Abstract
Introduction:
Humeral shaft fractures are quite common in orthopedics and represent 1-3% of adult fractures. The surgical treatment is the a better choice in order to obtain a reduction and stable alignment and to prevent the complications. The goal of this study was to compare the three techniques (IMN, LCP and EF) in the treatment of diaphyseal fractures of the humerus in the adult patient.
Materials and Methods:
We examined 79 patients with diaphyseal fractures of the humerus. 32 were treated with plaque (LCP), 26 with intramedullary nail (IMN) and 21 with eternal fixer (FE) The clinical and radiographic follow-up was done at 1.3, 6 and 12 months. As rating scales we used the ASES and SF-36. We recorded all the complications.
Results:
The median follow-up was 11.5 months (9-16). The operative time was significantly smaller in the case of FE (47 ‘) with a statistically significant difference compared with other techniques. Even the blood loss was lower in the case of FE (60ml), compared to nails (160ml) and LCP (330ml) p <0.05. We had no differences in the duration of hospitalization and the ASES SF-36 score. We had 2 cases of non-union in the LCP group, 1 case in the IMN group and no cases in the FE group. In IMN group we had one case of radial transient paralysis. We did not have any deep infection, in the FE group 8 patients we had superficial secretions from pins.
Conclusion:
From the results of our study, it is clear that the treatment of humeral shaft fractures guarantee overlapping results with the use of plates, of intramedullary nails, or with the external fixator. Consequently, the choice of which technique to use should be determined based on the experience of the operator and patient compliance.
Keywords: Humeral Shaft fractures, Plate, External Fixation, Intramedullary nailing, Outcomes, bleeding, complications
1. INTRODUCTION
Humeral shaft fractures are quite common in orthopedics and represent 1-3% of adult fractures [13]. Although the conservative treatment in some cases may be the most suitable choice with good outcome, the surgical treatment, in most cases, is the a better choice in order to obtain a reduction and stable alignment, especially in the case of comminuted fractures, floating shoulder, multiple trauma, neurovascular compromise, nonunion, open fractures, pathological fractures, and the failure of conservative treatment [4].
Developments in the ORIF technique have increased and improved the results of surgical treatment. The most commonly used techniques are: osteosynthesis with plate and screws (LCP, locking compression plate) [5], the splint with intramedullary nail (IMN), and the external fixation (EF) [6]. These techniques have different biomechanical and physiological aspects, each with their advantages and disadvantages [7-12]. Although there are numerous randomized clinical trials and meta-analysis that have attempted to guide the surgeon in choosing the most appropriate treatment, there is little evidence and no consensus as to what is the most suitable treatment. There is no specific algorithm for deciding since it is necessary to take into account many factors before reaching a final decision as to which treatment to implement.
The goal of this study was to compare the three techniques (IMN, LCP and EF) in the treatment of diaphyseal fractures of the humerus in the adult patient. In order to properly assess the techniques, we looked at clinical outcomes (assessed by ASES score), the SF-36, the psychological status by The Short Form Health Survey, the length of stay, complication rate and the incidence of nonunion.
2. MATERIALS AND METHODS
We looked at all of the diaphyseal humeral fractures treated between 2013 and 2015, totaling 79 patients. Of these, 42 were women and 37 men. The left upper limb was involved in 45 cases and the right in 34. We excluded from the study: exposed fractures, fractures with paralysis of the radial nerve, patients under 18 years of age and over 85 years, patients with pre-existing limb fractures, pathologic fractures, and patients treated after 48h post-injury. The inclusion criteria were humeral shaft fractures without articular involvement treated within 48h post-injury. Out of 79 patients, 32 were treated with open synthesis and plate (LCP), 26 with locked intramedullary nail (IMN), and the remaining 21 with EF.
The patients’ ages ranged from 18 to 85 years old (mean 56.3), the right side was affected in 34 cases and the left in 45 cases. All fractures were classified according to the AO classification and were: 49 type A, 18 type B and 12 type C. The summary of the characteristics of the three groups are listed in Table 1.
Table 1.
Patient characteristics
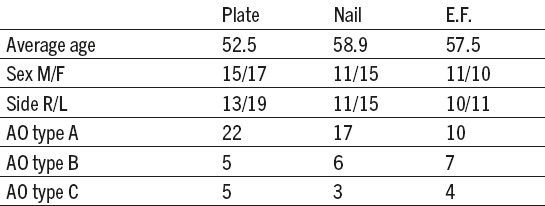
Table 2.
ASES Score. (4=normal; 3=mild compromise; 2=difficulty; 1=with aid; 0=unable)
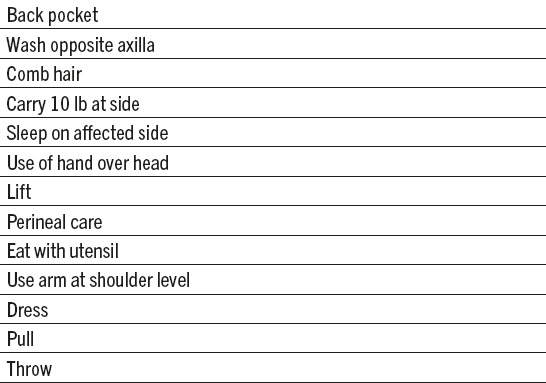
Table 4.
Superficial infections were resolved with oral antibiotics
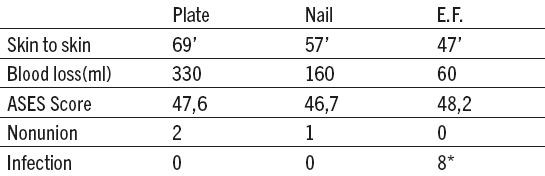
Figure 1.

(A) X-ray after the surgical management with plate and screws in 12-B1 according AO/OTA’s Classification.. (B)The bone healing after four months from surgery.
Figure 2.

(A) X-ray shows the humeral shaft fracture, 12-A3 according AO/OTA’s Classification. (B) The X-rays shows the bone healing after 4 month from the surgical management with locked intramedullary nail.
Figure 3.
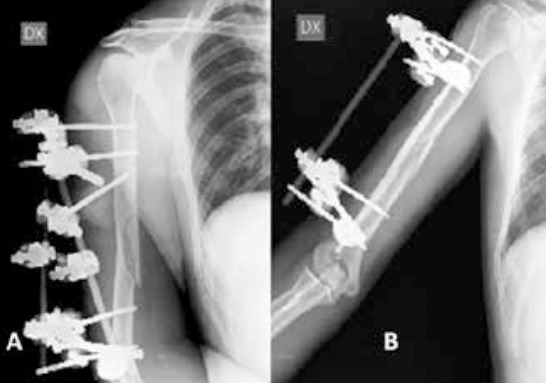
(A) X-ray after the surgical management with modular external fixation in 12-B1 according AO/OTA’s Classification. (B)The bone healing after four months before the hardware remotion.
Prior to surgery all patients were evaluated with at least two x-rays and normal pre-operative procedures. In 56 patients, anesthesia with plexus block at the level of the brachial plexus was administered, and in 23 patients general anesthetic was administered. All patients were administered a single dose of cefazolin 2g IV pre-operative antibiotic prophylaxis. Patients allergic to beta-lactam were administered clindamycin 600 mg IV. Surgery was performed on a glossy radio operating table, in the beach chair position.
Post-operative X-rays were performed in all cases, in order to determine whether the reduction of the fracture was optimal, the correct positioning of the synthetic means, and any kind of iatrogenic complications.
The clinical and radiographic follow-up was carried out with clinical controls at 15 days, 1 month, 3 months, 6 months, and 12 months post-surgery, and annually thereafter. Clinical evaluation criterion was when the patient was able to use the limb without pain. The functional recovery evaluation was performed using the ‘American Shoulder and Elbow Surgeons’ shoulder score (ASES) [13]. Additionally, we evaluated the psychological impact of the type of intervention and the quality of life before and after surgery using The Short Form Health Survey[14]. The Short Form Questionnaire (SF-36) was also used, which is a valid tool to evaluate the health of patients. It is commonly used in health economics as a variable in the quality-adjusted life year calculation to determine the cost-effectiveness of treatment. This tool consists of eight different scaled scores that grade each patient with points from 0-100. [15]
X-ray evaluations of all patients were performed with standard projections of the humerus shaft at 1 month, 3 months, 6 months, and 12 months. The radiographic consolidation of the fracture was used as the evaluation end point (defined as the moment when x-rays show bridging callus across the fracture site).
We also calculated blood loss, averaged with a variant of the Gross formula [16], that corresponds to the blood volume (body weight X 70 ml/kg) multiplied by the hematocrit pre-operative minus the hematocrit post-surgery. The result is compared to the average hematocrit.
Blood loss = Blood volume X (Initial Htc – Final Htc)/Average Htc
Finally, the complication rate of the three surgical procedures was assessed and compared based on laboratory data. Immediately post-operative and at subsequent check-ups, patients were monitored for signs of infection, persistence of pain, recovery of the ROM of the elbow and glenohumeral joint, neurovascular status and any other complications.
In all patients post-operatively, the arm was supported in a neck sling for 3-5 days, and the active and passive mobilization of the elbow and shoulder began 4 weeks after surgery
In the LCP group, the locking compression plate (LCP, Synthesis) was used. The anterolateral path, centered on the fracture, was used as a pathway to access the fracture and, when possible, lag screws and a neutralization plate were used. When the extension of the fracture was very distal, the radial nerve was isolated. Regarding the plate length, plates with 9 to 13 holes were used positioning at least three screws proximally and three distally to the fracture.
In the IMN group, antegrade intramedullary nailing was used (T2 humeral nail, Stryker®). The nail was secured with two proximal locking screws and a distal screw. The surgical incision was performed from the outer side of the acromion, along the lateral aspect of the arm, passing through the deltoid muscle and rotator cuff. In all cases, a pre-reaming of the endosteum was performed. Regarding the nail diameter, a 7mm nail was used in 9 patients and an 8mm nail was used in the remaining 17 patients.
In 21 patients from the EF group, after manual reduction guided by fluoroscope, first, the pins were distally positioned through a small incision at the level of the lateral humeral ridge, then the proximal pins were secured through mini-incisions of the skin and trans-deltoid. After closing the External Fixation System, a pin was placed with joint clamps and a connecting rod 2 cm proximally from the fracture. Finally, a cross bar was added to increase the rigidity of the system. The cross bar and the intermediate pin was removed about 30 days after surgery.
Descriptive statistics were used to summarize the characteristics of the study group and subgroups, including means and standard deviations of all continuous variables. The T-test was used to compare continuous outcomes. The Chi-square test or Fisher’s exact test (in subgroups smaller than 10 patients) were used to compare Categorical variables. The statistical significance was defined as p<0.05..
3. RESULTS
The average follow-up was 11.5 months (9-16). In all cases, stitches were removed after 2 weeks. The duration of surgery (skin to skin) was an average of 69 minutes for the LCP, 57 minutes for the IMN, and 47 minutes for the EF. The difference between the times appears statistically significant (p value <0.05), confirming that the external fixation is the most rapid technique compared to the intramedullary splint and to the synthesis with plate.
Blood loss, calculated using a variant of the Gross formula, was an average of 330ml in patients treated with osteosynthesis with LCP, 160ml in patients treated with intramedullary nailing, and 60ml in the external fixation group, demonstrating the presence of a statistically significant difference (p value <0.05) between the three techniques. The hospital stay did not show statistically significant differences among the three groups; In fact, all the patients were discharged between the 2nd and the 4th post-operative day (on average 2.9). The ASES Score points were 47.6 (40-52) for LCP, 46.7 for IMN (38-52) and 48.2 (41-52) for EF (p value> 0.05).
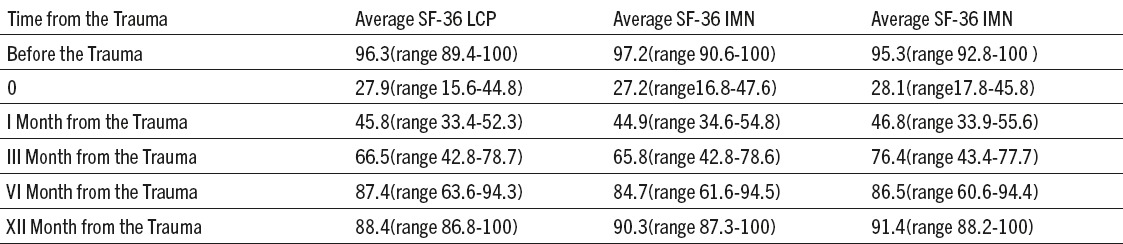
Regarding complications, for LCP there were two cases of nonunion that were treated by new synthesis with a plate, for IMN there was one case of nonunion that was treated by removing the nail and new synthesis with plate, and in the EF group there were no cases of nonunion (Tab 3). Regarding the SF-36 score, the average was 88.4 in the LCP group, 90.3 and 91.4, respectively, in the IMN and EF groups (with no statistically significant difference). Regarding the results of the psychological subcategories, however, they were better in the IMN group, with p<0.05, compared to the other two groups.
Table 3.
Trend of the Follow-Up to two years of quality of life measured by The Short Form Health Survey (SF-36). At the twelfth month of follow-up there was not a statistically significant difference (p. >0.05) between the three groups.
One patient of the IMN group had a transient paralysis of the radial nerve, which resolved itself spontaneously.
In the EF group, the external fixator was removed on average after 89 days (56-123) and all fractures radiologically showed complete healing after 6 months.
Regarding infectious complications, there were no deep infections. Only the EF group had 8 cases of secretions at the pin tract level, which resolved with oral antibiotic therapy using amoxicillin 1 g/day for 7 days.
4. DISCUSSION
The management of diaphyseal humeral fractures remains controversial [17]. Fractures of the humeral shaft resulting from low-energy trauma can be treated successfully with conservative methods [18,19]. This approach combines the advantages of non-operative management with the benefits of early functional treatment. Surgical treatment is reserved for exposed fractures, in cases of neurovascular injury, in obese patients in polytrauma, in patients with extension of the fracture into the joints, and conservative treatment fails [20,21]. Often, patients request the possibility of early mobilization and without restrictions, which is why there has been an increase in the use of surgery. Beyond that, several studies report disadvantages of conservative treatment with high percentages of nonunion, especially in certain fracture patterns and loss of reduction compared to surgical treatment [22].
An advantage of the conservative treatment is the fact that the humerus is not a load bearing limb and deformity can tolerate up to 30° varus, 20° in procuravatum, and shortenings up to 4cm and therefore, does not necessitate an anatomical reduction of extra-articular fractures [23]. The conservative treatment can lead, however, to a certain loss of extra-rotation, flexion and abduction of the shoulder in 10% to 30% of cases. Furthermore, in about 10% of the patients, there may be a loss of flexion and extension of the elbow [24-25].
Regarding the surgical techniques, there are different operating methods: plate osteosynthesis, intramedullary nails and external fixation.
The plate osteosynthesis allows anatomical reduction of the fracture, the direct viewing, interfragmentary compression of the fracture and the chance to explore and isolate the radial nerve [21]. Nowadays, various studies consider it superior to intramedullary nailing and it remains the preferred technique in the fractures of the humeral shaft [26-28]. However, this technique has the disadvantage of extensive surgical dissections, as well as soft tissue and the radial nerve damage [21]. Moreover, the presence of unsightly scars and the opening of the central point of fracture with the loss of the hematoma fracture, represent other disadvantages of this technique [29]. The most recent plates (LCDCP) give better results than previous ones and can also be used with minimally invasive techniques [30]. This study did not produce statistically significant differences in the ASES score in patients treated with plates with respect to the other two groups, but there was higher blood loss and a longer surgery duration. Intramedullary nails have gained popularity in recent years due to their load-sharing properties, better aesthetic results due to smaller incisions, and how they preserve the biology of the fracture. Load-sharing properties of IMN are especially useful in osteoporotic patients who, today, are a growing proportion [31].
Initially, doubts regarding the use of nails were due to the high percentage of re-operations due to technical errors and the high rate of nonunion [29]. Other studies have described joint stiffness at the entry point of the nail and impingement symptoms [32,33]. The introduction of the nail through the rotator cuff creating irreversible damage and limitation of shoulder mobility, has been the subject of debate in past decades. However, more recent studies have demonstrated the safety of this technique, probably due to being more cautious with the rotator cuff [34]. O’Donnell [34], in a study of 33 patients with an intramedullary nail, who underwent an MRI on the 11th post-operative day, found complications in 21 patients (63.6%): 10 had sub-acromial bursitis, 5 had a partial tear of the rotator cuff, one had a complete rupture of the supraspinatus and 4 had inflammatory changes of the acromioclavicular joint. These problems with the morbidity of nail entry point level can be reduced with a transversal approach to rotator cuff tendons and their reconstruction after placement of the nail [35].
In our study, only 1 patient developed nonunion (3.8%) after IMN for humeral shaft fractures. A recent Cochrane review states that the union rate after IMN is comparable to that of [35] plates. Other authors insist that the reductions listed in the percentage of nonunion depends on proper surgical technique and the elimination of the fracture gap [30,36,37].
In our opinion, the improvements in surgical technique and implant design have improved the results of IMN compared with past decades. In fact, the current nails are wider, more rigid and allow for a dynamic compression of the fracture. They also have multiple and multi-directional points of fixation both proximally and distally, in order to ensure an angular stability [38].
As for external fixation, international literature has very few articles regarding the treatment of diaphyseal fractures of the humerus with external fixation. The main indications for the use of external fixation in diaphyseal humeral fractures are open fractures, polytrauma patients, patients with severe skin problems, gunshot wounds and pediatric fractures [39-40].
We have expanded this indication for the ease and rapidity of application, ease of reduction, good fracture stabilization, the possibility of maintaining the reduction over time and the opportunity to correct eventual decompositions during the treatment. Furthermore, it is a less invasive technique with respect to the others, it doesn’t cause lesions at the level of the rotator cuff or elbow joint, and it doesn’t damage the biology of the fracture. One of the main features that differentiates the external fixation from the other methods of treatment is its’ ability to ensure adequate stability without excessive rigidity, which is crucial for a good healing of the fracture. One of the main limitations of external fixation is patient compliance and the possibility of injuries to the radial nerve during the insertion of the distal pins. No patients in our cases of external fixation showed nonunion, and there were only 8 cases of Grade 1 pin tract secretions according to the CkChan’s scale, and they were resolved with oral antibiotic therapy [41].
As for the functional evaluation performed with SF-36, there were no significant differences between the three groups. The differences in the subjective results of the SF-36 score are due, primarily, to the psychological condition of the patient. In fact, despite the minimally invasive intramedullary nailing, very often the patients complain of rotator cuff pain, generally caused by the surgical procedure. On the contrary, patients treated with plates, sometimes, report pain and aesthetic damage in the area of the incision. Lastly, some patients treated with modular external fixation complain of the fixator. This affects compliance, but at the same time, it is positively balanced by the awareness that no additional surgery has to be performed for the removal of any internal devices.
5. CONCLUSION
From the results of our study, it is clear that the treatment of humeral shaft fractures guarantee overlapping results with the use of plates, of intramedullary nails, or with the external fixator. Consequently, the choice of which technique to use should be determined based on the experience of the operator and patient compliance.
Footnotes
• Conflict of interest: none declared.
Author’s contribution: Michele Bisaccia, Luigi Meccariello, Giuseppe Rinonapoli, Giuseppe Rollo, Marco Pellegrino, Andrea Schiavone, Cristina Ibáñez Vicente Pellegrino Ferrara, Marco Filipponi and Auro Caraffa disclose any financial and personal relationships with other people or organizations that could inappropriately influence (bias) their work. Examples of potential conflicts of interest include employment, consultancies, stock ownership, honorarium, paid expert testimony, patent applications/registrations, and grants or other funding.
REFERENCES
- 1.Cole PA, Wijdicks CA. The operative treatment of diaphyseal humeral shaft fractures, Hand Clin. 2007;23:437–48. doi: 10.1016/j.hcl.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Ekholm R, Adami J, Tidermark J, et al. Fractures of the shaft of the humerus: an epidemiological study of 401 fractures. J Bone Joint Surg Br. 2006;88:1469–73. doi: 10.1302/0301-620X.88B11.17634. [DOI] [PubMed] [Google Scholar]
- 3.Bisaccia M, Luigi Piscitelli, et al. Epidemiology of injuries and diseases due to overuse in rugby: observational study of the players of “Cus Perugia rugby”. International Journal of Surgery and Medicine. 2016;2(3):167–70. doi:10.5455/ijsm.rugby-injury. [Google Scholar]
- 4.Denard A, Jr, Richards JE, Obremskey WT, et al. Outcomes of nonoperativevs operative treatment of humeral shaft fractures: a retrospective study of 213 patients. Orthopedics. 2010;33:552. doi: 10.3928/01477447-20100625-16. [DOI] [PubMed] [Google Scholar]
- 5.Idoine JD, 3rd, French BG, Opalek JM, et al. Plating of acute humeral diaphyseal fractures through an anterior approach in multiple trauma patients. J Orthop Trauma. 2012;26:9–18. doi: 10.1097/BOT.0b013e318214ebd5. [DOI] [PubMed] [Google Scholar]
- 6.Kulkarni Sunil G, Varshneya Ankit, Jain Mohit, Kulkarni Vidhisha S, Kulkarni Govind S, Kulkarni Milind G, Kulkarni Ruta M. Antegrade interlocking nailing versus dynamic compression plating for humeral shaft fractures. Journal of orthopaedic surgery (Hong Kong) 2012;20(3):288–91. doi: 10.1177/230949901202000304. [DOI] [PubMed] [Google Scholar]
- 7.An Z, Zeng B, He X, Chen Q, Hu S. Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. International Orthopaedics. 2010;34(1):131–6. doi: 10.1007/s00264-009-0753-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garnavos C. Diaphyseal humeral fractures and intramedullary nailing: Can we improve outcomes?, Indian Journal of Orthopaedics. 2011;45(3):208–15. doi: 10.4103/0019-5413.67117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asen B, Rashkov M, Enchev D. Complications after interlocking intramedullary nailing of humeral shaft fractures. Injury. 2014;45:S9–S15. doi: 10.1016/j.injury.2013.10.044. [DOI] [PubMed] [Google Scholar]
- 10.Shabtai L, Dolkart O, Chechik O, Amar E, Steinberg E, Mozes G, Maman E. Incidence and Severity of Infections After Closed Reduction and External Fixation of Proximal Humeral Fractures. J Orthop Trauma. 2013;27(4):e81–6. doi: 10.1097/BOT.0b013e318269b3e9. doi:10.1097/BOT.0b013e318269b3e9. [DOI] [PubMed] [Google Scholar]
- 11.Scaglione M, Fabbri L, Dell’Omo D, Goffi A, Guido G. The role of external fixation in the treatment of humeral shaft fractures: a retrospective case study review on 85 humeral fractures. Injury. 2015;46(2):265–9. doi: 10.1016/j.injury.2014.08.045. doi:10.1016/j.injury.2014.08.045. [DOI] [PubMed] [Google Scholar]
- 12.Beckmann JT, Hung M, Bounsanga J, Wylie JD, Granger EK, Tashjian RZ. Psychometric evaluation of the PROMIS Physical Function Computerized Adaptive Test in comparison to the American Shoulder and Elbow Surgeons score and Simple Shoulder Test in patients with rotator cuff disease. J Shoulder Elbow Surg. 2015;24(12):1961–7. doi: 10.1016/j.jse.2015.06.025. doi:10.1016/j.jse.2015.06.025. [DOI] [PubMed] [Google Scholar]
- 13.Montzeri A, Gohoshtasbi A, Vahdaninia M, Gandek B. The short form health survey (SF-36): translation and validation study of the Iranian version, Qual Life Res. 2005;14(3):875–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 14.Gao FQ, Li ZJ, Zhang K, Sun W, Zhang H. Four Methods for Calculating Blood-loss after Total Knee Arthroplasty. Chin Med J (Engl) 2015;128(21):2856–60. doi: 10.4103/0366-6999.168041. doi:10.4103/0366-6999.168041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carroll EA, Schweppe M, Langfitt M, Miller AN, Halvorson JJ. Management of humeral shaft fractures. J Am Acad Orthop Surg. 2012;20(7):423–33. doi: 10.5435/JAAOS-20-07-423. [DOI] [PubMed] [Google Scholar]
- 16.Gross JB. Estimating Allowable Blood Loss: Corrected for Dilution, Anesthesiology. 1983;58(3):277–80. doi: 10.1097/00000542-198303000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Koch PP, Gross DF, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg. 2002;11(2):143–50. doi: 10.1067/mse.2002.121634. [DOI] [PubMed] [Google Scholar]
- 18.Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000;82(4):478–86. doi: 10.2106/00004623-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Attum B, Obremskey W. Treatment of Humeral Shaft Fractures: A Critical Analysis Review. JBJS Rev. 2015;3(9) doi: 10.2106/JBJS.RVW.N.00119. doi:10.2106/JBJS.RVW.N.00119. [DOI] [PubMed] [Google Scholar]
- 20.Westrick E, Hamilton B, Toogood P, Henley B, Firoozabadi R. Humeral shaft fractures: results of operative and non-operative treatment. Int Orthop. 2016 doi: 10.1007/s00264-016-3210-7. doi:10.1007/s00264-016-3210-7. [DOI] [PubMed] [Google Scholar]
- 21.Ali E, Griffiths D, Obi N, Tytherleigh-Strong G, Van Rensburg L. Nonoperative treatment of humeral shaft fractures revisited. J Shoulder Elbow Surg. 2015;24(2):210–4. doi: 10.1016/j.jse.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 22.Klenerman L. Fractures of the shaft of the humerus. J Bone Joint Surg Br. 1996;48:105–11. [PubMed] [Google Scholar]
- 23.Koch PP, Gross DF, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg. 2002;11(2):143–50. doi: 10.1067/mse.2002.121634. [DOI] [PubMed] [Google Scholar]
- 24.Fjalestad T, Strømsøe K, Salvesen P, Rostad B. Functional results of braced humeral diaphyseal fractures: why do 38% lose external rotation of the shoulder? Arch Orthop Trauma Surg. 2000;120(5-6):281–5. doi: 10.1007/s004020050465. [DOI] [PubMed] [Google Scholar]
- 25.Ma J, Xing D, Ma X, Gao F, Wei Q, Jia H, Feng R, Yu J, Wang J. Intramedullary nail versus dynamic compression plate fixation in treating humeral shaft fractures: grading the evidence through a meta-analysis. PLoS One. 2013;8(12):e82075. doi: 10.1371/journal.pone.0082075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dai J, Chai Y, Wang C, Wen G. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures: a meta-analysis of RCTs and nonrandomized studies. J Orthop Sci. 0014;19(2):282–91. doi: 10.1007/s00776-013-0497-8. [DOI] [PubMed] [Google Scholar]
- 27.Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011;(6):CD005959. doi: 10.1002/14651858.CD005959.pub2. [DOI] [PubMed] [Google Scholar]
- 28.Walker M, Palumbo B, Badman B, Brooks J, Van Gelderen J, Mighell M. Humeral shaft fractures: a review. J Shoulder Elbow Surg. 2011;20(5):833–44. doi: 10.1016/j.jse.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 29.Livani B, Belangero WD, Castro de Medeiros R. Fractures of the distalthird of the humerus with palsy of the radial nerve: management using minimally-invasive percutaneous plate osteosynthesis. J Bone Joint Surg Br. 2006;88(12):1625–8. doi: 10.1302/0301-620X.88B12.17924. [DOI] [PubMed] [Google Scholar]
- 30.Rommens PM, Kuechle R, Bord T, Lewens T, Engelmann R, Blum J. Humeral nailing revisited, Injury. 2008;39(12):1319–28. doi: 10.1016/j.injury.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 31.Robinson CM, Bell KM, Court-Brown CM, McQueen MM. Locked nailing of humeral shaft fractures. Experience in Edinburgh over a two-year period. J Bone Joint Surg Br. 1992;74(4):558–62. doi: 10.1302/0301-620X.74B4.1624516. [DOI] [PubMed] [Google Scholar]
- 32.Ouyang H, Xiong J, Xiang P, Cui Z, Chen L, Yu B. Plate versus intramedullary nail fixation in the treatment of humeral shaft fractures: an updated meta-analysis. J Shoulder Elbow Surg. 2013;22(3):387–95. doi: 10.1016/j.jse.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Verdano MA, Pellegrini A, Schiavi P, Somenzi L, Concari G, Ceccarelli F. Humeral shaft fractures treated with antegrade intramedullary nailing: what are the consequences for the rotator cuff? Int Orthop. 2013;37(10):2001–7. doi: 10.1007/s00264-013-2007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Donnell TM, McKenna JV, Kenny P, Keogh P, O’Flanagan SJ. Concomitant injuries to the ipsilateral shoulder in patients with a fracture of the diaphysis of the humerus. J Bone Joint Surg Br. 2008;90(1):61–5. doi: 10.1302/0301-620X.90B1.19215. [DOI] [PubMed] [Google Scholar]
- 35.Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011;(6):CD005959. doi: 10.1002/14651858.CD005959.pub2. [DOI] [PubMed] [Google Scholar]
- 36.Tsourvakas S, Alexandropoulos C, Papachristos I, Tsakoumis G, Ameridis N. Treatment of humeral shaft fractures with antegrade intramedullary locking nail, Musculoskelet Surg. 2011;95(3):193–8. doi: 10.1007/s12306-011-0126-7. [DOI] [PubMed] [Google Scholar]
- 37.Cole PA, Wijdicks CA. The operative treatment of diaphyseal humeral shaft fractures, Hand Clin. 2007;23(4):437–48. doi: 10.1016/j.hcl.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 38.Spiguel AR, Steffner RJ. Humeral shaft fractures. Curr Rev Musculoskelet Med. 2012;5(3):177–83. doi: 10.1007/s12178-012-9125-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Okcu G, Aktuglu K. Management of shotgun-induced fractures of the humerus with Ilizarov external fixator. J Orthop Traumatol. 2004;2:92–7. [PubMed] [Google Scholar]
- 40.Bisaccia M, Meccariello L, Manni M, et al. Treatment of acute proximal humeral fractures in children with modular external fixator. JAD. 2016;5(6):497–501. doi:10.1016/j.joad.2016.08.021. [Google Scholar]
- 41.Bisaccia M, Manni M, Colleluori G, et al. The management of pin-care in external fixation technique: Povidone-iodine versus sodium hypochlorite 0,05% (Amukina-med®) medications. EMBJ. 2016;11(10):81–7. doi:10.3269/1970-5492.2016.11.10. [Google Scholar]


