Abstract
Background
Although nutritional status is influenced by multi-dimensional aspects encompassing physical and emotional well-being, there is limited research on this complex relationship.
Objective
The purpose of this study was to examine the interplay between indicators of physical health (perceived health status and self-care capacity) and emotional well-being (depressive affect and loneliness) on rural older adults’ nutritional status.
Design
The cross-sectional study was conducted from June 1, 2007 to June 1, 2008.
Participants/setting
A total of 171 community-dwelling older adults, 65 years and older, who resided within non-metro rural communities in the U.S. participated in this study.
Main outcome measures
Participants completed validated instruments measuring self-care capacity, perceived health status, loneliness, depressive affect, and nutritional status.
Statistical analyses performed
Structural equation modeling (SEM) was employed to investigate the complex interplay of physical and emotional health status with nutritional status among rural older adults, Chi-square statistic, CFI, RMSEA and SRMR were used to assess model fit.
Results
Chi-square statistic and the other model fit indices showed the hypothesized SEM model provided a good fit to the data (χ2 (2)=2.15, p=0.34; CFI=1.00; RMSEA=0.02; SRMR=0.03). Self-care capacity was significantly related with depressive affect (γ = −0.11, p=0.03) whereas self-care capacity was not significantly related with loneliness. Perceived health status had a significant negative relationship with both loneliness (γ = −0.16, p=0.03) and depressive affect (γ = −0.22, p=0.03). Although loneliness showed no significant direct relationship with nutritional status, it showed a significant direct relationship with depressive affect (β = 0.46, p<0.01). Finally, the results demonstrated that depressive affect had a significant negative relationship with nutritional status (β = −0.30, p<0.01). The results indicated physical health and emotional indicators have significant multi-dimensional associations with nutritional status among rural older adults.
Conclusions
The present study provides insights into the importance of addressing both physical and emotional well-being together to reduce potential effects of poor emotional well-being on nutritional status, particularly among rural older adults with impaired physical health and self-care capacity.
Keywords: Rural older adults, depressive affect, loneliness, perceived health status, self-care capacity, nutritional status
INTRODUCTION
Maintaining good nutritional status is essential for healthy aging in rural America. Health promotion programming is one implementation practitioners can use to identify and monitor the health needs of rural older adults.1 Previous research suggests that poor nutritional status among older adults is associated with decreased immune function, greater healthcare expenditure, and longer hospital stays.2 Thus, it is vital to understand risk factors that may place older adults at greater risk of poor nutritional status.
The association between emotional well-being and nutritional status has been well documented.3,4 Particularly, depression and feelings of loneliness have been identified as key risk factors for malnutrition among older adults.3,5,6 Older adults suffering from depressive symptoms tend to lose their appetite, refuse to eat, and experience weight loss.7,8 Depressive symptoms are also associated with unhealthy food choices such as increased intake of foods high in added sugars and lower intake of fruits or vegetables.9,10 In addition, loneliness can affect older adults’ appetites, resulting in consumption of fewer regular meals, more frequent use of convenience foods, and decreased amount and variety of foods eaten.3,11,12
Poor emotional well-being among older adults is hypothesized to be a behavioral response to aging-related impairments that compromise physical health and impair self-care capacity.13,14 Cohen-Mansfield and Parpura-Gill proposed a theoretical framework “Model of Depression and Loneliness” (MODEL) based on the Cognitive-Behavioral Theory to explain the interaction between physical health status and emotional well-being.14 In this theory, poor self-care capacity is strongly associated with feelings of loneliness among older adults.14 Furthermore, poor self-care capacity can lead to restricted social activities, which can contribute to depressive symptoms among older adults.15 In addition, Savikko, et al.16 reported poor health status was a potential contributor to feelings of loneliness. Previous studies also have found a negative association between low perceived health status and depressive symptoms in community-dwelling older adults.13,17 Empirical evidence suggests feelings of loneliness are also a strong predictor of depressive symptoms among socially isolated older adults.18,19 Thus, the relationship between physical health and emotional well-being is complex and multifactorial.
Not only is poor physical health associated with diminished emotional well-being, it is also related to poor nutritional status among older adults.20 Donini and colleagues17 reported that older adults with impaired self-care capacity to grocery shop and prepare meals were at a greater risk of malnutrition. Thus, a vicious cycle can be generated where progressive functional decline, poor nutritional status, and emotional decline exacerbate each other.
Unfortunately, older adults residing in rural areas generally have fewer opportunities for social interaction. This is commonly due to geographic isolation and out-migration of younger adults who serve as supportive resources.21 Due to this limited social engagement, older adults living in rural areas are more likely to experience feelings of loneliness and depressive symptoms.22 Studies have reported older adults residing in rural areas have higher rates of depressive symptoms than those living in urban areas.23,24 In addition, rural older adults have been reported to face a greater number of chronic conditions and impaired self-care capacity than older adults residing in urban areas.25
Although nutritional status is influenced by multi-dimensional aspects encompassing physical and emotional well-being, there is limited research on this complex relationship.26 Identifying the interplay of these factors on rural older adults’ nutritional status can serve as a basis for development of nutrition education programs to improve nutritional status.
Cohen-Mansfield and Parpura-Gill 14 developed the theoretical model to examine predictors of loneliness among low-income older adults including physical health and emotional well-being variables. Therefore, this study extended upon the MODEL to further inform the associations among physical health (perceived health status and self-care capacity), and emotional well-being (depressive affect and loneliness), along with the addition of nutritional status among rural older adults.
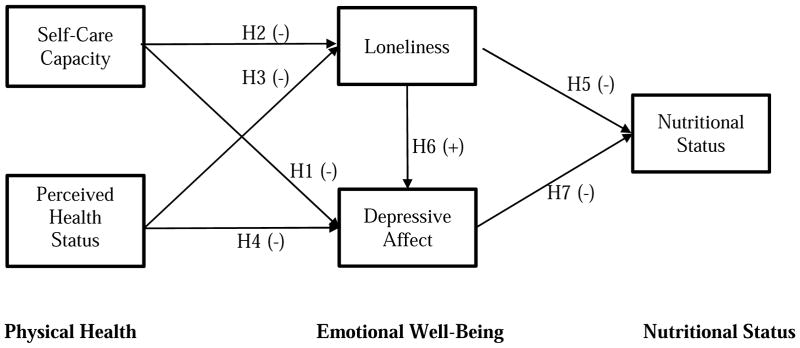
The following hypotheses and expected outcomes of the investigation included (Figure 1):
Figure 1.
Proposed Structural Equation Modeling model for the relationship of physical health, emotional well-being, and nutritional status.
H1: Lower self-care capacity will have a direct negative relationship with depressive affect.
H2: Lower self-care capacity will have a direct negative relationship with loneliness.
H3: Lower perceived health status will have a direct negative relationship with loneliness.
H4: Lower perceived health status will have a direct negative relationship with depressive affect.
H5: Higher loneliness will have a direct negative relationship with nutritional status.
H6: Higher loneliness will have a direct positive relationship with depressive affect.
H7: Higher depressive affect will have a direct negative relationship with nutritional status.
-
H1
Lower self-care capacity will have a direct negative relationship with depressive affect.
-
H2
Lower self-care capacity will have a direct negative relationship with loneliness.
-
H3
Lower perceived health status will have a direct negative relationship with loneliness.
-
H4
Lower perceived health status will have a direct negative relationship with depressive affect.
-
H5
Higher loneliness will have a direct negative relationship with nutritional status.
-
H6
Higher loneliness will have a direct positive relationship with depressive affect.
-
H7
Higher depressive affect will have a direct negative relationship with nutritional status.
METHODS
Study Setting and Subjects
The U.S. Office of Management and Budget Metropolitan Statistical Areas (OMBMS) definition and the U.S. census definition of rural were used to target rural community-dwelling older adults.27 Community-dwelling older adults, 65 years and older, who resided within non-metro rural communities located in Northwest Oklahoma with populations of 2,500 or less were solicited to participate in this cross-sectional study. All participants were solicited and recruited through the Oklahoma aging service network including senior nutrition and activity sites, Oklahoma Aging Division, Area Agencies on Aging, and Oklahoma State University Cooperative Extension Service County Educators. Survey procedures were conducted at senior nutrition and activity sites as well as County Cooperative Extension Service office sites from June 2007 to June 2008.
In order to identify individuals who required assistance in reading, writing, and comprehension, cognitive status of all interested participants was screened using the Short-Portable Mini-Mental Status Questionnaire (SPMSQ), a brief 10-item instrument used to examine short and long term recall of information. 28 Based on SPMSQ recommendations, participants scoring ≥ 4 were excluded from the study due to a score indicative of mild to moderate dementia.28 After excluding two individuals based on the SPMSQ cut-off score, a total of 171 participants were included in analyses. Participation in this study involved completion of a self-report survey.
The study protocol was approved by the Oklahoma State University Institutional Review Board (IRB) for Human Subjects. All participants were asked to read and sign an informed consent form. For those who needed assistance, a trained member of the research team conducted a private one-to-one reading and explanation of the informed consent.
Measures
Socio-demographic information
Socio-demographic information was collected from participants including age, gender, race/ethnicity, marital status, education, and annual income.
Perceived Health Status
The 4-item Subjective Health Perceptions Scale from the Duke Older Americans Resources and Services Procedures (OARS) was used to assess perceived health status.29 Item scores were summed to create a perceived health status score. Perceived health status scores range from 4 to 14. A higher score represents higher perceived health, whereas a lower score indicates lower perceived health. Cronbach’s alpha reliability for this measure in the current study was satisfactory at α = 0.76.
Self-Care Capacity
The 13-item Self-Care Capacity Scale from the OARS was used to assess ability to perform activities of daily living (bathing, dressing, eating, getting in or out of bed or a chair, walking, and toileting) and instrumental activities of daily living (shopping, cooking, and cleaning). Item scores are summed to derive a self-care capacity score. Self-care capacity scores range from 13 to 39. A higher score reflects higher self-care capacity, whereas a lower score indicates lower self-care capacity. The OARS Self-Care Capacity Scale items have evinced high reliability (r = 0.84).29 Cronbach’s alpha reliability in the present study emerged as moderate at α = 0.57.
Loneliness
The 10-item University of California, Los Angeles Loneliness Scale-Version was used to assess feeling of loneliness.30 Item scores are used to create a loneliness score. Loneliness scores range from 10 to 29. A lower score reflects low feelings of loneliness, whereas a higher score indicates higher feelings of loneliness. Cronbach’s alpha reliability for the loneliness scale in the present study was 0.75.
Depressive Affect
The 10-item Geriatric Depression Scale was used to measure depressive affect.31 Item scores were summed to derive a Geriatric Depression Scale score. Geriatric depression scale scores range from 0 to 10 with a higher score indicating a higher depressive affect and a lower score indicating lower depressive affect. Cronbach’s alpha reliability for the geriatric depression scale in the present study was 0.77.
Nutritional Status
Nutritional status was measured using the Mini-Nutritional Assessment Short-Form (MNA-SF), which is a validated assessment tool used to identify risk of malnutrition among older adults in clinics, hospitals, and nursing homes.32 The MNA-SF includes measurements on height, weight, appetite, weight loss, mobility, acute psychological stress, and neuropsychological problems.32 BMI, appetite, weight loss, mobility, psychological stress, and neuropsychological problems scores were summed to derive a nutritional status score. Nutritional status scores range from 0 to 14. A higher score indicates higher nutritional status, whereas a lower score indicates lower nutritional status.
Statistical Analysis
Descriptive statistics and correlation analysis have been conducted prior to the primary data analysis. Response rate for each measure was also assessed. Structural equation modeling (SEM) using Mplus 7.133 was employed to investigate the complex interplay of physical and emotional indicators with nutritional status among rural older adults. Figure 1 presents the theoretical SEM model used to examine the research questions. To assess whether the theoretical model fit the data, various fit indices associated with SEM techniques were examined: χ2 goodness-of-fit test, comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). General fit indices cutoff values indicating acceptable fit are CFI ≥ 0.90, RMSEA<0.08, and SRMR ≤ 0.08.34,35,36 Descriptive statistics and correlation analyses were conducted using IBM SPSS Statistics for windows, Version 22.0.37 Given that all hypotheses were directional, one-tailed p-values (p <0.05, p<0.01) were reported for the parameter estimates in the SEM model.
RESULTS
Table 1 includes descriptive statistics for participant socio-demographic characteristics. A total of 171 rural older adults (age ranged 65 -101 years) participated in the study with an average age of 77.5. The majority of participants were female (70.2%) and white (98.8%). Close to half of the participants were married (49.7%) and had at least a high school degree (43.5%). Forty-five percent of participants reported annual incomes less than $20,000, and 55% reported annual incomes greater than or equal to $20,000.
Table 1.
Socio-demographic characteristics of older adults residing in rural Oklahoma.
| Variable | Frequency (n=171) | Percentage (%) | Mean ± SD1 |
|---|---|---|---|
| Age (years) | 77.5 ± 8.2 | ||
| Gender | |||
| Male | 51 | 29.8 | |
| Female | 120 | 70.2 | |
| Race/Ethnicity | |||
| White | 169 | 98.8 | |
| Hispanic/Latino | 1 | 0.6 | |
| Asian | 1 | 0.6 | |
| Marital Status | |||
| Never Married | 3 | 1.8 | |
| Married | 83 | 49.7 | |
| Widowed | 70 | 41.9 | |
| Divorced | 9 | 5.4 | |
| Separated | 2 | 1.2 | |
| Education | |||
| Grade School/Junior High | 9 | 5.3 | |
| Some High School | 20 | 11.8 | |
| High School/Vocational | 74 | 43.5 | |
| Some College | 31 | 18.2 | |
| College | 12 | 7.1 | |
| Some Post-Graduate | 17 | 10.0 | |
| Masters’ Degree/PhD | 7 | 4.1 | |
| Annual Income | |||
| Below $10,000 | 23 | 16.4 | |
| $10,000–$19,999 | 40 | 28.6 | |
| $20,000–$29,999 | 24 | 17.1 | |
| $30,000–$39,999 | 18 | 12.9 | |
| $40,000 and higher | 35 | 25.0 | |
Standard deviation.
Table 2 presents descriptive statistics (i.e., mean, standard deviation, and range) for the variables used in the SEM model to examine the research hypotheses. Given that one of the important assumptions for using SEM analysis is the normality of the employed data, basic descriptive analyses were conducted to check skewness and kurtosis of the outcome variables used in the SEM model. The results showed that all three dependent variables included in the SEM model were adequately normally distributed (skewness<3; kurtosis<7) 38 with no severe violation of normality. Zero-order correlation coefficients for the variables are also presented in Table 2. As shown in the Table 2, there was a significant positive correlation between self-care capacity and perceived health status (Pearson r= 0.31). While there was a significant positive correlation between depressive affect and loneliness (r=0.42), depressive affect was negatively correlated with perceived health status (r=−0.31) and nutritional status (r=−0.27). More nuanced and complex relationships were examined using SEM model. Participants’ response rates were relatively high, with a small missing data rate ranging from 1.1 to 8.1% across all measures used in the SEM model. Given that no systematic missing data pattern was found, missing at random was assumed for further analyses. Full information maximum likelihood robust estimation method (estimator=MLR) in Mplus was used to obtain the parameter estimates by handling missing data in any outcome variables and adjusting the standard errors given non-normality. A total of 168 participants after removing three cases, who had missing data on predictor variables, were included for further analysis by default for using ESTIMATOR=MLR in Mplus 7.1.
Table 2.
Descriptive statistics and correlations among self-care capacity, perceived health, loneliness, depressive affect and nutritional status in Structural Equation Modeling model among older adults residing in rural Oklahoma.
| Perceived Health Status c | Self-Care Capacity d | Loneliness e | Depressive Affect f | Nutritional Status g | |
|---|---|---|---|---|---|
| Correlation | |||||
| Self-Care Capacity | 0.31a | - | - | - | - |
| Loneliness | −0.13 | 0.05 | - | - | - |
| Depressive Affect | −0.31a | −0.14 | 0.42a | - | - |
| Nutritional Status | 0.15 | 0.13 | −0.07 | −0.27a | - |
| Mean | 9.75 | 38.38 | 18.09 | 1.36 | 12.09 |
| SDb | 2.11 | 1.15 | 4.23 | 1.93 | 1.48 |
| Minimum | 4.00 | 33.00 | 10.00 | 0.00 | 8.00 |
| Maximum | 14.00 | 39.00 | 29.00 | 9.00 | 14.00 |
| Skewness | - | - | 0.17 | 1.83 | −0.72 |
| Kurtosis | - | - | −0.58 | 3.41 | −0.07 |
Significant at p<0.01
Standard deviation.
Perceived health status was measured using the Subjective Health Perceptions Scale.29 Perceived health status scores range from 4 to 14. A higher score represents higher perceived health.
Self-Care Capacity was measured using the Self-Care Capacity Scale.29 Self-care capacity scores range from 13 to 39. A higher score reflects higher self-care capacity.
Loneliness was measured using the Loneliness Scale-Version.30 Loneliness scores range from 10 to 29. A higher score indicates higher feelings of loneliness.
Depressive Affect was measured using the Geriatric Depression Scale.31 Depression scores range from 0 to 10 with a higher score indicating a higher depressive affect.
Nutritional Status was measured using the Mini-Nutritional Assessment Short-Form.32 Nutritional Status scores range from 0 to 14. A higher score indicates high nutritional status.
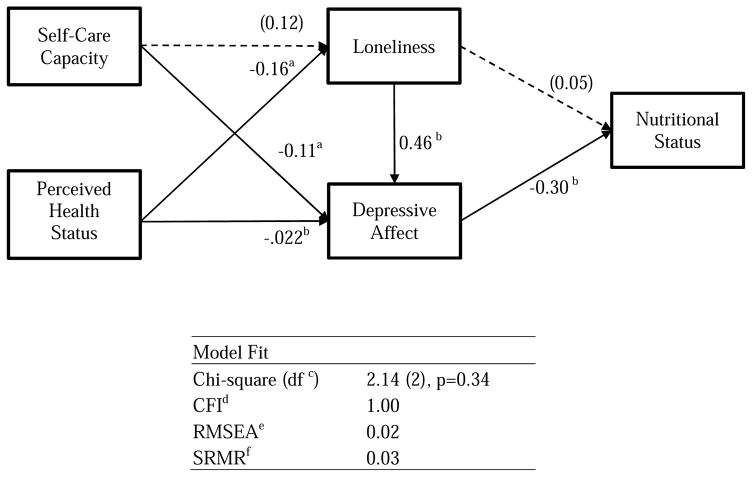
Figure 2 presents the SEM results for the standardized parameter estimates with the model fit indices. All of the model fit indices supported the hypothesized model to fit the data. Chi-square statistic was not significant (χ2 (2)=2.15, p=0.34), indicating a good fit of the hypothesized model to the data, and other model fit indices exhibited good fit as well (i.e., CFI=1.00, RMSEA=0.02, and SRMR=0.03). Given the model fit was good, the parameter estimates for each hypothesis were interpreted. As shown in Figure 2, self-care capacity was significantly related with depressive affect (γ = −0.11, p=0.03), meaning that participants were more depressed as self-care capacity was more limited (H1), whereas self-care capacity was not significantly related with loneliness (H2). As hypothesized, perceived health status had a significant negative relationship with both loneliness (γ = −0.16, p=0.03; H3) and depressive affect (γ = −0.22, p=0.03; H4), indicating that lower perceived health status related to higher loneliness and depressive affect. Although loneliness showed no significant direct relationship with nutritional status (H5), it showed a significant direct relationship with depressive affect (β = 0.46, p<0.01; H6), indicating participants who were lonelier were more depressed. Finally, the results demonstrated that depressive affect had a significant negative relationship with nutritional status (β = −0.30, p<0.01; H7), meaning that participants who were more depressed were more likely to have poor nutritional status. This finding further supports the growing body of evidence linking poor nutritional status with an increased risk of depressive symptoms.6,26 Table 3 provides more detailed information on the estimated parameters, corresponding standard errors, and one-tailed p-values.
Figure 2.
Structural Equation Modeling results with standardized parameter estimates and model fit indices
aSignificant at p<0.05
bSignificant at p<0.01
cdegree of freedom
dcomparative fit index
eroot mean square error of approximation
fstandardized root mean square residual
All path coefficients are standardized; numbers are standardized parameter estimates. Dotted lines represent p> 0.05 or p> 0.01 and solid lines represent p< 0.05 or p< 0.01
Table 3.
Summary of parameter estimates for the relationship of physical health, emotional well-being, and nutritional status among older adults residing in rural Oklahoma.
| Path | Parameter Estimate | S.E. | One-tailed p-value |
|---|---|---|---|
| H1: Self-Care Capacity → Depressive Affect | −0.11 | 0.06 | 0.033 |
| H2: Self-Care Capacity → Loneliness | 0.12 | 0.08 | 0.063 |
| H3: Perceived Health Status → Loneliness | 0.16 | 0.08 | 0.027 |
| H4: Perceived Health Status → Depressive Affect | −0.22 | 0.07 | 0.002 |
| H5: Loneliness → Nutritional Status | 0.05 | 0.10 | 0.302 |
| H6: Loneliness → Depression | 0.46 | 0.07 | 0.001 |
| H7: Depression → Nutritional Status | −0.30 | 0.10 | 0.001 |
DISCUSSION
The specific aim of this study was to examine the interplay between indicators of physical health (perceived health status and self-care capacity) and emotional well-being (depressive affect and loneliness) with rural older adults’ nutritional status. In order to gain a holistic understanding of these complex relationships, the present study adopted the MODEL as a fundamental framework.
The present study hypothesized that poor physical health status (impaired self-care capacity, low perceived health status) would have a direct negative relationship with emotional well-being (loneliness, depressive affect). Although the hypothesis related to loneliness was not supported in the present study, rural older adults with impaired self-care capacity had higher depressive affect. Similarly, previous studies have reported that older adults who experience difficulties in performing daily activities were at increased risk of depression.39,40 This finding suggests impaired self-care capacity may affect older adults’ ability to participate in social activities with others, which may lead to social isolation. In turn, inability to maintain daily activities due to impaired self-care capacity can increase the risk of depression.13,18,41
Findings from this study also indicated rural older adults with lower perceived health status experienced greater feelings of loneliness and depressive affect. A negative association between perceived health status, loneliness, and depressive affect has been frequently reported from previous studies.13,16,17 Meta analyses including quantitative as well as qualitative studies have also shown poor self-perceived health is a strong risk factor for depression among older adults.42 In addition, the present study hypothesized that loneliness would have a direct positive relationship with depressive affect. Results from this study extended the previous findings by confirming that loneliness was also a strong predictor of depressive affect among rural older adults.18,19,43 This finding suggests that feeling lonely might potentially be a risk indicator of a depressed mood state.
The present study hypothesized that poor emotional well-being would negatively influence nutritional status. While loneliness did not directly influence nutritional risk, depressive affect did have a direct negative relationship with nutritional status. This finding is consistent with those of recent studies conducted with both hospitalized and community-dwelling older adults.6,44 Although depression has been shown to be a major predictor of nutritional status in older adults, the mechanism of this negative relationship between depression and nutritional status has not been fully investigated.44,45 However, one proposed hypothesis explains that depression may influence motivation to eat less and lose appetite.46 As a consequence of reduced food intake, older adults may experience weight loss, which in turn may lead to a higher incidence of nutritional risk. Conversely, poor nutrition itself has been proposed as a predictor of depression as a result of lack of nutrients such as folate, vitamin B 12 that are required for neurotransmitter changes,14, 47 suggesting that the association between depression and nutritional risk may be bidirectional.
While many previous studies examined the nutritional risk factors associated with emotional well-being and physical health, there is limited research exploring the complex interplay between indicators of physical health and emotional well-being on rural older adults’ nutritional status. The present study may be the first to investigate both physical and emotional well-being as risk factors on nutritional status. The results from the present study revealed that nutritional status is directly influenced by emotional well-being and this emotional well-being is also strongly associated with physical health status. Unfortunately, rural older adults have been reported to experience higher levels of loneliness, depressive symptoms, and poorer health status compared to urban older adults.22,48 Thus, the combined experience of poor emotional well-being and impaired physical health status put rural older adults at greater risk of malnutrition.
Several studies have reported that providing social support has a protective effect against impaired physical health in old age. Social support is also believed to act as a buffer against the negative consequences of depressive symptoms on impaired self-care capacity.49 In fact, previous studies reported socialization opportunities provided by the Older American Act Nutrition Program (OAANP) helped alleviate older adults’ depressive symptoms, feelings of loneliness, as well as increases their perception of health and appetite due to having others to eat within a social atmosphere.50
Thus, findings from the present study imply that providing health promotion programs for rural older adults including efforts to promote emotional well-being as well as to provide social support, particularly for those with limited self-care capacity, could improve nutritional status. One venue to provide health promotion programs for rural older adults is the OAANP, which provides not only nutritious meals but also offers many opportunities for older adults to socialize. Including both physical and emotional well-being components into senior nutrition programs could possibly decrease the risk of malnutrition, prevent physical and emotional decline, and ultimately assist rural older adults in maintaining their health and ability to live independently in their communities.
Although results from the present study provide insights into the importance of both physical and emotional well-being on nutritional status, it has several limitations. First, selection bias might have affected the results of the present study. Study participants were selected using convenience sampling, which may have resulted in homogenous participant pool. Furthermore, convenience sampling may have introduced a selection effect whereby participants may represent older adults who are in better emotional and physical health than the general population. For future studies, using randomized sampling would result in greater heterogeneity. Second, although there is the growing body of evidence that the association between poor nutrition and an increased risk of depressive symptoms is bidirectional, the present study used a cross-sectional methodology. Therefore, it is not appropriate for exploring causal relationships between the variables. Third, the study used a geographically limited sample recruited from Northwest Oklahoma. Therefore, findings from the present study cannot be generalized to rural older adults elsewhere.
CONCLUSIONS
With the rapidly increasing older adult population, health promotion programs aimed at improving nutritional status can play an important role in successful aging. Older adults residing in rural areas are at increased risk of poor nutritional status, which is influenced by multi-dimensional aspects encompassing physical and emotional well-being. Identifying factors influencing nutritional status is critical when health care professionals plan programs to assist older adults in achieving and maintaining optimal nutritional status. Our findings suggest that physical and emotional well-being should be addressed together. This is particularly important for rural older adults with impaired physical health and self-care capacity, in order to reduce potential effects of poor emotional well-being on nutritional status.
Acknowledgments
Funding/Support Disclosure
Funding for the present research was provided by the Donna Cadwalader Research and Development Grant. Research reported in this publication is supported in part by the National Institute on Aging (K01AG045342).
Footnotes
Conflict of Interest
No authors report a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ortman JM, Velkoff VA, Hogan H. Population estimates and projections. U.S department of Commerce; Economics and Statistics and Administration: U.S. Census Bureau; 2014. An aging nation: The older population in the United States; pp. 25–1140. [Google Scholar]
- 2.Brownie S. Why are elderly individuals at risk of nutritional deficiency? Int J Nurs Pract. 2006;12:110–118. doi: 10.1111/j.1440-172X.2006.00557.x. [DOI] [PubMed] [Google Scholar]
- 3.Eskelinen K, Hartikainen S, Nykanen I. Is loneliness associated with malnutrition in older people? Int J of Gerontol. 2016;10(1):43–45. [Google Scholar]
- 4.Fratiglioni L, Wang HX, Ericsson K, Maytan M, Winblad B. Influence of social network on occurrence of dementia: A community-based longitudinal study. The Lancet. 2000;355(9212):1315–1319. doi: 10.1016/S0140-6736(00)02113-9. [DOI] [PubMed] [Google Scholar]
- 5.Walker D, Beauchene RE. The relationship of loneliness, social isolation, and physical health to dietary adequacy of independently living elderly. J Am Diet Assoc. 1991;91(3):300–304. [PubMed] [Google Scholar]
- 6.German L, Feldblum I, Bilenko N, Castel H, Harman-Boehm I, Shahar DR. Depressive symptoms and risk for malnutrition among hospitalized elderly people. J Nut Health Aging. 2008;12(5):313–318. doi: 10.1007/BF02982661. [DOI] [PubMed] [Google Scholar]
- 7.Donini LM, Savina C, Cannella C. Eating habits and appetite control in the elderly: The anorexia of aging. Int Psychogeriatr. 2003;15:73–87. doi: 10.1017/s1041610203008779. [DOI] [PubMed] [Google Scholar]
- 8.Marcus EL, Berry EM. Refusal to eat in the elderly. Nutr Rev. 1998;56:163–171. doi: 10.1111/j.1753-4887.1998.tb06130.x. [DOI] [PubMed] [Google Scholar]
- 9.Jeffery RW, Linde JA, Simon GE, et al. Reported food choices in older women in relation to body mass index and depressive symptoms. Appetite. 2009;52:238–240. doi: 10.1016/j.appet.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Konttinen H, Mannisto S, Sarlio-Lahteenkorva S, Silventoinen K, Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption: A population-based study. Appetite. 2010;54:473–479. doi: 10.1016/j.appet.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Frongillo EA, Rauschenbach BS, Roe DA, Williamson DF. Characteristics related to elderly persons’ not eating for 1 or more days: Implications for meal programs. Am J Public Health. 1992;82(4):600–602. doi: 10.2105/ajph.82.4.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen CCH, Schilling LS, Lyder CH. A concept analysis of malnutrition in the elderly. J Adv Nurs. 2001;36(1):131–142. doi: 10.1046/j.1365-2648.2001.01950.x. [DOI] [PubMed] [Google Scholar]
- 13.Alpass FM, Neville S. Loneliness, health and depression in older males. Aging Ment Health. 2003;7(3):212–216. doi: 10.1080/1360786031000101193. [DOI] [PubMed] [Google Scholar]
- 14.Cohen-Mansfield J, Parpura-Gill A. Loneliness in older persons: A theoretical model and empirical findings. Int Psychogeriatr. 2007;19(02):279–294. doi: 10.1017/S1041610206004200. [DOI] [PubMed] [Google Scholar]
- 15.Webber AP, Martin JL, Harker JO, Josephson KR, Rubenstein LZ, Alessi CA. Depression in older patients admitted for post acute nursing home rehabilitation. J Am Geriatr Soc. 2005;53(6):1017–1022. doi: 10.1111/j.1532-5415.2005.53322.x. [DOI] [PubMed] [Google Scholar]
- 16.Savikko N, Routasalo P, Tilvis RS, Strandberg TE, Pitkälä KH. Predictors and subjective causes of loneliness in an aged population. Arch of Gerontol Geriatr. 2005;41(3):223–233. doi: 10.1016/j.archger.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Demura S, Sato S. Relationships between depression, lifestyle and quality of life in the community dwelling elderly: A comparison between gender and age groups. J Physiol Anthropol Appl Human Sci. 2003;22(3):159–166. doi: 10.2114/jpa.22.159. [DOI] [PubMed] [Google Scholar]
- 18.Blazer DG. Depression in late life: Review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58(3):M249–M265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 19.Chapman DP, Perry GS. Depression as a major component of public health for older adults. Prev Chronic Dis. 2008;5(1):A22. [PMC free article] [PubMed] [Google Scholar]
- 20.Jurschik P, Torres J, Sola R, Nuin C, Botigue T, Lavedan A. High rates of malnutrition in older adults receiving different levels of health care in Lleida, Catalonia: An assessment of contributory factors. J Nutr Elder. 2010;29(4):410–422. doi: 10.1080/01639366.2010.521043. [DOI] [PubMed] [Google Scholar]
- 21.Locher JL, Burgio KL, Yoels WC, Ritchie CS. The social significance of food and eating in the lives of older recipients of meals on wheels. J Nutr Elder. 1997;17(2):15–33. [Google Scholar]
- 22.Marshall TA, Stumbo PJ, Warren JJ, Xie X-J. Inadequate nutrient intakes are common and are associated with low diet variety in rural, community- dwelling elderly. J Nutr. 2001;131(8):2192–2196. doi: 10.1093/jn/131.8.2192. [DOI] [PubMed] [Google Scholar]
- 23.Probst JC, Laditka SB, Moore CG, Harun N, Powell MP, Baxley EG. Rural-urban differences in depression prevalence: implications for family medicine. Fam Med. 2006;38(9):653. [PubMed] [Google Scholar]
- 24.Baernholdt M, Yan G, Hinton I, Rose K, Mattos M. Quality of life in rural and urban adults 65 years and older: Findings from the National Health and Nutrition Examination Survey. J Rural Health. 2012;28(4):339–347. doi: 10.1111/j.1748-0361.2011.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson JE. Demographic characteristics of rural elderly. New York: NY Columbia University Press; 2005. [Google Scholar]
- 26.Yoshimura K, Yamada M, Kajiwara Y, Nishiguchi S, Aoyama T. Relationship between depression and risk of malnutrition among community- dwelling young-old and old-old elderly people. Aging Ment Health. 2013;17(4):456–460. doi: 10.1080/13607863.2012.743961. [DOI] [PubMed] [Google Scholar]
- 27.Wan H, Sengupta M, Velkoff VA, DeBarros KA. U.S. Census Bureau, Current population reports: 65+ in the United States. 2005. Washington, DC: U.S. Government Printing Office; 2005. [Google Scholar]
- 28.Pfeiffer EA. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:440. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 29.Fillenbaum GG. Multidimensional functional assessment of older adults: The Duke Older Americans Resources and Service Procedures. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- 30.Russell D, Peplau LA, Ferguson ML. Developing a measure of loneliness. J Per Asses. 1978;42:290–294. doi: 10.1207/s15327752jpa4203_11. [DOI] [PubMed] [Google Scholar]
- 31.Yesavage JA, Brink TL, Rose TL. Handbook of psychiatric measures. Washington DC: American Psychiatric Association; 2000. Geriatric depression scale (GDS) [Google Scholar]
- 32.Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF) J Gerontol A Biol Sci Med Sci. 2001;56(6):M366–M372. doi: 10.1093/gerona/56.6.m366. [DOI] [PubMed] [Google Scholar]
- 33.Muthén LKaM, BO . Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; 2015. [Google Scholar]
- 34.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 35.Browne MW, Cudeck R. Alternative ways of assessing model fit. Sage focus editions. 1993;154:136. [Google Scholar]
- 36.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 37.IBM Corp. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013. [Google Scholar]
- 38.Kline RB. Principles and practice of structural equation modeling. 3. New York: Guilford Press; 2010. [Google Scholar]
- 39.Anstey KJ, von Sanden C, Sargent-Cox K, Luszcz MA. Prevalence and risk factors for depression in a longitudinal, population-based study including individuals in the community and residential care. Am J Geriatr Psychiatry. 2007;15(6):497–505. doi: 10.1097/JGP.0b013e31802e21d8. [DOI] [PubMed] [Google Scholar]
- 40.Webber AP, Martin JL, Harker JO, Josephson KR, Rubenstein LZ, Alessi CA. Depression in older patients admitted for post acute nursing home rehabilitation. J Am Geriatr Soc. 2005;53:1017–1022. doi: 10.1111/j.1532-5415.2005.53322.x. [DOI] [PubMed] [Google Scholar]
- 41.Bruce ML, McAvay GJ, Raue PJ, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159(8):1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- 42.Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. Am J Psychiatry. 2003;160(6):1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- 43.Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol Aging. 2006;21(1):140. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- 44.Cabrera M, Mesas A, Garcia A, de Andrade S. Malnutrition and depression among community-dwelling elderly people. J Am Med Dir Assoc. 2007;8(9):582–584. doi: 10.1016/j.jamda.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 45.Callen BL, Wells TJ. Screening for nutritional risk in community-dwelling old-old. Public Health Nurs. 2005;22(2):138–146. doi: 10.1111/j.0737-1209.2005.220207.x. [DOI] [PubMed] [Google Scholar]
- 46.Bodnar LM, Wisner KL. Nutrition and depression: Implications for improving mental health among childbearing-aged women. Biol Psychiatry. 2005;58(9):679–685. doi: 10.1016/j.biopsych.2005.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fava M, Borus JS, Alpert JE, Nirenberg AA, Rosenbaum JF, Bottiglieri T. Folate, vitamin B12, and homocysteine in major depressive disorder. Am J Psychiatry. 1997;154:426–428. doi: 10.1176/ajp.154.3.426. [DOI] [PubMed] [Google Scholar]
- 48.Kulkowski K, Coon PJ. Comparison of nutritional risk between urban and rural elderly. Ostomy Wound Manage. 2004;50:46–58. [PubMed] [Google Scholar]
- 49.Hays JC, Saunders WB, Flint EP, Kaplan BH, Blazer DG. Social support and depression as risk factors for loss of physical function in late life. Aging Ment Health. 1997;1(3):209–220. [Google Scholar]
- 50.Wunderlich S, Bai Y, Piemonte J. Nutrition risk factors among home delivered and congregate meal participants: Need for enhancement of nutrition education and counseling among home delivered meal participants. J Nutr Health Aging. 2011;15(9):768–7. doi: 10.1007/s12603-011-0090-9. [DOI] [PubMed] [Google Scholar]