Abstract
Objective:
Tobacco cigarette smoking is one of the major leading causes of death throughout the world. Smoking has both acute and chronic effect on haematological parameters. The aim of the present study was to assess the extent of adverse effects of cigarette smoking on biochemical characteristics in healthy smokers.
Subjects and Method:
One hundred and fifty six subjects participated in this study, 56 smokers and 100 non-smokers. The smokers were regularly consuming 10-20 cigarettes per day for at least 3 years. Complete blood cell count was analyzed by CELL-DYN 3700 fully automatic haematological analyzer.
Results:
The smokers had significantly higher levels of white blood cell (p<0,001), hemoglobin (p=0,042), mean corpuscular volume (p=0,001) and mean corpuscular hemoglobin concentration (p<0,001). All other measured parameters did not differ significantly. Cigarette smoking caused a significant increase (p<0,001) in red blood cells, white blood cells (p=0,040), hemoglobin (p<0,001), hematocrit (p=0,047) and mean corpuscular hemoglobin (p<0,001) in males in comparison to female smokers.
Conclusion:
In conclusion, our study showed that continuous cigarette smoking has severe adverse effects on haematological parameters (e.g., hemoglobin, white blood cells count, mean corpuscular volume, mean corpuscular hemoglobin concentration, red blood cells count, hematocrit) and these alterations might be associated with a greater risk for developing atherosclerosis, polycythemia vera, chronic obstructive pulmonary disease and/or cardiovascular diseases.
Keywords: cigarette smoking, haematological parameters, healthy population
1. INTRODUCTION
According to the data of the World Health Organization, approximately 5 million people die globally each year from the diseases caused by smoking, and if this trend continues, it is expected that by 2015, that number would be 10 million.
Numerous studies indicated that smoking had adverse effects on human health and represented a predisposing factor for development of various pathological conditions and diseases, such as the chronic obstructive pulmonary disease (1), cancer (2), pancreatitis (3), gastrointestinal disorders (4), periodontal disease (5), metabolic syndrome (6), and some autoimmune diseases (7).
Cigarette smoking is associated with an increased risk of cardiovascular diseases, including coronary artery disease, peripheral vascular disease (8), ischaemic heart disease (9), atherosclerosis (10), myocardial infarction (10) and stroke (11).
The exact mechanisms of occurrence of these disorders in smokers are not known, but it is presumed that these effects are caused by abnormalities in the blood rheology, infection and inflammation, oxidative stress, and alterations of antithrombotic and fibrinolysis system.
Tobacco smoke contains over 4000 compounds that have a more or a less adverse effect on human health, among which free radicals, the nicotine and the carbon monoxide are considered the most responsible for pharmacological effects.
The nicotine induces formation of a clot in the coronary arteries, it weakens the vascular activity, and increases endothelium dysfunction. Increase in the level of carboxy-haemoglobin may cause hypoxia, and it is also responsible for sub-endotheliaoedema considering that it alters the vascular permeability and accumulation of lipids (12).
Free radicals and peroxides from the tobacco smoke are clearly linked with physiological phenomenon such as synthesis of prostaglandins and thromboxane, and they are also involved in the pathogenesis of various diseases including atherosclerosis, carcinoma, and inflammatory processes.
Effects of smoking on alterations of hemostatic and fibrinolythic system, antioxidant status and hematology parameters were extensively studied, but the studies presented inconsistent results. The present study was conducted to compare the effect of cigarette smoking on some haematological parameters between smokers and age-matched non-smoker controls.
2. METHODS
Patients
Present study was carried out to investigate the relationship effect of cigarette smoking on haematological parameters in a group of clinically healthy volunteers. A total of 156 subjects were enrolled in the study, 56 smokers and 100 non-smokers in the age range 40-55 years. The subjects were recruited from the Clinical Centre of the University in Sarajevo and the General Hospital Tešanj. The smokers were regularly consuming 10-20 cigarettes per day for at least 3 years. Each subject gave an informed consent and study protocol was approved by the Ethical Review Committee. Data on smoking habits and the amount of tobacco consumed were collected by a self-administered questionnaire to be filled in by the participants. Subjects included in this study were free of evidence of active liver and kidney disease, chronic pancreatitis, gastrointestinal disease, inflammatory bowel, history of ischaemic heart disease or and diastolic blood pressure, endocrine disorders, infection, and hormonal therapy.
Anthropometric and biochemical measurements
In all the subjects arterial blood pressure, blood pressure and anthropometric data (height, weight and waist circumference) were measured. Waist circumference was measured at the midpoint between the lowest rib and the iliac crest. BMI was calculated as body weight (kg) divided by body height (m) squared. Blood pressure of each subject was measured with a mercury Sphygmomanometer and a standard stethoscope. Blood samples were drawn after an overnight fast. Each test procedure was carried out between 7-10 a.m.
The subjects underwent the following tests: Blood pressure examination to rule out hypertension, estimation of the serum lipid profile, evaluation of the fasting and post prandial blood glucose levels to rule out diabetes, red blood cell count, total leukocyte count, differential leukocyte count, platelet count, packed cell volume, hemoglobin, serum urea and creatinine levels. Complete blood cell count was analyzed by CELL-DYN 3700 fully automatic haematological analyzer.
Statistical analysis
Statistical analysis was performed using SPSS version 20.0 (SPSS Inc.). Before statistical analysis, normal distribution and homogeneity of the variances were tested using Kolmogorov-Smirnov test respectively. Groups were compared using Student’s unpaired t test for parameters with normal distribution or Mann–Whitney test for parameters with non-normal distribution. Correlations between parameters were analyzed using the Pearson R test for variables with normal distribution and the Spearman test for variables with non-normal distribution. Data are expressed as mean ± standard deviation or medians (interquartile range). P < 0,05 was considered significant.
3. RESULTS
Table 1 shows baseline characteristics of 156 subjects. The Mean ± SD age of subjects was 50,00 ± 0,477 years. All the subjects were normotensive having mean systolic blood pressure 122,33 ± 1,093 and mean diastolic blood pressure 79.85 ± 0.498.
Table 1.
Baseline characteristics of the subjects. Data expressed as Mean ± SD
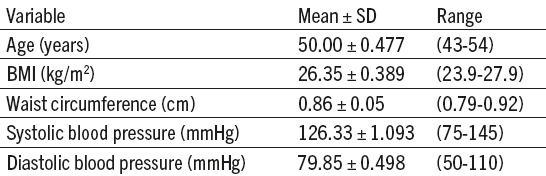
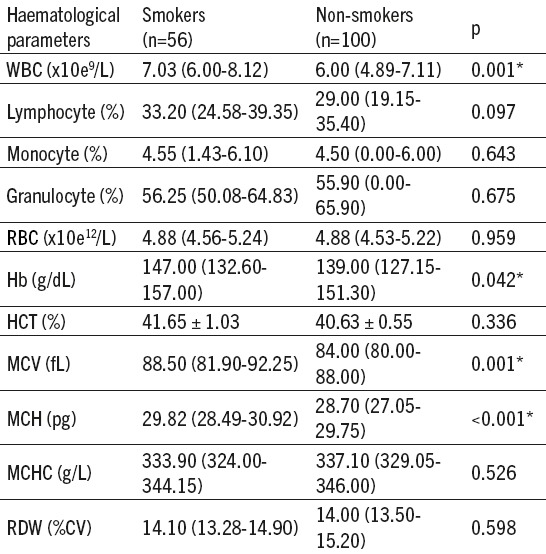
Table 2 compares the haematological parameters between smokers and non-smokers which shows a statistically significant increase in total leucocyte count, hematocrit, mean corpuscular hemoglobin and hemoglobin in smokers. The rest of the parameters were not statistically significant.
Table 2.
Comparison of haematological parameters between smokers and non-smokers. Data are presented as means ± SD or medians (interquartile range). *Significance of difference in Mann-Whitney test for data following non-normal distributed and t-test for normal distributed date. WBC-White blood cells, RBC-Red blood cells, HB-Haemoglobin, HTC-Haematocrit, MCV-Mean Corpuscular Volume, MCH-Mean Corpuscular Haemoglobin, MCHC-Mean Corpuscular Haemoglobin Concentration, RDW-Red Blood Cell Distribution Width
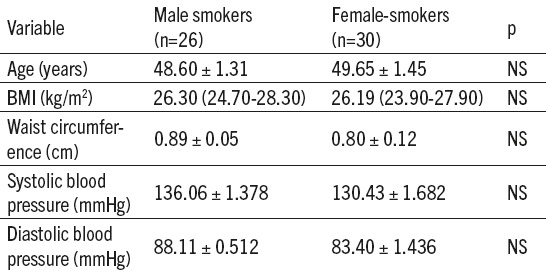
After the analysis of the effects of cigarette smoking on haematological parameters of all the participants in the study, we divided a group of smokers (n= 56) by sex. The Table 3 shows that there was no statistically significant difference in age, body mass index (BMI), waist circumference and blood pressure between the male and female smokers.
Table 3.
Baseline characteristics of the smoker subjects -gender differences. Data are presented as means ± SD or medians (interquartile range), NS-Non-significance of difference in Mann-Whitney test for data following non-normal distributed and t-test for normal distributed date. BMI-body mass index.
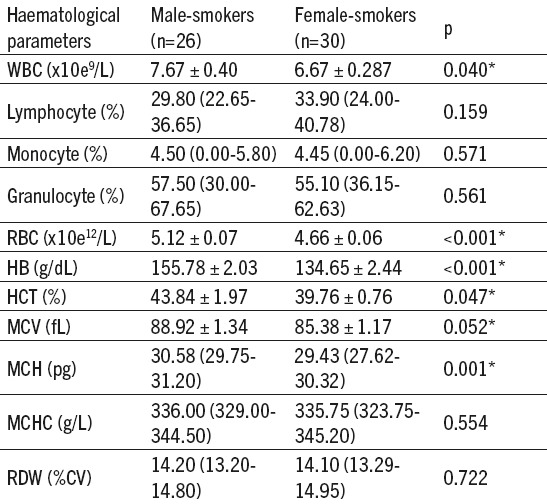
The analysis of gender differences in the group of smokers showed statistically significant difference in the number of leukocytes. The values of leukocytes were statistically higher in male subjects compared to female respondents. A statistically significant difference between other parameters of white blood cells is not found. Male population of smokers had a statistically higher values for the number of red blood cells and hemoglobin, hematocrit, mean corpuscular volume (MCV) and mean corpuscular hemoglobin (MCH) values (Table 4).
Table 4.
Differences haematological parameters between male and female smokers. Data are presented as means ± SD or medians (interquartile range). *Significance of difference in Mann-Whitney test for data following non-normal distributed and t-test for normal distributed date. WBC-White blood cells, RBC-Red blood cells, HB-Haemoglobin, HTC-Haematocrit, MCV-Mean Corpuscular Volume, MCH-Mean Corpuscular Haemoglobin, MCHC-Mean Corpuscular Haemoglobin Concentration, RDW-Red Blood Cell Distribution Width.
4. DISCUSSION
The results of our findings showed that cigarette smoking has severe adverse effects on haematological parameters (e.g., hemoglobin - Hb, hematocrit - HCT, white blood cells count - WBC, red blood cells count - RBC, MVC, MCH).
Smokers and non-smokers had almost equal values of the total erythrocyte count. Statistically significant larger values of erythrocytes were noted in male smokers in relation to female smokers.
In our study, the values of hemoglobin were significantly larger in smokers than in non-smokers regardless of the sex, while there was no significant difference in values of hematocrit between these two groups of subjects. However, male smokers had significantly larger values of hematocrit in relation to female smokers. The significant increase in Hb in smoker group is correlated with previous studies (13-15).
In study made by Lakshmi et al. (16) the hematocrit and Hb level were significantly higher in smokers and among the smokers the RBC count was significantly increased as the intensity of smoking increases. White head et al. in their study observed that hemoglobin concentration and hematocrit was significantly increased in those smoking more than 10 cigarettes per day (17).
Increase in hemoglobin concentration is believed to be mediated by exposure of carbon monoxide and some scientists suggested that increase in hemoglobin level in blood of smokers could be a compensatory mechanism. Carbon monoxide binds to Hb to form carboxy hemoglobin, an inactive form of hemoglobin having no oxygen carrying capacity. Carboxyhemoglobin also shifts the Hb dissociation curve in the left side, resulting in a reduction in ability of Hb to deliver oxygen to the tissue. To compensate the decreased oxygen delivering capacity, smokers maintain a higher hemoglobin level than non-smokers (18).
Increased number of erythrocytes and values of hematocrit in male smokers can be explained by the fact that tissue hypoxia caused by increased creation of carboxy hemoglobin leads to an increased secretion of erythropoietin, thus increasing erythropoiesis. Carbon monoxide from the tobacco smoke also leads to an increase in permeability of the capillaries which decreases the volume of plasma, which finally mimics the condition of polycythemia, characterized by an increased share of the erythrocytes in the blood volume, which is reflected also through increased values of hematocrit (14, 19).
MCV, MCH and MCHC are three main red blood cell indices that help in measuring the average size and hemoglobin composition of the red blood cells.
Our study established significantly larger values of mean corpuscular volume (MCV) and mean corpuscular hemoglobin (MCH) among smokers, while differences in values of MCHC and RDW were not significant between smokers and non-smokers. Larger values of MCV and MCH in smokers, in relation to non-smokers were confirmed by other studies as well (20, 21). In the study of Kung et al. (21), the values of these parameters exceeded the values of the reference interval and were characteristic for findings for some diseases such as kidney dysfunction, hyperuricaemia, hypertensio nor hypercholesterolemia. These results contradict the results of the study Pankaj et al. (22) who did not find any significant changes in MCV and MCH between smokers and non-smokers. They found significantly low value of MCHC (p<0,009) among smokers.
In contrast our finding, in study made by Salamzadeh, the amounts of MCH and MCHC in the smoker group were significantly lower (p<0,05) compared to those of the non-smoker group (23). No difference was observed between the platelets count and MCV in two groups.
Asif et al. found increase in MCV and decrease in MCH and MCHC levels in smokers (24). MCV indicates the size of a red blood cell and presence of red cells smaller or larger than normal size means the person has anemia, elevated levels of MCV in our study indicates that subjects might suffer from megaloblastic, haemolytic, pernicious or macrocytic anemia usually caused by iron and folic acid deficiencies.
MCH is the average weight of hemoglobin that is present inside single red blood cell whereas MCHC denotes the amount of hemoglobin in a specific volume of ‘packed’ red corpuscles or cells.
Our study established a significantly larger number of leukocytes in smokers of both sexes, in relation to non-smokers. Also, the values of leukocyte count were statistically significantly larger in male smokers.
The increased total leukocyte count observed in smokers is similar to earlier studies (25, 26). Although the exact mechanism of how smoking increases the number of leukocytes is not fully clarified, the smoking induced leukocytosis has several factors and can be explained in different ways.
Some authors claim that increase in the number of leukocytes can be the consequence of nicotine induced release of catecholamine and steroid hormones from the core of the adrenal gland. It is known that increase in the level of certain endogenic hormones, such as epinephrine and cortisol, result in increase in the number of leukocytes (27, 28). Additionally, the irritating effect of the tobacco smoke on the respiratory tree with the resulting inflammation can also contribute to increase in the number of leukocytes. It was established that inflammatory stimulation of the respiratory tract induces the increase of the inflammatory markers in circulation, especially cytokines, which affect the number of leukocytes.
The best characterized responses of microcirculation to inflammation include a decreased vasomotor function, reduced capillary perfusion, adhesion of leukocytes and thrombocytes, activation of coagulation cascade and increased thrombosis, increased vascular permeability, and increase in the rate of proliferation of blood and lymphatic vessels. The answer to inflammation is activation of various cells that normally circulate in the blood (leukocytes, thrombocytes) or exist in the walls of blood vessels (endothelial cells, pericytes) or in the perivascular space (fat cells, macrophages) (29).
Adhesion of leukocytes on vascular endothelium is a trademark of inflammatory processes. Leukocytes are tied to endothelium and stay inert, after which they can migrate in the intercellular space between those very cells. The whole process of leukocyte adhesion on endothelium cells is regulated by sequential activation of various families of adhesion molecules, which are situated on the cell surface and facilitate cell interaction, fixation of the cells on the wall of blood vessels, and their movement. Lecithin-like adhesion glycoproteins, so called selectins, mediate in movement of leukocytes, while firm adhesion and subsequent trans-endothelium migration of leukocytesis mediated by interaction of integrin (CD11/CD18, VLA-4) situated on leukocytes and immunoglobulin-like adhesion molecules on endothelium cells (ICAM-1, VCAM-1) (30).
It is possible that increased number of leukocytes in peripheral blood of healthy smokers is linked with the phenomenon of cell movement from other lymphoid organs in the peripheral blood or that smoking decreases the ability of adhesion of these cells on endothelium cells of blood vessels, which leads to general increase in the number of blood cells (31).
Reports on differential blood work related with smoking are not consistent. Aula and Qadir demonstrated significant increase in leukocytes, neutrophils, eosinophils, basophils, lymphocytes and monocytes in smokers in relation to the control group of non-smokers (32). From the other side, Kastelein et al. established no significant difference in values of neutrophils in middle-aged smokers and non-smokers (33). The same results were demonstrated by our study as well, where the values of granulocytes, which include neutrophils, were not significantly increased. However, unlike the study of Kasteleinaet al., which established in smokers statistically significantly larger values of basophils, lymphocytes and monocytes, our study did not confirm the influence of the smoking status on the said parameters of the white blood line in healthy volunteers.
It is assumed that atherogenic effect of cigarette smoking may be partially mediated by leukocytes. The Leukocyte number represents maybe the most useful and simple biomarker of endothelium damage. Presence of chronically increased number of leukocytes in smokers contributes in pathogenesis of smoking related diseases, especially ischaemic vascular disease, considering that increase in aggregation of leukocytes predisposes microcirculatory occlusion and vascular damage. Several studies confirmed that the number of leukocytes represents an independent predictor of atherosclerosis and cardiovascular diseases (34, 35). High leukocyte number in smokers, especially in males, established in our study, points that they have a higher risk of atherosclerosis and cardiovascular diseases in relation to non-smokers.
5. CONCLUSION
From the present study, we can concluded that continuous cigarette smoking increases erythrocyte count, hemoglobin concentration, hematocrit, leukocyte count, mean corpuscular volume and mean corpuscular hemoglobin concentration and these alterations might be associated with a greater risk for developing atherosclerosis, polycythaemiavera, chronic obstructive pulmonary disease and/or cardiovascular diseases.
Acknowledgments
Author thank all subject who participated in the study, as well as to the physicians and paramedical staff from the Department of Endocrinology, Clinical Center University of Sarajevo and General Hospital Tesanj who assisted in the study.
Footnotes
• Declaration of interest: Authors have no conflict of interest to declare.
REFERENCES
- 1.Buist AS, Vollmer WM, McBurnie MA. Worldwide burden of COPD in high- and low-income countries. Part I. The Burden of Obstructive Lung Disease (BOLD) Initiative. Int J Tuberc Lung Dis. 2008;12:703–8. [PubMed] [Google Scholar]
- 2.Vineis P, Alavanja M, Buffler P, Fontham E, Franceschi S, Gao YT, et al. Tobacco and cancer: recent epidemiological evidence. Journal of the National Cancer Institute. 2004;96(2):99–106. doi: 10.1093/jnci/djh014. [DOI] [PubMed] [Google Scholar]
- 3.Barreto SG. How does cigarette smoking cause acute pancreatitis? Pancreatology: official journal of the International Association of Pancreatology. 2016;16(2):157–63. doi: 10.1016/j.pan.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Li LF, Chan RL, Lu L, Shen J, Zhang L, Wu WK, et al. Cigarette smoking and gastrointestinal diseases: the causal relationship and underlying molecular mechanisms (review) International journal of molecular medicine. 2014;34(2):372–80. doi: 10.3892/ijmm.2014.1786. [DOI] [PubMed] [Google Scholar]
- 5.Gautam DK, Jindal V, Gupta SC, Tuli A, Kotwal B, Thakur R. Effect of cigarette smoking on the periodontal health status: A comparative, cross sectional study. Journal of Indian Society of Periodontology. 2011;15(4):383–7. doi: 10.4103/0972-124X.92575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slagter SN, van Vliet-Ostaptchouk JV, Vonk JM, Boezen HM, Dullaart RP, Kobold AC, et al. Associations between smoking, components of metabolic syndrome and lipoprotein particle size. BMC medicine. 2013;11:195. doi: 10.1186/1741-7015-11-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harel-Meir M, Sherer Y, Shoenfeld Y. Tobacco smoking and autoimmune rheumatic diseases. Nature clinical practice Rheumatology. 2007;3(12):707–15. doi: 10.1038/ncprheum0655. [DOI] [PubMed] [Google Scholar]
- 8.Lu JT, Creager MA. The relationship of cigarette smoking to peripheral arterial disease. Reviews in cardiovascular medicine. 2004;5(4):189–93. [PubMed] [Google Scholar]
- 9.Law MR, Morris JK, Wald NJ. Environmental tobacco smoke exposure and ischaemic heart disease: an evaluation of the evidence. Bmj. 1997;315(7114):973–80. doi: 10.1136/bmj.315.7114.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arteriosclerosis, thrombosis, and vascular biology. 2014;34(3):509–15. doi: 10.1161/ATVBAHA.113.300156. [DOI] [PubMed] [Google Scholar]
- 11.Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert review of cardiovascular therapy. 2010;8(7):917–32. doi: 10.1586/erc.10.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gossett LK, Johnson HM, Piper ME, Fiore MC, Baker TB, Stein JH. Smoking intensity and lipoprotein abnormalities in active smokers. Journal of clinical lipidology. 2009;3(6):372–8. doi: 10.1016/j.jacl.2009.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah BK, Nepal AK, Agrawal M, Sinha AK. The effects of cigarette smoking on hemoglobin levels compared between smokers and non-smokers. Sunsari Technical College Journal. 2012;1(1):42–4. [Google Scholar]
- 14.Nadia MM, Shamseldein HA, Sara AS. Effects of Cigarette and Shisha Smoking on Hematological Parameters: An analytic case-control study. International Multispeciality Journal of Health. 2015;1(10):44–51. [Google Scholar]
- 15.Jena SK, Purohit KC, Misra AK. Effect of Chrnoic Smoking on Hematological Parameteres. International Journal of Current Research. 2013;5(2):279–82. [Google Scholar]
- 16.Lakshmi AS, Lakshmanan A, Kumar GP, Saravanan A. Effect of Intensity of Cigarette Smoking on Haematological and Lipid Parameters. Journal of Clinical and Diagnostic Research. 2014;8(7):11–3. doi: 10.7860/JCDR/2014/9545.4612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitehead TP, Robinson D, Allaway SL, Hale AC. The effects of cigarette smoking and alcohol consumption on blood hemoglobin, erythrocytes and leukocytes: a dose related study on male subjects. Clinical and laboratory hematology. 1995;17(2):131–8. [PubMed] [Google Scholar]
- 18.Aitchison R, Russell N. Smoking - a major cause of polycythaemia. Journal of the Royal Society of Medicine. 1988;81(2):89–91. doi: 10.1177/014107688808100212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verma RJ, Patel CS. Effect of smoking on Haematological parameters in Human Beings. Journal of Cell and Tissue Research. 2015;5(1):337. [Google Scholar]
- 20.Khan MI, Bukhari MH, Akhtar MS, Brar S. Effect of smoking on Red Blood Cells Count, Hemoglobin Concentration and Red Cell indices. P J M H S. 2014;8(2):361–4. [Google Scholar]
- 21.Kung CM, Wang HL, Tseng ZL. Cigarette smoking exacerbates health problems in young men. Clinical and investigative medicine Medecine clinique et experimentale. 2008;31(3):E138–49. doi: 10.25011/cim.v31i3.3471. [DOI] [PubMed] [Google Scholar]
- 22.Pankaj J, Reena J, Mal KL, Ketan M. Effect of cigarette smoking on haematological parameters: comparison between male smokers and non-smokers. IJSN. 2014;5(4):740–3. [Google Scholar]
- 23.Salamzadeh J. The hematologic effects of cigarette smoking in healthy men volunteers. Article. 2004;3:41–4. [Google Scholar]
- 24.Asif M KS, Umar Z, Malik A, et al. Effect of cigarette smoking based on haematological parameters: comparison between male smokers and non-smokers. Turkish Journal of Biochemistry. 2013;38(1):75–80. [Google Scholar]
- 25.Inal B, Hacibekiroglu T, Cavus B, Musaoglu Z, Demir H, Karadag B. Effects of smoking on healthy young men’s hematologic parameters. Northern clinics of Istanbul. 2014;1(1):19–25. doi: 10.14744/nci.2014.39974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Higuchi T, Omata F, Tsuchihashi K, Higashioka K, Koyamada R, Okada S. Current cigarette smoking is a reversible cause of elevated white blood cell count: Cross-sectional and longitudinal studies. Preventive medicine reports. 2016;4:417–22. doi: 10.1016/j.pmedr.2016.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kapoor D, Jones TH. Smoking and hormones in health and endocrine disorders. European journal of endocrinology. 2005;152(4):491–9. doi: 10.1530/eje.1.01867. [DOI] [PubMed] [Google Scholar]
- 28.Deutsch V, Lerner-Geva L, Reches A, Boyko V, Limor R, Grisaru D. Sustained leukocyte count during rising cortisol level. Acta haematologica. 2007;118(2):73–6. doi: 10.1159/000103216. [DOI] [PubMed] [Google Scholar]
- 29.Granger DN, Senchenkova E. Inflammation and the Microcirculation. San Rafael (CA) 2010 [PubMed] [Google Scholar]
- 30.Langer HF, Chavakis T. Leukocyte-endothelial interactions in inflammation. Journal of cellular and molecular medicine. 2009;13(7):1211–20. doi: 10.1111/j.1582-4934.2009.00811.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parry H, Cohen S, Schlarb JE, Tyrrell DA, Fisher A, Russell MA, et al. Smoking, alcohol consumption, and leukocyte counts. American journal of clinical pathology. 1997;107(1):64–7. doi: 10.1093/ajcp/107.1.64. [DOI] [PubMed] [Google Scholar]
- 32.Aula FA, Qadir FA. Effects of Cigarette Smoking on Some Immunological and Hematological Parameters in Male Smokers in Erbil City. Jordan Journal of Biological Sciences. 2012;6(2):159–66. [Google Scholar]
- 33.Kastelein TE, Duffield R, Marino FE. Acute Immune-Inflammatory Responses to a Single Bout of Aerobic Exercise in Smokers;The Effect of Smoking History and Status. Frontiers in immunology. 2015;6:634. doi: 10.3389/fimmu.2015.00634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Madjid M, Awan I, Willerson JT, Casscells SW. Leukocyte count and coronary heart disease: implications for risk assessment. Journal of the American College of Cardiology. 2004;44(10):1945–56. doi: 10.1016/j.jacc.2004.07.056. [DOI] [PubMed] [Google Scholar]
- 35.Loimaala A, Rontu R, Vuori I, Mercuri M, Lehtimaki T, Nenonen A, et al. Blood leukocyte count is a risk factor for intima-media thickening and subclinical carotid atherosclerosis in middle-aged men. Atherosclerosis. 2006;188(2):363–9. doi: 10.1016/j.atherosclerosis.2005.11.021. [DOI] [PubMed] [Google Scholar]


