Introduction
Key Teaching Points.
-
•
Electrophysiologic study is necessary to differentiate fasciculoventricular pathway (FVP) from potentially dangerous atrioventricular accessory pathways, especially anteroseptal or midseptal bypass tracts. Even in the absence of symptoms, the literature supports serious consideration of invasive evaluation for risk stratification.
-
•
Presence of FVP is confirmed in a patient with preexcitation on electrophysiological study by observing prolongation of the A-H interval without a change in H-V interval during incremental or programmed atrial stimulation and fixed preexcitation with decremental AV node conduction. In a typical accessory pathway, AV nodal Wenckebach is absent, as it is masked by conduction over the accessory pathway. For the same reason, blocked P waves are not observed because the pathway offers an alternate route to the ventricle.
-
•
FVP has never been demonstrated to be incorporated into a circus movement supraventricular tachycardia. When tachycardias are present in the setting of normal AV node function, FVP acts as an innocent bystander. As such, its presence does not increase risk of sudden cardiac death.
A history of ventricular preexcitation conditions is disqualifying from service in the United States Navy.1 Between 0.1% and 0.3% of the population have elements of electrocardiographic preexcitation,2 with these conditions being managed based on the presence or absence of symptoms. A diagnosis of Wolff-Parkinson-White syndrome is established when patients with electrocardiographic preexcitation develop symptoms of palpitations or presyncope.3 Because the risk of sudden cardiac death in these patients is estimated to be 4% over a lifetime4 and because of the necessity for sailors to spend prolonged periods in medically austere environments, these conditions typically prohibit military service.
Fasciculoventricular pathway (FVP) is a very rare form of preexcitation resulting from an accessory connection between either the bundle of His or the fascicles and the ventricle.5 Patients with FVP demonstrate ventricular preexcitation on electrocardiogram (ECG) but are not at risk of reciprocal tachycardias or sudden cardiac death.6 We present a case of a young sailor who presented with evidence of ventricular preexcitation on surface ECG (Figure 1). An electrophysiological study was performed and these findings were deemed secondary to FVP. The sailor subsequently obtained a waiver of physical standards for continued special duty.
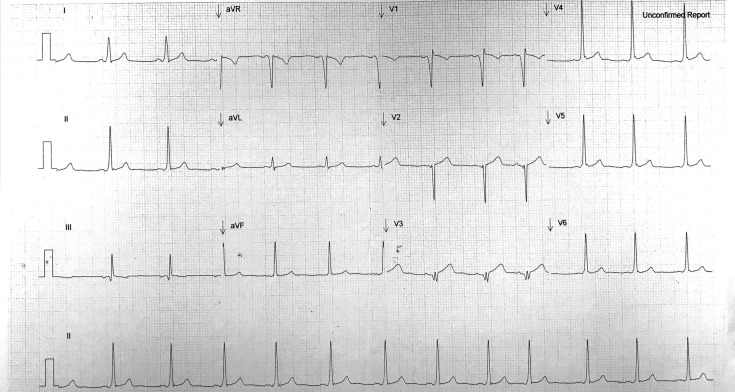
Figure 1.
Patient's 12-lead surface electrocardiogram. Sinus rhythm at 75 beats per minute, PR interval of 128 ms, QRS interval of 98 ms, and QTc interval of 411 ms. Evidence of preexcitation demonstrated by slurred QRS upstroke (delta wave) in leads V4-V6.
Case report
A 22-year-old male seaman on active duty in the US Navy submarine service presented with acute onset of right-sided chest discomfort during a physical readiness test. On examination, his vital signs were within normal limits and the chest discomfort was reproducible with palpation. An ECG showed normal sinus rhythm with a PR interval of 128 ms, delta waves in leads V4–V6 (Figure 1). Laboratory results and imaging were unremarkable. The pain resolved spontaneously without intervention. The patient was referred to the Undersea Medical Officer to assess his duty status.
Further evaluation included a transthoracic echocardiogram that did not show any evidence of structural heart disease. A stress echocardiogram was negative for ischemia. During that study, electrocardiographic delta waves were present at rest, persisted at peak activity, disappeared during early recovery, and returned shortly thereafter. An event monitor worn for 22 days showed sinus rhythm without any evidence of ectopy.
According to the physical standards governing service in the submarine force, a history of ventricular preexcitation conditions is considered disqualifying.1 The instruction specifically notes that a waiver to continue duty will be considered for personnel with a ventricular preexcitation ECG pattern who: “(a) Have never had a documented dysrhythmia, (b) Have never had a symptomatic episode consistent with a paroxysmal dysrhythmia (e.g. palpitations, dizziness, chest pain, dyspnea, loss of consciousness), and (c) Have been found to be at extremely low risk for a future event as determined by a cardiologist in conjunction with electrophysiologic study if indicated.”
Given that the patient's history was not clearly consistent with Wolff-Parkinson-White syndrome as well as his desire to return to duty, an electrophysiological study was obtained for identification of any potentially arrhythmogenic substrate and further risk stratification of the ventricular preexcitation syndrome.
Baseline measurements included a sinus cycle length of 780 ms, PR of 125 ms, QRS of 120 ms, and QT of 380 ms. A-H interval was 47 ms. H-V interval was 15 ms, providing confirmatory evidence of ventricular preexcitation. There was no VA conduction at baseline. With incremental pacing at 360 ms, the QRS normalized and the H-V interval was 50 ms. Antegrade Wenckebach occurred at 340 ms.
Adenosine administration demonstrated prolongation of the A-H interval while the H-V interval remained constant. Isoproterenol was given. Para-Hisian pacing as outlined by Hirao and colleagues7 was performed and yielded a nodal response. There was no change in atrial activation sequence during these maneuvers, suggesting the absence of an accessory pathway connecting the atrium to the ventricle.
With single atrial premature beats, the accessory pathway blocked at 300/240 ms. Aggressive stimulation at 300/200/200/240 ms resulted in block at the AV node without any echo beats. Burst pacing from the atria and the ventricle did not reveal any inducible tachycardia. Anterograde effective refractory period of the accessory pathway was observed at 250 ms. Atrial fibrillation was induced and the shortest R-R interval was 280 ms, above the interval concerning for potentially malignant arrhythmia.
All findings of the electrophysiological study were consistent with a diagnosis of FVP. No ablation was performed. Although the patient's presentation could have potentially disqualified him from continued submarine service, a special duty waiver was submitted on his behalf. The waiver was granted because of the careful elucidation of his conducting system in the electrophysiological study. At 1 year follow-up, the patient remains asymptomatic and as a newly qualified submariner, he is a productive member of his boat's crew.
Discussion
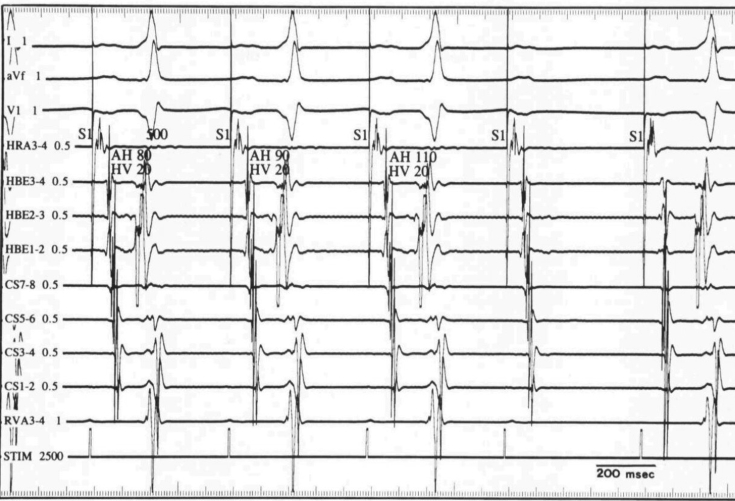
FVP is very rare, occurring in 1.2% to 5.1% of patients with symptomatic preexcitation.8, 9, 10, 11 No data have been published or presented regarding the prevalence in patients without symptoms. Surface ECG alone is insufficient to differentiate between typical atrioventricular accessory pathways and FVP.12 Presence of FVP is confirmed in a patient with preexcitation by observing prolongation of the A-H interval without a change in H-V interval during incremental or programmed atrial stimulation and fixed preexcitation with decremental AV node conduction. (Figure 2).13, 14 These subnodal bypass tracts have not been found to participate in circus movement supraventricular tachycardias and their precarious anatomic location would confer high risk of irreversible conduction system damage during ablation. Thus, no intervention is recommended.
Figure 2.
Intracardiac tracing during atrial pacing at 500 msec during adenosine infusion in a similar case.14 FVP is identified by prolongation of the AH interval and constant degree of preexcitation with fixed H-V interval. When AV node is blocked, block occurs in accessory pathway simultaneously. (Republished with permission of John Wiley and Sons Inc from the Journal of Cardiovascular Electrophysiology; permission conveyed through copyright clearance center).
In this case, it was necessary to obtain more information regarding presence of potentially arrhythmogenic substrate in order to meet US Navy physical standards for submarine duty, but there is evidence to support invasive testing in a broader population with preexcitation. Recent American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines suggest that existing evidence in the literature supports risk stratification with an electrophysiological study in certain circumstances, even in the absence of symptoms.15 Most importantly, data from the largest registry of patients with preexcitation syndromes showed that malignant arrhythmias correlate more with the electrophysiological properties of the accessory pathway than with the presence or absence of symptoms.16 Specifically, Pappone and colleagues16 identified inducible atrioventricular reentrant tachycardia triggering atrial fibrillation and short accessory pathway effective refractory period (less than 240 ms) as risk factors for sudden cardiac death. Both findings were absent in our patient's evaluation.
Conclusion
What has previously been regarded as an electrocardiographic curiosity5 could have had potentially serious consequences for this patient's livelihood and adversely impacted US Navy submarine force operational readiness. Instead, the electrophysiological study facilitated the diagnosis of FVP, allowed for adequate risk stratification for malignant arrhythmia and sudden cardiac death, and ultimately led to our patient's return to duty.
References
- 1.Manual of the Medical Department, NAVMED P-117. Falls Church, VA: US Navy Bureau of Medicine and Surgery; 2017.
- 2.Hiss R.G., Lamb L.E. Electrocardiographic findings in 122,043 individuals. Circulation. 1962;25:947–961. doi: 10.1161/01.cir.25.6.947. [DOI] [PubMed] [Google Scholar]
- 3.Munger T.M., Packer D.L., Hammill S.C., Feldman B.J., Bailey K.R., Ballard D.J., Holmes D.R., Jr., Gersh B.J. A population study of the natural history of Wolff-Parkinson-White syndrome in Olmsted County, Minnesota, 1953-1989. Circulation. 1993;87:866–873. doi: 10.1161/01.cir.87.3.866. [DOI] [PubMed] [Google Scholar]
- 4.Al-Khatib S.M., Pritchett E.L. Clinical features of Wolff-Parkinson-White syndrome. Am Heart J. 1999;138:403–413. doi: 10.1016/s0002-8703(99)70140-7. [DOI] [PubMed] [Google Scholar]
- 5.Tung R., Sklyar E., Josephson M. An unusual form of preexcitation: fasciculoventricular bypass tract. Heart Rhythm. 2008;5:1767–1768. doi: 10.1016/j.hrthm.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 6.De Ponti R., Salerno-Uriarte J.A. “Mahaim” fasciculoventricular fibers: rare variant of ventricular preexcitation or subtle clinical problem? Heart Rhythm. 2005;2:7–9. doi: 10.1016/j.hrthm.2004.10.036. [DOI] [PubMed] [Google Scholar]
- 7.Hirao K., Otomo K., Wang X., Beckman K.J., McClelland J.H., Widman L., Gonzalez M.D., Arruda M., Nakagawa H., Lazzara R., Jackman W.M. Para-Hisian pacing. A new method for differentiating retrograde conduction over an accessory AV pathway from conduction over the AV node. Circulation. 1996;94:1027–1035. doi: 10.1161/01.cir.94.5.1027. [DOI] [PubMed] [Google Scholar]
- 8.Sternick E.B., Gerken L.M., Vrandecic M.O., Wellens H.J. Fasciculoventricular pathways: clinical and electrophysiologic characteristics of a variant of preexcitation. J Cardiovasc Electrophysiol. 2003;14:1057–1063. doi: 10.1046/j.1540-8167.2003.03206.x. [DOI] [PubMed] [Google Scholar]
- 9.Ratnasamy C., Khan D., Wolff G.S., Young M.L. Clinical and electrophysiological characteristics of fasciculoventricular fibers in children. Int J Cardiol. 2008;123:257–262. doi: 10.1016/j.ijcard.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Gallagher J.J., Smith W.M., Kasell J.H., Benson D.W., Jr., Sterba R., Grant A.O. Role of Mahaim fibers in cardiac arrhythmias in man. Circulation. 1981;64:176–189. doi: 10.1161/01.cir.64.1.176. [DOI] [PubMed] [Google Scholar]
- 11.Abbott J.A., Scheinman M.M., Morady F. Coexistent Mahaim and Kent accessory connections: diagnostic and therapeutic implications. J Am Coll Cardiol. 1987;10:364–372. doi: 10.1016/s0735-1097(87)80020-7. [DOI] [PubMed] [Google Scholar]
- 12.Sternick E.B., Rodriguez L.M., Gerken L.M., Wellens H.J. Electrocardiogram in patients with fasiculoventricular pathways: a comparative study with anteroseptal and midseptal accessory pathways. Heart Rhythm. 2005;2:1–6. doi: 10.1016/j.hrthm.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 13.Josephson M.E. Josephson's Clinical Cardiac Electrophysiology: Techniques and Interpretations. 5th ed. Wolters Kluwer Health; Philadelphia, PA: 2016. Preexcitation syndromes; pp. 434–436. [Google Scholar]
- 14.Ganz L.I., Elson J.J., Chenarides J.G. Preexcitation in a child with syncope: where is the connection? J Cardiovasc Electrophysiol. 1998;9:892–895. doi: 10.1111/j.1540-8167.1998.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 15.Al-Khatib S.M., Arshad A., Balk E.M., Das S.R., Hsu J.C., Joglar J.A., Page R.L. Risk stratification for arrhythmic events in patients with asymptomatic pre-excitation: a systematic review for the 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2016;13:e222–e237. doi: 10.1016/j.hrthm.2015.09.017. [DOI] [PubMed] [Google Scholar]
- 16.Pappone C., Vicedomini G., Manguso F. Wolff-Parkinson-White syndrome in the era of catheter ablation: insights from a registry study of 2169 patients. Circulation. 2014;130:811–819. doi: 10.1161/CIRCULATIONAHA.114.011154. [DOI] [PubMed] [Google Scholar]