Abstract
Purpose
To assess the relationship between SDOCT features and functional outcomes for diabetic macular edema (DME) undergoing treatment with intravitreal bevacizumab.
Methods
IRB-approved retrospective consecutive case series of eyes receiving intravitreal bevacizumab (1.25 mg) for DME. SDOCT features were evaluated and correlated with functional response to anti-VEGF therapy.
Results
One hundred fifty-nine eyes of 159 subjects were included in this study. Mean visual acuity improved from 20/76 to 20/58. The proportion of eyes with 20/40 or greater visual acuity increased with treatment (35% at initial visit, 51% at final visit). SDOCT factors that were associated with functional outcomes to anti-VEGF therapy include ellipsoid zone integrity and severity of intraretinal fluid.
Conclusions
SDOCT features appear to provide important markers for functional response to anti-VEGF therapy in DME.
Keywords: diabetic macular edema, anti VEGF, bevacizumab, OCT, SDOCT, retinal architecture
Introduction
Diabetic retinopathy is among the leading causes of significant visual impairment in the working-age adult population.1 Diabetic macular edema (DME) is the most frequent cause of vision loss in diabetic retinopathy.2 Recently, anti-VEGF therapy has been established as a first-line therapy for DME. The overall efficacy of anti-VEGF therapy for both anatomic and functional improvement has been established in multiple studies. 3,4,6-12 Although studies have shown clear improvement in macular edema on OCT, a disconnect still remains in some patients who demonstrate anatomic improvement in macular edema but do not demonstrate a concordant functional response.7,13,14
The purpose of this study is to evaluate the longitudinal SDOCT dynamics that occur during anti-VEGF therapy and to evaluate how these features are associated with functional response to anti-VEGF therapy.
Patients and Methods
Study population
This is a Cleveland Clinic IRB-approved, retrospective consecutive case series of eyes with DME undergoing treatment with intravitreal off-label bevacizumab (1.25 mg, Genentech, San Francisco, CA). Inclusion criteria for this study included clinical diagnosis of diabetic retinopathy, center-involving DME based on SDOCT, treatment of DME with intravitreal bevacizumab, and a minimum 12-week follow-up. Exclusion criteria included any of the following within 3 months of initiation of bevacizumab therapy: intraocular surgery, intravitreal steroid, or laser photocoagulation (i.e., panretinal photocoagulation, macular grid/focal photocoagulation). Additional exclusion criteria included the presence of significant media opacity (e.g., significant cataract, vitreous hemorrhage, corneal scar), presence of co-existing macular disease (e.g., age-related macular degeneration, vascular occlusive disease), previous treatment with alternative anti-VEGF therapy, macular ischemia based on fluorescein angiography, and previous vitreoretinal surgery. If both eyes were receiving anti-VEGF therapy, one eye was selected for study inclusion. Clinical variables were collected including visual acuity, intraocular pressure, and procedure-related complications. Designated time points included baseline, 3-months, 6-months and final follow-up. Snellen VA was converted to logMAR notation for statistical analysis.
Definition and Management of DME
Center-involving DME was defined as foveal-involving fluid on SDOCT in association with the clinical diagnosis of diabetic retinopathy. All patients underwent a minimum of 1 intravitreal injection of 1.25 mg bevacizumab. Patients were treated with a pro re nata (PRN) protocol based on the presence of center-involving DME. As this was a retrospective study, predefined retreatment criteria was not possible. However, in accordance with the standard practice of the clinicians involved in the study, retreatment was performed based on SDOCT criteria of persistent or recurrent fovea-involving intraretinal fluid. Foveal involving intraretinal fluid would be typically observed if the visual acuity was 20/20 and the patient was asymptomatic. Subjects were typically followed every 4-8 weeks based on the treating physician's discretion.
SDOCT qualitative analysis
SDOCT (Cirrus, Carl Zeiss Meditec, Oberkochen, Germany) scans were performed and were reviewed for each timepoint in a masked fashion. Each scan was reviewed for multiple variables, including central subfield thickness (CST), macular volume (MV), posterior vitreous separation (PVS), epiretinal membrane (ERM), intraretinal fluid (IRF), subretinal fluid (SRF) and ellipsoid zone (EZ) integrity. Variables with additional classification included ERM, IRF, and EZ integrity. ERM was graded as foveal or extrafoveal. IRF was classified by severity as absent, mild-moderate or severe. Severe IRF was defined as IRF throughout greater or equal to 50% of the linear scan of the horizontal raster scan of the fovea. EZ integrity was graded as intact, partial disruption, moderate disruption, or severe disruption. Similar to IRF, EZ integrity was graded on the horizontal raster scan of the fovea. A partially disrupted EZ was defined as a weak reflectivity band. Moderate disruption involved EZ signal loss at fovea but was present elsewhere in the scan. Severe disruption of the EZ was defined as loss of the signal along the entire scan.
Statistical analysis
In order to assess the potential differences in SDOCT findings, those eyes with dramatic response to anti-VEGF therapy (e.g., gaining 3 lines or more of vision, losing 3 lines or more of vision) were compared for SDOCT parameters. In addition, those eyes with more moderate changes (1 line or more of loss or gain) were also compared for SDOCT parameters. To compare two groups, Student t-test was used with parametric distribution data. Mann-Whitney U and Chi-square test was also utilized to compare two groups with nonparametric data. Pearson's correlation coefficient test was used to assess the relationship between visual acuity change and OCT parameters and findings. The data were analyzed with Minitab 17 Statistical Software (State College, PA: Minitab, Inc., 2010). A p-value less than 0.05 was considered statistically significant.
Results
Clinical Overview of Eyes with Diabetic Macular Edema
A total of 159 eyes of 159 patients were included in this study. The patient characteristics are found in Table 1. Of those 159 patients, 92 (58%) were male, and 67 (42%) were female. The mean age was 62.7 ± 11.4 years and mean duration of DM was 12.6 ± 8.4 years. Initial mean VA was 20/76 (logMAR units; 0.58 ± 0.41) with 56 eyes (35%) at 20/40 or better. Final VA was 20/58 (logMAR units; 0.46 ± 0.44). Eighty-one eyes (51%) were at 20/40 or better VA at final visit. Fifty eyes (31%) gained 3-line or greater vision improvement and 15 eyes (9%) experienced a 3-line or greater vision loss. The mean number of intravitreal anti-VEGF injections received was 6.1 ± 3.4. The mean follow-up was 16.7 ± 8.6 month.
Table 1. Clinical Demographics.
| Clinical Demographics | |
|---|---|
|
| |
| Number Eyes (Cases) | 159 (159) |
| Age (mean ± SD) | 62.7 ± 11.4 |
| Gender (Male / Female) | 92 / 67 |
| Duration of DM (year) | 12.6 ± 8.4 |
| Lens Status (Phakic / IOL) | 106 / 53 |
| Diabetic Retinopathy Status (NPDR / PDR) | 97 / 62 |
| Number of Injections | 6.1 ± 3.4 |
| Baseline BCVA 20/40 or better (Number / %) | 56 / 35% |
SD: standard deviation; DM: diabetes mellitus; IOL: intraocular lens; NPDR: nonproliferative diabetic retinopathy; PDR: proliferative diabetic retinopathy; BCVA: best-corrected visual acuity
Qualitative SDOCT Features
At baseline, 75 of 159 eyes (46%) were identified to have a PVS. At final follow-up, the presence of a PVS was noted 97 eyes (61%, p = 0.00035). An ERM was present in 30 eyes (19%) at baseline, and at final follow-up increased to 43 eyes (27%, p = 0.02). At baseline, 43 eyes (27%) had subretinal fluid (SRF) and 149 eyes (95%) had intraretinal fluid (IRF). At final visit, 11 eyes (7%) had SRF and 146 eyes (92%) showed IRF (P < 0.0001, 0.39, respectively). EZ disruption of any level was detected in 126 eyes (80%) at baseline and 113 eyes (71%) at final follow-up (p = 0.023).
OCT Features and Visual Gain and Loss with Anti-VEGF Therapy
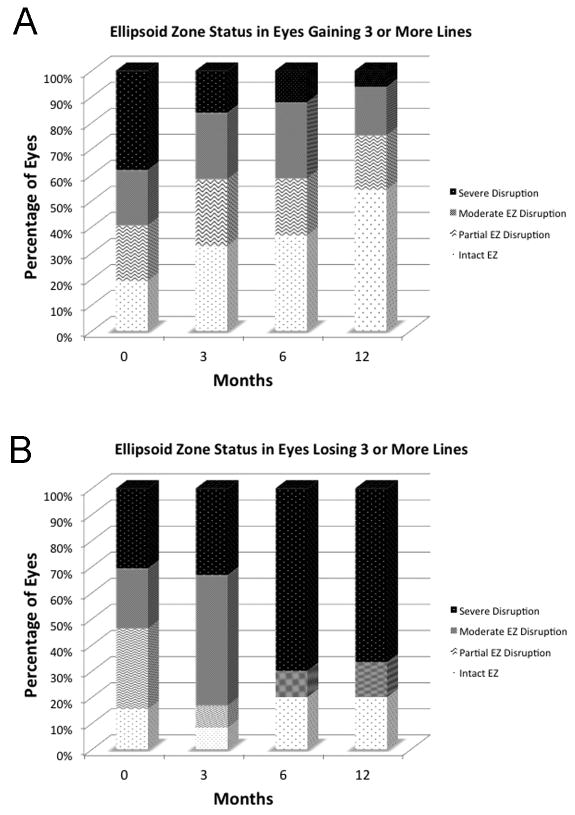
Eyes which gained 3-lines or more were compared to eyes that lost 3-lines or more with respect to SDOCT parameters. In eyes gaining 3-lines or more, complete EZ integrity was noted in 26 of 50 eyes (52%) at final follow-up. On the other hand, eyes that lost 3-lines or more exhibited moderate to severe EZ disruption in 12 of 15 eyes (80%) at final follow-up. Longitudinal changes in EZ status were also different between the groups, Figure 1. In addition to EZ integrity, baseline severe IRF was significantly greater in eyes gaining 3 lines or more of VA compared to eyes that lost 3 lines or more (p = 0.026). Posterior vitreous separation, ERM, and SRF were not significantly difference between these two groups.
Figure 1.
Longitudinal ellipsoid zone dynamics stratified by significant visual gain (3 lines or more, A) or significant visual loss (3 lines or more). A. In eyes gaining 3 lines or more, the number of cases with an intact ellipsoid zone increased over time, whereas the number of eyes with severe disruption decreased. B. In the eyes that lost 3 lines or more, the number of eyes with severe disruption increased and the number of eyes with intact ellipsoid zone decreased.
In examining eyes with more moderate changes in visual acuity, 72 eyes (45%) gained 1-line or more of visual acuity following treatment and 31 (20%) experienced 1 line or greater vision loss. PVS, ERM and SRF were not significantly difference between these two groups. The presence of severe IRF and EZ status at baseline were significantly different between these two groups, similar to the more significant responders (P < 0.001, 0.014, respectively).
Baseline Visual Acuity: OCT Features and Anti-VEGF Response
The correlation between OCT findings and treatment response was also assessed in the context of baseline VA (e.g., eyes at 20/40 or better at baseline, eyes at 20/50 or worse at baseline). Eyes with visual acuity 20/40 or better at the baseline (n = 56) showed stable visual acuity at the final follow-up (mean line change; -0.27 ± 1.5). The cases with visual acuity 20/50 or less at the base line (n = 103) showed visual acuity improvement at the final visit (mean line change; 1.9 ± 3.9). The presence of SRF (P = 0.045), severe IRF (P < 0.001) and EZ status (P < 0.001) at baseline was significantly higher in the 20/50 or worse group.
In the eyes with VA of 20/50 or worse at baseline, 48 cases (47%) showed 3-lines or more VA improvement at last visit. In eyes gaining 3 lines or more of VA, the baseline VA (20/140) was significantly worse than those eyes that did not gain 3 or more lines of VA with baseline 20/50 or worse vision (20/108, p = 0.018). There was no difference in baseline EZ status between these 2 groups, however there was a significantly higher incidence of severe IRF at baseline in those eyes gaining 3 lines or more compared to those that did not (78% vs 0%, P < 0.001). The final VA between these two groups was significantly different. Although the baseline visual acuity was lower in those eyes gaining 3 lines or more, the final visual acuity was significantly better compared to those that did not gain 3 lines ore more (20/45 vs 20/126, p < 0.001). At final follow-up, EZ restoration was significantly higher in those eyes gaining 3 lines or more compared to eyes that did not (54% vs 18%,p = 0.00013). The incidence of severe IRF was reduced from 78% to 40% in those eyes gaining 3 lines or more. Whereas, it increased from 0% to 13% in those eyes that did not gain 3 lines or more.
Quantitative Assessment of OCT Features in DME
At initial visit, the mean CST was 441.2 microns and 356.3 microns at final visit (P < 0.0001). In eyes that gained 3 lines or more, CST was 474.9 microns at baseline and 338.2 microns at 12 months (29% of decrease from initial visit). This weakly but significantly correlated with VA change (p = 0.029). In eyes that lost 3 or more lines, CST was 500.6 microns at baseline and decreased to 396.5 microns at final visit (21% of decrease from initial visit). This change did not correlate with VA change. Macular volume appeared to show more clear differences in the impact of anti-VEGF therapy between the two groups. The macular volume in those eyes gaining 3 or more lines was reduced by 12.2% over the course of the study compared to a reduction of 2.4% in those eyes losing 3 or more lines of vision (P = 0.024).
Discussion
Although numerous reports have demonstrated the efficacy of intravitreal anti-VEGF therapy for DME, the ideal approach to management, including drug choice and therapeutic regimen have not been fully established. The recent Protocol T results has changed the conversation regarding optimal anti-VEGF regimens for DME therapy, as well as the potential impact of baseline clinical features (e.g., visual acuity, OCT thickness)15 Although aflibercept was more effective for visual improvement at 1-year in eyes with worse baseline visual acuity (e.g., 20/50 or worse), there appeared to be no differences in functional outcomes between drugs when initial visual impairment was mild (e.g., 20/40 or better). Given that multiple factors, ranging from macular ischemia to potential systemic parameters, 13 may impact the pathogenesis and prognosis of DME, identifying optimal treatment regimens and potential imaging biomarkers is critical to facilitate improved patient counseling and enhance overall outcomes. In this study, we examined the potential OCT features that may be associated with anti-VEGF response. Around one-third of eyes gained 3-lines or more of VA, but 10% of eyes lost 3-lines ore more of VA. The functional response to anti-VEGF therapy was correlated with select baseline SDOCT features, including EZ status and severity of IRF.
Haritoglou C et al reported the correlation between retinal thickness and visual acuity 6 weeks following intravitreal bevacizumab for DME.16 Soheilian M et al also reported the correlation between central macular thickness and vision change up to 6 weeks following intravitreal bevacizumab for DME.17 There are several reports evaluating the central retinal thickness on OCT following DME treatment.13,16-20 In our study, the degree of CST change in eyes gaining 3-lines or more correlated to visual acuity change at 12 months, but this correlation did not hold true in eyes that did not gain 3-lines or more.
One key feature in visual prognosis in many diseases is the EZ status. Minimal research has evaluated EZ dynamics and DME response to anti-VEGF therapy. The correlation between EZ integrity and visual function by utilizing microperimetry.21 In that report, disruption of EZ was correlated with a significant decrease in point sensitivity in eyes with DME, but this did not evaluate the impact of EZ status and anti-VEGF response. In our manuscript, EZ integrity was significantly associated with VA response to anti-VEGF therapy. The EZ status may be a particular important marker for overall prognosis with anti-VEGF therapy. Novel approaches to EZ metrics, including quantitative assessment may provide additional insights into its prognostic value.22 In this study, eyes that have an intact EZ at baseline may do particularly well with anti-VEGF therapy.
Given the recent findings of the Protocol T study, this report also evaluated eyes for anti-VEGF response based on initial VA. In our study, 47% of the cases with visual acuity 20/50 or less at initial visit showed 3 lines or more visual acuity improvement. In these eyes, the presence of severe IRF was more frequently present compared to eyes that did not show similar improvement. The IRF severity improved in eyes gaining 3 lines or more while undergoing anti-VEGF therapy. It is not clear why those eyes with more severe IRF tended to gain more visual acuity. One possible reason includes that eyes with less IRF may have more baseline macular ischemia with less room for improvement. Additionally, simply having a greater amount of fluid at baseline may also allow for more significant reduction in IRF with anti-VEGF therapy with concomitant improvement in visual acuity. Although the EZ status was similar at baseline in these 2 groups, there was significantly greater EZ reconstitution/recovery in eyes that improved 3 lines or more. The relative contribution of EZ recovery and IRF improvement to the overall change in VA is not known and deserves further research.
As with any retrospective analysis, there are important limitations of this study. In particular, a lack of both a control group and standardized treatment regimen makes some of the results challenging to interpret. The overall magnitude of OCT thickness reduction may also suggest undertreatment. Limited angiographic data provides a challenge in accounting for macular ischemia. Quantitative metrics for intraretinal fluid, subretinal fluid, and ellipsoid zone integrity are not readily available. Our group and others are developing quantitative assessment tools for many of these pathology characteristics, including volumetric intraretinal fluid assessment and ellipsoid zone quantification.22,23 In the future, these analytic tools may provide new insights into overall OCT features and disease response.
In conclusion, this report demonstrates that baseline SDOCT features may be associated with overall functional response to anti-VEGF therapy. Further investigation with a more regimented treatment paradigm and quantitative assessment of OCT pathologic variables would be helpful to validate the predictive value of these characteristics at baseline.
Acknowledgments
Funding Support: NIH/NEI K23-EY022947-01A1 (JPE); Ohio Department of Development TECH-13-059 (JPE, SKS); Research to Prevent Blindness (Cole Eye Institutional Grant); The Robert Machemer Foundation Vitreoretinal Scholarship (YI)
Footnotes
Financial Disclosures: YI: None; DP: None; PKK: Thrombogenics (C), Alcon (C), Novartis (C), Allegro (C); RPS: Regeneron (C) Genentech (C), Thrombogenics (C), Alcon (C); JPE: Bioptigen (C, P), Thrombogenics (C, R), Genentech (R), Regeneron (R), Leica (C), Zeiss (C), Synergetics (P), Alimera (C), Santen (C), Alcon (C)
References
- 1.Rogers SL, Tikellis G, Cheung N, et al. Retinal arteriolar caliber predicts incident retinopathy: the Australian Diabetes, Obesity and Lifestyle (AusDiab) study. Diabetes Care. 2008 Apr;31(4):761–3. doi: 10.2337/dc07-1622. [DOI] [PubMed] [Google Scholar]
- 2.Petrella RJ, Blouin J, Davies B, Barbeau M. Prevalence, Demographics, and Treatment Characteristics of Visual Impairment due to Diabetic Macular Edema in a Representative Canadian Cohort. J Ophthalmol. 2012;2012:159167. doi: 10.1155/2012/159167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soheilian M, Ramezani A, Bijanzadeh B, et al. Intravitreal bevacizumab (avastin) injection alone or combined with triamcinolone versus macular photocoagulation as primary treatment of diabetic macular edema. Retina. 2007 Nov-Dec;27(9):1187–95. doi: 10.1097/IAE.0b013e31815ec261. [DOI] [PubMed] [Google Scholar]
- 4.Solaiman KA, Diab MM, Abo-Elenin M. Intravitreal bevacizumab and/or macular photocoagulation as a primary treatment for diffuse diabetic macular edema. Retina. 2010 Nov-Dec;30(10):1638–45. doi: 10.1097/IAE.0b013e3181e1ed07. [DOI] [PubMed] [Google Scholar]
- 5.Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol. 1995 Sep;113(9):1144–55. [PubMed] [Google Scholar]
- 6.Soheilian M, Ramezani A, Obudi A, et al. Randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus macular photocoagulation in diabetic macular edema. Ophthalmology. 2009 Jun;116(6):1142–50. doi: 10.1016/j.ophtha.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Lam DS, Lai TY, Lee VY, Chan CK, et al. Efficacy of 1.25 MG versus 2.5 MG intravitreal bevacizumab for diabetic macular edema: six-month results of a randomized controlled trial. Retina. 2009 Mar;29(3):292–9. doi: 10.1097/IAE.0b013e31819a2d61. [DOI] [PubMed] [Google Scholar]
- 8.Rajendram R, Fraser-Bell S, Kaines A, et al. A 2-year prospective randomized controlled trial of intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema: 24-month data: report 3. Arch Ophthalmol. 2012 Aug;130(8):972–9. doi: 10.1001/archophthalmol.2012.393. [DOI] [PubMed] [Google Scholar]
- 9.Diabetic Retinopathy Clinical Research Network. Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015 Mar 26;372(13):1193–203. doi: 10.1056/NEJMoa1414264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korobelnik JF, Do DV, Schmidt-Erfurth U, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2014 Nov;121(11):2247–54. doi: 10.1016/j.ophtha.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Domalpally A, Ip MS, Ehrlich JS. Effects of intravitreal ranibizumab on retinal hard exudate in diabetic macular edema: findings from the RIDE and RISE phase III clinical trials. Ophthalmology. 2015 Apr;122(4):779–86. doi: 10.1016/j.ophtha.2014.10.028. [DOI] [PubMed] [Google Scholar]
- 12.Elman MJ, Aiello LP, Beck RW, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010 Jun;117(6):1064–1077. doi: 10.1016/j.ophtha.2010.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsuda S, Tam T, Singh RP, et al. The impact of metabolic parameters on clinical response to VEGF inhibitors for diabetic macular edema. J Diabetes Complications. 2014 Mar-Apr;28(2):166–70. doi: 10.1016/j.jdiacomp.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Kriechbaum K, Prager S, Mylonas G, et al. Intravitreal bevacizumab (Avastin) versus triamcinolone (Volon A) for treatment of diabetic macular edema: one-year results. Eye (Lond) 2014 Jan;28(1):9–15. doi: 10.1038/eye.2013.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015 Mar 26;372(13):1193–203. doi: 10.1056/NEJMoa1414264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haritoglou C, Kook D, Neubauer A, et al. Intravitreal bevacizumab (Avastin) therapy for persistent diffuse diabetic macular edema. Retina. 2006 Nov-Dec;26(9):999–1005. doi: 10.1097/01.iae.0000247165.38655.bf. [DOI] [PubMed] [Google Scholar]
- 17.Soheilian M, Ramezani A, Obudi A, et al. Randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus macular photocoagulation in diabetic macular edema. Ophthalmology. 2009 Jun;116(6):1142–50. doi: 10.1016/j.ophtha.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 18.Cheema HR, Al Habash A, Al-Askar E. Improvement of visual acuity based on optical coherence tomography patterns following intravitreal bevacizumab treatment in patients with diabetic macular edema. Int J Ophthalmol. 2014 Apr 18;7(2):251–5. doi: 10.3980/j.issn.2222-3959.2014.02.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takamura Y, Tomomatsu T, Matsumura T, et al. The effect of photocoagulation in ischemic areas to prevent recurrence of diabetic macular edema after intravitreal bevacizumab injection. Invest Ophthalmol Vis Sci. 2014 Jul 15;55(8):4741–6. doi: 10.1167/iovs.14-14682. [DOI] [PubMed] [Google Scholar]
- 20.Mushtaq B, Crosby NJ, Dimopoulos AT, et al. Effect of initial retinal thickness on outcome of intravitreal bevacizumab therapy for diabetic macular edema. Clin Ophthalmol. 2014 Apr 28;8:807–12. doi: 10.2147/OPTH.S56624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yohannan J, Bittencourt M, Sepah YJ, et al. Association of retinal sensitivity to integrity of photoreceptor inner/outer segment junction in patients with diabetic macular edema. Ophthalmology. 2013 Jun;120(6):1254–61. doi: 10.1016/j.ophtha.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Itoh Y, Vasanji A, Ehlers JP. Volumetric ellipsoid zone mapping for enhanced visualisation of outer retinal integrity with optical coherence tomography. Br J Ophthalmol. 2015 doi: 10.1136/bjophthalmol-2015-307105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu D, Yuan A, Kaiser PK, et al. A novel segmentation algorithm for volumetric analysis of macular hole boundaries identified with optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54(1):163–9. doi: 10.1167/iovs.12-10246. [DOI] [PubMed] [Google Scholar]