Abstract
Although asthma self-management depends on ongoing and accurate self-assessment by the patient, pediatric asthma patients have weak skills in the area of symptom perception. Before developing an asthma game targeted to improving asthma self-management and improved symptom awareness, we sought to identify gaps in existing games. To clarify the role of relatedness and autonomy in asthma health game design, we investigated symptom awareness, vocabulary, and self-determination through a series of semi-structured interviews with children suffering from asthma. Using self-determination theory as a framework, interviews were oriented to patients' illness experience and vocabulary related to symptomatology, as well as to recreational activities. Formative analysis of the interviews reveals attitudes, perceptions, and motivational factors arising in the context of childhood asthma, and it elucidates the images and vocabulary associated with both illness experience and recreational activities. Qualitative assessment of patient perspectives leads to specific recommendations for game design ideas that will support market entry of a spirometer-controlled game for children with asthma.
Keywords: : Asthma, Self-determination, Games, Child, Recreational activities, Chronic disease
Introduction
With an estimated prevalence of nearly 8.3% in the United States, asthma is the most common chronic disease of childhood.1 More than half of children with asthma experience exacerbations annually, and 53% of children feel that their asthma is not well controlled.1,2 Exacerbations and poor adherence to asthma medications are undoubtedly related to pediatric asthma patients' relatively weak skills in the area of symptom perception.3 Discrepant assessments of symptoms between patients, parents, and providers compound this problem, and they highlight the need to develop patient-centered educational tools.2,4–8
Asthma-related games for health have included games that deal primarily with cognitive content and education, rather than symptom perception per se: The Quest for the Code (Starlight) is a game that requires the player to solve a puzzle by using their knowledge of asthma triggers and medications. The goal of the game is to let kids understand asthma and identify ways of responding to its changing symptoms. Lungtropolis (ORCAS) is an arcade game of puzzles that presents details of managing asthma. SpiroGame ties spirometry measurements to two complex games with different levels of difficulty.9,10 Bronkie the Bronchiasaurus is an asthma game in which the protagonist navigates a fantasy world where a villain has stolen a machine to keep the air clean; players must employ their knowledge of asthma management to clean up the air and move through the game.11 Asthma-related health games may contribute to self-management skills,12 whereas available games tend to take a didactic, cognitive, or physical training approach, and they do not address symptom perception directly. The optimal design of a game that is oriented to empower symptom perception, especially if it is to compete with other recreational digital media, depends on a sound understanding of children's disease-related vocabulary, perceptions, and motivational context.
Self-determination theory (SDT) identifies competence, autonomy, and relatedness as the building blocks of intrinsic motivation. In the clinical arena, SDT predicts that interventions with the best chance of promoting health-related behavior change (e.g., adherence) will be those meeting these three needs.13,14 A premise of this study, and of the games for health movement in general, is that the avidity of many adolescents for digital entertainment reflects the capacity of such activity to meet these basic needs.15 Moreover, Parisod et al. found an increased efficacy of games that are designed “according to some theoretical framework, in a multidisciplinary team including the target audience.”16 Using SDT as a framework, we sought to examine attitudes, perceptions, and motivational factors that play a role in childhood asthma, with a specific focus on accounts of illness experience and on preferred recreational activities.
One way to improve pediatric patients' awareness of their lung mechanics is to give them a chance to “play with their breath” by using a spirometer—a device that renders graphic, real-time representations of the user's breath volume and flow—as a game controller.17 Currently, digital spirometer games are limited to “warm-up” casual games during diagnostic spirometry within a clinical setting. Manufacturers of diagnostic spirometry have tried to solve the problem of children's affective engagement by interpolating playful characters onto a screen during this laboratory test. This design feature of diagnostic spirometry indicates spirometer manufacturers' interest in engaging children's sense of competence and playfulness by giving them a brief opportunity to practice, effectively coordinating their oral and respiratory muscles as required for reliable spirometry.
Beyond the spirometry technique, spirometer-controlled breath games could have implications for breath awareness. As with other games utilizing biofeedback, spirometer games provide the player with a different kind of “flow”: direct, real-time information regarding dynamic changes in airway resistance. Preliminary experience of other pediatric patients with chronic respiratory disease suggests that spirometer games have the potential to engage players' attention and sense of fun.17,18
Guided by SDT, and to inform design specifications of a spirometer-controlled game that will support symptom awareness, interviews reported here aimed at elucidating vocabulary and narrative regarding illness experience (asthma symptoms, experience with medications, and illness experience), and recreational activities, among asthma patients attending a pediatric pulmonary clinic. What images do pediatric patients use to describe their symptoms? In what areas of their lives do pediatric asthma patients feel in control? What are their preferred recreational activities, digital and nondigital? What do they think of a digital game aimed at improving asthma symptom awareness? This knowledge will have important implications for the design of an asthma health game.
Methodology
Subjects were recruited from the outpatient Children's Specialty Clinic and from inpatient admissions to the Vermont Children's Hospital. Subjects had to have an existing diagnosis of asthma—mild persistent or worse—for inclusion. Subjects with other co-existing chronic illnesses were excluded from the study. Parents consented to the study, and patients older than the age of 11 also gave verbal assent to be interviewed. A total of 15 children, 87% of whom were male, met inclusion criteria (Table 1). The average age of the interviewees was 11.9 years old (SD of ±2.7, range of 7–17).
Table 1.
| Demographics | |
|---|---|
| Gender (% male) | 87 |
| Age (mean ± SD [range]) | 11.9 ± 2.7 (7–17) |
| Gaming hours per day estimated (mean ± SD [range])a | 1.2 ± 1.2 (0.12–3) |
Gaming hours were calculated by assigning 1 hour values to the reported gaming frequency, if average length of play was not otherwise specified.
The major interview domains were asthma experience, recreational activities, and brainstorming on an asthma game for health. After a literature review of core issues in pediatric asthma, including review of a questionnaire from the SDT community website, a semi-structured interview guide was created and is included as Figure 3 in the appendix.19 Subjects were asked directive questions regarding their autonomy with regard to asthma medication (without distinction made between preventative and rescue medication regimes), and also about what activities, in general, were compelled versus elective.
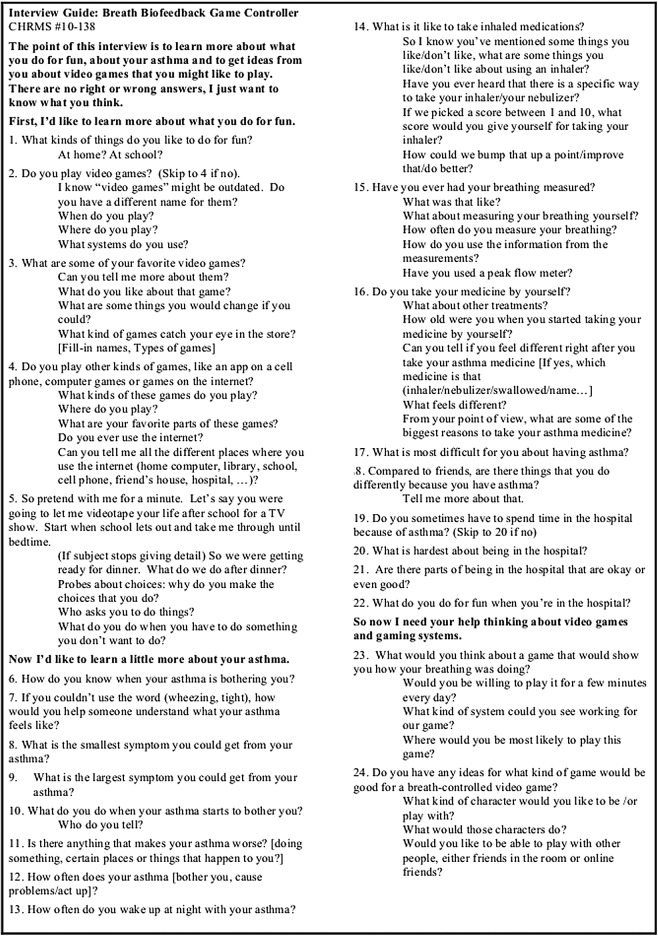
FIG. 3.
This template was used to guide open-ended interviews of children with asthma.
Interviews were recorded and then transcribed verbatim by a research assistant. After transcription, a team of three readers read each transcript individually and generated subcategories from each question and answer pair. After the subcategories were generated, all three readers came to consensus on the subcategories to include in the final analysis. The transcripts were then entered line by line into a spreadsheet and recoded by all three readers by subcategory. The subcategory coded spreadsheets were compared, and agreement was reached on the appropriate subcategory code for each question and answer pair. Finally, a summary sentence for each subject in each subcategory was generated and assimilated into a summary paragraph for all subjects for each subcategory.
Results
Illness experience—symptom vocabulary
“When I feel a tightness in my body, that's when I know I have asthma.”
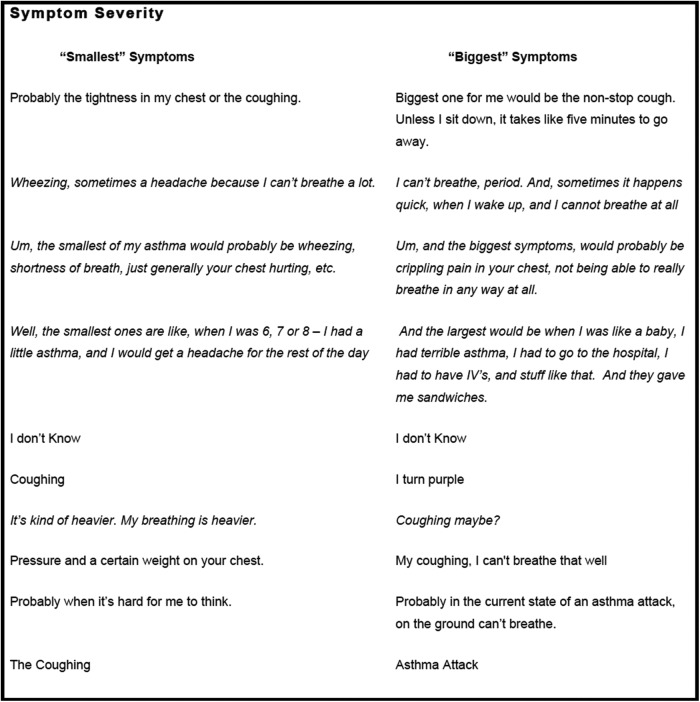
For the 15 children interviewed, the most common phrases to describe asthma-associated symptoms include can't breathe, chest tightness, wheezing, and cough, with can't breathe commonly identified as the “biggest” or most severe symptom experienced (Figs. 1 and 2). Most children could identify symptoms associated with an asthma attack, though one child was unable to describe associated symptoms, and another denied having asthma altogether. Other children described symptoms in vague terms such as “I feel like something's going wrong,” and “I can't do as many things.” Interviewees interpreted decreasing daytime exacerbations and/or a decrease in nocturnal awakenings as signs of improved asthma control.
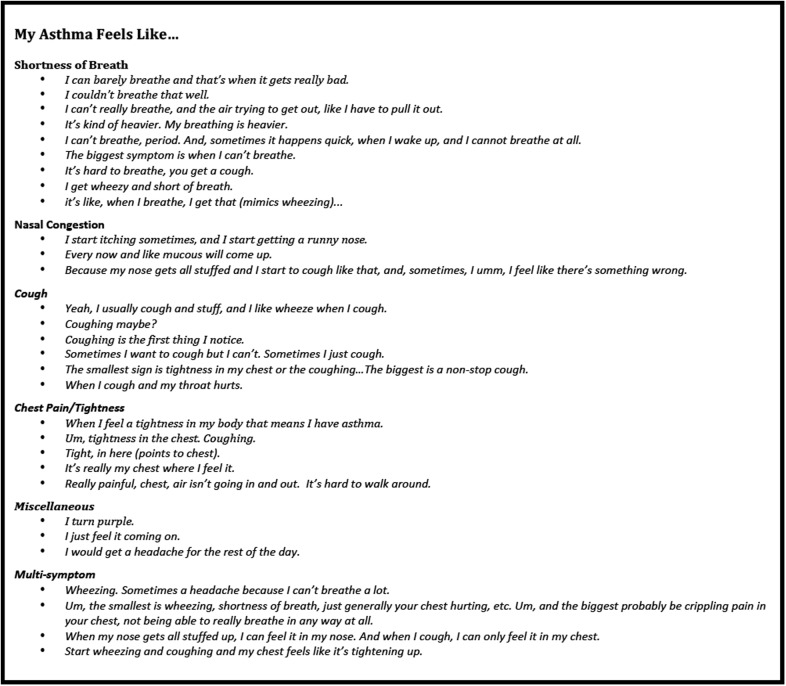
FIG. 1.
Respondents' descriptions of asthma symptoms are stratified into review of system categories.
FIG. 2.
Interviewees' responses are organized by symptom severity into two categories, least severe or “smallest” symptom and most severe or “biggest” symptom.
Self-identified symptom triggers fell into three main categories: activity associated, concurrent illness, and environmental. Of the 11 children who identified specific triggers for asthma symptoms, 8 identified exertion as a significant trigger. Examples included gym class, the mile run trial, basketball practice, and active videogames such as Wii™ boxing. Concurrent colds and/or allergies were commonly identified as tied to increasing nocturnal symptoms. Temperature extremes as well as seasonal shifts were commonly identified environmental triggers. Finally, two interviewees, respectively, identified smoke and pulmonary function testing (“PFTs”) as triggers.
Illness experience—medications
“It's tough and you can feel it go down your throat.” “Tastes really bad.” “Yeah, usually it's within 1–5 minutes I feel better. Don't feel total effects until maybe a half hour later.” “I take it because generally if I don't, I'll have a hard time the next day and it's not fun.”
Some children attributed unpleasant tastes or sensations to their inhaler. Others described forgetting the spacer, forgetting to take a second puff, taking too early of a puff, and not waiting long enough before physical activity. Many respondents were especially brief in their responses or unable to elaborate on particular details of medication use, such as the experience of using an inhaler. Children reported mixed benefits from inhaler use: Some noticed no symptomatic relief, whereas others identified a substantial improvement.
Parents were reported by interviewees as having varying levels of involvement, ranging from supervision of inhaler use, to allowing autonomous medication use, with most children receiving at least some form of a parental reminder. Motivation for medication use ranged from extrinsic—parental figures threatening punishment—to intrinsic—a direct association of personal benefit. The words of other interviewees suggested intrinsic sources of motivation: Take medication because: “… My doctor told me to,” or because “[if I don't] I'd probably get my hamsters taken away.” Take medications so: “… my asthma will get better,” or “… if I don't, I'll have a hard time the next day and it's not fun.” Still, most individuals' responses suggested a role for both forms of motivation: They realized the inherent benefit of their treatments, but required reminders and negative reinforcements to stay consistent. Most individuals' descriptions suggested both forms of motivation.
Illness experience—spirometry
“It feels like you're giving up all your breath.”
Although all had undergone clinical spirometry, few subjects recalled the experience of spirometry/pulmonary function testing. Some focused on the “not fun,” obligatory aspect of pulmonary function tests, a sense that “it feels like you're giving up all your breath.” Others enjoyed the gaming aspect of the test, “it was fun, I wanted to kill the clown” (one of the PFT scenarios at our center includes a graphic where exhalations inflate and, ultimately, cause a balloon to explode, killing a clown character). The majority, however, concluded that they “don't think about it that much.”
Illness experience—hospitalization
About half of our subjects gave accounts of being in the hospital, or being rushed to the hospital, for their asthma. Although there was a clear sense that their symptoms were intensified both during and before the stay, most subjects also recalled recreational activities as a “bright side” to hospitalization. These included games and diversions such as scooters, videogames, and crafts. Respondents voiced dislike of intravenous lines and injections.
Illness experience—life with asthma
“… you can't be next to a fire with marshmallows …”
From a summer activity to gym class and sports, subjects identified missing out as the most difficult part of life with asthma. For some interviewees, avoiding triggers or symptoms led them to skip activities entirely. For others, the need for an inhaler meant that they had to stop engaging in desired activities such as basketball, soccer, and other team sports. One subject shared that he stopped playing soccer, because his “asthma was getting harder to control.” Another concluded that “it affects everything that I do.” Interviewees also noted that they avoided full exertion for fear of causing an asthma exacerbation: “I'm almost afraid to go out and try too hard and then end up suffering.” Other challenges included missing extensive school, recurrent nocturnal symptoms, and fatigue associated with disrupted sleep and a feeling of being “weak” or an “outcast.” Interviewees identified relatedness over the idea of asthma: Friends with asthma were cited as a positive influence, because they can look out for one another and take a break without feeling as left out.
Recreation—general
When asked about favorite recreational activities, interviewees reported a range of physical activities, including: football, basketball, baseball, hockey, soccer, badminton, karate, swimming, wrestling, bicycling, skateboarding, hunting, and fishing. Almost all individuals (14/15) engaged in some form of outdoor activity. Three participants engaged in activities requiring a greater degree of responsibility such as tutoring, community service, animal care, and housework. Most individuals included TV and videogames in their list of favored recreational activities.
When asked about compelled activities, subjects most often brought up house-hold responsibilities and homework. In these arenas, respondents consistently reported a parental role, ranging from gentle reminders to verbal scolding or “getting grounded.” The degree of intrinsic versus extrinsic motivation contributing to such activities ranged among interviewees. Statements suggesting extrinsic motivation included doing homework because “… my mom wants me to” or “… to get my grades and get out of school”; cleaning room because: “… if I don't, my mom flips.”
All 15 children specified prior digital gaming experience—length of play was not otherwise specified during the interview (Table 1). Interviewees reported playing an array of games: first-person shooter games such as Call of Duty and Ghost Recon; hand-held games such as Super Mario Brothers; internet-based games such as Addictinggames.com and Farmville; computer games such as World of War Craft, Woonscape, and Destroy All Humans; and Wii Sports. Gaming platforms included Wii, Xbox®, Nintendo® 64, Game Cube, Play Station 2, DS, personal computers, and cell phones.
Individuals identified favorite games and systems based on heightened physical interaction, found in Wii games; and multi-player function, seen in Nintendo's Super Smash brothers; collaborative online games such as World of Warcraft; and Xbox Live where friends talk online via headsets during team-oriented gaming.
Other features interviewees found desirable included multiple levels/worlds, customizability, and point-earning/score-keeping. Interviewees described a range of time spent with videogames, from several hours daily, to only on weekends. Most individuals described some ambivalence regarding their autonomy in deciding to engage with digital games—how this activity competes with homework and other responsibilities.
Recreation—games for health ideas
“Go through part of the body to the parts that have the asthma…search the body…see about medication…do something to help that part feel better”
“I want to be Justin Bieber (describes how singing would tie into the breathing component).”
“It would have to be something that was an active experience, like for the Wii or the Playstation, where you move around.”
“It would be a good balance because sometimes your asthma can interfere with having fun.”
Respondents' ideas for breath-activated game scenarios included a breath-powered hunting game, a racecar game, and a balloon-inflating carnival game. Themes occurring in daily gaming suggested for an asthma-related game that included a multi-player component, multiple levels and worlds, and some form of score keeping that could be tabulated over hours or days.
Discussion
Considering symptom perception as a relatively weak, but ostensibly remediable, area of competence in pediatric asthma patients, these interviews explored narratives of pediatric asthma patients regarding their bodily awareness of asthma. The interviews also focused on pediatric asthma patients' sense of competence, autonomy, and relatedness (SDT constructs) in the context of their illness experience, and of their recreational activities. The recurring themes that we identified inform the design of digital educational media aimed at improving symptom awareness in pediatric asthma patients.
Illness experience
Interviewees conveyed their knowledge, beliefs, and attitudes regarding symptoms, medication, and the illness role in general, including interactions with the healthcare system.
Symptom terminology often featured conventional, clinical style terms for subjects' symptoms (“wheezing, cough). Narrative also included relatively charged, dramatic imagery to describe asthma symptoms: chest tightness, just can't breathe, heavy breathing, weight on your chest, and crippling chest pain (Fig. 1). By meeting pediatric patients at their level of linguistic competence for symptom description, game imagery that aligns with these descriptions may have a better chance of engaging players' attention.
The variability of responses may cast light on the “communication gap” regarding self-report of asthma symptoms, and it may also indicate that asthma patients experience variable symptoms that are not directly related to bronchospasm. One previous study found that half of asthma patients report nonstandard asthma symptoms, whereas two other studies found that parents of children with poorly controlled asthma paradoxically reported good control.4–6 Together, these findings indicate the benefit of a design feature that could align asthma symptoms with asthma control, so as to help get players and their parents “on the same page” with regard to identifying and tallying the frequency of asthma symptoms.
Variability in the severity of subjective ratings of breathlessness for a degree of airflow obstruction reflects a range of perceptual skill among patients with asthma that may also be age dependent.4,20 Improving this skill may impact healthcare costs, considering the association between inaccurate symptom perception and increased healthcare utilization (hospitalization and ER visits).21
Medication
Narratives carried a range of attitudes regarding subjects' experience with medication. Many disliked using an inhaler because of the time, the distraction from preferred activities, and unpleasant taste, though some appreciated the relief of their symptoms. Summary descriptions of asthma symptoms only occasionally touched on medications' impact on their symptoms. This paucity of narrative regarding medications' impact may also relate to pediatric patients' reported tendency to ignore early warning signs of asthma exacerbations. The frequent ambivalence and ambiguous valuations of medication also accord with the findings of Naimi et al., whose subjects also struggled with dislike of the taste, with being busy or distracted, and with ambivalence about efficacy.7 Game design features specifically addressing the efficacy of medication when used sooner versus later could help address these issues.
Illness role
Illness role is another quality that varied among our subjects. The majority of respondents described both extrinsic and intrinsic motivation. It is unclear whether the components of motivation—autonomy, competency, and relatedness as described in the framework of SDT—develop on a similar timeline for treatment adherence as compared with other tasks of childhood such as homework and chores. In a study involving children with CF, we found that children reported relatively lower levels of autonomy and relatedness when discussing respiratory therapies compared with other daily activities.22 This finding points to an area of psychological stress for pediatric asthma patients that spirometer games can address in a number of ways. Responsive design features could include support for autonomy, and specifically tailored themes such as a multiplayer component or online play, as well as keeping track of scores to target relatedness as well as competency.
Studies by Vilozni et al. on SpiroGame support this prediction. In a trial of children using either SpiroGame or traditional commercial software with a simulation of blowing out candles, SpiroGame was associated with a statistically significant improvement in spirometry performance. A subsequent study found that these improvements in spirometry were reproducible even in very young children.9,10 Another study by Lieberman studied subjects who played Bronkie the Bronchiasaurus (Bronkie) and found that a single 40 minute session of game play was associated with an improvement in self-efficacy and asthma knowledge that persisted for a month.11 In another arm of the trial, Bronkie was compared with a traditional asthma education video and adolescents who played the videogame demonstrated statistically significant improvements in asthma self-efficacy. These studies support the idea that health games can support autonomy in the area of self-management and support decision making in chronic pediatric illness.9–11,23,24
Finally, the narratives of our subjects revealed the emotional burden of pediatric asthma. In alignment with prior research, subjects reported a strong sense that asthma causes them to miss out on desired activities, especially sports, games, and physical education. A factor to consider that we also found in a previous study involving interviews with pediatric patients with cystic fibrosis might be termed a “will to be normal.”22 Protudjer et al. probed a similar idea and found that children with asthma engaged in many strategies to normalize theirs lives with asthma.23 A trial of Bronkie in an inpatient setting found that there was high demand for the videogame for all pediatric patients regardless of admission diagnosis and that opportunities for social interaction were highly valued.11 By integrating everyday recreational activities (digital games) with awareness of changing disease activity, spirometer games have the potential to address the need for social connectivity, even in the face of chronic illness.
Recreational activity
Interview findings reveal the following reference points for the design of a digital game that could support symptom perception in pediatric asthma: (1) a social and/or competitive component with multiplayer or online play; (2) use of multiple levels/worlds; (3) an ability to track one's progress; (4) a kinesthetic component tracking inspiratory and expiratory movements; and (5) use or access to the game within the healthcare setting, since such sites, particularly the hospital, represent cross-roads where symptom discussions often take place, and considering that children already avail themselves of digital games for diversion in this setting. Prior studies illustrate how aspects of game design play a critical role in devising technologies that successfully impact clinical measures.25 Additional features suggested by prior literature include player selection and modification of protagonists to mimic player characteristics. For example, a player who has triggers related to allergies might have more play scenarios comprising this trigger whereas a player who uses the Emergency Room heavily could address how to avoid those visits.26
Conclusion
In summary, our results indicate that subjects do have a sense of what is needed for self-management and do have a strong autobiographical sense of their own fluctuating symptoms. Subjects' sense of autonomy relative to their asthma was strongly colored by a sense of dependence on medication, and on their parents' continual oversight of appropriate medication use. The sense of relatedness relative to illness experience was perhaps the most emotionally laden, conflicted area of the research findings, since subjects repeatedly found themselves with a loss of sense of relatedness due to contingencies imposed by their chronic illness.
These studies and our findings point to game design features that could support an approach to symptom perception, and awareness of medication benefits, as train-able competencies. Such an approach could improve asthma-related health outcomes while containing costs. For example, a spirometer game mechanic that prompts the player to explicitly compare pre- versus post-medication breath challenges could bridge a cognitive gap between symptom experience and medication effect.
The pooling of the target users' narratives regarding symptom vocabulary, social burdens of chronic illness, medication impacts, and self-directed activities, recreational and otherwise, support the development of an asthma-related digital game. In a broader context, interviews with would-be health-gamers can support game design efforts by elucidating children's understanding of their own disease process. Design lessons learned from this qualitative, exploratory study support the incorporation of themes of relatedness and autonomy in health game design.
Acknowledgments
This work was supported by NIH Grant R43 103370. The authors thank Jackie Swartz and the staff of the University of Vermont Medical Center for help in arranging interviews. They also thank Vermont Children's Hospital for providing space to carry out this study, and Dr. Thomas Lahiri who introduced the study to subjects (pediatric patients with asthma). They are grateful to the parents and children who kindly participated in this study.
Author Disclosure Statement
Dr. Bingham is co-inventor on a product patent held by the University of Vermont and has an affiliation with Respirames, Inc., a for-profit entity focused on health game research and development. The other authors have disclosed no conflict of interest.
References
- 1.Centers for Disease Control. Most Recent Asthma Data. 2015
- 2.Shefer G, Donchin M, Manor O, et al. Disparities in assessments of asthma control between children, parents, and physicians. Pediatr Pulmonol 2014; 49:943–951 [DOI] [PubMed] [Google Scholar]
- 3.Feldman JM, McQuaid EL, Klein RB, et al. Symptom perception and functional morbidity across a 1‐year follow‐up in pediatric asthma. Pediatr Pulmonol 2007; 42:339–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoos HL, Kitzman H, McMullen A, et al. The language of breathlessness: Do families and health care providers speak the same language when describing asthma symptoms? J Pediatr Health Care 2005; 19:197–205 [DOI] [PubMed] [Google Scholar]
- 5.Guyatt GH, Juniper EF, Griffith LE, et al. Children and adult perceptions of childhood asthma. Pediatrics 1997; 99:165–168 [DOI] [PubMed] [Google Scholar]
- 6.Carroll W, Wilhaber J, Brand P. Parent misperception of control in childhood/adolescent asthma: The Room to Breathe survey. Eur Respir J 2012; 39:90–96 [DOI] [PubMed] [Google Scholar]
- 7.Naimi DR, Freedman TG, Ginsburg KR, et al. Adolescents and asthma: Why bother with our meds? J Allergy Clin Immunol 2009; 123:1335–1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Price D, Ryan D, Pearce L, et al. The burden of paediatric asthma is higher than health professionals think: Results from the Asthma In Real Life (AIR) study. Prim Care Respir J 2002; 11:30–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vilozni D, Barker M, Jellouschek H, et al. An interactive computer-animated system (SpiroGame) facilitates spirometry in preschool children. Am J Respir Crit Care Med 2001; 164:2200–2205 [DOI] [PubMed] [Google Scholar]
- 10.Vilozni D, Barak A, Efrati O, et al. The role of computer games in measuring spirometry in healthy and “asthmatic” preschool children*. Chest 2005; 128:1146–1155 [DOI] [PubMed] [Google Scholar]
- 11.Lieberman DA. Management of chronic pediatric diseases with interactive health games: Theory and research findings. J Ambul Care Manage 2001; 24:26–38 [DOI] [PubMed] [Google Scholar]
- 12.Hieftje K, Edelman EJ, Camenga DR, et al. Electronic media-based health interventions promoting behavior change in youth: A systematic review. JAMA Pediatr 2013; 167:574–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bruzzese JM, Kingston S, Sheares BJ, et al. Adherence to asthma medication regimens in urban African American adolescents: Application of self-determination theory. Health Psychol 2014; 33:461–464 [DOI] [PubMed] [Google Scholar]
- 14.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000; 55:68–78 [DOI] [PubMed] [Google Scholar]
- 15.Rigby CS, Przybylski A. The motivational pull of video games: A self determination theory. Motiv Emot 2006; 30:347–363 [Google Scholar]
- 16.Parisod H, Pakarinen A, Kauhanen L, et al. Promoting children's health with digital games: A review of reviews. Games Health J 2014; 3:145–156 [DOI] [PubMed] [Google Scholar]
- 17.Bingham PM, Bates JH, Thompson-Figueroa J, Lahiri T. A breath biofeedback computer game for children with cystic fibrosis. Clin Pediatr 2010; 49:337–342 [DOI] [PubMed] [Google Scholar]
- 18.Bingham PM, Lahiri T, Ashikaga T. Pilot trial of spirometer games for airway clearance practice in cystic fibrosis. Respir Care 2012; 57:1278–1284 [DOI] [PubMed] [Google Scholar]
- 19.Self-Determination Theory website. http://selfdeterminationtheory.org/ (accessed February24, 2017)
- 20.Manning HL, Schwartzstein RM. Respiratory sensations in asthma: Physiological and clinical Implications. J Asthma 2001; 38:447–460 [DOI] [PubMed] [Google Scholar]
- 21.Rhee H, Belyea MJ, Halterman JS. Adolescents' perception of asthma symptoms and health care utilization. J Pediatr Health Care 2011; 25:105–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bingham PM, Meyer M. Self determination and health behaviors in children with cystic fibrosis. Open Pediatr Med J 2011; 5:1–7 [Google Scholar]
- 23.Protudjer JL, Becker AB, Marchessault GD, Korzyrskyj AL. Normalization strategies of children with asthma. Qual Health Res 2009; 19:94–104 [DOI] [PubMed] [Google Scholar]
- 24.Kato PM, Cole SW, Bradlyn AS, et al. A video game improves behavioral outcomes in adolescents and young adults with cancer: A randomized trial. Pediatrics 2008; 122:e305–e317 [DOI] [PubMed] [Google Scholar]
- 25.Huss K, Winkelstein M, Nanda J, et al. Computer game for inner-city children does not improve asthma outcomes. J Pediatr Health Care 2003; 17:72–78 [DOI] [PubMed] [Google Scholar]
- 26.Bartholomew LK, Shegog R, Parcel GS, et al. Watch, Discover, Think, and Act: A model for patient education program development. Patient Educ Couns 2000; 39:253–268 [DOI] [PubMed] [Google Scholar]