Abstract
Obesity remains a serious public health issue in adolescents, who may be subjected to weight stigma leading to increased stress and poor health outcomes. Stigma can be detrimental to adolescents during self-identity formation. The purpose of this study was to examine weight stigma in adolescents in light of the Identity Threat Model of Stigma. A cross-sectional correlational design was used to examine the relationships among the variables of weight stigma, psychosocial stress, coping styles, disordered eating, and physical inactivity. Regression modeling and path analysis were used to analyze the data. Over 90% of the sample had scores indicating weight stigma or antifat bias. Avoidant coping style and psychosocial stress predicted disordered eating. The strongest path in the model was from avoidant coping to disordered eating. The Identity Threat Model of Stigma partially explained adolescents’ weight stigma. Nursing practice implications are discussed.
Keywords: stigma, adolescents, weight status, obesity, identity
In the United States, 12.7 million youth between the ages of 2 and 19 years are obese (Centers for Disease Control and Prevention [CDC], 2014). Many of these youth may be subjected to weight stigma resulting in negative social and health outcomes. Consider the student forced to sit in a desk that is too small or an obese teen being the object of stares at a public beach. Adolescents may be particularly sensitive and vulnerable to weight stigma and its consequences, which could impede emotional and social development (Puhl & Latner, 2007). In addition to the adverse medical consequences associated with obesity itself, internalized weight stigma can result in a chronic stress response (MacLean et al., 2009) and play a role in the development of behaviors which can adversely affect health, such as unhealthy eating patterns (Puhl, Moss-Racusin, & Schwartz, 2007) and exercise avoidance (Vartanian & Novak, 2011). A paucity of research exists on weight-based stigma, particularly among adolescents; furthermore, in spite of the continued problem of youth obesity, recent research remains insufficient.
Significance and Nature of Weight Stigma
Weight stigma refers to an identity threat in response to negative weight-related biases, stereotypes, and prejudices toward an adolescent because he or she is overweight or obese; it can be subtly or openly manifested (Major & O’Brien, 2005; Puhl & Latner, 2007). Youth experience weight stigma through verbal teasing, physical and cyber bullying, and social exclusion. Sadly, the most frequent source of weight stigma is a member of the individual’s family; obese women implicated their parents when describing the worst of their prior experiences, and 69% reported being stigmatized by family members on multiple occasions (Puhl, 2009).
Although an area of concern at any age, weight stigma may be particularly damaging when experienced during childhood and adolescence, a time when social relationships are forged, and peer rejection is keenly felt (Puhl & Latner, 2007). The literature is quite sparse on the psychological and physiological effects of weight stigma (Major, Eliezer, & Rieck, 2012); yet, preliminary evidence suggests stigma exerts negative long-term effects upon youth. Secondary school–aged children who have been targeted for frequent victimization have poorer social and emotional adjustment (Nansel, Craig, Overpeck, Saluja, & Ruan, 2004).
Weight-based stigma may also be associated with weight management strategies which are ineffective or harmful, such as avoidance of physical activity, disordered eating (DE) patterns, or increased calorie consumption (Puhl et al., 2007; Schvey, Puhl, & Brownell, 2011). Studies have demonstrated an increased preference for foods high in fats and sugars in individuals reporting greater stress exposure (Morris, Beilharz, Maniam, Reichelt, & Westbrook, 2015). Chronic stress has been associated with the development of eating disorders in adolescents (Rojo, Conesa, Bermudez, & Livianos, 2006). Gluck (2006) stated that adult obese patients reported stress as a trigger in binge episodes. Fourth to sixth graders reported unhealthy eating as a coping mechanism for stress (Jenkins, Rew, & Sternglanz, 2005).
We know little about how individuals cope with the stress of obesity stigma. Suggestions for coping range from losing weight to changing public perceptions of obesity (Puhl & Brownell, 2003). In a recent literature review, it was hypothesized that the emotional coping style of confirmation may be an internalization of weight stigma in obese individuals, and may represent a “surrender” to what is viewed as an unchangeable situation (Sikorski, Luppa, Luck, & Riedel-Heller, 2015). Coping styles that are emotion- or avoidance-based have been linked with binge eating behavior, dieting, and elevated scores measuring DE patterns (Baigrie & Giraldez, 2008).
Stigma may also negatively impact other health behaviors and lead to avoidance of physical activity. Among college-aged women, stigma experiences were related to an increased desire for exercise avoidance (Vartanian & Shaprow, 2008). In children and adolescents aged 10 to 14 years, appearance-related teasing was associated with a preference for sedentary isolative type activities in overweight participants (Hayden-Wade et al., 2005).
The Identity Threat Model of Stigma (Major & O’Brien, 2005) provided the conceptual framework for this study. Adolescence was operationalized as ages 13 to 20 years and included the developmental stage of identity versus role confusion (Erikson, 1950). Briefly, in the theoretical model, the stigmatized person is the target. The effects of stigma are mediated by the target’s understanding of how he or she is viewed by others, and by his or her interpretation of the social context. A decreased or devalued social identity is conveyed to persons possessing certain features or attributes and is socially constructed within a particular context. The stigmatized person appraises situational cues that convey the risk of being devalued, as well as “collective representations (knowledge of cultural stereotypes)” (Yang et al., 2007, p. 1527), and concludes that he or she belongs to a devalued group within a particular society or context. Stigma’s effects on the social identity can be internalized, thus producing changes in the psychological realm leading to fear and stress. Appraisal of the contextual situational cues and collective representations produces fear in the target of being judged, creating a threat to identity. Responses to the threat produce involuntary emotional or physiological responses, such as stress, as well as voluntary coping efforts, such as eating and physical activity. The model theorizes that chronic repeated exposure to stigma, in tandem with ineffective coping efforts, can adversely affect outcomes in health, academic achievement, and self-esteem (Major & O’Brien, 2005). Preliminary support came from a study utilizing this framework, in which weight-related identity threat led to increased cardiovascular stress measures and negative stress-related emotions in 99 overweight women (Major et al., 2012).
Purpose
Obese children and adolescents may be subjected to stigmatization over their weight status. Relationships between weight stigma, psychosocial stress, coping styles, DE, and physical inactivity have not been previously explored. The purpose of this study was to determine the effects of weight stigma, stress, and avoidant coping mechanisms on DE and physical activity.
Method
The researchers used a cross-sectional, multivariable, correlational design, and invited a convenience sample of students in the ninth to 12th grades, attending either one private or one of three public high schools in Alabama, Louisiana, and Mississippi to participate. Two schools were in urban communities, one was in a suburban community, and a fourth in a rural area. Although the total student population of the four schools was almost 4,000, the average minority enrollment at the schools was only 19%. The researchers were not afforded access to the entire school population—in fact, at one of the schools, the researchers were only allowed access to the girls’ physical education class. Thus, the sample lacked gender and ethnic diversity. However, the sample reflected the four schools’ diversity geographically, socioeconomically, and in age (from early to late adolescence).
Data were collected during one academic year. The University of Mississippi Medical Center Institutional Review Board (IRB) approved the study. Informed consent of parents and assent of students were required for the student to participate in the study.
Measures
Instruments were selected to measure the concepts of the Identity Threat Model of Stigma (Major & O’Brien, 2005). All instruments were well validated and reliable. Participants completed the Implicit Association Test (IAT; Greenwald & Banaji, 1995; Teachman & Brownell, 2001), the Coping Responses Inventory–Youth (CRI-Youth; Moos, 1993), the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983), and selected questions from the Youth Risk Behavior Survey (YRBS; CDC, 2011).
The IAT, a timed test used to measure subconscious automatic attitudes, screens for implicit weight bias (stigma) in the model. Implicit measures have been widely used in social science research to access and bring to awareness deeply held views operating automatically, even contrary to views consciously expressed. The CRI-Youth, a 48-item self-report inventory, measures the style of coping responses, which represents the volitional (coping) response in the model. The instrument measures cognitive or behavioral coping efforts, as well as approach or avoidant strategies to the coping process. The CRI-Youth is used for ages 12 to 18 years, and is written on a sixth-grade reading level. The PSS, a 10-item scale, measures the degree one perceives their life events as stressful and represents the nonvolitional response to stigma in the model. It has been validated for use in individuals with junior high educational levels and above. Finally, selected questions from the YRBS measured the health outcomes of the model, specifically DE behaviors, physical activity levels, and self-perceived weight status of participants. Questions on DE queried if fasting, diet pills, self-induced vomiting, or laxatives were used to control weight in the last 30 days. Questions on physical activity included number of days per week of 60 min or more of activity, as well as screen time in hours per day. The YRBS was developed by the CDC as a component of their Youth Risk Behavior Surveillance System, and has been used by the CDC to surveil six categories of health risk behaviors of youth in all 50 states, on a biennial basis since 1990. In addition to these instruments, the students completed a demographic questionnaire, developed by the authors, to capture the personal characteristics of the model, as well as to describe the sample. The demographic questionnaire was written in a fill-in-the-blank style; participants wrote in all responses without choosing from preselected options.
Data Collection Procedures
School officials gave permission to conduct the study at their institutions. The researchers were on campus at each site for face-to-face recruitment. An information sheet was given to the students to take home to the parents and guardians if they were interested in participating. Parents willing to allow their child to participate signed and returned the parental consent. The research team returned to the school the following day to collect parental consents and obtain signed student assent.
The surveys were completed in the following order: the IAT, the CRI-Youth, the PSS, the demographic questionnaire, and the YRBS. This was necessary as both the IAT and the CRI-Youth require a script to be read aloud to the participants. In addition, the IAT requires two timed practice demonstrations, followed by the administration of two timed tasks, with instructions given between the practice demonstrations and the tasks.
Results were hand-scored and entered into a spreadsheet. Individual paths were tested using linear or logistic regression; path analysis was used to ascertain relationships among all variables of the Identity Threat Model of Stigma (Major & O’Brien, 2005). Data were analyzed using IBM SPSS 22.0 for measures of central tendency and linear regression, and path analysis was conducted using IBM SPSS AMOS 22.0 software.
Results
Sample Characteristics
The sample (N = 302) demographics were 76.5% White, 11.9% Black, 2.3% Hispanic, and 6.6% Other (2.6% had missing data on race). Most (72%) were female. All high school grades were represented in the sample, with 43.7% of the sample enrolled in the ninth grade. Almost 30% of the sample was 15 years of age. For maternal education, a proxy for socioeconomic status (SES), most mothers were college graduates (28.5%) or had some college (24.2%).
Children’s age-adjusted body mass index (BMI) indicated the majority was in the healthy weight category (62.9%). The categories of overweight and obese students were nearly equal (13.2% and 13.9%, respectively), thus representing over a quarter of the students (27.1%) when combined. Only nine (3%) participants were underweight. On the YRBS questions, almost half of the participants (49.3%) indicated they were “about the right weight.” Over a third of the students (35.4%) indicated they were overweight. Half of this sample (50.5%) indicated they were trying to lose weight. Nearly 40% said they were trying to stay the same weight or were not trying to do anything about their weight (see Table 1).
Table 1.
Demographic Characteristics.
| Characteristic | Frequency (N = 302) | Percentage |
|---|---|---|
| Race/ethnicity | ||
| White | 231 | 76.5 |
| Black | 36 | 11.9 |
| Hispanic | 7 | 2.3 |
| All Other | 20 | 6.6 |
| Missing | 8 | 2.6 |
| Gender | ||
| Female | 218 | 72.2 |
| Male | 79 | 26.2 |
| Missing | 5 | 1.7 |
| Age (years) | ||
| 14 | 63 | 20.9 |
| 15 | 89 | 29.5 |
| 16 | 71 | 23.5 |
| 17 | 56 | 18.5 |
| 18 | 8 | 2.6 |
| Missing | 15 | 5.0 |
| Maternal education level | ||
| <High school | 29 | 9.6 |
| High school graduatea | 63 | 20.9 |
| Some college or trade school | 73 | 24.2 |
| College graduate | 86 | 28.5 |
| Missing | 51 | 16.9 |
| Weight status (BMI for age) | ||
| Underweight | 9 | 3.0 |
| Normal weight | 190 | 62.9 |
| Overweight | 40 | 13.2 |
| Obese | 42 | 13.9 |
| Missing | 21 | 7.0 |
| Self-perception of weight status | ||
| Underweight | 43 | 14.2 |
| Right weight | 149 | 49.3 |
| Overweight | 85 | 28.1 |
| Very overweight | 22 | 7.3 |
| Missing | 3 | 1.0 |
Note. BMI = body mass index.
High school diploma or equivalent.
Weight Stigma, Stress, Avoidant Coping, DE, and Physical Activity
IAT (weight stigma) scores ranged from −5.0 to 24.0 with a mean of 9.15. The majority (94%) of the sample indicated a positive IAT effects score, indicative of weight stigma or antifat bias in an overwhelming majority of the participants. Even though the majority of the records were positive, the data were not skewed, as analysis was based on the mean, rather than 0. The histogram on this variable was normally distributed; therefore, no normalization nor transformation of this variable was necessary for analysis.
For perceived stress (PSS), the median was 20.5, with a range of 4 to 40; higher scores indicated higher perceived stress level. Eighteen students (6%) scored 31 or greater, indicating these participants endorsed the highest stress perception. The frequency of 143 participants (47%) scored above the median, indicating they perceived more stress in their day-to-day life than their average participant peer. No participants reported 0 perceived stress.
On the CRI-Youth (Moos, 1993), the following subscales indicated avoidant coping responses: Cognitive Avoidance, Acceptance or Resignation, Seeking Alternative Rewards, and Emotional Discharge. Of these responses, the greatest number of participants used cognitive avoidance, with 40.9% reporting full-scale use of this strategy; this was followed by acceptance or resignation at 38.5% and emotional discharge at 33.2%. Of avoidant coping strategies, seeking alternative rewards was used the least. However, when the avoidant categories were combined, approximately one third (n = 95) of the sample indicated moderate or full-scale adoption of an avoidant style of coping.
Responses of DE from the three questions of the YRBS indicated that fasting for over 24 hr as a weight control strategy was endorsed by the largest percentage of those affirming DE at 15.4% (n = 46). DE was defined as engaging in any one (or more) of the behaviors addressed, and when responses were combined into an overall DE variable, 20.4% (n = 61) of the participants were categorized as having DE. On the three questions related to physical activity or sedentary behavior, almost a fourth of the sample (n = 87) did not meet the 60 min at least 3 times per week recommendation (CDC, 2015). Furthermore, it has been recommended that students watch no more than 2 hr of TV per day (Council on Communications and Media, 2013); slightly more than half the sample (n = 142) did not meet the recommendation. Finally, computer and gaming screen time recommendations are less than 2 hr per day. Over half of the sample (n = 179) did not meet this recommendation (see Table 2).
Table 2.
Youth Risk Behavior Survey Outcome Variables.
| Indicator | Frequency | Percentage |
|---|---|---|
| Disordered eating | ||
| No disordered eating | 238 | 78.8 |
| Disordered eatinga | 61 | 20.2 |
| Fasting | 46 | 15.2 |
| Took pills, etc. | 21 | 7.0 |
| Vomited/laxatives | 16 | 5.3 |
| Missing | 3 | 1.0 |
| Active for 60 min/week | ||
| 0–2 days | 83 | 27.5 |
| 3–4 days | 90 | 29.8 |
| ≥5 days | 125 | 41.4 |
| Missing | 4 | 1.3 |
| Hours of TV watching/day | ||
| <2 hr | 81 | 26.8 |
| 2–3 | 131 | 43.4 |
| 4 | 47 | 15.6 |
| ≥5 | 37 | 12.3 |
| Missing | 6 | 2.0 |
| Computer and/or gaming hours/day | ||
| <2 | 130 | 43.0 |
| 2–3 | 80 | 26.5 |
| 4 | 60 | 19.9 |
| >5 | 27 | 8.9 |
| Missing | 5 | 1.7 |
Some participants endorsed more than one disordered eating behavior.
Regression and Path Analysis
Demographic predictors of weight stigma
In the Identity Threat Model of Stigma (Major & O’Brien, 2005), personal characteristics influence stigma; in the tested model, the demographic variables were regressed to assess their impact on weight stigma. In this path, the exogenous demographic variables were maternal education level (proxy for socioeconomic level), grade (proxy for age), race/ethnicity, gender, and BMI category; and the dependent variable was IAT effects, which is the measure of weight stigma. White race was the referent variable for race/ethnicity. Female gender was coded as 1 for the gender variable. For this regression model, the ANOVA, representing the cumulative contributions of all variables, was significant (F = 5.161, p < .001). Maternal education level, grade, and BMI category were all significant predictors, with p values <.001, .01, and .03, respectively. Similar results were obtained when a linear regression model was run using BMI percentile, instead of BMI category; again, the ANOVA was significant (F = 5.063, p < .001). Maternal education level, grade, and BMI percentile remained significant, with p values <.001, .01, and .04, respectively.
DE and physical activity paths
With demographic variables included, direct paths from perceived stress to DE (p = .35) or physical activity (p = .78) were not significant. Avoidant coping was a predictor of DE (p = .01), with participants endorsing avoidant coping more than 1.44 times as likely to also endorse DE. The path from avoidant coping to physical activity was not significant. The direct path from weight stigma to both DE and physical activity was nonsignificant (p = .17 and .63, respectively). Weight stigma to DE and physical activity through perceived stress did not change the direct paths results.
Regression was utilized to test the indirect paths from weight stigma to the outcome variables of DE and physical inactivity through increased perceived stress and avoidant coping. The regression model was significant (p < .001), accurately predicting 79.3% of the cases. With these three variables added into the model, only avoidant coping was demonstrated as a predictor (p = .001), with p values for PSS and IAT effects of .21 and .56, respectively. However, for the DE outcome variable of fasting alone, the model was stronger (p < .001, Hosmer and Lemeshow test p = .82). For the fasting variable alone, 84.6% of the cases were accurately predicted. The model was significant for avoidant coping (p = .01) and also significant for PSS (p = .03); however, the IAT effects variable was not significant (p = .58). Those who endorsed avoidant coping were 1.4 times more likely to also endorse fasting; those with increased PSS were 1.17 times more likely to endorse fasting. The model was not significant for either physical inactivity variable.
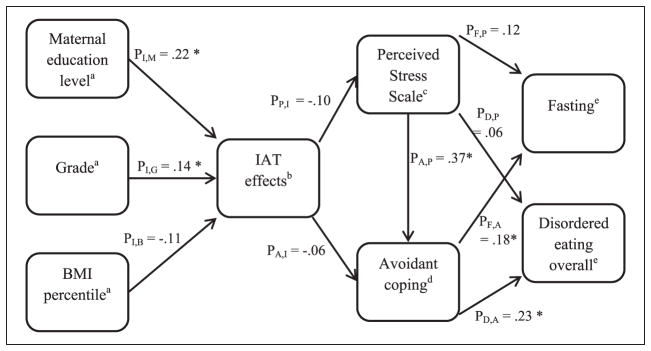
Final regression analysis and path model
The direct and indirect paths from weight stigma, PSS, and avoidant coping to the outcome variables were analyzed using Amos. The path analysis provided support for a direct path from PSS to avoidant coping (p < .001), and a direct path from avoidant coping to fasting (p = .01) and to DE overall (p < .001). Unlike the regression analysis, the path from PSS to the outcome variables was not significant in the Amos analysis.
Finally, demographic variables were added to the model. Using logistic regression for the variable of fasting, this model was significant (p = .01) and accurately predicted 85.8% of cases. For the variable of DE overall, the model was significant (p = .002), with 81.8% of cases predicted accurately. When all variables were added to the model, only avoidant coping was significant (p = .02), and those with avoidant coping were 1.2 times more likely to endorse DE overall. When the demographic variable of BMI percentile was included in the model, rather than BMI category, the model was significant (p = .01) and accurately predicted 85.8% of the cases, and the only significant demographic variable was female gender (p = .04). For the DE overall variable, when BMI percentile rather than BMI category was included, the model was also significant (p = .001), and accurately predicted 80.9% of cases. Significant variables in the model were BMI percentile and avoidant coping with both p values of .02. Neither model with the two physical inactivity overall variables was significant.
When the final path model was diagramed and analyzed in Amos, using BMI percentile, the model would only run successfully if female gender and the race/ethnicity variables were not included. Taken together, the Identity Threat Model of Stigma (Major & O’Brien, 2005) provided the conceptual framework for this study. Although there were no significant paths from the IAT to PSS, the p value of .073 suggests some marginal effects of the IAT toward the PSS, Avoidant Coping, and DE; therefore, the authors conclude that the model provides a partial theoretical explanation for weight stigma in this sample. Furthermore, the following significant paths were found. The personal characteristics of maternal education level, grade, and BMI percentile predicted weight stigma. The involuntary responses to the identity threat of weight stigma were predictive of the voluntary response of avoidant coping. The voluntary response of avoidant coping was significantly predictive of the outcome variables of DE and fasting. The final path diagram and modified theoretical model is displayed in the diagram (Figure 1).
Figure 1.
Path analysis for weight stigma as identity threat.
Note. BMI = body mass index.
a. Represents demographic data and personal characteristics. Maternal education level is a proxy for socioeconomic status; grade is a proxy for age.
b. Represents weight stigma.
c. Represents involuntary response to weight stigma.
d. Represents voluntary response to weight stigma.
e. Represents health outcomes.
*A significant path with a p value <.05.
Discussion
Using the Identity Threat Model of Stigma (Major & O’Brien, 2005), the research team theorized collective representations of obesity in society, personal characteristics of the targeted individual, and stigmatizing experiences as situational cues that influence perception of a social identity threat in the weight-stigmatized youth. These representations trigger responses to that threat and ultimately influence weight-related, modifiable health behaviors of DE and physical activity. Identity threat appraisal was operationalized as an implicit association based on weight. In this sample, maternal educational level and grade level affected IAT. Surprisingly, in this sample, IAT did not significantly predict stress, coping, DE, or physical activity as hypothesized or as modeled in the Identity Threat Model (Major & O’Brien, 2005). Stress as a nonvolitional response was indirectly influential and significant on DE through avoidant coping, the measure of a volitional response. IAT, stress, and coping did not have an effect on physical activity. To the researchers’ knowledge, testing Major and O’Brien’s model in weight-based stigma has not previously been done. Using data from over 300 youth, the Identity Threat Model as an explanation of weight-related stigma was only partially supported in this study. It is possible that weight-based stigma is different from other stigma types, and the theory structure is unique. Another possibility could be the instrument used to measure identity threat appraisal that did not adequately capture the full extent of weight stigma the individual experiences.
Conceptually, implicit associations can be a good measure of identity threat appraisal. With the IAT, the aim was to determine the individual’s own beliefs about themselves and others, essentially uncovering their internalization of weight-based identity. Identity threat appraisal is likely a multidimensional concept of which IAT is just one dimension. Nonetheless, 94% of this sample reported a positive IAT effects score, indicating weight stigma or bias in an overwhelming majority of the sample.
Several findings are noteworthy. Over half of the participants reported trying to lose weight. Comparison of frequency counts on the YRBS items indicated that the participants’ self-perceptions did not accurately match his or her actual weight status. Although almost two thirds of the participants were in the normal weight category, less than half perceived and reported themselves as being “about the right weight.” In addition, 27% were actually overweight or obese, but 35% thought they were. Almost 20% exhibited an aspect of DE, with fasting for more than 24 hr the most common behavior used to control weight. This is consistent with a recent meta-analysis of 36 studies that estimated about a quarter of children and adolescents had DE behaviors (He, Cai, & Fan, 2017).
Only 13% in this sample met the recommended 60 min of physical activity per day. This is lower than the national average. Overall, 21.6% of 6- to 19-year-old U.S. children met the guidelines (National Physical Activity Plan, 2016), which has remained consistently low despite focused efforts to increase physical activity among all ages. Physical exercise can reduce stress and can be an opportunity to exit the Cyclic Obesity/Weight-Based Stigma “COBWEBS” loop (Tomiyama, 2014). More so, physical activity is an important public health intervention that has positive effects on physical fitness, management of weight, and preventing chronic disease (Poitras et al., 2016).
The median for PSS was 23, slightly higher than other studies (Williams, Turner-Henson, Langhinrichsen-Rohling, & Azuero, 2017). Over half the sample utilized all four of the avoidant coping strategies to some degree. When avoidant categories were combined, approximately one third of the sample endorsed full use of the avoidant style of coping.
Indirectly increased perceived stress was a predictor of DE behavior through avoidant coping. Avoidant coping was a significant predictor in the final model. Jenkins et al. (2005) demonstrated that in primary and middle school children, perceived stress was associated with unhealthy eating behaviors, and food was used as a coping strategy. Other authors also found relationships between stress and binge eating (Freeman & Gil, 2004; Gluck, 2006). Unhealthy or DE behaviors may be a coping attempt to deal with stress. Women who have DE respond poorly to stress and have maladaptive styles of coping that may worsen binge eating (Freeman & Gil, 2004). These study findings support Puhl and Luedicke (2011) who sought to determine how adolescents cope with weight-based victimization at school. Students who reported a negative affective response to weight teasing or bullying were more likely to use avoidant coping strategies (such as avoiding gym class) and increased food consumption coping strategies (such as binge eating).
This study had a number of strengths. First, the large sample included over 300 participants and was geographically diverse, comprised of students from three different southeastern states from rural, urban, and suburban schools. Another strength was that the sample included students of all weights and BMI status, recognizing that weight stigma might occur in underweight and normal weight adolescents. Furthermore, a community-based sample is a relative strength as many studies draw participants from weight loss treatment or clinical centers. The sample was diverse in its composition of different aged adolescents and multiple socioeconomic situations. An additional strength was the use of the PSS, the CRI-Youth, and questions from the YRBS, all of which have been widely used and validated in adolescents.
Limitations in this study include the nonrandomized sample, which consisted of more females than males. Data were cross-sectional and thus may be subject to variation in how the student felt that day, for example, response bias in those who were having a bad day. Students were asked to recall events over the past 30 days on measures of physical activity, screen time, and DE, which may have introduced biased responses.
This study has implications for future research into the phenomenon of weight-based stigma, particularly theorized as an identity threat. Research to determine whether identity threat appraisal is a single or multidimensional concept and the best instruments to tap those dimensions is needed. For example, the Weight Bias Internalization Scale (Durso & Latner, 2008) may provide a different perspective of how strongly weight bias is internalized in studies that include adolescents with overweight and obesity.
Research into adolescent coping strategies is needed; young adolescents, in particular, have not settled on a coping style, and there may be interventions that could assist young adolescents in developing problem-focused strategies, which may lead to interventions to prevent DE behaviors. School nurses should consider regular screenings for increased perceived stress at school health fairs. The PSS is a free, downloadable instrument, validated for all adolescent age groups, and takes only minutes to complete. Based on positive screens, the school nurse could intervene by teaching alternative coping strategies that are problem-focused rather than avoidant. This would be of particular importance for school nurses working with younger adolescents, as they held the highest weight stigma in this study and typically have the fewest coping strategies in their behavioral repertoire. Also, these recommendations are consistent with those of Puhl, Peterson, and Luedicke (2012) who assessed the preferences of adolescent targets of weight-based victimization as to their perceptions of what may be helpful in coping with and preventing future weight-based victimization. Adolescents not only identified they most preferred help from their friends and peers, but they also desired help from school personnel and parents. To support their coping efforts, they preferred inclusion and target-support interventions from friends, peers, and parents, but they preferred bully focused discipline strategies from teachers and coaches.
Using data from 302 adolescents from three states and the Identity Threat Model of Stigma (Major & O’Brien, 2005), implicit weight stigma or bias was associated with DE, but not with physical activity. Also relevant, adolescents perceived themselves to be more overweight than they actually were. Stress was high among these adolescents, and avoidant coping strategies used were likely to be ineffective over the long term, thus possibly contributing to behaviors that worsen health. The Identity Threat Model of Stigma (Major & O’Brien, 2005) may be valuable in examining weight-based stigma, but further testing is needed.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was made possible, in part, by a seed grant from The University of Mississippi Medical Center School of Nursing. Jennifer C. Robinson is partially supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 1U54GM115428.
Footnotes
Authors’ Note
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Baigrie S, Giraldez L. Examining the relationship between binge eating and coping strategies in a sample of Spanish adolescents. Spanish Journal of Psychology. 2008;11:172–180. doi: 10.1017/s1138741600004212. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Healthy youth! YRBSS: Youth risk behavior surveillance system. 2011 Retrieved from http://www.cdc.gov/healthyy-outh/yrbs/index.htm.
- Centers for Disease Control and Prevention. Childhood obesity facts. 2014 Retrieved from http://www.cdc.gov/obesity/data/childhood.html.
- Centers for Disease Control and Prevention. How much physical activity do children need? 2015 Retrieved from https://www.cdc.gov/physicalactivity/basics/children/
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Council on Communications and Media. Children, adolescents, and the media. Pediatrics. 2013;132:958–961. doi: 10.1542/peds.2013-2656. [DOI] [PubMed] [Google Scholar]
- Durso SE, Latner JD. Understanding self-directed stigma: Development of the weight bias internalization scale. Obesity. 2008;16(Suppl 2):S80–S86. doi: 10.1038/oby.2008.448. [DOI] [PubMed] [Google Scholar]
- Erikson E. Childhood and society. New York, NY: W. W. Norton; 1950. [Google Scholar]
- Freeman L, Gil K. Daily stress, coping, and dietary restraint in binge eating. International Journal of Eating Disorders. 2004;36:204–212. doi: 10.1002/eat.20012. [DOI] [PubMed] [Google Scholar]
- Gluck M. Stress response and binge eating disorder. Appetite. 2006;46:26–30. doi: 10.1016/j.appet.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Greenwald A, Banaji M. Implicit social cognition: Attitudes, self-esteem, and stereotypes. Psychological Review. 1995;102:4–27. doi: 10.1037/0033-295x.102.1.4. [DOI] [PubMed] [Google Scholar]
- Hayden-Wade H, Stein R, Ghaderi A, Saelens B, Zabinski M, Wilfley D. Prevalence, characteristics, and correlates of teasing experiences among overweight children vs. non-overweight peers. Obesity Research. 2005;13:1381–1392. doi: 10.1038/oby.2005.167. [DOI] [PubMed] [Google Scholar]
- He J, Cai Z, Fan X. Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta-analysis. International Journal of Eating Disorders. 2017;50:91–103. doi: 10.1002/eat.22661. [DOI] [PubMed] [Google Scholar]
- Jenkins S, Rew L, Sternglanz R. Eating behaviors among school-age children associated with perceptions of stress. Issues in Comprehensive Pediatric Nursing. 2005;28:175–191. doi: 10.1080/01460860500227580. [DOI] [PubMed] [Google Scholar]
- MacLean L, Edwards N, Garrard M, Sims-Jones N, Clinton K, Ashley L. Obesity, stigma and public health planning. Health Promotion International. 2009;24:88–93. doi: 10.1093/heapro/dan041. [DOI] [PubMed] [Google Scholar]
- Major B, Eliezer D, Rieck H. The psychological weight of weight stigma. Social Psychological & Personality Science. 2012;3:651–658. doi: 10.1177/1948550611434400. [DOI] [Google Scholar]
- Major B, O’Brien LT. The social psychology of stigma. Annual Review of Psychology. 2005;56:393–421. doi: 10.1146/annurev.psych.56.091103.070137. [DOI] [PubMed] [Google Scholar]
- Moos R. Coping Responses Inventory: CRI-Youth form professional manual. Lutz, FL: Psychological Assessment Resources; 1993. [Google Scholar]
- Morris M, Beilharz J, Maniam J, Reichelt A, Westbrook RF. Why is obesity such a problem in the 21st century? The intersection of palatable food, cues and reward pathways, stress, and cognition. Neuroscience & Biobehavioral Reviews. 2015;58:36–45. doi: 10.1016/j.neubiorev.2014.12.002. [DOI] [PubMed] [Google Scholar]
- Nansel T, Craig W, Overpeck M, Saluja G, Ruan W. Cross-national consistency in the relationship between bullying behaviors and psychosocial adjustment. Archives of Pediatrics and Adolescent Medicine. 2004;158:730–736. doi: 10.1001/archpedi.158.8.730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Physical Activity Plan. 2016 U.S. report card on physical activity for children and youth. Columbia, SC: Author; 2016. [Google Scholar]
- Poitras VJ, Gray CE, Borghese MM, Carson V, Chaput J, Janssen I, … Tremblay MS. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Applied Physiology, Nutrition, and Metabolism. 2016;41:S197–S239. doi: 10.1139/apnm-2015-0663. [DOI] [PubMed] [Google Scholar]
- Puhl RM. Childhood obesity and stigma. 2009 Retrieved from http://www.obesityaction.org/educational-resources/resource-articles-2/childhood-obesity-resource-articles/childhood-obesity-and-stigma.
- Puhl RM, Brownell K. Ways of coping with obesity stigma: Review and conceptual analysis. Eating Behaviors. 2003;4:53–78. doi: 10.1016/s1471-0153(02)00096-x. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Latner JD. Stigma, obesity, and the health of the nation’s children. Psychological Bulletin. 2007;133:557–580. doi: 10.1037/0033-2909.133.4.557. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Luedicke J. Weight-based victimization among adolescents in the school setting: Emotional reactions and coping behaviors. Journal of Youth and Adolescence. 2011;41:27–40. doi: 10.1007/s10964-011-9713-z. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Moss-Racusin CM, Schwartz MB. Internalization of weight bias: Implications for binge eating and emotional well-being. Obesity. 2007;15:19–23. doi: 10.1038/oby.2007.521. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Peterson J, Luedicke J. Strategies to address weight-based victimization: Youths’ preferred support interventions from classmates, teachers, and parents. Journal of Youth and Adolescence. 2012;42:315–327. doi: 10.1007/s10964-012-9849-5. [DOI] [PubMed] [Google Scholar]
- Rojo L, Conesa L, Bermudez O, Livianos L. Influence of stress in the onset of eating disorders: Data from a two-stage epidemiological controlled study. Psychosomatic Medicine. 2006;68:628–635. doi: 10.1097/01.psy.0000227749.58726.41. [DOI] [PubMed] [Google Scholar]
- Schvey N, Puhl R, Brownell K. The impact of weight stigma on caloric consumption. Obesity. 2011;19:1957–1962. doi: 10.1038/oby.2011.204. [DOI] [PubMed] [Google Scholar]
- Sikorski C, Luppa M, Luck T, Riedel-Heller S. Weight stigma “gets under the skin”—Evidence for an adapted psychological mediation framework—A systematic review. Obesity. 2015;23:266–276. doi: 10.1002/oby.20952. [DOI] [PubMed] [Google Scholar]
- Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: Is anyone immune? International Journal of Obesity and Related Metabolic Disorders. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- Tomiyama A. Weight stigma is stressful. A review of evidence for the Cyclic Obesity/Weight-Based Stigma model. Appetite. 2014;82:8–15. doi: 10.1016/j.appet.2014.06.108. [DOI] [PubMed] [Google Scholar]
- Vartanian LR, Novak S. Internalized societal attitudes moderate the impact of weight stigma on avoidance of exercise. Obesity. 2011;19:757–762. doi: 10.1038/oby.2010.234. [DOI] [PubMed] [Google Scholar]
- Vartanian LR, Shaprow JC. Effects of weight stigma on exercise motivation and behavior: A preliminary investigation among college-aged females. Journal of Health Psychology. 2008;13:131–138. doi: 10.1177/1359105307084318. [DOI] [PubMed] [Google Scholar]
- Williams SG, Turner-Henson A, Langhinrichsen-Rohling J, Azuero A. Depressive symptoms in 9th graders: Stress and physiological contributors. Applied Nursing Research. 2017;34:24–28. doi: 10.1016/j.apnr.2017.01.001. [DOI] [PubMed] [Google Scholar]
- Yang L, Kleinman A, Link B, Phelan J, Lee S, Good B. Culture and stigma: Adding moral experience to stigma theory. Social Science & Medicine. 2007;64:1524–1535. doi: 10.1016/j.socscimed.2006.11.013. [DOI] [PubMed] [Google Scholar]