Abstract
Purpose
The purposes of the analysis were to compare long-acting reversible contraception (LARC) use estimates that include all reproductive age women with estimates that are limited to women at risk for unintended pregnancy and to examine trends for adolescents (15–19 years) and young adults (20–24 years).
Methods
Using the 2006–2010 and 2011–2013 National Surveys of Family Growth, we compared LARC estimates for all women with estimates limited to women at risk for unintended pregnancy (those who were sexually experienced, and neither pregnant, seeking pregnancy, postpartum or infecund). We used t tests to detect differences according to the population included and to evaluate trends for adolescents and young adults.
Results
Among adolescents and young adults, 56% and 14%, respectively, have never had vaginal intercourse, versus 1%–4% for women aged 25–44 years. Given the high percentage of adolescents and young adults who never had vaginal intercourse, LARC estimates were higher for these age groups (p < .05), but not for women aged 25–44 years, when limited to those at risk for unintended pregnancy. Among adolescents at risk, the increase in LARC use from 2006–2008 (1.1%) to 2008–2010 (3.6%) was not significant (p = .07), and no further increase occurred from 2008–2010 to 2011–2013 (3.2%); by contrast, among young adults at risk, LARC use increased from 2006–2008 (3.2%) to 2008–2010 (6.9%) and from 2008–2010 to 2011–2013 (11.1%).
Conclusions
Because many adolescents and young adult women have never had vaginal intercourse, for these groups, including all women underestimates LARC use for pregnancy prevention. Among young adults, use of LARC for pregnancy prevention has increased but remains low among adolescents.
Keywords: LARC (long-acting reversible contraception), NSFG (National Survey of Family Growth), Youth-friendly services, Sexual experience
Recent estimates indicate nearly half (45%) of all pregnancies in the United States are unintended, and this percentage is substantially higher for adolescents (15–19 years, 75%) and young adults (20–24 years, 59%) as compared with older women (31%–42%) [1,2]. Calculations that have been limited to the population of women who are sexually active also suggest that unintended pregnancy rates are higher among adolescents and young adults as compared with older women [3]. Given these patterns, data are needed to evaluate the impact of improved contraceptive use among adolescents and young adult women who have initiated sexual activity and are at comparatively high risk for unintended pregnancy.
Intrauterine devices and implants, known as long-acting reversible contraception (LARC), require no user effort after insertion and have typical-use failure rates that are comparable to sterilization (<1%) and lower than other commonly used methods, including oral contraceptives (9%) and condoms (18%) [4]. Despite concerns expressed by some providers about the suitability of LARC for young and nulliparous women [5,6], these methods are safe for women of all ages [7], including adolescents, and are recommended by the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics as first-line contraceptive options that can be combined with condoms to provide optimal protection against unintended pregnancy and sexually transmitted infections [5,8].
Recent analyses of the National Survey of Family Growth (NSFG) suggest that LARC use is increasing among U.S. women of reproductive age and remains highest for women aged 25–34 years [9–11]. However, to provide an overall picture of LARC use among women of reproductive age, these reports either included all women, or women using contraception, without taking into account their risk for having an unintended pregnancy. Accounting for unintended pregnancy risk may be especially important for adolescents and young adults: recent estimates indicate that >50% of adolescents and >10% of young adults (vs. 1%–3% of women aged 25–44 years) report they have never had vaginal intercourse [12] and therefore should be at very low risk for unintended pregnancy. Consequently, their inclusion enlarges the denominator and underestimates the use of LARC and other contraceptive methods for pregnancy prevention. Conversely, to the extent that contraception is being used for alternative reasons (e.g., control of acne, heavy menstrual periods), the inclusion of sexually inexperienced women enlarges the numerator beyond the extent appropriate for estimating the use of contraception for pregnancy prevention.
Given the large proportion of adolescents and young adults who report they have never had vaginal intercourse and are at very low risk for unintended pregnancy, the objectives of this analysis were (1) to compare LARC use estimates that include all women with estimates that are limited to women at risk for unintended pregnancy and assess the relative difference for adolescents and young adults versus women in older age groups and (2) to generate trend estimates for adolescents and young adults on the use of LARC for the purpose of pregnancy prevention and assess whether patterns of change differ for estimates that include all women versus the population of women at risk for unintended pregnancy.
Methods
We used data from the 2006–2010 and 2011–2013 NSFGs. The NSFG is conducted by the Centers for Disease Control’s National Center for Health Statistics in collaboration with other agencies of the U.S. Department of Health and Human Services. The survey is based on self-reported data and focuses on fertility, sexual activity, contraceptive use, reproductive health care, family formation, childcare, and related topics, using a stratified, multistage probability sample to create nationally representative estimates for women and men aged 15–44 years in the United States. Interviews are conducted in person by female interviewers. Female respondents are asked to indicate each of the contraceptive methods they or their male partner used every month for up to 4 years before their interview and including the month of their interview. Women who report they are not currently pregnant but were sexually active and did not use a method during their interview month are asked if their reason for not using contraception is that they were trying to get pregnant. The 2006–2010 and 2011–2013 NSFGs contain 12,279 and 5,601 interviews of women with response rates of 78% and 73.4%, respectively [13,14]. We excluded earlier NSFGs because the number of adolescent LARC users was too low to produce reliable estimates [11].
For this analysis, we considered women at risk for unintended pregnancy if they reported they had ever had vaginal intercourse with a male partner and they were neither pregnant, seeking pregnancy, postpartum, or infecund. For each 5-year age group, we calculated the percentage of women we considered at risk for unintended pregnancy and the percentages in each category we did not consider at risk (i.e., the percentage of women who had never had vaginal intercourse, as well as the percentages of women who were pregnant, seeking pregnancy, postpartum or infecund). Among women who reported they had never had vaginal intercourse, we then calculated the percentage who were using contraception.
We defined LARC users as women who reported current use of an intrauterine device or implant. We then estimated LARC use across age groups, first including all women, and a second time limiting the population included to women at risk for unintended pregnancy. For these calculations, we combined the 2006–2010 and 2011–2013 data sets to allow for sufficient sample size for each 5-year age group and performed t tests to detect differences in LARC use by the population included. Finally, among adolescents and young adults, we assessed changes in LARC use over time, first among the full set of women in these age groups, and then a second time among the population at risk for unintended pregnancy. For these analyses we used t tests to compare June 2006–2008 versus July 2008 to June 2010 estimates, and July 2008 to June 2010 versus September 2011–2013 estimates, using the sample weights that allow the 2006–2010 survey to be separated into two time periods.
All analyses were conducted using SAS callable SUDAAN, version 9.3 (RTI International, Research Triangle Park, NC), to account for the complex sample and design variables of the NSFG. The NSFG was approved by the institutional review board at the National Center for Health Statistics of the Centers for Disease Control and Prevention.
Results
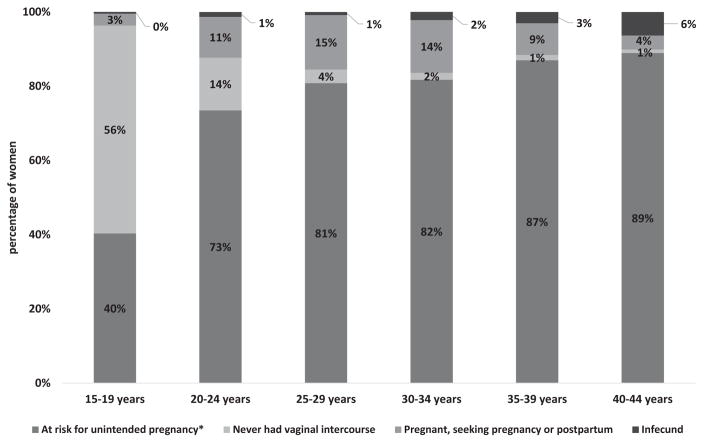
Across age groups, the combined 2006–2010 and 2011–2013 data set indicated that progressively smaller percentages of women were excluded from the population at risk for unintended pregnancy because they either reported they had never had vaginal intercourse or they were pregnant, seeking pregnancy, postpartum, or infecund (Figure 1). The proportion included in the population at risk for unintended pregnancy was greatest for women aged 35–44 years, although >50% of women in this age group reported use of sterilization, which is as effective as LARC but is only an option for women who have completed their desired childbearing.
Figure 1.
Percentage distribution of women by category of risk for unintended pregnancy and age group, National Survey of Family Growth, 2006–2010 and 2011–2013. *Women are considered at risk if they have ever had vaginal intercourse and are not pregnant, seeking pregnancy, postpartum, or infecund.
Adolescents aged 15–19 years and young adults aged 20–24 years were most commonly excluded from the population at risk for unintended pregnancy because they reported they had never had vaginal intercourse (56% and 14%, respectively, for adolescents and young adults), although 11% of young adults also were excluded because they reported they were pregnant, seeking pregnancy, or postpartum. Of the adolescents and young adults who reported they had never had vaginal intercourse, 11% were using contraception (data not shown); among these users, most reported pills (86%) or injectables (10%) as their most effective method, while the use of LARC was too low to produce reliable estimates.
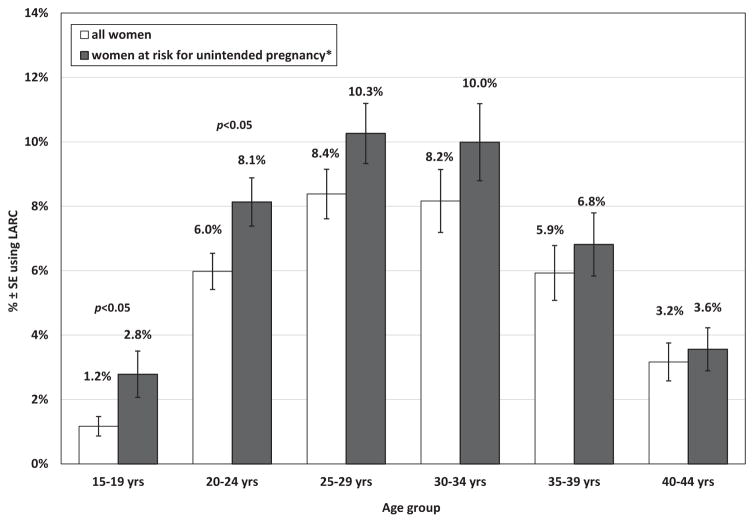
Figure 2 shows estimates of LARC use by age group for all women and then limited to women at risk for unintended pregnancy. Across age groups, differences by the population included were progressively smaller; LARC use estimates limited to women at risk for unintended pregnancy as compared to all women were 138% higher for adolescents aged 15–19 years, 36% higher for young adults aged 20–24 years, and 12%–22% higher for women aged 25–44 years. Differences by the population included were significant for adolescents (p < .05) and young adults (p < .05), but not for women 25–44 years.
Figure 2.
Percentage of women using LARC by age group, National Survey of Family Growth, 2006–2010 and 2011–2013. *Women are considered at risk if they have ever had vaginal intercourse and are not pregnant, seeking pregnancy, postpartum, or infecund.
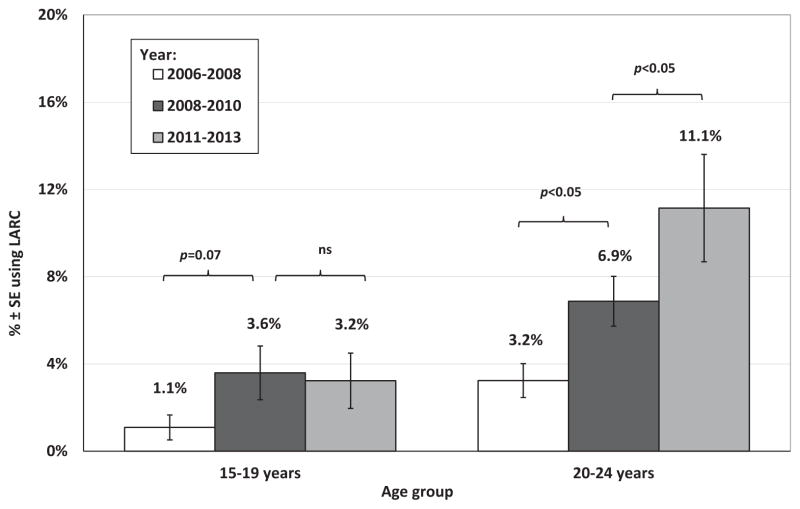
Among all adolescents aged 15–19 years, including those who reported they had never had vaginal intercourse and were not considered at risk for unintended pregnancy, LARC use increased from 2006–2008 (.4%, standard error [SE] = .2) to 2008–2010 (1.5%, SE = .5; p = .05), but increased no further from 2008–2010 to 2011–2013 (1.4%, SE = .5; not significant; analysis not shown). Among adolescents at risk for unintended pregnancy, the increase in LARC use from 2006–2008 (1.1%, SE = .6) to 2008–2010 (3.6%, SE = 1.2) was not significant (p = .07), and no further increase occurred from 2008–2010 to 2011–2013 (3.2%, SE = 1.3; not significant; Figure 3). Among all young adults, LARC use increased from 2006–2008 (2.3%, SE = .5) to 2008–2010 (5.2%, SE = .8; p < .05) and again from 2008–2010 to 2011–2013 (8.2%, SE = 1.0; p < .05; analysis not shown). Similarly, among young adults at risk for unintended pregnancy, LARC use increased from 2006–2008 (3.2%, SE = .8) to 2008–2010 (6.9%, SE = 1.1; p < .05) and again from 2008–2010 to 2011–2013 (11.1%, SE = 1.3; p < .05; Figure 3).
Figure 3.
Percentage of women aged 15–19 and 20–24 years at risk for unintended pregnancy* using LARC, National Survey of Family Growth, 2006–2008, 2008–2010, and 2011–2013. *Women are considered at risk if they have ever had vaginal intercourse and are not pregnant, seeking pregnancy, postpartum, or infecund.
Discussion
This analysis suggests for adolescents aged 15–19 years and young adults aged 20–24 years, it is important to limit the population to those who are at risk for unintended pregnancy when estimating the use of LARC for pregnancy prevention. Although estimates showed a similar pattern of change over time irrespective of the population included, estimates limited to individuals at risk for unintended pregnancy were 138% higher for adolescents due to the exclusion of the high proportion who reported they had never had vaginal intercourse. Estimates of LARC use for pregnancy prevention were 36% higher for young adults aged 20–24 years, both because of the comparatively high proportion who reported they had never had vaginal intercourse and because of the proportion who reported they were pregnant, seeking pregnancy, or postpartum. Estimates limited to the population at risk for unintended pregnancy indicate the use of LARC for pregnancy prevention has continued to increase among young adult women but remains low among adolescents.
Traditional calculations that include all women of reproductive age provide a broad picture of contraceptive use patterns among the full U.S. population. However, greater precision is needed to estimate the proportion of women at risk who have been effectively targeted by prevention efforts. Because over half of the adolescents in our analysis reported they had never had vaginal intercourse, by excluding these individuals, we reduced our denominator proportionally more in this as compared to any other age group, with important implications for measuring the use of LARC for pregnancy prevention. Adolescent pregnancy prevention efforts address the risk of unintended pregnancy that all adolescents face after menarche both by encouraging them to delay having sex and by promoting the use of effective contraception among those who have decided to begin having sex [15]. Because many adolescents do remain sexually inactive throughout their teen years [16], on a population level, estimates are needed that exclude individuals from the denominator who have never had sex. While some individuals may simply not disclose their history of sexual activity through self-reported data, as a group, individuals who report they have never had sex are at very low risk. Consequently, separate estimates are needed for those adolescents who report they have begun having sex, so that we can assess efforts to provide contraception for those who as a group face a more measurable risk [17]. Conversely, on a population level, including individuals who are using contraception for alternative reasons (e.g., control of acne, heavy menstrual periods) can enlarge the numerator beyond the extent appropriate for estimating the use of contraception for pregnancy prevention. In our analysis, use of LARC among adolescents and young adults who reported they had never had vaginal intercourse was rare, suggesting minimal influence on our numerator, but use of pills was more common. Given the well-documented noncontraceptive benefits of oral contraceptives [4], more careful evaluation is needed on the reasons for use among those who have never had vaginal intercourse to ensure that individuals excluded are not using this method in anticipation of sexual imitation.
For this analysis, we considered all women who reported they had ever had vaginal intercourse to be at risk for unintended pregnancy so long as they were not pregnant, seeking pregnancy, postpartum, or infecund. Estimates with a more restrictive inclusion for sexual activity (e.g., estimates considering women at risk only if they reported having vaginal intercourse in the past 3 months [12]) would further limit the denominator and may result in even higher estimates of LARC use. Similarly, estimates based on the population of women currently using contraception take women out of the denominator if they are not using any method of contraception, irrespective of whether they are sexually experienced or sexually active, and again may result in higher estimates [9,10].
In addition to illustrating the importance of carefully defining the population of women included in estimates of the use of LARC for pregnancy prevention, this analysis reinforces the need to generate estimates separately for adolescents and for young adult women. NSFG estimates of LARC use for women aged 15–24 years combined show the increase for this age group from 2006–2010 to 2011–2013 was much smaller than the increase for women aged 25–34 years [10,11]. Given our analysis shows LARC use among adolescents aged 15–19 years did not change over this time period, using a combined age group of women aged 15–24 years masks the marked increase among young adults aged 20–24 years. Indeed, subsequent analyses looking at women aged 20–24 years separately have shown large increases for this age group, but no change for adolescents aged 15–19 years [9].
Use of LARC among adolescents and young adults who have initiated sexual activity can provide more effective protection against unintended pregnancy than the methods women in these age groups use most often (i.e., pills and condoms) [12]. However, barriers to accessing LARC remain, including high upfront costs and complex reimbursement requirements, patient misperceptions and lack of awareness of LARC, and lack of health care provider training on insertion and removal and the suitability of LARC for young and nulliparous women [6,18–21]. This final barrier may be particularly salient for adolescents as compared with young adults. A recent national survey of publicly funded clinics found that healthcare providers discuss LARC more often with young adults as compared to adolescents [22]. However, providers discussed LARC with a higher percentage of adolescents at facilities offering youth-friendly services (e.g., confidential services, extended hours, online scheduling, youth-friendly materials and environment, staff trained on teen communication) [22], and research has shown that adolescents frequently select LARC as their preferred option when counseled about these methods along with the range of appropriate methods [23,24]. Given the recent position statements issued by the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics encouraging providers to discuss LARC with adolescents [5,8], data are needed to assess whether the use of these methods increases among adolescents as it has for young adults and women in older age groups.
IMPLICATIONS AND CONTRIBUTION.
Because many adolescents and young adult women have never had vaginal intercourse, limiting calculations for these age groups to individuals who are sexually experienced and at risk for unintended pregnancy provides more accurate estimates of the use of long-acting reversible contraception and other contraceptives for pregnancy prevention.
Acknowledgments
Funding Sources
The authors received no external funding for this work.
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374:843–52. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health. 2014;104(Suppl 1):S43–8. doi: 10.2105/AJPH.2013.301416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finer LB. Unintended pregnancy among U.S. adolescents: Accounting for sexual activity. J Adolesc Health. 2010;47:312–4. doi: 10.1016/j.jadohealth.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Hatcher RA, Trussell J, Nelson AL, et al. Contraceptive technology. 20. Atlanta, GA: Ardent Media, Inc; 2011. [Google Scholar]
- 5.American College of Obstetricians Gynecologists. Adolescents and long-acting reversible contraception: Implants and intrauterine devices. Committee Opinion No. 539. Obstet Gynecol. 2012;120:983–8. doi: 10.1097/AOG.0b013e3182723b7d. [DOI] [PubMed] [Google Scholar]
- 6.Harper CC, Blum M, de Bocanegra HT, et al. Challenges in translating evidence to practice: The provision of intrauterine contraception. Obstet Gynecol. 2008;111:1359–69. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control. US medical eligibility criteria for contraceptive use, 2010. MMWR Recomm Rep. 2010;59:1–86. [PubMed] [Google Scholar]
- 8.American Academy of Pediatrics Committee on adolescence. Contraception for adolescents. Pediatrics. 2014;134:e1244–56. [PubMed] [Google Scholar]
- 9.Kavanaugh M, Jerman J, Finer L. Changes in use of long-acting reversible contraceptive methods among U.S. women, 2009–2012. Obstet Gynecol. 2015;126:917–27. doi: 10.1097/AOG.0000000000001094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daniels K, Daugherty J, Jones J, et al. Current contraceptive use and variation by selected characteristics among women aged 15–44: United States, 2011–2013. Natl Health Stat Rep. 2015;86:1–15. [PubMed] [Google Scholar]
- 11.Branum AM, Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15–44. NCHS Data Brief. 2015;188:1–8. [PubMed] [Google Scholar]
- 12.Jones J, Mosher W, Daniels K. Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995. Natl Health Stat Rep. 2012;60:1–25. [PubMed] [Google Scholar]
- 13.Groves R, Mosher W, Lepkowski J, et al. Planning and development of the continuous national survey of family Growth. National Center for Health Statistics. Vital Health Stat. 2009;1:1–73. [PubMed] [Google Scholar]
- 14.Daniels K, Daugherty J, Jones J. Current contraceptive status among women aged 15–44: United States, 2011–2013. NCHS Data Brief. 2014;173:1–8. [PubMed] [Google Scholar]
- 15.Goesling B, Colman S, Trenholm C, et al. Programs to reduce teen pregnancy, sexually transmitted infections, and associated sexual risk behaviors: A systematic review. J Adolesc Health. 2014;54:499–507. doi: 10.1016/j.jadohealth.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Martinez G, Abma J. Sexual activity, contraceptive use, and childbearing of teenagers aged 15–19 in the United States. NCHS Data Brief. 2015;209:1–8. [PubMed] [Google Scholar]
- 17.Santelli JS, Lindberg LD, Finer LB, et al. Explaining recent declines in adolescent pregnancy in the United States: The contribution of abstinence and improved contraceptive use. Am J Public Health. 2007;97:150–6. doi: 10.2105/AJPH.2006.089169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hathaway M, Torres L, Vollett-Krech J, et al. Increasing LARC utilization: Any woman, any place, any time. Clin Obstet Gynecol. 2014;57:718–30. doi: 10.1097/GRF.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 19.Brown MK, Auerswald C, Eyre SL, et al. Identifying counseling needs of nulliparous adolescent intrauterine contraceptive users: A qualitative approach. J Adolesc Health. 2013;52:293–300. doi: 10.1016/j.jadohealth.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Potter J, Rubin SE, Sherman P. Fear of intrauterine contraception among adolescents in New York City. Contraception. 2014;89:446–50. doi: 10.1016/j.contraception.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoopes AJ, Gilmore K, Cady J, et al. A qualitative study of factors that influence contraceptive choice among adolescent school-based health center patients. J Pediatr Adolesc Gynecol. 2016;29:259–64. doi: 10.1016/j.jpag.2015.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kavanaugh ML, Jerman J, Ethier K, et al. Meeting the contraceptive needs of teens and young adults: Youth-friendly and long-acting reversible contraceptive services in U.S. family planning facilities. J Adolesc Health. 2013;52:284–92. doi: 10.1016/j.jadohealth.2012.10.276. [DOI] [PubMed] [Google Scholar]
- 23.Secura GM, Madden T, McNicholas C, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med. 2014;371:1316–23. doi: 10.1056/NEJMoa1400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: Widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46:125–32. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]