaks after 120 minutes of inactivity only reduced daily sedentary behavior by 26.2 minutes) (8). This example highlights how physiologic findings on the benefits of breaking-up sitting can be directly translated into new intervention goals (22, 25). This trial also provides evidence to inform the temporal thresholds that will trigger interventions. Another approach for determining the optimal temporal threshold is the microrandomized trial (41). These trials randomly vary (within participants) the duration of sedentary time needed to trigger an intervention. Results lead to the specific decision rules for triggering just-in-time interventions. These decision rules can even be optimized to target different contexts or populations (e.g., a 30 min threshold may optimize behavior change at home whereas a 120 min threshold may optimize behavior change at worksites)
Another persistent challenge with just-in-time interventions is our limited understanding of the proximal antecedents of sedentary behavior (i.e., behaviors/actions occurring immediately prior to sedentary behavior). The cues that trigger habitual behaviors are likely to vary from one person to the next based on their individual learning histories. People may not even be aware of the cues that trigger their habits! Absent advance information about cues, temporal thresholds have been used as intervention triggers but those may not be optimal either. In practice, it can be difficult – or simply too disruptive – to interrupt ongoing sedentary behavior when competing motivational incentives are often present to facilitate sedentary behavior (e.g., rewards from eating, entertainment, or social activity). In this case, it may be wise to shift our focus away from using risk-based vulnerabilities (e.g., extended sedentary behavior) to trigger intervention and toward reward-based opportunities to initiate competing behaviors that require a transition to an upright and more physically active state. This shift in emphasis may require deeper consideration of the contextual cues that can initiate standing and walking but may be overlooked. We anticipate that interventions for reducing sedentary time will be most effective if they are timed to interrupt habitual sedentary behavior before it starts. Thus, interventions need to (a) improve effortful down-regulation of sedentary behavior via reflective motivational processes (e.g., form plans for when, where, and how to reduce sedentary behavior), (b) reduce the reward value of sedentary activities that reinforce habit strength (e.g., watch entertaining shows standing up and sit for commercials), and (c) capitalize on available cues for alternative, rewarding activities that involve standing and walking (i.e., leverage other habits that would predispose a person to standing or walking to displace sitting time). Advances in wearable technology and data science are opening new possibilities for capturing behavior in different contexts. These tools may uncover the cues that are essential for understanding and modifying this high-volume habitual behavior.
Summary and Future Research Questions
This review provided a state of the knowledge update on the robust body of evidence that has emerged, primarily within the past five years, related to sedentary behavior and health impacts among adults. A notable feature of this body of evidence is the synergistic, solutions-oriented research across the behavioral research framework that has led to specific, actionable studies that ultimately may inform future public health recommendations (Figure 1). Building on some of the landmark studies on lifestyle physical activity, much progress has been made in recent years in understanding the etiology and behavioral aspect of sitting. This work has raised a host of new research questions and some of the most pressing questions are summarized in Table 1.
Table 1.
Major questions and future directions in sedentary behavior research domains
| Observational | Behavioral determinants and theories |
|---|---|
|
|
| Experimental | Behavioral Change Interventions |
|
|
Both observational and experimental evidence indicates benefits for replacing sedentary behavior with a range of physical activities, including light-intensity activities of everyday living that were not previously recommended as “health-enhancing” behaviors (60). Prospective reductions in sedentary time are associated with lower mortality and disease risk, highlighting the need for effective interventions. Experimental studies have provided evidence regarding the physiologic and cardiometabolic benefits of breaking up and reducing sitting time, and these studies provide biological support for the epidemiologic studies and have informed workplace interventions designed to increase the number of daily breaks from prolonged sitting. More research is needed to reveal the timing and patterning of different postures/behaviors/intensities that are linked with health. Prospective observational evidence is needed to understand the optimal balance between different activity intensities and how patterns of behaviors affects hard-disease end-points. Experimental studies that manipulate sedentary behavior and the frequency and duration of breaks for longer-periods of time will directly inform intervention targets (Table 1).
The critical next step for the field is to translate the observational and experimental findings into feasible and effective interventions that complement and extend our efforts to promote moderate-vigorous aerobic physical activity. Application of existing behavioral theories and intervention methods that have been found to be effective for facilitating the adoption and maintenance of exercise have been less successful when targeting sedentary behavior as a means to increase daily activity. Recent behavioral research has led to new thinking about the differences and similarities in the determinants of these two distinct behaviors (sedentary and exercise) and has led to interventions targeting the microenvironment as well as a search for specific determinants of sedentary behaviors. New evidence about the within- and between-day variations in sedentary behavior is infusing a sensitivity to time-varying motivational processes into health behavior theory. Future research in the behavioral domain should focus on answering questions regarding identifying where and why people are sedentary to identify cues that may be modifiable (Table 1).
In closing, we shaped this review to stimulate new research, improve interventions and increase the efficacy of intervention efforts that seek to reduce sedentary time. It is worth noting that the benefits of reducing or replacing sedentary time with light intensity activity appear stronger for those who are less active (6, 51, 52). Future research should examine the health-impact of longer-term sedentary time reduction in less active populations, including those with chronic conditions and older adults. Ultimately, if such interventions are efficacious for improving health, it will be important to evaluate whether increases in activities of daily living can “pave the way” for promoting enhanced participation in moderate-intensity exercise. If not, sequential or parallel interventions will be necessary to explicitly target increases in moderate-vigorous intensity exercise, which remains the most robust and evidence-based target for activity interventions to improve health. Given the inverse relationship between sedentary behavior and physical activity, new intervention approaches that seek to reduce sitting and harness the powerful health benefits of physical activity are likely to improve human health.
Acknowledgments
The authors would like to thank Henley Kim, MFA for her contribution in designing Figure 1.
The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of the present study do not constitute endorsement by ACSM.
Dunstan was supported by an NHMRC Senior Research Fellowship (NHMRC #1078360) and the Victorian Government’s Operational Infrastructure Support Program. Buman was supported by the National Institutes of Health (R01CA198971, R18DK109516, R21NR016046). Matthews was supported by the Intramural Research Program at the National Institutes of Health.
References
- 1.Arem H, Moore SC, Patel A, et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015;175(6):959–67. doi: 10.1001/jamainternmed.2015.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashour M, Bekiroglu K, Yang CH, et al. On the mathematical modeling of the effect of treatment on human physical activity. Proceedings of the 2016 IEEE Conference on Control Applications (CCA) 2016:1084–91. [Google Scholar]
- 3.Benatti FB, Ried-Larsen M. The effects of breaking up prolonged sitting time: a review of experimental studies. Med Sci Sports Exerc. 2015;47(10):2053–61. doi: 10.1249/MSS.0000000000000654. [DOI] [PubMed] [Google Scholar]
- 4.Bergouignan A, Rudwill F, Simon C, Blanc S. Physical inactivity as the culprit of metabolic inflexibility: Evidences from bed-rest studies. J Appl Physiol. 2011;111(4):1201–10. doi: 10.1152/japplphysiol.00698.2011. [DOI] [PubMed] [Google Scholar]
- 5.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical activity: A molecular reason to maintain daily low-intensity activity. J Physiol. 2003;551(2):673–82. doi: 10.1113/jphysiol.2003.045591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32. doi: 10.7326/M14-1651. [DOI] [PubMed] [Google Scholar]
- 7.Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17):2395–401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- 8.Bond DS, Thomas JG, Raynor HA, et al. B-MOBILE - A Smartphone-Based Intervention to Reduce Sedentary Time in Overweight/Obese Individuals: A Within-Subjects Experimental Trial. Plos One. 2014;9(6) doi: 10.1371/journal.pone.0100821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brodersen NH, Steptoe A, Williamson S, Wardle J. Sociodemographic, developmental, environmental, and psychological correlates of physical activity and sedentary behavior at age 11 to 12. Ann Beh Med. 2005;29(1):2–11. doi: 10.1207/s15324796abm2901_2. [DOI] [PubMed] [Google Scholar]
- 10.Brown WJ, Bauman AE, Bull FC, Burton NW. Development of evidence-based physical activity recommendations for adults (18–64 years) Report Prepared for the Ausatralian Government Department of Health. 2012:161. [Google Scholar]
- 11.Buman MP, Winkler EA, Kurka JM, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–2006. Am J Epidemiol. 2014;179(3):323–34. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- 12.Bureau of Labor and Statistics. [Accessed Nov 2016];American Time Use Survey. 2016 Available from: http://www.bls.gov/tus/tables.htm.
- 13.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–31. [PMC free article] [PubMed] [Google Scholar]
- 14.Chaiken S, Trope Y. Dual-process theories in social psychology. New York, NY: Guilford Press; 1999. p. 657. [Google Scholar]
- 15.Chastin SF, Egerton T, Leask C, Stamatakis E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity (Silver Spring) 2015;23(9):1800–10. doi: 10.1002/oby.21180. [DOI] [PubMed] [Google Scholar]
- 16.Chastin SF, Palarea-Albaladejo J, Dontje ML, Skelton DA. Combined Effects of Time Spent in Physical Activity, Sedentary Behaviors and Sleep on Obesity and Cardio-Metabolic Health Markers: A Novel Compositional Data Analysis Approach. PLoS One. 2015;10(10):e0139984. doi: 10.1371/journal.pone.0139984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 Decades in US Occupation-Related Physical Activity and Their Associations with Obesity. Plos One. 2011;6(5) doi: 10.1371/journal.pone.0019657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Conroy DE, Maher JP, Elavsky S, Hyde AL, Doerksen SE. Sedentary Behavior as a Daily Process Regulated by Habits and Intentions. Health Psychology. 2013;32(11):1149–57. doi: 10.1037/a0031629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crespo NC, Mullane SL, Zeigler ZS, Buman MP, Gaesser GA. Effects of Standing and Light-Intensity Walking and Cycling on 24-h Glucose. Med Sci Sports Exerc. 2016;48(12):2503–11. doi: 10.1249/MSS.0000000000001062. [DOI] [PubMed] [Google Scholar]
- 20.Danquah IH, Kloster S, Holtermann A, et al. Take a Stand!-a multi-component intervention aimed at reducing sitting time among office workers-a cluster randomized trial. Int J Epidemiol. 2016 doi: 10.1093/ije/dyw009. E pub April 19. [DOI] [PubMed] [Google Scholar]
- 21.De Cocker K, Duncan MJ, Short C, van Uffelen JG, Vandelanotte C. Understanding occupational sitting: prevalence, correlates and moderating effects in Australian employees. Prev Med. 2014;67:288–94. doi: 10.1016/j.ypmed.2014.07.031. [DOI] [PubMed] [Google Scholar]
- 22.Dempsey PC, Larsen RN, Sethi P, et al. Benefits for type 2 diabetes of interrupting prolonged sitting with brief bouts of light walking or simple resistance activities. Diabetes Care. 2016;39(6):964–72. doi: 10.2337/dc15-2336. [DOI] [PubMed] [Google Scholar]
- 23.Dempsey PC, Sacre JW, Larsen RN, et al. Interrupting prolonged sitting with brief bouts of light walking or simple resistance activities reduces resting blood pressure and plasma noradrenaline in type 2 diabetes. J Hypertens. 2016 doi: 10.1097/hjh.0000000000001101. [DOI] [PubMed] [Google Scholar]
- 24.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, 3rd, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281(4):327–34. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 25.Dunstan DW, Kingwell BA, Larsen R, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35(5):976–83. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duvivier BM, Schaper NC, Bremers MA, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS One. 2013;8(2):e55542. doi: 10.1371/journal.pone.0055542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–10. doi: 10.1016/S0140-6736(16)30370-1. [DOI] [PubMed] [Google Scholar]
- 28.Fishman EI, Steeves JA, Zipunnikov V, et al. Association between Objectively Measured Physical Activity and Mortality in NHANES. Med Sci Sports Exerc. 2016;48(7):1303–11. doi: 10.1249/MSS.0000000000000885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: A meta-analysis. JAMA. 2011;305(23):2448–55. doi: 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haskell W. Dose-Response Issues From a Biological Perspective. In: Bouchard C, Shepard R, Stephens T, editors. Physical Activity, Fitness, and Health. Champaign, IL: Human Kinetics; 1994. pp. 1030–9. [Google Scholar]
- 31.Healy GN, Eakin EG, Owen N, et al. A Cluster RCT to Reduce Office Workers’ Sitting Time: Impact on Activity Outcomes. Med Sci Sports Exerc. 2016 doi: 10.1249/MSS.0000000000000972. E pub May 17. [DOI] [PubMed] [Google Scholar]
- 32.Healy GN, Winkler EA, Owen N, Anuradha S, Dunstan DW. Replacing sitting time with standing or stepping: associations with cardio-metabolic risk biomarkers. Eur Heart J. 2015;36(39):2643–9. doi: 10.1093/eurheartj/ehv308. [DOI] [PubMed] [Google Scholar]
- 33.Henson J, Davies MJ, Bodicoat DH, et al. Breaking up prolonged sitting with standing or walking attenuates the postprandial metabolic response in postmenopausal women: a randomized acute study. Diabetes Care. 2016;39(1):130–8. doi: 10.2337/dc15-1240. [DOI] [PubMed] [Google Scholar]
- 34.Howard BJ, Fraser SF, Sethi P, et al. Impact on hemostatic parameters of interrupting sitting with intermittent activity. Med Sci Sports Exerc. 2013;45(7):1285–91. doi: 10.1249/MSS.0b013e318285f57e. [DOI] [PubMed] [Google Scholar]
- 35.Inzlicht M, Schmeichel BJ. What Is Ego Depletion? Toward a Mechanistic Revision of the Resource Model of Self-Control. Perspectives on Psychological Science. 2012;7(5):450–63. doi: 10.1177/1745691612454134. [DOI] [PubMed] [Google Scholar]
- 36.Kahneman D. Thinking fast and slow. New York, New York: 2011. p. 499. [Google Scholar]
- 37.Katzmarzyk PT. Standing and mortality in a prospective cohort of Canadian adults. Med Sci Sports Exerc. 2014;46(5):940–6. doi: 10.1249/MSS.0000000000000198. [DOI] [PubMed] [Google Scholar]
- 38.Keadle SK, Arem H, Moore SC, Sampson JN, Matthews CE. Impact of changes in television viewing time and physical activity on longevity: a prospective cohort study. Int J Behav Nutr Phys Act. 2015;12:156. doi: 10.1186/s12966-015-0315-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Keadle SK, Moore SC, Sampson JN, Xiao Q, Albanes D, Matthews CE. Causes of Death Associated With Prolonged TV Viewing: NIH-AARP Diet and Health Study. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.King A, Buman M, Hekler E. Physical activity strategies in populations. In: Kahan S, Gielen A, Fagan P, editors. Health behavior change in populations: The state of the evidence and roles for key stakeholders. Baltimore, MD: Johns Hopkins University Press; 2014. p. 1023. [Google Scholar]
- 41.Klasnja P, Hekler EB, Shiffman S, et al. Microrandomized Trials: An Experimental Design for Developing Just-in-Time Adaptive Interventions. Health Psychology. 2015;34:1220–8. doi: 10.1037/hea0000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kohl HW, 3rd, Dunn AL, Marcus BH, Blair SN. A randomized trial of physical activity interventions: design and baseline data from project active. Med Sci Sports Exerc. 1998;30(2):275–83. doi: 10.1097/00005768-199802000-00016. [DOI] [PubMed] [Google Scholar]
- 43.Koohsari MJ, Sugiyama T, Sahlqvist S, Mavoa S, Hadgraft N, Owen N. Neighborhood environmental attributes and adults’ sedentary behaviors: Review and research agenda. Prev Med. 2015;77:141–9. doi: 10.1016/j.ypmed.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 44.Larsen RN, Kingwell BA, Sethi P, Cerin E, Owen N, Dunstan DW. Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutr Metab Cardiovasc Dis. 2014;24(9):976–82. doi: 10.1016/j.numecd.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 45.Lee J, Kuk JL, Ardern CI. The relationship between changes in sitting time and mortality in post-menopausal US women. J Public Health. 2016;38(2):270–8. doi: 10.1093/pubmed/fdv055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leon-Munoz LM, Martinez-Gomez D, Balboa-Castillo T, Lopez-Garcia E, Guallar-Castillon P, Rodriguez-Artalejo F. Continued sedentariness, change in sitting time, and mortality in older adults. Med Sci Sports Exerc. 2013;45(8):1501–7. doi: 10.1249/MSS.0b013e3182897e87. [DOI] [PubMed] [Google Scholar]
- 47.Maher JP, Conroy DE. Habit strength moderates the effects of daily action planning prompts on physical activity but not sedentary behavior. J Sport Exerc Psychol. 2015;37(1):97–107. doi: 10.1123/jsep.2014-0258. [DOI] [PubMed] [Google Scholar]
- 48.Maher JP, Conroy DE. A Dual-Process Model of Older Adults’ Sedentary Behavior. Health Psych. 2016;35(3):262–72. doi: 10.1037/hea0000300. [DOI] [PubMed] [Google Scholar]
- 49.Marteau TM, Hollands GJ, Fletcher PC. Changing Human Behavior to Prevent Disease: The Importance of Targeting Automatic Processes. Science. 2012;337(6101):1492–5. doi: 10.1126/science.1226918. [DOI] [PubMed] [Google Scholar]
- 50.Matthews CE, Keadle SK, Sampson J, et al. Validation of a previous-day recall measure of active and sedentary behaviors. Med Sci Sports Exerc. 2013;45(8):1629–38. doi: 10.1249/MSS.0b013e3182897690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Matthews CE, Keadle SK, Troiano RP, et al. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in US adults. Am J Clin Nutr. 2016 Nov;104(5):1424–1432. doi: 10.3945/ajcn.116.135129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matthews CE, Moore SC, Sampson J, et al. Mortality Benefits for Replacing Sitting Time with Different Physical Activities. Med Sci Sports Exerc. 2015;47(9):1833–40. doi: 10.1249/MSS.0000000000000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mcleroy KR, Bibeau D, Steckler A, Glanz K. An Ecological Perspective on Health Promotion Programs. Health Educ Qu. 1988;15(4):351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 54.McVeigh JA, Winkler EAH, Howie EK, et al. Objectively measured patterns of sedentary time and physical activity in young adults of the Raine study cohort. Int J Behav Nutr Phys Act. 2016;13:41. doi: 10.1186/s12966-016-0363-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mekary RA, Lucas M, Pan A, et al. Isotemporal substitution analysis for physical activity, television watching, and risk of depression. Am J Epidemiol. 2013;178(3):474–83. doi: 10.1093/aje/kws590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Neuhaus M, Eakin EG, Straker L, et al. Reducing occupational sedentary time: a systematic review and meta-analysis of evidence on activity-permissive workstations. Obesity Reviews. 2014;15(10):822–38. doi: 10.1111/obr.12201. [DOI] [PubMed] [Google Scholar]
- 57.Otten JJ, Jones KE, Littenberg B, Harvey-Berino J. Effects of Television Viewing Reduction on Energy Intake and Expenditure in Overweight and Obese Adults A Randomized Controlled Trial. Arch Int Med. 2009;169(22):2109–15. doi: 10.1001/archinternmed.2009.430. [DOI] [PubMed] [Google Scholar]
- 58.Owen N, Healy GN, Matthews CE, Dunstan DW. Too Much Sitting: The Population Health Science of Sedentary Behavior. Exer Sport Sci Rev. 2010;38(3):105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pellegrini CA, Hoffman SA, Daly ER, Murillo M, Iakovlev G, Spring B. Acceptability of smartphone technology to interrupt sedentary time in adults with diabetes. Trans Behav Med. 2015;5(3):307–14. doi: 10.1007/s13142-015-0314-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Physical Activity Guidelines Committee. Physical Activity Guidelines Committee Report. U.S. Dpeartment of Health and Human Services; Washington, DC: 2008. [Accessed November 2016]. Available from: www.health.gov/paguidelines/report. [Google Scholar]
- 61.Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obesity Reviews. 2014;15(11):905–19. doi: 10.1111/obr.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Quartiroli A, Maeda H. Self-determined Engagement in Physical Activity and Sedentary Behaviors of US College Students. Int J Exer Sci. 2014;7(1):10. doi: 10.70252/SVGJ1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Restaino RM, Walsh LK, Morishima T, et al. Endothelial dysfunction following prolonged sitting is mediated by a reduction in shear stress. Am J Phys. 2016;310(5):H648–53. doi: 10.1152/ajpheart.00943.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Saelens BE, Handy SL. Built environment correlates of walking: a review. Med Sci Sports Exerc. 2008;40(7 Suppl):S550–66. doi: 10.1249/MSS.0b013e31817c67a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q. 2009;87(1):123–54. doi: 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Salmon J, Ball K, Hume C, Booth M, Crawford D. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: Switch-Play. Intl J Obes. 2008;32(4):601–12. doi: 10.1038/sj.ijo.0803805. [DOI] [PubMed] [Google Scholar]
- 67.Schmid D, Leitzmann M. Television Viewing and Time Spent Sedentary in Relation to Cancer Risk: A Meta-Analysis. Asia-Pac J Clin Onco. 2014;10:244–5. doi: 10.1093/jnci/dju098. [DOI] [PubMed] [Google Scholar]
- 68.Sheeran P, Gollwitzer PM, Bargh JA. Nonconscious Processes and Health. Health Psychology. 2013;32(5):460–73. doi: 10.1037/a0029203. [DOI] [PubMed] [Google Scholar]
- 69.Shrestha N, Kukkonen-Harjula KT, Verbeek JH, Ijaz S, Hermans V, Bhaumik S. Workplace interventions for reducing sitting at work. Cochrane Database Syst Rev. 2016;(3) doi: 10.1002/14651858.CD010912.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Spruijt-Metz D, Hekler E, Saranummi N, et al. Building new computational models to support health behavior change and maintenance: new opportunities in behavioral research. Trans Behav Med. 2015;5(3):335–46. doi: 10.1007/s13142-015-0324-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stamatakis E, Rogers K, Ding D, et al. All-cause mortality effects of replacing sedentary time with physical activity and sleeping using an isotemporal substitution model: a prospective study of 201,129 mid-aged and older adults. Int J Behav Nutr Phys Act. 2015;12:121. doi: 10.1186/s12966-015-0280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tew GA, Posso MC, Arundel CE, McDaid CM. Systematic review: height-adjustable workstations to reduce sedentary behaviour in office-based workers. Occupational Medicine-Oxford. 2015;65(5):357–66. doi: 10.1093/occmed/kqv044. [DOI] [PubMed] [Google Scholar]
- 73.Thosar SS, Bielko SL, Mather KJ, Johnston JD, Wallace JP. Effect of prolonged sitting and breaks in sitting time on endothelial function. Med Sci Sports Exerc. 2015;47(4):843–9. doi: 10.1249/MSS.0000000000000479. [DOI] [PubMed] [Google Scholar]
- 74.Thyfault JP, Krogh-Madsen R. Metabolic disruptions induced by reduced ambulatory activity in free-living humans. J Appl Physiol. 2011;111(4):1218–24. doi: 10.1152/japplphysiol.00478.2011. [DOI] [PubMed] [Google Scholar]
- 75.van Dantzig S, Geleijnse G, van Halteren AT. Toward a persuasive mobile application to reduce sedentary behavior. Pers Ubiq Comput. 2013;17(6):1237–46. [Google Scholar]
- 76.Wijndaele K, Orrow G, Ekelund U, et al. Increasing objectively measured sedentary time increases clustered cardiometabolic risk: a 6 year analysis of the ProActive study. Diabetologia. 2014;57(2):305–12. doi: 10.1007/s00125-013-3102-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wiseman AJ, Lynch BM, Cameron AJ, Dunstan DW. Associations of change in television viewing time with biomarkers of postmenopausal breast cancer risk: the Australian Diabetes, Obesity and Lifestyle Study. Cancer Causes Control. 2014;25(10):1309–19. doi: 10.1007/s10552-014-0433-z. [DOI] [PubMed] [Google Scholar]
- 78.Wood W, Runger D. Psychology of Habit. Ann Rev Psych. 2016;67:289–314. doi: 10.1146/annurev-psych-122414-033417. [DOI] [PubMed] [Google Scholar]
- 79.Zeigler ZS, Mullane SL, Crespo NC, Buman MP, Gaesser GA. Effects of Standing and Light-Intensity Activity on Ambulatory Blood Pressure. Med Sci Sports Exerc. 2016;48(2):175–81. doi: 10.1249/MSS.0000000000000754. [DOI] [PubMed] [Google Scholar]
- 80.Zeigler ZS, Swan PD, Bhammar DM, Gaesser GA. Walking Workstation Use Reduces Ambulatory Blood Pressure in Adults With Prehypertension. J Phys Act Health. 2015;12(Suppl 1):S119–27. doi: 10.1123/jpah.2013-0487. [DOI] [PubMed] [Google Scholar]