Abstract
Introduction:
Stroke is one of the largest socio medical problems of modern times. In addition to the third leading cause of death, it is the first cause of non-trauma disability. Numerous studies show a correlation of risk factors and arteriosclerotic lesions in the coronary arteries and carotid arteries.
Patients and methods:
Study was conducted at the Clinical Center University of Sarajevo, Clinic for Cardiology surgery, methodologically cross-sectional study and partly manipulative and clinical prevention study, conducted on a representative sample of 100 patients. The subject was divided into 2 groups, coronary and non-coronary patients. Both groups of patients underwent color Doppler of carotid arteries, medical history and laboratory analysis.
Results:
The results confirm the hypothesis that the critical carotid artery stenosis is more present in patients with coronary disease, while the association of risk factors has been demonstrated for diabetes, hypertension and dyslipidemia.
Conclusion:
Screening of carotid arteries in patients scheduled for coronary revascularization is essential. With the presence of critical stenosis of the carotid artery, surgery of carotid artery should be done before coronary revascularization. The implementation of aggressive education and prevention of risk factors for cardiovascular disease is needed.
Keywords: carotid artery stenosis, coronary/non coronary patients, diabetes mellitus, hypertension, dyslipidemia
1. INTRODUCTION
Now a days arteriosclerotic cardiovascular disease are the leading cause of death in the World and represent the biggest problem in health systems in the developed World because of the cost, which is required for the purpose of prevention and treatment (1).
In Germany, it is the third most common cause of death, while currently in the United States there are about 4 million people who have had a stroke. Also, stroke is the most common cause of disability incurred. Only about 10% of patients fully recover (2, 3).
According to the recommendations given by the “American Heart Association Guidelines” under asymptomatic critical carotid artery indicated for surgical treatment, means the unilateral stenosis greater than 80% for patients with ulcerated plaque and patients who are scheduled for cardiac surgery (4).
In bilateral stenosis of carotid arteries, there are different opinions what degree of stenosis is an indication for surgical treatment, but the largest number of surgeons considered that it is the presence of unilateral stenosis of 65% and contralateral from 75-99%. These bilateral stenosis in most cases are with symptomatic character (5).
The highest percentage of patients who are scheduled for aortocoronary surgery are those with two vessel and three vessel coronary artery disease, and indications for surgical intervention are stenotic changes of the coronary blood vessels greater than 70% (6, 7).
2. OBJECTIVES
The aim of this study was, that in patients selected for coronary angiography, to determine the percentage of those in which critical asymptomatic carotid stenosis was present, and compare the number and correlation of risk factors in coronary and non-coronary patients. Also on the basis of the results obtained and considering the problems, to set guidelines for the prevention of stroke and reducing risk factors.
3. PATIENTS AND METHODS
The study was designed as across-sectional study, a part of the clinical and manipulative-prevention studies. The setting of the study was the Heart Center, Clinical Center University of Sarajevo.
All patients who meet the requirements for inclusion in the study and who gave their written consent were included in the study during the one calendar year. The patients were divided into two groups, the test group were patients with a positive coronary angiography finding and in whom surgery is indicated or cardiac interventional treatment, and the other, a control group, patients with a negative coronary angiography and in whom conservative treatment is indicated.
All the patients beside the medical and family history and physical examination, had laboratory analysis with a special emphasis on the presence off at in the blood.
After this analysis, color Duplex analysis of the carotid arteries with the same ultrasound machine, cardiovascular ultrasound Ocuson Siemens CV70, with linear probe of 7 MHz was done. Based on the committed color duplex scan of the carotid arteries the degree of stenosis is determined, using the grading according to NASCET study, which was graded so that the first degree of stenosis represented stenosis 0-29%, the second level of 30-69%, and third degree 70-99%.
Color Duplex scan of the carotid arteries was made by the authors of the study, and controlled by an independent certified ultrasound. Two examiners were doing the analysis independently of one another and not know in other clinical and laboratory data of the patient tested.
Statistical analysis
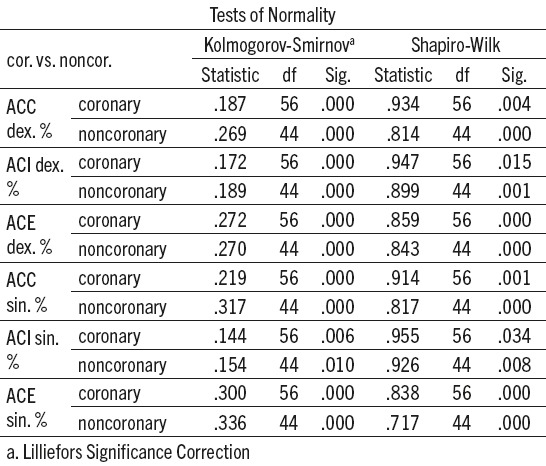
Statistical processing are done in IBM SPSS Statistics 20, Excel and STATS 2.0. We used the Kolmogorov-Smirnov and Shapiro-Wilks test to examine the normality of distribution. Furthermore, to test the hypothesis, we used the Mann-Whitney test, which tests the difference between the ranks and is used as an on parametric counter part of the t-test.
We used the t-test for measuring the difference between the two groups when it comes to parametric data. From the tests we have used, Chi square test to test the difference between the frequencies of the results, and the test of independent proportions, if the Chi Square test was not possible to implement.
Together with the Chi square test, we used the Fisher’s exact test, which is quite accurate on smaller samples and it is high lighted in the processing of the results.
4. RESULTS
To be able to determine what kind of tests we use for statistical processing for our hypothesis, we had to first of all examine the normality of the distribution of the data included in the calculation. We did the Kolmogorov-Smirnov test (K-S) and Shapiro-Wilk test (S-H). They tested the differences between our distribution and mean values of the distribution of data that have the same mean and certainly are arranged by the normal curve. If there is statistical significance, we conclude that our distribution results are significantly different from the normal distribution, and in this case we use non-parametric statistics. In the second case, we use parametric procedures.
All KS tests show that in our case the distributions are significantly different from normal value at the level of p <0.01, so we use non-parametric procedures, if we talk about the scales variables.
To determine whether there are statistically significant differences between coronary and non coronary patients when it comes to the value of stenosis of ACC, ACI and ACE, we will use the Mann-Whitney test (M-W), which is the counter part of the t-test in parametric statistics, but is calculated with mean ranks instead of the classic mean values. The Table 2. shows the values of the M-W test. As can be seen all the values show a statistically significant difference between stenosis in coronary and non coronary patients on the level of p<0.01 or p<0.05. Differences in stenosis in the location of ACC dex., ACC sin., ACI sin. and ACE sin. Were at the level of p <0.01, and the other differences were at p <0.05. All significant differences go in favor of coronary patients, or in other words, the value of stenosis are significantly higher in coronary patients.
Table 2.
The values of M-W test
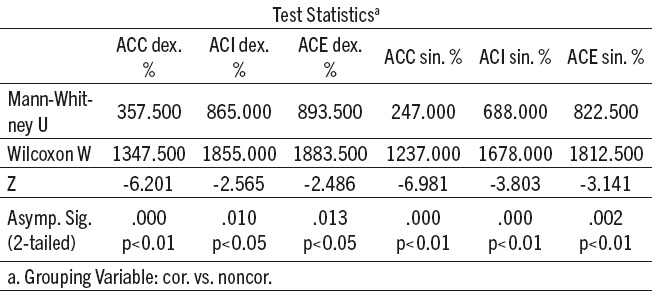
Table 1.
Tests of normality
The data in Table 3. tells us that if any of the mean values rank is higher in coronary patients, it means that the value of stenosis in that position is higher in coronary than in non coronary patients. For example, given that we have proved that there is a statistically significant difference in the location of ACC sin. at the level of p <0.01and have a mean value rank for coronary patients of MrangK=68.09 and MrangNK=28.11, it is clear that this position have higher values of stenosis in coronary patients, because the mean rank value is more than double. The same goes for other statistical differences.
Table 3.
Mean values of ranks for M-W tests
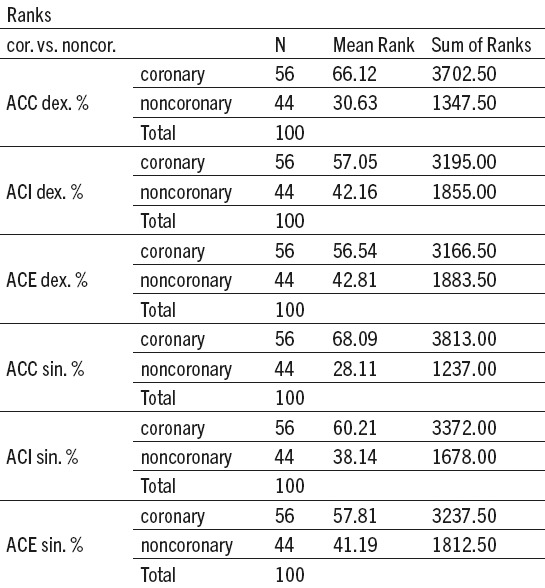
Table 4.
Stenosis values by categories-for coronary and non-coronary patients. ACC sin/dex – Artery Carotis Communis left/right; ACI sin/dex - Artery Carotis Interna left/right; ACE sin/dex – Artery Carotis Externa left/right
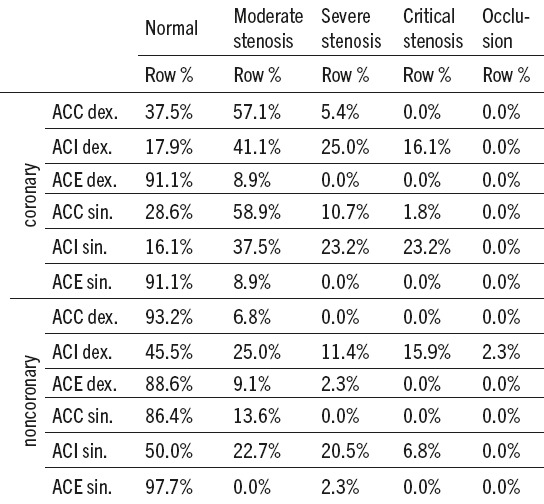
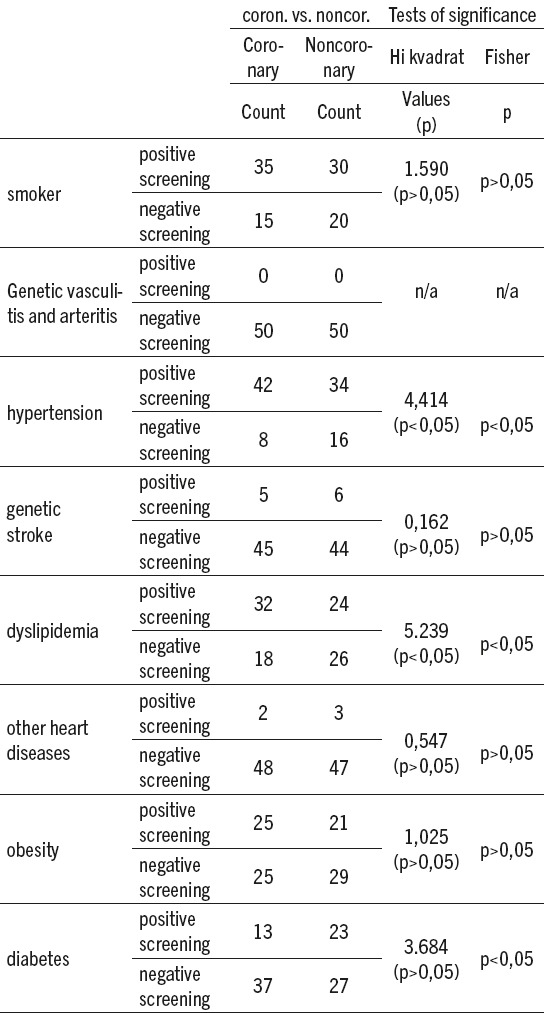
Table 5.
The values of χ2 (Chi) square and Fisher’s test with risk factors
The above table shows that we divided the values of stenosis in six positions and in the categories of normal findings, moderate stenosis, severe stenosis, critical stenosis and occlusion. What interests us are the values of critical stenosis, frequency of occurrence and the percentage reporting in relation to the coronary and non coronary patients.
In coronary patients at three positions a value was 0%, which means that at these positions sufficiently large values of stenosis were not measured. In the group of non coronary patients we had four such positions. In essence, we are able to measure whether there is a statistically significant difference between the number of patients with critical stenosis in the coronary and non coronary groups. Data gained from the independent test of proportion, saying that only between the number of critical stenosis on the position ACI sin. there is a statistically significant difference at the level of p <0.05 between coronary and non coronary patients.
The table above shows the realized frequency factors among coronary and non coronary patients as well as the corresponding values of Chi square test and Fisher. As can be see nonly a statistically significant difference was found among patients with diabetes, dyslipidemia, and those with hypertension (at the level of p <0.05). Specifically, among coronary patients, there are significantly fewer negative screening for hypertension than among non coronary patients and significantly fewer of those with a positive screening for diabetes.
None of the other factors did not show significant and in all other cases, we argue that there is no statistically significant difference between coronary and non coronary patients.
5. DISCUSSION
Coronary artery disease (CAD) is recognized as one of the possible causes of perioperative stroke. Age, other vascular disease, smoking, previous cerebrovascular events, female gender, diabetes, hypertension, carotid artery murmur are signals for screening. The presence of symptoms of carotid disease is alarming and certainly correlates with poor outcome, but the absence of symptoms is not a particular security for a good outcome. Unfortunately, the first symptom of carotid artery stenosis (CAS) in heart patients can be one of the most serious complications - stroke.
ACI stenosis has greater clinical significance than ACE stenosis. If the patient has only ACE stenosis, endarterectomy should not be done because there is no risk of brain infarction. Although ACI clinically is not significant, ACE has great significance for the collateral circulation as one of the most common collateral circulation is via branches of ACE. Large studies NASCET and ECTS confirmed the great clinical significance of ACI stenosis that is greater than 70%. It was found that patients who have symptomatic ACI stenosis greater than 70% must be exposed to carotid endarterectomy.
According to our results in 16 patients asymptomatic critical stenosis, in which it was indicated for surgical intervention, was found. Ten patients from the coronary group and 6 patients from the non coronary group were operated.
In a study by Liapis and al. They showed that the incidence of severe carotid stenosis in patients scheduled for CABG was in the range of 2.8 to 22%, depending on other comorbidity (8).
The above studies confirm that our results obtained in whole, coincide with the published study results.
In a multicenter study, which was conducted in 1662 patients with asymptomatic carotid artery disease, it was found that over 60% of asymptomatic carotid stenosis were indicated for surgical treatment, which in turn were divided into two groups, one for surgical treatment and the other for drug therapy. Length of follow-up was 5 years. The results undoubtedly went in favor of surgical treatment of carotid stenosis because the rate of complications in terms of ICV and death in the surgical group was 4.1%, while in the group that was treated with medications, the complication rate was 11%, which represents the frequency of complications over 100% relative to the surgical group (9).
Our results show that among the patients from the coronary group, those with moderate stenosis were 41%, with severe stenosis 23%, and those with critical stenosis 16.1%, where as in the group of non coronary patients with moderate stenosis were 22.7%, with severe stenosis 20.5%, and those with critical stenosis 6.8%. Most of them were critical stenosis in patients of middle age, while the representation of female was slightly ahead of the male population, 22% vs.17%, but not statistically significant differences. These correspond to the results of our study Cirilo et al. as well as in studies Rath et al. (10, 11).
Our results show that the degree of ACE stenosis in both groups was not significant, and the highest percentage of patients - coronary 91.1% vs. non coronary 86.4% had a normal finding.
In a study by Yasaka et al., it was found that in the Japanese population smoking, hypertension, low levels of high density lipoproteins, diabetes mellitus and hypercholesterolemia are associated with atherosclerosis of the extracranial part of carotid arteries (12).
Smoking, as a risk factor, in our study did not differ than in studies mentioned before, and there are no significant differences between the two observed groups.
As for hypertension, we found that it is significantly higher in the patients with coronary heart disease (83.7%) compared with patients from non coronary group (16.3%). Sandler et al.in their large study demonstrated that daily variability and instability of systolic pressure are a most important predictor of early atherosclerosis on the location of common carotid artery bifurcation (13).
Diabetes has a negative impact on bran circulation, as well as on circulation of coronary and peripheral arteries. Diabetic patients frequently suffer from arteriosclerotic changes in extracranial arteries in the neck (14). In patients who underwent ultrasound examination, diabetic patients had five times the present calcified plaques than patients without diabetes (15). The presence of diabetes in patients with a stroke is 3 times higher than in other patients (16), which is the risk of getting a stroke increased by 150% to 400% compared to patients without diabetes (17, 18, 19).
Over production of triglyceride-rich lipoproteins and reduced clearance by lipoprotein lipase leads to hypertriglyceridemia, which is very common in diabetes (20).
Interestingly, the low levels of HDL-and one of the characteristics for abnormalities in type 2 diabetes. Diabetic patients with CAD often have a combination of elevated triglycerides and low level of HDL than high-level of total LDL cholesterol (21).
Our results show that there is undoubtedly significant correlation with association of 3 risk factors in both groups, hypertension, diabetes and dyslipidemia.
6. CONCLUSION
Based on the results of our work can be said that carotid disease is closely associated with coronary heart disease, so the early selection of patients with carotid artery stenosis, carotid endarterectomy treatment and modification of cardiovascular risk factors, is essential in primary and secondary prevention of a stroke.
Asymptomatic carotid critical stenosis is present in a higher percentage in coronary patients.
Evident is the presence of risk factors, but the greatest significance for coronary and carotid disease is complex of the three risk factors - high blood pressure, diabetes and dyslipidemia.
The constant control of smoking, hypertension, hyperlipidemia and use of antiplatelet therapy was shown to reduce the risk of the stroke in patients with carotid artery disease. Particular attention should be paid to screening of non coronary patients if some of the risk factors persist, especially if there are combined at least 3 of the above mentioned risk factors. The focus should be on changing life style, but it is very important to treat hypertension, increased lipids and diabetes in the prevention of carotid disease. The introduction of preoperative carotid arteries Colour Doppler in patients scheduled for operative treatment is imperative.
Footnotes
• Conflict of interest: none declared.
REFERENCES
- 1.Masic I, Rahimic M, Dilic M. Socio-medical Characteristic of coronary disease in Bosnia and Herzegovina and the world. Mater Sociomed. 2011;23(3):171–83. doi: 10.5455/msm.2011.23.171-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yasaka M, Yamaguchi T, Shichiri M. Distribution of atherosclerosis and risk factors in atherothrombotic occlusion. Stroke. 1993;24:206. doi: 10.1161/01.str.24.2.206. [DOI] [PubMed] [Google Scholar]
- 3.Masic I, Alajbegovic J. The Significance of the Psychosocial Factors Influence in Pathogenesis of Cardiovaskular Disease. Int J Prev Med. 2013 Nov;4(11):1323–30. [PMC free article] [PubMed] [Google Scholar]
- 4.Martin MJ, Whisnant JP, Sayre GP. Occlusive vascular disease in the extracranial cerebral circulation. Arch Neurol. 1960;3:530–5. doi: 10.1001/archneur.1960.00450050050006. [DOI] [PubMed] [Google Scholar]
- 5.The North American Symptomatic Carotid Endarterectomy Trial. Surgical results in 1415 patients. Stroke. 1999;30:1751–8. doi: 10.1161/01.str.30.9.1751. [DOI] [PubMed] [Google Scholar]
- 6.Harold L, Lazar J, Menzoian O, et al. Coronary Artery Bypass Grafting in Patients With Cerebrovascular Disease. Ann Thorac Surg. 1998;66:968–74. doi: 10.1016/s0003-4975(98)00687-0. [DOI] [PubMed] [Google Scholar]
- 7.Murphy MO, Ghosh J, Omorphos S, Dunning J. In patients undergoing cardiac surgery does asymptomatic significant carotid artery stenosis warrant carotid endarterectomy? Interactive CardioVasc Thorac Surg. 2005;4:344–9. doi: 10.1510/icvts.2005.108878. [DOI] [PubMed] [Google Scholar]
- 8.Westaby S. Coronary revascularisation in ischemic cardiomyopathy. Surg Clin North Am. 2004;84:179–99. doi: 10.1016/S0039-6109(03)00207-X. [DOI] [PubMed] [Google Scholar]
- 9.de Weerd M, Greving JP, de Jong AW, Buskens E, Bots ML. Prevalence of asymptomatic carotid artery stenosis according to age and sex: systematic review and metaregression analysis. Stroke. 2009;40:1105–13. doi: 10.1161/STROKEAHA.108.532218. [DOI] [PubMed] [Google Scholar]
- 10.North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade stenoses. N Engl J Med. 1991;325:445–53. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 11.Cirilo F, Renzulli A, Leonardo G, Romano G, de Feo M, Corte AD, et al. Incidence of Carotid Lesions in Patients Undergoing Coronary Artery Bypass Graft. Heart Views. 2000;1:402–7. [Google Scholar]
- 12.Filsoufi F, Rahmanian PB, Castillo JG, et al. Incidence, topography, predictors and long-term survival after stroke in patients undergoing coronary artery bypass grafting. Ann Thorac Surg. 2008;85:862–70. doi: 10.1016/j.athoracsur.2007.10.060. [DOI] [PubMed] [Google Scholar]
- 13.Janne S, Tolstrup, Ulla A. Hvidtfeldt, Esben Meulengracht Flachs, Donna Spiegelman. Smoking and Risk of Coronary Heart Disease in Younger, Middle-Aged, and Older Adults. American Journal of Public Health. 2012:e1–e7. doi: 10.2105/AJPH.2012.301091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sander D, Kukla C, Klingelhöfer J, Winbeck K, Conrad B. Relationship Between Circadian Blood Pressure Patterns and Progression of Early Carotid Atherosclerosis. Circulation. 2000;102:1536–41. doi: 10.1161/01.cir.102.13.1536. [DOI] [PubMed] [Google Scholar]
- 15.Fabris F, Zanocchi M, Bo M, et al. Carotid plaque, aging, and risk factors. Stroke. 1994;25:1133–40. doi: 10.1161/01.str.25.6.1133. [DOI] [PubMed] [Google Scholar]
- 16.Friedlander AH, Maeder LA. The prevalence of calcified carotid artery atheromas on the panoramic radiographs of patients with type 2 diabetes mellitus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:420–4. doi: 10.1016/s1079-2104(00)70122-3. [DOI] [PubMed] [Google Scholar]
- 17.Himmelmann A, Hansson L, Svensson A, et al. Predictors of stroke in the elderly. Acta Med Scand. 1988;224:439–43. doi: 10.1111/j.0954-6820.1988.tb19608.x. [DOI] [PubMed] [Google Scholar]
- 18.Jamrozik K, Broadhurst RJ, Forbes S, et al. Predictors of death and vascular events in the elderly. Stroke. 2000;31:863–8. doi: 10.1161/01.str.31.4.863. [DOI] [PubMed] [Google Scholar]
- 19.Folsom AR, Rasmussen ML, Chambless LE, et al. Prospective associations of fasting insulin, body fat distribution, and diabetes with risk of ischemic stroke. Diabetes Care. 1999;22:1077–83. doi: 10.2337/diacare.22.7.1077. [DOI] [PubMed] [Google Scholar]
- 20.Hankey GJ, Jamrozik K, Broadhurst RJ, et al. Longterm risk of first recurrent stroke in the Perth Community Stroke Study. Stroke. 1998;29:2491–2500. doi: 10.1161/01.str.29.12.2491. [DOI] [PubMed] [Google Scholar]
- 21.Sniderman AD, Scantlebury T, Cianflone K. Hypertriglyceridemic hyperapob: the unappreciated atherogenic dyslipoproteinemia in type 2 diabetes mellitus. Ann Intern Med. 2001;135:447–59. doi: 10.7326/0003-4819-135-6-200109180-00014. [DOI] [PubMed] [Google Scholar]


