Abstract
Purpose
To determine whether there are in vivo differences of γ-aminobutyric acid (GABA) levels in frontal and parietal regions of Alzheimer’s disease (AD) patients, compared with healthy controls using magnetic resonance spectroscopy (1H-MRS).
Materials and Methods
Fifteen AD patients and fifteen age- and gender-matched healthy controls underwent 1H-MRS of the frontal and parietal lobes using the “MEGA-Point Resolved Spectroscopy Sequence” (MEGA-PRESS) technique, and cognitive levels of subjects were evaluated using Mini-Mental State Examination (MMSE) tests. MRS data were processed using the Gannet program. Because the signal detected by MEGA-PRESS includes contributions from GABA, macromolecules and homocarnosine, it is labeled as “GABA+” rather than GABA. Differences of GABA+/Cr ratios between AD patients and controls were tested using covariance analysis, adjusting for gray matter fraction. The relationship between GABA+/Cr and MMSE scores was also analyzed.
Results
Significant lower GABA+/Cr ratios were found in the parietal region of AD patients compared with controls (P = 0.041). In AD patients, no significant correlations between GABA+/Cr and MMSE scores were found in either the frontal (r = −0.164; P = 0.558) or parietal regions (r = 0.025; P = 0.929).
Conclusion
Decreased GABA+/Cr levels were present in the parietal region of patients with AD in vivo, suggesting that abnormalities of the GABAergic system may be present in the pathogenesis of AD.
Keywords: Alzheimer’s disease, GABA, 1H-MRS, MMSE, MEGA-PRESS
Alzheimer’s Disease (AD) is a progressive neuro-degenerative disorder, characterized by behavioral abnormalities and cognitive deficits. Increasing evidence suggests that inhibitory neurotransmitter system dysfunction may be involved in AD (1). γ-Aminobutyric acid (GABA) is the predominant inhibitory neurotransmitter in the human brain (2), and is considered to be associated with cognitive function (1). A variety of studies, including postmortem (3), neuroimaging (4), and animal model systems (5), have suggested that GABAergic dysfunction is involved in AD.
MRS enables the noninvasive in vivo measurement of major neurometabolite levels in various neurodege-nerative diseases (6). However, the accuracy of conventional in vivo 1H-MR spectroscopy for the measurement of GABA measurement is limited by its relatively low concentration, and spectral overlap with the signals of glutamate (Glu), N-acetylaspartate (NAA), total creatine (Cr), and macromolecules (MM). With the development of edited MRS methods, however, such as MEGA-Point Resolved Spectroscopy method (MEGA-PRESS), brain GABA levels may be more reliably estimated (7), and has been measured both in normal human brain (8) and in various psychiatric diseases (9).
Moreover, the relationship between brain metabolites levels and cognitive impairment remains poorly explored. Although the correlation between NAA and Mini-Mental State Examination (MMSE) scores has been reported (10), the relationship between GABA level and cognitive impairments remains unknown.
In this initial study, the edited MRS technique MEGA-PRESS was used to explore in vivo brain GABA levels in patients with AD, and age- and gender-matched healthy control subjects. The assessment of the relationship between GABA levels and cognitive impairments in AD patients were also performed.
MATERIALS AND METHODS
Subjects
Fifteen patients with clinical diagnosis of AD (9 women and 6 men aged 55–79 years, mean = 65.73 ± 8.53 years) and 15 age- and gender-matched healthy control subjects (HC) (8 women and 7 men aged 61–76 years, mean = 66.33 ± 4.62 years) were recruited in this study (Table 1). AD patients were diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR Fourth Edition (DSM-IV) (11), the National Institute of Neurological and Communicative Disorders and the Alzheimer’s Disease and Related Disorders Association criteria (NINDS-ADRDA) (12). To obtain an overall assessment of cognitive function, all subjects were administered the MMSE (13) by a trained neuro-psychologist, blinded to the MRI data, on the same day of the MR examination. Exclusion criteria included: (i) a history of a severe brain trauma or psychiatric disease; (ii) intake of medication that may affect cognitive function, e.g., donepezil, memantine; (iii) major ischemic vascular damage, e.g., cerebral ischemic stroke; or (iv) subcortical arteriosclerotic encephalopathy, leukoaraiosis, as diagnosed by conventional brain MRI. The age- and gender-matched control subjects had no history of cognitive decline, previous neurologic or psychiatric disorder. Local Ethical Committee approval and written informed consent from all the subjects and their guardians were obtained before study initiation.
Table 1.
Demographic, MRS, and Segmentation Dataa of AD Patients and Control Subjects
| AD | HC | P valueb | |
|---|---|---|---|
| Number | 15 | 15 | – |
| Age | 65.73 ± 8.53y | 66.33 ± 4.62y | 0.81 |
| Female, no. (%) | 9 (60.00%) | 8 (57.33%) | 0.724 |
| Age of onset | 64.07 ± 9.38y | – | – |
| Duration of illness | 2.27 ± 1.01y | – | – |
| MMSE | 15.87 ± 5.03 | 29.20 ± 0.86 | <0.001 |
| Frontal region: | |||
| GABA+/Cr level | 0.098 ± 0.008 | 0.104 ± 0.022 | 0.345 |
| GABA+ FitError | 7.04% ± 1.61% | 5.60% ± 1.20% | 0.151 |
| GM/(GM+WM) | 55.30% ± 5.29% | 56.94% ± 1.34% | 0.26 |
| Parietal region: | |||
| GABA+/Cr level | 0.086 ± 0.016 | 0.099 ± 0.012 | 0.041 |
| GABA+ FitError | 6.11% ± 1.84% | 5.51% ± 2.42% | 0.900 |
| GM/(GM+WM) | 54.69% ± 5.70% | 57.61% ± 2.00% | 0.07 |
AD = Alzheimer’s disease; HC = healthy controls; MMSE = Mini-Mental State Examination; GM = gray matter; WM = white matter.
Data are given as mean ± standard deviation (SD).
Significant differences between groups are tested by analysis of covariance with P <0.05 accepted as significant.
MRI/MRS Study Protocol
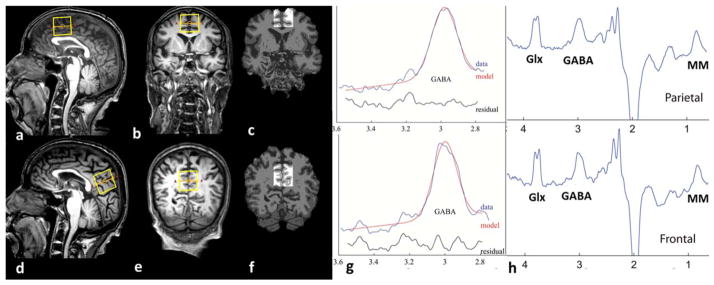
All MRI/MRS experiments were performed on a 3 Tesla (T) scanner (Philips Achieva TX, Best, The Netherlands) equipped with an eight-channel phased-array head coil. Before the MRS examination, T1-weighted three-dimensional (3D) turbo field echo (TFE) images were used for localization, with major parameters as follows: TR = 8.2 ms; TE = 3.7 ms; slice thickness = 1 mm; resolution = 256 × 256; FOV = 24×24 cm2; and flip angle = 8°. The MRS voxels (volume size 3 × 3 × 3 cm3) were set on medial frontal region and the parietal region (Fig. 1). These regions were chosen because they were large enough to accommodate the 27 cm3 voxel, and prior postmortem studies have suggested GABAergic dysfunction in frontal, parietal (and temporal) regions (1). The median sagittal plane was selected as a reference slice for voxel localization: the voxel in the frontal region was prescribed superior to the genu of the corpus callosum, aligned with the shape of the corpus callosum, and positioned on the medial aspect of the axial plane; the voxel in the parietal region was prescribed posterior and superior to the splenium of the corpus callosum, aligned with the shape of the corpus callosum, and positioned again on the medial aspect of the axial plane. All of the voxels were positioned in a manner to avoid the lateral ventricle and skull.
Figure 1.
The position of voxels, corresponding segmentation data and representative spectra. The (a,d) and (b,e) panels show the position of volumes of interest in frontal (upper) and parietal regions (lower) on sagittal and coronal T1-weighted TFE images in an AD patient. The corresponding results of brain segmentation are shown in the frontal (c) and parietal regions (f). (g, h) Show the representative MEGA-PRESS spectra processed using the “Gannet 2.0” toolkit in frontal and parietal regions of AD. (g) Shows the curve-fitting of the GABA peak using Gannet, the red lines in the panels are the results of the GannetFit curve-fitting, the blue lines show the postphase and frequency aligned GABA data, and the black line is the residual difference between the experimental data and the curve-fit. (h) is the MEGA-PRESS difference spectrum. The Glx, GABA and MM peaks resonate at 3.7, 3.0 ppm and 0.9 ppm respectively.
1H-MRS
The MEGA-PRESS sequence (7) was used for GABA editing, with the parameters as follows: TR = 2000 ms; TE = 68 ms; 320 signal averages; acquisition bandwidth = 1000 Hz; scan duration 13 min. J-evolution for GABA was refocused during odd-numbered acquisitions (ON) but not during even-numbered acquisitions (OFF) by applying Gaussian inversion pulse to the 3CH2 resonance of GABA at 1.9 ppm (ON) and symmetrically about the water peak at 7.5 ppm (OFF), respectively. Water suppression was carried out using chemical shift-selective (CHESS) pulses after automatic optimization. FASTMAP shimming of the VOI was conducted automatically before each acquisition.
The difference of the “ON” and “OFF” spectra provided an edited spectrum of GABA. The signal detected at 3.02 ppm with these parameters and the MEGA-PRESS technique is known to contain contributions from both macromolecules (MM) and homocarnosine (14), hence, the detected signal is referred to as GABA+ rather than GABA. Quantification was performed using the Gannet 2.0 toolkit, a Matlab-based quantitative batch analysis tool for analyzing GABA MEGA-PRESS spectra (15). Gannet contains two modules: GannetLoad and GannetFit. The GannetLoad module is used to parse certain variables from the data headers, apply a line broadening of 3 Hz, and frequency and phase correct the individual spectra using Spectral Registration (16). GannetFit uses a single-Gaussian model to fit the edited GABA+ signal and evaluates GABA+ relative to creatine (Cr), which has been reported to be unchanged in AD in previous studies (17,18). In this manuscript, the GABA+/Cr ratio is referred to as GABA+ level. GannetFit also provides the standard deviation of the fitting residual divided by the amplitude of the fitted peaks, generating the overall FitError which reflects the signal-to-noise ratio. Only spectra with a relative FitError of GABA+ below 10% were used for the statistical analysis.
VOI Segmentation
Different voxel proportions of gray matter (GM), white matter (WM), and cerebrospinal fluid (CSF) in 1H-MRS may confound group differences in metabolite measurement. To determine if tissue composition differences, between AD subjects and healthy controls, could account for differences in GABA+ level, each MRS voxel was segmented as GM, WM, or CSF using the 3D T1-weighted brain images and the automatic brain segmentation program (Fig. 1), FAST (FMRIB’s automated segmentation tool) in the FSL package (Oxford University, Oxford, UK) (19). The VOIs were co-registered to the anatomical images using the “Re-creation of VOI” Matlab tool (20). Tissue GM fractions were obtained by calculating the ratio of GM volume to the GM+WM volumes in the VOIs. The concentrations of GABA and Cr in CSF were considered to be negligible.
Statistical Analysis
Statistical analyses were conducted using the Statistical Package for Social Sciences software (SPSS 17.0, Chicago, IL). MRS data were presented as mean ± standard deviation (SD) values. The differences of GABA+ levels between patients and controls were tested using analysis of covariance (ANCOVA), adjusting for GM/(GM+WM). Spearman correlation coefficients were used to assess the presence of linear associations between GABA+ levels and MMSE scores. P-values of less than 0.05 were considered as significant.
RESULTS
The Demographic Characteristics of Study Subjects
The demographic information and the results of memory test of the subjects are presented in Table 1. There was no difference in age (P = 0.812) and gender distribution (P = 0.724) between the two groups. The AD patients (range, 10–23; mean = 15.9 ± 5.0) performed significantly worse on the MMSE than controls (range, 28–30; mean = 29.2 ± 0.9) (P <0.001).
VOI Segmental Results
The mean GM tissue fraction GM/(GM +WM) was 55.3% and 54.7% in the frontal and parietal regions, respectively, in AD patients, and 56.9% and 57.6%, respectively, in HC (Table 1). There were no significant differences in GM fraction in the VOIs between AD patients and HC (frontal region, p = 0.254; parietal region, p = 0.072).
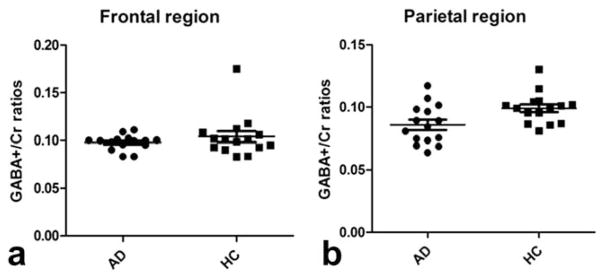
Comparisons of GABA+ Level Between Groups (AD Patients versus Control Subjects)
Edited spectra were successfully obtained from the frontal and parietal regions in all 15 AD patients and 15 controls (Fig. 2), with mean GABA+ FitError of frontal and parietal voxels 7.0% and 5.6%, respectively, for AD patients, 6.1% and 5.5% for HC (Table 1). A significantly lower GABA+ level was found in parietal region of AD patients, relative to controls (P = 0.041). Lower mean GABA+ levels were also found in the frontal region (0.098 ± 0.008), compared with HC (0.104 ± 0.022), but this was not statistically significant (P = 0.345). (Table 1; Fig. 2).
Figure 2.
The GABA+/Cr ratios of AD patients and HC in frontal (a) and parietal (b) regions. The mean and standard deviation of GABA+/Cr ratios are displayed. a: Shows that the mean GABA+/Cr ratios are lower in AD than in HC in frontal region (P = 0.345), but no statistical difference is detected. There does appear to be one “outlier” value in the control group, however, no significant differences are found in this region between AD and HC, whether this point is included or not. b: Shows GABA+/Cr ratios of AD group are significantly decreased in the parietal region (P = 0.041).
Correlation of GABA+ Levels With Cognitive Function
MMSE scores were evaluated in all subjects. No significant correlations were found between MMSE and GABA+ levels, either in frontal (r = −0.164, P = 0.558) or parietal voxels (r = −0.025, P = 0.929). Also, with regard to the correlation of MMSE scores and GABA+ levels in healthy controls, no statistical correlation was detected (frontal region: r = 0.178, P = 0.526; parietal region: r = −0.197, P = 0.481).
DISCUSSION
The main result of this study is that significantly decreased GABA+ levels were present in the parietal region of AD patients, as compared to age- and gender-matched healthy controls. The mean GABA+ levels in the frontal region also showed a trend (not statistically significant) to be lower in AD than HC. To the best of our knowledge, this is the first in vivo demonstration of reduced GABA+ levels in AD patients. Because GABA is primarily localized to inhibitory neurons (21), GABA+ level deficits could indicate either loss or dysfunction of GABAergic neurons in AD. These findings are consistent with previous postmortem studies, which observed decreased GABA levels in temporal, parietal, occipital and frontal cortex in AD samples (3,22–24). Similar findings have also been reported in animal model studies: a transgenic AD rat model study found lower GABA levels in dorsal hippocampus and frontal cortex at age 9 months (25), and an MRS study of mouse AD model (5xFAD) also found decreased GABA levels at age 40 months (26).
As stated above, the GABA deficit may be due to either GABAergic neuronal loss or dysfunction; if due to dysfunction, either GABA synthesis itself or enzymatic deficiency in glutamate-glutamine cycling may be implicated (27). A study of the TgCRND8 AD mouse model found lower glutamate decarboxylase (GAD67 -the enzyme that catalyses the conversion of glutamate to GABA) in the hippocampus, and suggested that amyloid-βtoxicity contribute to the GABA neuron dysfunction, followed at later stages by cell death (28). Single photon emission computed tomography (SPECT) studies have also demonstrated reduced GABAA/benzodiazepine (BZD) receptor density in the frontal and parietotemporal lobes of patients with AD, and in the parietal lobe of patients with mild cognitive impairment (MCI) (29,30). GABA-A subunit studies found that, in the hippocampus, mRNA for GABA-A subunits α1, α5, β3 were decreased in AD patients with severe neuropathology (31) and α1, α2 GABA-A subunit expression was reduced in early and late AD stages (32).
Because the results of this and prior studies suggest that the GABAergic system is involved in the pathogenesis of AD, it is, therefore, also a potential a target for AD therapies. Of interest, it was found that the administration of a GABA-chloride ionophore antagonist to aging rats could protect the animals from age-related decline in cognitive functions, and losses of hippocampal neurons (5), suggesting that the GABAergic systems does contribute to cognitive dysfunction in AD and may be amenable to prophylactic treatments. However, the current study and a previous SPECT study on GABAA/BZD receptors in AD found no significant correlation between MMSE scores and GABAA/BZD receptor availability in any brain regions tested (30). The lack of correlation between MMSE and regional GABA+ levels may be due in part to the limited sample size, and a follow-up study in a larger cohort of AD patients will be required to answer this question definitively.
Limitations
The data acquisition strategy for this study has several limitations. First, as in most GABA MRS studies, the voxel volume used was relatively large (3 × 3 × 3 cm) due to the low intensity of the GABA+ signal. A smaller-VOI MRS approach may prove more efficient for region-specific analyses of brain GABA levels. Second, the MEGA-PRESS technique as implemented here at 3T, in addition to editing GABA, also contains contributions from co-edited macromolecules (MM), as well as a smaller contribution from the GABA-dipeptide homocarnosine. New methods for macromolecule suppression are being developed (33) which can detect “pure GABA,” and these methods should be used in future studies of AD. On the other hand, the concentration of homocarnosine in vivo is much lower than that of GABA (34), so isolated changes in homocarnosine are less likely to be driving the observed changes. Third, the study acquisition protocol did not include acquisition of nonsuppressed water scans, which precluded the calculation of GABA+ concentrations relative to the brain water signal. The results presented here are given as ratios to Cr, meaning that we were only able to present metabolite ratios. However, quantification relative to Cr is likely to be more robust (than water referencing) to possible group differences in brain water content and CSF due to atrophy (17,18). Fourth, the sample size of 15 in each group is rather small for a clinical study of this kind, and, therefore, these results should be viewed as preliminary, and will require confirmation in larger numbers of subjects. It is possible that the lack of an observed difference in the frontal region is more due to insufficient power (from a combination of sample size and high variance among controls) than any true regional difference.
Finally, although many prior MRS studies on AD have focused on the hippocampal region because of its important role in AD pathology, in this study the hippocampus was not studied. Because of the low concentration of GABA in the brain, the VOI of MEGA-PRESS technique is relatively large (3 × 3 × 3 cm3), much larger than the hippocampus itself, and would, therefore, have a considerable amount of partial volume with surrounding tissues. Additionally, hippocampal atrophy is a nearly ubiquitous finding in AD (35–37). The proportions of gray matter and white matter differ between AD patients and healthy controls, which may confound the results of GABA level alterations. As mentioned above, the MEGA-PRESS voxels were placed on the medial frontal and the parietal regions instead of the hippocampus region.
In conclusion, decreased GABA+ levels, as measured by edited MRS, were found in the parietal region of AD patients compared with age-matched controls. These in vivo results add to previous in vitro and animal model studies which suggest GABAergic system dysfunction in AD pathogenesis, as well as a potential treatment target for AD. More studies in larger numbers of patients, preferably using MM-suppression techniques, are required to probe the relation between regional GABA levels and cognitive impairment.
Acknowledgments
The authors thank the patients and healthy participants who volunteered for this study.
Contract grant sponsor: The National Natural Science Foundation of China; Contract grant number: 81171380/H1807.
References
- 1.Lanctot KL, Herrmann N, Mazzotta P, Khan LR, Ingber N. GABAergic function in Alzheimer’s disease: evidence for dysfunction and potential as a therapeutic target for the treatment of behavioural and psychological symptoms of dementia. Can J Psychiatry. 2004;49:439–453. doi: 10.1177/070674370404900705. [DOI] [PubMed] [Google Scholar]
- 2.Obata K. Synaptic inhibition and gamma-aminobutyric acid in the mammalian central nervous system. Proc Jpn Acad Ser B Phys Biol Sci. 2013;89:139–156. doi: 10.2183/pjab.89.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seidl R, Cairns N, Singewald N, Kaehler ST, Lubec G. Differences between GABA levels in Alzheimer’s disease and Down syndrome with Alzheimer-like neuropathology. Naunyn Schmiedebergs Arch Pharmacol. 2001;363:139–145. doi: 10.1007/s002100000346. [DOI] [PubMed] [Google Scholar]
- 4.Ball S, Busatto GF, David AS, et al. Cognitive functioning and GABAA/benzodiazepine receptor binding in schizophrenia: a 123I-iomazenil SPET study. Biol Psychiatry. 1998;43:107–117. doi: 10.1016/s0006-3223(97)00300-4. [DOI] [PubMed] [Google Scholar]
- 5.Marczynski TJ. GABAergic deafferentation hypothesis of brain aging and Alzheimer’s disease revisited. Brain Res Bull. 1998;45:341–379. doi: 10.1016/s0361-9230(97)00347-x. [DOI] [PubMed] [Google Scholar]
- 6.Bartha R, Smith M, Rupsingh R, Rylett J, Wells JL, Borrie MJ. High field (1)H MRS of the hippocampus after donepezil treatment in Alzheimer disease. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:786–793. doi: 10.1016/j.pnpbp.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Mescher M, Merkle H, Kirsch J, Garwood M, Gruetter R. Simultaneous in vivo spectral editing and water suppression. NMR Biomed. 1998;11:266–272. doi: 10.1002/(sici)1099-1492(199810)11:6<266::aid-nbm530>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 8.Choi IY, Lee SP, Merkle H, Shen J. In vivo detection of gray and white matter differences in GABA concentration in the human brain. Neuroimage. 2006;33:85–93. doi: 10.1016/j.neuroimage.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 9.Yoon JH, Maddock RJ, Rokem A, et al. GABA concentration is reduced in visual cortex in schizophrenia and correlates with orientation-specific surround suppression. J Neurosci. 2010;30:3777–3781. doi: 10.1523/JNEUROSCI.6158-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang W, Alexander GE, Chang L, et al. Brain metabolite concentration and dementia severity in Alzheimer’s disease: a (1)H MRS study. Neurology. 2001;57:626–632. doi: 10.1212/wnl.57.4.626. [DOI] [PubMed] [Google Scholar]
- 11.Gmitrowicz A, Kucharska A. Developmental disorders in the fourth edition of the American classification: diagnostic and statistical manual of mental disorders (DSM IV – optional book) Psychiatr Pol. 1994;28:509–521. [PubMed] [Google Scholar]
- 12.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 13.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 14.Rothman DL, Behar KL, Prichard JW, Petroff OA. Homocarnosine and the measurement of neuronal pH in patients with epilepsy. Magn Reson Med. 1997;38:924–929. doi: 10.1002/mrm.1910380611. [DOI] [PubMed] [Google Scholar]
- 15.Edden RAE, Puts NA, Harris AD, Barker PB, Evans CJ. Gannet: a batch-processing tool for the quantitative analysis of GABA-edited MRS spectra. J Magn Reson Imaging. 2013 doi: 10.1002/jmri.24478. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Near J, Edden R, Evans CJ, Paquin R, Harris A, Jezzard P. Frequency and phase drift correction of magnetic resonance spectroscopy data by spectral registration in the time domain. Magn Reson Med. 2014 doi: 10.1002/mrm.25094. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graff-Radford J, Kantarci K. Magnetic resonance spectroscopy in Alzheimer’s disease. Neuropsychiatr Dis Treat. 2013;9:687–696. doi: 10.2147/NDT.S35440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valenzuela MJ, Sachdev P. Magnetic resonance spectroscopy in AD. Neurology. 2001;56:592–598. doi: 10.1212/wnl.56.5.592. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Y, Brady M, Smith S. Segmentation of brain MR images through a hidden Markov random field model and the expectation-maximization algorithm. IEEE Trans Med Imaging. 2001;20:45–57. doi: 10.1109/42.906424. [DOI] [PubMed] [Google Scholar]
- 20.Roebuck JR, Windham JP, Hearshen DO. Segmentation of MRS signals using ASPECT (analysis of SPectra using Eigenvector Decomposition of Targets) Med Phys. 1994;21:277–285. doi: 10.1118/1.597289. [DOI] [PubMed] [Google Scholar]
- 21.Kelsom C, Lu W. Development and specification of GABAergic cortical interneurons. Cell Biosci. 2013;3:19. doi: 10.1186/2045-3701-3-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lowe SL, Francis PT, Procter AW, Palmer AM, Davison AN, Bowen DM. Gamma-aminobutyric acid concentration in brain tissue at two stages of Alzheimer’s disease. Brain. 1988;111:785–799. doi: 10.1093/brain/111.4.785. [DOI] [PubMed] [Google Scholar]
- 23.Sasaki H, Muramoto O, Kanazawa I, Arai H, Kosaka K, Iizuka R. Regional distribution of amino acid transmitters in postmortem brains of presenile and senile dementia of Alzheimer type. Ann Neurol. 1986;19:263–269. doi: 10.1002/ana.410190307. [DOI] [PubMed] [Google Scholar]
- 24.Ellison DW, Beal MF, Mazurek MF, Bird ED, Martin JB. A postmortem study of amino acid neurotransmitters in Alzheimer’s disease. Ann Neurol. 1986;20:616–621. doi: 10.1002/ana.410200510. [DOI] [PubMed] [Google Scholar]
- 25.Nilsen LH, Melo TM, Saether O, Witter MP, Sonnewald U. Altered neurochemical profile in the McGill-R-Thy1-APP rat model of Alzheimer’s disease: a longitudinal in vivo 1 H MRS study. J Neurochem. 2012;123:532–541. doi: 10.1111/jnc.12003. [DOI] [PubMed] [Google Scholar]
- 26.Mlynarik V, Cacquevel M, Sun-Reimer L, et al. Proton and phosphorus magnetic resonance spectroscopy of a mouse model of Alzheimer’s disease. J Alzheimers Dis. 2012;31:S87–S99. doi: 10.3233/JAD-2012-112072. [DOI] [PubMed] [Google Scholar]
- 27.Kugler P. Enzymes involved in glutamatergic and GABAergic neurotransmission. Int Rev Cytol. 1993;147:285–336. doi: 10.1016/s0074-7696(08)60771-8. [DOI] [PubMed] [Google Scholar]
- 28.Krantic S, Isorce N, Mechawar N, et al. Hippocampal GABAergic neurons are susceptible to amyloid-beta toxicity in vitro and are decreased in number in the Alzheimer’s disease TgCRND8 mouse model. J Alzheimers Dis. 2012;29:293–308. doi: 10.3233/JAD-2011-110830. [DOI] [PubMed] [Google Scholar]
- 29.Hanyu H, Kume K, Sato T, et al. Regional differences in cortical benzodiazepine receptors of Alzheimer, vascular, and mixed dementia patients. J Neurol Sci. 2012;323:71–76. doi: 10.1016/j.jns.2012.08.013. [DOI] [PubMed] [Google Scholar]
- 30.Pappata S, Varrone A, Vicidomini C, et al. SPECT imaging of GABA(A)/benzodiazepine receptors and cerebral perfusion in mild cognitive impairment. Eur J Nucl Med Mol Imaging. 2010;37:1156–1163. doi: 10.1007/s00259-010-1409-1. [DOI] [PubMed] [Google Scholar]
- 31.Rissman RA, De Blas AL, Armstrong DM. GABA(A) receptors in aging and Alzheimer’s disease. J Neurochem. 2007;103:1285–1292. doi: 10.1111/j.1471-4159.2007.04832.x. [DOI] [PubMed] [Google Scholar]
- 32.Luchetti S, Bossers K, Van de Bilt S, et al. Neurosteroid biosynthetic pathways changes in prefrontal cortex in Alzheimer’s disease. Neurobiol Aging. 2011;32:1964–1976. doi: 10.1016/j.neurobiolaging.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 33.Edden RA, Puts NA, Barker PB. Macromolecule-suppressed GABA-edited magnetic resonance spectroscopy at 3T. Magn Reson Med. 2012;68:657–661. doi: 10.1002/mrm.24391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Govindaraju V, Young K, Maudsley AA. Proton NMR chemical shifts and coupling constants for brain metabolites. NMR Biomed. 2000;13:129–153. doi: 10.1002/1099-1492(200005)13:3<129::aid-nbm619>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 35.Clerx L, van Rossum IA, Burns L, et al. Measurements of medial temporal lobe atrophy for prediction of Alzheimer’s disease in subjects with mild cognitive impairment. Neurobiol Aging. 2013;34:2003–2013. doi: 10.1016/j.neurobiolaging.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 36.Oosterman JM, Oosterveld S, Rikkert MG, Claassen JA, Kessels RP. Medial temporal lobe atrophy relates to executive dysfunction in Alzheimer’s disease. Int Psychogeriatr. 2012;24:1474–1482. doi: 10.1017/S1041610212000506. [DOI] [PubMed] [Google Scholar]
- 37.Visser PJ, Verhey FR, Hofman PA, Scheltens P, Jolles J. Medial temporal lobe atrophy predicts Alzheimer’s disease in patients with minor cognitive impairment. J Neurol Neurosurg Psychiatry. 2002;72:491–497. doi: 10.1136/jnnp.72.4.491. [DOI] [PMC free article] [PubMed] [Google Scholar]