Abstract
The current report is the case of a 30-year-old male patient who presented with symptomatology suggestive of appendicitis. However, careful history-taking and laboratory tests led to the diagnosis of Clostridium difficile colitis, resulting in successful nonsurgical management of this patient. Although both appendicitis and C. difficile colitis are common conditions, they are rarely diagnosed concurrently. This is reflected by paucity of literature describing this manifestation. Given this current presentation, the authors contend that the manifestation of extracolonic colitis within the appendix is possibly underdiagnosed or misdiagnosed as an acute appendicitis and thus potentially results in unnecessary surgical intervention. This report reminds physicians to consider the medical approach to managing acute appendicitis given the possibility of underlying C. difficile colitis as the causative factor.
1. Introduction
Acute appendicitis is considered among the most common abdominal surgical emergencies, a condition with an etiology that has yet to be elucidated and is currently considered multifactorial [1, 2]. C. difficile colitis is another common healthcare-associated condition and is a significant cause of morbidity and mortality among older adult hospitalized patients [3]. Appendicitis rarely presents secondary to colitis; indeed, to our knowledge, only three cases of appendicitis induced by C. difficile infection have been reported in the literature [4–6].
2. Case Report
A 30-year-old Hispanic man presented to the emergency department with several episodes of vomiting and nonbloody diarrhea for two days. This was accompanied by generalized abdominal cramps and dizziness. There was no history of recent travel, sick contacts, similar past illness, new foods, or medication changes. He denied fever, chest pain, cough, headache, shortness of breath, palpitations, loss of consciousness, or urinary complaints. Upon further questioning, the patient stated he had taken clindamycin for cellulitis two months priorly. Past medical and family history were noncontributory.
At the emergency department, patient was alert and oriented to person, place, and time and in no acute distress. He was afebrile, blood pressure was 79/50 mm of Hg, and heart rate was 108/minute. Cardiac, pulmonary, and skin examinations were normal. Abdominal examination revealed vague, mild, and diffuse abdominal tenderness on palpation. Bowel sounds were hyperactive and rectal tone was intact. The remainder of his physical examination was negative for other sources of infection.
Initial blood workup included complete blood count and revealed a white blood cell count of 19.2 × 109/L, hemoglobin 14.4 g/dL, hematocrit 41.2%, and platelets 90 × 109/L. A metabolic panel showed BUN 43 mg/dL, creatinine 5.12 mg/dL, AST 103 U/L, ALT 227 U/L, total bilirubin 3.2 mg/dL, and lactate 2.6 mg/dL. Coagulation profile revealed INR 1.2, PTT 37.9 seconds, and PT 14.3 seconds. Blood smear did not reveal schistocytes or fragmented RBCs. He had a normal haptoglobin, LDH, reticulocyte index, and fibrinogen. A sample for stool studies was sent at that time.
Given clinical and laboratory findings suggestive of sepsis, the patient was started on intravenous normal saline, metronidazole, and levofloxacin. He was then admitted under our care to the intensive care unit on that day for close monitoring; we made no subsequent changes in his management. An abdominal computed tomography indicated an enlarged appendix which measured 9.8 mm with periappendiceal inflammation suggestive of acute appendicitis without abscess (Figures 1 and 2). The general surgery service was consulted, who then recommended surgical intervention. As the patient was being prepared for surgery, his stool study polymerase chain reaction results returned as positive for Clostridium difficile toxin (NAP1 strain). The surgical service, therefore, decided that the patient should be continued on medical management, with plans to operate if a localized peritonitis were to develop in this setting. We subsequently obtained a consultation from our infectious disease specialists who added oral vancomycin to the patient's regimen.
Figure 1.

Axial section of abdominal CT scan with contrast demonstrating swollen appendix with 9.8 mm diameter, no appendicolith present.
Figure 2.
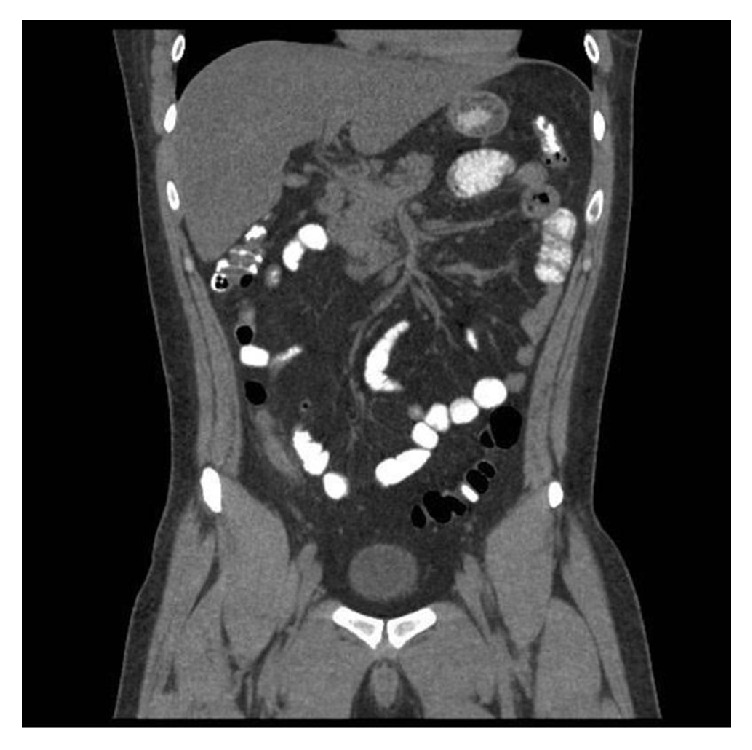
Coronal section of abdominal CT scan with contrast demonstrating swollen appendix with 9.8 mm diameter, no appendicolith present.
The remaining stool studies were negative for ova, parasites, Salmonella, Shigella, Campylobacter jejuni, and Escherichia coli. Workup for other sources of infections, including chest X-ray and blood and urine cultures, were negative. On the following day, the patient's laboratory studies showed significant improvement, and he appeared clinically better. Thus, the patient was transferred to the general medical floor for continued management. He was discharged home, following three days of observation, with instructions to continue oral vancomycin for 6 additional days and follow up with his primary care physician in one week.
3. Discussion
Although Clostridium difficile colitis and appendicitis are each very common independently, C. difficile as an etiology of appendicitis is uncommon. There have been only three reported cases of appendicitis induced by C. difficile infection in the literature [4–6]. Secretory diarrhea and C. difficile colitis are the most common complications for C. difficile toxins A and B after administration of any antimicrobial drug, but especially with ampicillin, cephalosporins, fluoroquinolones, and clindamycin [7]. Reports of extracolonic manifestations of C. difficile include bacteremia, visceral abscess formation (splenic abscess, pancreatic abscess, empyema, and pleural effusion), prosthetic device infections, encephalopathy, reactive arthritis, osteomyelitis, and soft tissue infections [8, 9].
The current report is a very rare case of acute appendicitis as an extracolonic manifestation of C. difficile. Although surgical treatment is often sought for appendicitis, studies have suggested medical treatment may be sufficient (albeit with possibility of recurrence). Moreover, if the etiology of the appendicitis is a treatable infection as in our case, it warrants the consideration of a medical approach; surgery could be scheduled later when the patient is stable. We present this report as a reminder to our physician colleagues to consider C. difficile colitis in their differential diagnosis in a similar clinical scenario.
Disclosure
This is the original work of the named authors.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Authors' Contributions
All the named authors have read and approve of the matter contained within the final draft of this report.
References
- 1.Humes D. J., Simpson J. Acute appendicitis. The British Medical Journal. 2006;333(7567):530–534. doi: 10.1136/bmj.38940.664363.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson J. E., Bickler S. W., Chang D. C., Talamini M. A. Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995-2009. World Journal of Surgery. 2012;36(12):2787–2794. doi: 10.1007/s00268-012-1749-z. [DOI] [PubMed] [Google Scholar]
- 3.Kelly C. P., LaMont J. T. Clostridium difficile—more difficult than ever. The New England Journal of Medicine. 2008;359(18):1932–1940. doi: 10.1056/NEJMra0707500. [DOI] [PubMed] [Google Scholar]
- 4.Coyne J. D., Dervan P. A., Haboubi N. Y. Involvement of the appendix in pseudomembranous colitis. Journal of Clinical Pathology. 1997;50(1):70–71. doi: 10.1136/jcp.50.1.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martirosian G., Bulanda M., Wójcik-Stojek B., et al. Acute appendicitis: the role of enterotoxigenic strains of bacteroides fragilis and clostridium difficile. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 2001;7(3):382–386. [PubMed] [Google Scholar]
- 6.Brown T. A., Rajappannair L., Dalton A. B., Bandi R., Myers J. P., Kefalas C. H. Acute Appendicitis in the Setting of Clostridium difficile Colitis: Case Report and Review of the Literature. Clinical Gastroenterology and Hepatology. 2007;5(8):969–971. doi: 10.1016/j.cgh.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Schroeder M. S. Clostridium dif ficile–associated Diarrhea. American Family Physician. 2005;71(5) http://search.ebscohost.com/login.aspx?direct=true&profile=ehost&scope=site&authtype=crawler&jrnl=0002838X&AN=16683095&h=ICp6j5%2B4hMbB7ovQxJa51mcJSJQBvMaa6cy1MG0tUU7mo77KNWC5Bd2iupLEVeoUG%2BHNsPZUu%2Fb4eEuTvZyWKA%3D%3D&crl=c. [PubMed] [Google Scholar]
- 8.Mattila E., Arkkila P., Mattila P. S., Tarkka E., Tissari P., Anttila V.-J. Extraintestinal clostridium difficile infections. Clinical Infectious Diseases. 2013;57(6):e148–e153. doi: 10.1093/cid/cit392. [DOI] [PubMed] [Google Scholar]
- 9.García-Lechuz J. M., Hernangómez S., San Juan R., Peláez T., Alcalá L., Bouza E. Extra-intestinal infections caused by Clostridium difficile. Clinical Microbiology and Infection. 2001;7(8):453–457. doi: 10.1046/j.1469-0691.2001.00313.x. [DOI] [PubMed] [Google Scholar]


